Introduction
Previous research has shown that older women use more formal care than older men (Einiö et al., Reference Einiö, Guilbault, Martikainen and Poulain2012; Dorin et al., Reference Dorin, Krupa, Metzing and Büscher2016), while older men use more informal care (McCann et al., Reference McCann, Donnelly and O'Reilly2012), and especially spousal care, than women (Dorin et al., Reference Dorin, Krupa, Metzing and Büscher2016; Schmidt, Reference Schmidt2017). The differences in morbidity and mortality between older women and men are considered important drivers of these gender differences in long-term care (LTC) use. Women report poorer health (Boerma et al., Reference Boerma, Hosseinpoor, Verdes and Chatterji2016) and tend to suffer more often from long-term disabling conditions (Bird et al., Reference Bird, Shugarman and Lynn2002; Meinow et al., Reference Meinow, Wastesson, Kåreholt and Kelfve2020), whereas men more often have fatal conditions (Crimmins et al., Reference Crimmins, Shim, Zhang and Kim2019). In addition, men are usually older than their wives (McCann et al., Reference McCann, Donnelly and O'Reilly2012). Hence women tend to outlive their husbands and are more often dependent on formal LTC services. Another reason for this gender gap is that care use is deeply rooted in and intertwined with family relations and social and cultural norms. In traditional gender roles, caregiving has been considered more natural to women than men (Williams et al., Reference Williams, Giddings, Bellamy and Gott2017). Such norms can promote female caregiving for male partners, parents and relatives. In addition, men have been reported to prefer informal care use more often than women (Pinquart and Sorensen, Reference Pinquart and Sorensen2002) and to have higher expectations regarding informal caregiving from their partner (Williams et al., Reference Williams, Giddings, Bellamy and Gott2017). Thus, both health and social factors contribute to older men using more informal care – especially spousal care – than women, and to women using more formal care than men.
Such an individual-level explanation needs to be placed in the context of societal changes: in many countries the health and social resources of the older population as well as LTC policies have changed considerably in the past decades. This may have impacted both the demand for and supply of LTC in the older population (Agree and Glaser, Reference Agree, Glaser and Uhlenberg2009; Broese van Groenou and De Boer, Reference Broese van Groenou and De Boer2016). This raises the question of whether and to what extent men and women have been differently affected by these changes, and whether the gender gap in care use has possibly been affected as a result. The main aim of this study is to explore the robustness of the gender gap in various types of LTC use over a period of two decades (1995–2016) in the Netherlands.
Following the behavioural care model of Andersen and Newman (Reference Andersen and Newman2005), there are three types of individual determinants of care use: the need for care (health), the disposition to use care (e.g. education, mastery) and factors enabling the use of care (e.g. social resources). We add to current knowledge by identifying gender-related factors concerning the need for care, the disposition to use care and the factors enabling the use of care (Andersen and Newman, Reference Andersen and Newman2005). As such, we can identify and discuss, for example, gender-specific barriers to seeking care and access to care services. At the individual level, the model of Andersen and Newman (Reference Andersen and Newman2005) considers gender as a key determinant of health-care use, but there is less research available on how gender is associated with care use and which gender-related factors contribute to differences in care use. Observing the developments in care use over time in a single country study has the advantage that the entire study population experienced the same societal changes. When the individual-level changes are taken into account, better insight into the importance of societal factors, i.e. changes in LTC policies, is obtained. Trends in care use may thus in part be related to changes over time in these individual determinants at the population level and in part to unobserved changes in a societal context such as family relations and social and cultural norms, and LTC policies (Figure 1). Hence, we expect this exploration to add to our insight into how individual- and societal-level developments intertwine.
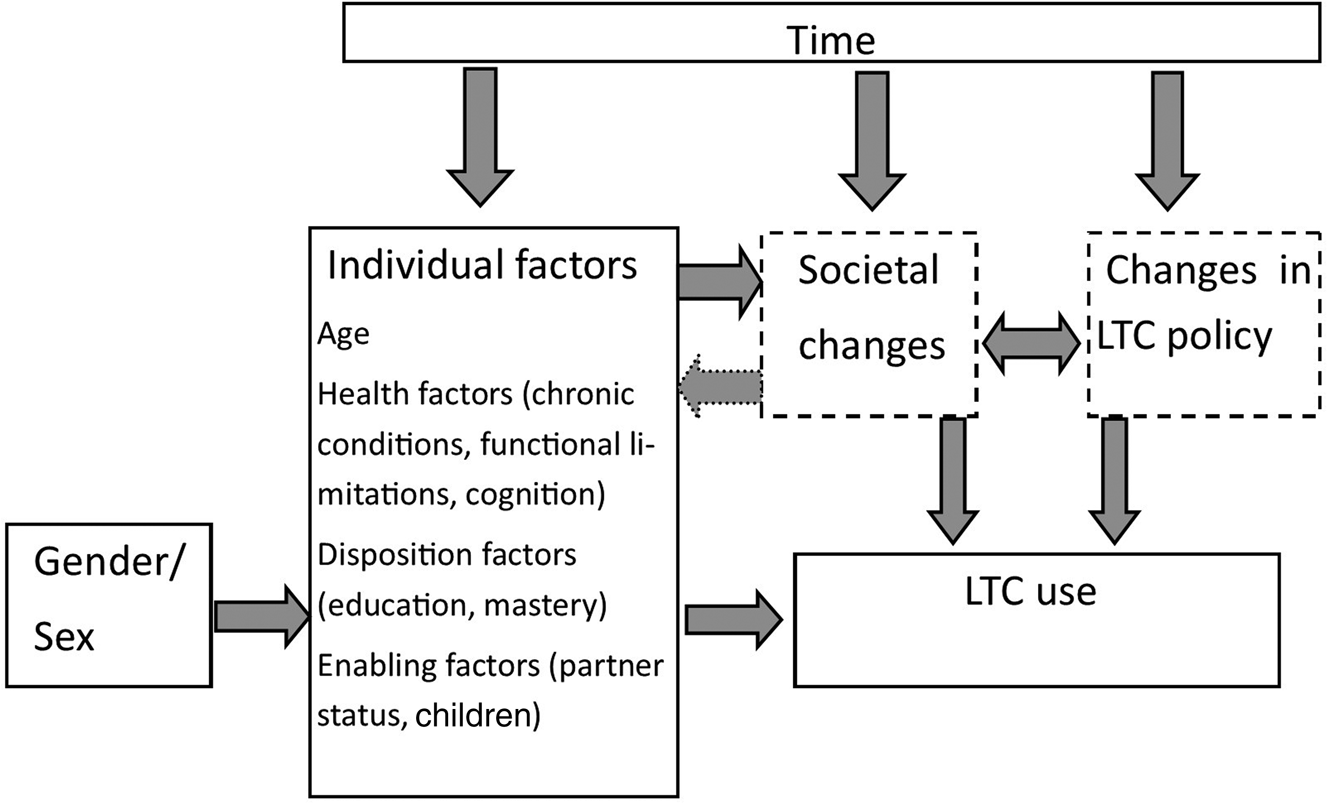
Figure 1. The conceptual framework of the determinants of care use.
Note: LTC: long-term care.
Source: Modified from the theoretical framework for health services utilisation by Andersen and Newman (Reference Andersen and Newman2005).
In the following, we elaborate on various developments in the Netherlands that may have impacted the gender gap in the use and non-use of care among the older population. The types of LTC use under study are formal care (home care and residential care), informal care (spousal care and other types of informal care) and privately paid help (generally in the household). Our research questions are:
(1) To what degree has the gender gap in the five types of care use and non-use of care changed between 1995 and 2016?
(2) To what degree are the gender differences in care use and their possible changes over time explained by individual determinants of care use (i.e. need, dispositional and enabling)?
Need for care
One important driver of the use of any type of care is health impairment: being in good health predicts the non-use of care, whereas being in poor health predicts the use of care. The fact that women have suffered from long-term disabling conditions more often than men (Bird et al., Reference Bird, Shugarman and Lynn2002; Meinow et al., Reference Meinow, Wastesson, Kåreholt and Kelfve2020) contributes to women's greater use of care. In the context of population ageing, both men's and women's life expectancies are increasing (Jørgensen et al., Reference Jørgensen, Fors, Nilsson, Enroth, Aaltonen, Sundberg, Brønnum-Hansen, Strand Bjørn, Chang and Jylhä2018), and in high-income and high-education countries such as the Netherlands, men's life expectancy is catching up with women's (GBD 2016 Mortality Collaborators, 2017). Yet, even though older men are living longer than before, they still have fewer health problems than older women. Deeg et al. (Reference De Meijer, Bakx, Van Doorslaer and Koopmanschap2018) showed that from 1992 to 2016, the proportion of years spent in poor health remained lower for men than for women. Hence, it is possible that persistent health differences between men and women maintain the gender gap in the use of all types of care.
Disposition to use care
The disposition to use care reflects to what degree one intends to ask for help from others, and whether one prefers formal, informal or privately paid care. A recent scoping review by Lehnert et al. (Reference Lehnert, Heuchert, Hussain and König2019) concluded that a mix of personal and social characteristics determines the preferred care arrangement, with the wish to remain independent and to avoid becoming a burden to others prevailing. Gender, socioeconomic status, and personality factors are important drivers of care preferences. Women, those with higher education or income and with a greater sense of mastery, generally prefer formal care or privately paid care over informal care (Pinquart and Sorensen, Reference Pinquart and Sorensen2002; Rogero-García and Rosenberg, Reference Rogero-García and Rosenberg2011; Lee et al., Reference Lee, Revelli, Dickson and Marier2022). Traditionally, older men have a greater sense of mastery (Cassidy and Davies, Reference Cassidy and Davies2003) and higher levels of education (Grundy and Holt, Reference Grundy and Holt2001) than older women. Educational levels and sense of mastery have increased significantly among older adults in the past decades (Drewelies et al., Reference Drewelies, Deeg, Huisman and Gerstorf2018), particularly so among older women. If gender differences in level of education and sense of mastery have decreased, this may affect the gender gap in informal, formal and privately paid care use, and reduce the gender gap over time.
Social resources
The most important driver of the use of partner care obviously is the availability of a spouse. As older men have a spouse more often than older women, men are more likely to use partner care. The relatively greater increase in men's longevity implies that recent older cohorts are more likely to live with a partner than earlier cohorts, which means that partner care is more readily available, in particular for older women (Ryan et al., Reference Ryan, Smith, Antonucci and Jackson2012). This narrowing gender difference in partner status may contribute to a decrease in gender differences in spousal care over time.
Non-spousal informal care is generally provided by adult children. Previous studies have shown that older women receive non-spousal informal care more often than older men (Chappell et al., Reference Chappell, Dujela and Smith2014; Dorin et al., Reference Dorin, Krupa, Metzing and Büscher2016). Several socio-cultural changes may have affected the ability and willingness of adult children to provide care to their parents. In post-modern societies, gender equality in education, work and family roles is more highly valued than before, resulting in increasing numbers of women taking up employment and increasing numbers of men taking up care roles. In addition, the higher retirement age of potential caregivers (Agree and Glaser, Reference Agree, Glaser and Uhlenberg2009; Broese van Groenou and De Boer, Reference Broese van Groenou and De Boer2016) and the weakening of norms regarding family obligations (Fingerman et al., Reference Fingerman, Pilleman, Silverstein and Suitor2012; Tsutsui et al., Reference Tsutsui, Muramatsu and Higashino2013) may pose challenges to informal care provision, particularly for adult children combining work and care. There is no explicit reason to assume that adult children will reduce their help to their father more than to their mother, or the other way around. Thus, the decline in availability of informal care from someone other than a spouse may have affected older men to the same extent as older women. The use of care from adult children is therefore expected to decrease, but it is expected that the gender gap in the use of non-spousal informal care has not changed over time.
Policy changes in the supply of LTC
As in many other Western European countries, the LTC scheme in the Netherlands has undergone several reforms in the past decades (Da Roit, Reference Da Roit2012; Plaisier et al., Reference Plaisier, Verbeek-Oudjik and de Klerk2017). Originally launched as a generous universal scheme in the 1990s, the supply of residential LTC in the Dutch LTC scheme has been substantially reduced since the 2000s. A brief increase in the supply of formal home care in the early 2000s was followed by restrictions in eligibility in 2007, when responsibility for household help shifted from national to local government. A major reform in 2015 further increased the threshold to residential care, and the allocation of personal and nursing care was decentralised to general practitioners and district nurses. At the same time, these policy efforts were aimed at compensating for the increasing scarcity of formal LTC resources by making care more tailor-made, affording the recipient greater responsibility for arranging their own care according to their personal needs and so increasing the efficiency of formal care provision (De Meijer et al., Reference Deeg, Comijs, Hoogendijk, Van der Noordt and Huisman2015; Janssen et al., Reference Janssen, Jongen and Schroder-Back2016). These policy changes have led to a decrease in residential care (Alders et al., Reference Alders, Comijs and Deeg2017) and an increase in the use of home care (Plaisier et al., Reference Plaisier, Verbeek-Oudjik and de Klerk2017) over time. A more restrictive LTC scheme could change the gender gap in the use of care services. Changes in the availability of publicly provided care, particularly residential and home care services, may also impact the use of informal care or privately paid care. The use of formal and residential care is strongly linked to health and partner status, which explains why older women use formal and residential care more often than older men. Yet, the supply of publicly provided services is also an important factor here. Given that women have been more dependent on formal and residential care than men, they might be affected most by more restrictive LTC policies. Thus, it is expected that the changes in care policies reduce the gender gap in formal home care use and in residential care use.
As laid out above, we assume that differences in care use are in part attributable to differences between cohorts and between men and women in individual resources: in particular, health, education, sense of mastery, and the availability of a spouse and/or children. Moreover, substitution effects between formal, informal and privately paid care must be taken into account. Specifically, reduced formal LTC supply will place increasing pressure on informal care, and reduced availability of formal LTC as well as non-spousal care will increase the volume of care purchased privately. Our analyses will give insight into (a) the gender difference in the use of informal, formal and privately paid home care, residential care and in non-use over time; (b) the degree to which gender differences in care use are explained by individual determinants of care use (needs, disposition and enabling factors; Andersen and Newman, Reference Andersen and Newman2005) and the substitution between types of care; and (c) the difference in changes in care use over time between men and women (interaction effect of gender and year of observation). Any unexplained gender differences will shed more light on the extent to which unobserved societal changes, i.e. socio-cultural changes or LTC policy changes, may affect the gender differences in care use.
Data and methods
Our data were drawn from the Longitudinal Aging Study Amsterdam (LASA). LASA is an ongoing longitudinal study focusing on the determinants, trajectories and consequences of physical, cognitive, emotional and social functioning (Hoogendijk et al., Reference Hoogendijk, Deeg, Poppelaars, van der Horst, Broese van Groenou, Comijs, Pasman, van Schoor, Suanet, Thomése, van Tilburg, Visser and Huisman2016). The first interviews were carried out in 1992/93 among respondents aged 55–85 (N = 3,107). Measurement waves have been conducted every three to four years. The original LASA sample is based on a nationally representative sample of older adults from three geographic regions in the Netherlands (Huisman et al., Reference Huisman, Poppelaars, van der Horst, Beekman, Brug, van Tilburg and Deeg2011). In addition to the baseline cohort, new cohorts aged 55–65 were added in 2002/03 and 2012/13. In this study, we use face-to-face interview data from seven measurement waves in 1995/96, 1998/99, 2002/03, 2005/06, 2008/09, 2011/12 and 2015/16. In all measurements, interviews have been conducted with both community-dwellers and people living in residential homes. To ensure comparability across different waves, only persons aged 70–88 were included in the samples (6,527 observations/2,655 cases) as data from this age range are available in all waves.
Outcome variables
This study concentrates on six outcomes. The five care types studied were informal (personal) care provided by the partner, informal care provided by someone other than the partner, publicly provided formal home care, privately purchased home care, and residential care. Two questions were asked: ‘Do you receive help with personal care, for example, washing, bathing, dressing?’ and ‘Do you receive help with household activities, for example, cleaning, shopping, cooking?’ If answered in the affirmative, the respondent was asked who provided this type of help. For partner care, only personal care was included in this study because there were differences across waves in which household tasks were defined as help from the partner. Informal care by someone other than a partner included personal care and/or household help provided by an unpaid care-giver (son or daughter, other relative or in-law, neighbour or friend). Formal home care included personal care and/or household help provided by a professional care-giver from a home care organisation. Privately paid home care included personal care and/or household help by a privately paid helper, generally not a professional but more likely a household helper. One of the living arrangement options observed by the interviewer was residential care. In the Netherlands, residential care is care offered in a facility round-the-clock for those who are unable to live in the community and who have high care needs. The sixth outcome variable consisted of the use of neither personal care nor household help at home or in residential care and was therefore titled non-use of care.
Explanatory variables
In line with the Andersen and Newman model, we distinguish the time variable and three domains of explanatory variables indicating to individual determinants of care use (Figure 1). The time variable, i.e. the year of observation in seven measurement years, refers to the historical time period and the specific LTC policy of that time. To indicate need, three indicators of health were included: cognitive functioning as measured by the Mini-Mental State Examination (MMSE) score, which ranges from 0 to 30 (Folstein et al., Reference Folstein, Folstein and McHugh1975); number of functional limitations as measured by six activities: difficulty using stairs, using own or public transport, cutting toenails, dressing and undressing, sitting down and standing up from a chair, and walking outside for five minutes without stopping (range 0–6, the highest score referring to difficulty with all six activities); and number of chronic conditions out of seven major conditions: (a) chronic lung disease, (b) cardiac disease, (c) peripheral arterial disease, (d) diabetes, (e) cerebrovascular accident, (f) osteoarthritis or rheumatoid arthritis and (g) cancer. Disposition variables included education and sense of mastery. Educational level ranged from low (elementary school only) through medium (secondary education) to high (college, university or higher). Sense of mastery, i.e. the feeling that one has control over events and ongoing situations, was measured by a five-item scale, with the sum score ranging from 5 to 25, a higher score indicating a greater sense of mastery (Pearlin and Schooler, Reference Pearlin and Schooler1978). Enabling variables included social resources, i.e. living with a partner (0, 1), having a partner outside the household (0, 1) and number of living children. Age (in years) was used as a control variable in all analyses.
Statistical analysis
All six outcome variables were dichotomous. Gender compares males (0) with females (1). Year of observation was used as the explanatory variable that refers to the historical time period (Swinkels et al., Reference Swinkels, Suanet, Deeg and Broese van Groenou2016). It was included as a categorical variable in order to be able to detect non-linear trends. Descriptive statistics were provided for all variables under study for men and women separately in all years of observation (Table 1). The possible multicollinearity was tested between the explanatory variables with the variance inflation factor values and coldiag2 (Stata 16), and with correlation coefficients, when applicable. Multicollinearity was not observed. For multivariate statistical analysis, we applied generalised estimating equations logistic regression using IBM Statistics 25 and Stata/S.E. 14.2. This method accounts for the interdependence of observations of individuals who participated in multiple waves. An exchangeable correlation matrix was used. In all analyses, age is included to account for possible differences in the age distribution between years of observation.
Table 1. Descriptive statistics for all variables under study by gender and by year of observation
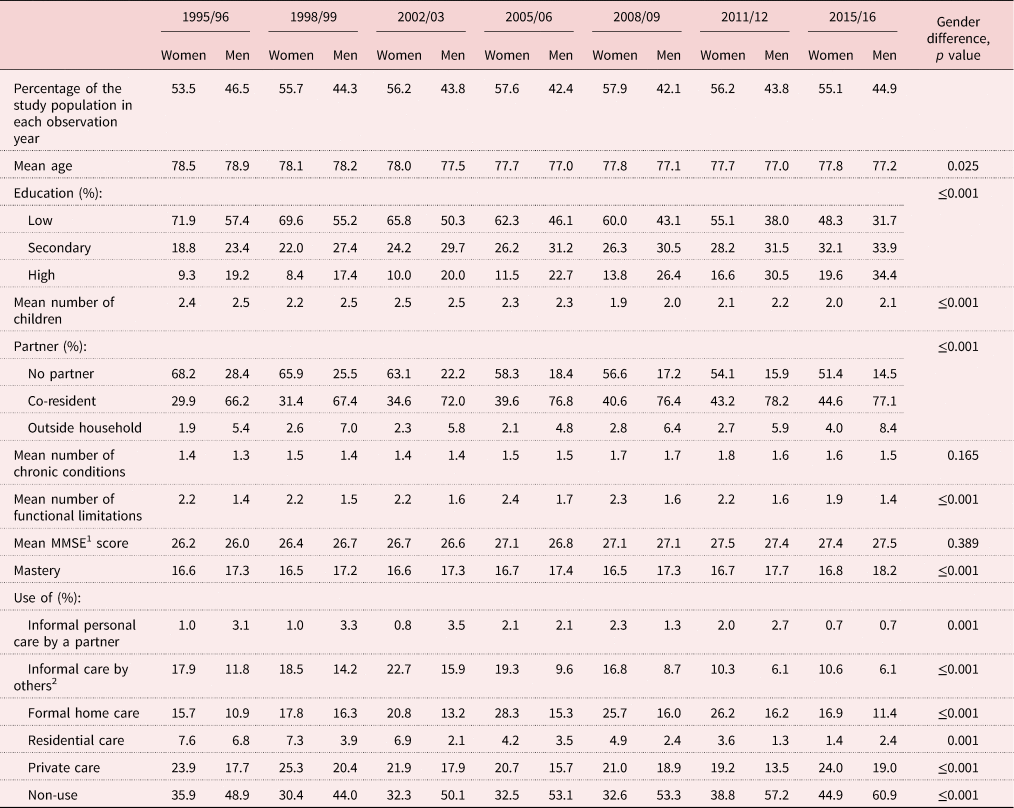
Notes: Frequencies are adjusted for age using estimated margin means from multinomial regression analysis or estimated margin means from analysis of variance. 1. MMSE: Mini-Mental State Examination. 2. Children, other relatives, neighbours or friends.
For each care type, analyses were run in six or seven steps. First, age, gender and year of observation were included in Model 1 to examine the effect of gender on care use. Next, possible explanatory variables were added to the models separately: the need variables (Model 2), the disposition variables (Model 3), the enabling variables (Model 4) and the use of other types of home care (Model 5). Model 5 was run only for the four types of home care, excluding residential care and non-use. The full models (Model 6) included all the explanatory variables. The interaction models included the interaction effect of gender × year of observation. Based on the interaction models, predictive margins were calculated to demonstrate the interaction between the observation year and gender in graphs (StataCorp, nd); this statistic reports predictions at average values of the covariates.
Results
Gender differences in health and social resources
Table 1 shows the age-adjusted gender differences in each year of observation for all variables under study. Women were slightly older and lower educated than men. Mean age decreased slightly over the study period, from 78.5 to 77.8 for women and from 78.9 to 77.2 for men. Women had a higher mean number of chronic conditions and functional limitations. Average MMSE did not differ between the genders. Sense of mastery was higher in men. Men proved to have better social resources, as they had more children on average and more often co-resided with a partner than women.
Change in health and social resources and care use over time
Table 1 shows descriptive statistics (age-adjusted) for increasing trends in educational level and living with a partner and a decreasing trend in the number of children for both men and women. The number of functional limitations and chronic conditions first increased and then decreased for both men and women. Cognitive functioning and sense of mastery increased for both men and women. The statistical analyses (Table 2; Models 1 and full models) show that when the individual factors are taken into account, the odds of using formal home care increased while the odds of using residential care decreased over time. Also, the use of privately paid home care was lower in some of the study years compared to the reference year (1995/96). The odds of not using any care increased in the later study years. The odds of using informal care by someone other than a spouse fluctuated over time, while there are no statistically significant changes in the use of informal care by a spouse.
Table 2. Gender differences in use of different care types in 1995–2016. Figures marked in bold indicate a statistically significant difference.

Notes: Generalised estimating equations for logistic regression. Models 1: age, gender, year of observation. Full models: adjusted for education, partner status, children, Mini-Mental State Examination (MMSE) score, mastery, number of chronic conditions and functional limitations, use of formal home care, private home care or informal care provided by partner/other than partner. 1. Almost everyone who received personal care from their partner lived with their partner. To improve the fit of the model, when studying personal care by a partner, living with a partner is used as the reference group. OR: odds ratio. CI: confidence interval. Ref.: reference category. NA: not applicable.
Gender differences in care use
Personal care provided by a partner
In almost all years, more men than women received personal care from their partner (Table 1). The gender difference was statistically significant when age and year of observation were taken into account (Table 2; Figure 2, Model 1). The addition of health information (Figure 2, Model 2), education and mastery (Figure 2, Model 3) and use of other types of care (Figure 2, Model 5) to the models somewhat diminished but did not remove the statistically significant difference between men and women. However, the inclusion of social resources (information on partner status and children) rendered the association of gender non-significant, with the odds ratio nearing 1.0 (Figure 2, Model 4), implying that differences in social resources explain the gender difference. The interaction term was significant for 2008/09 (Table 3, Model 1). Adding need, disposition and enabling factors to the full models (Table 3; Figure 3a) rendered the interaction effect non-significant for 2008/09, but in 2005/06 (compared to reference year) the increase in informal care by a partner was larger for women than for men. The mostly non-significant interaction effects imply that the change in partner care over the years was rather similar for men and women.
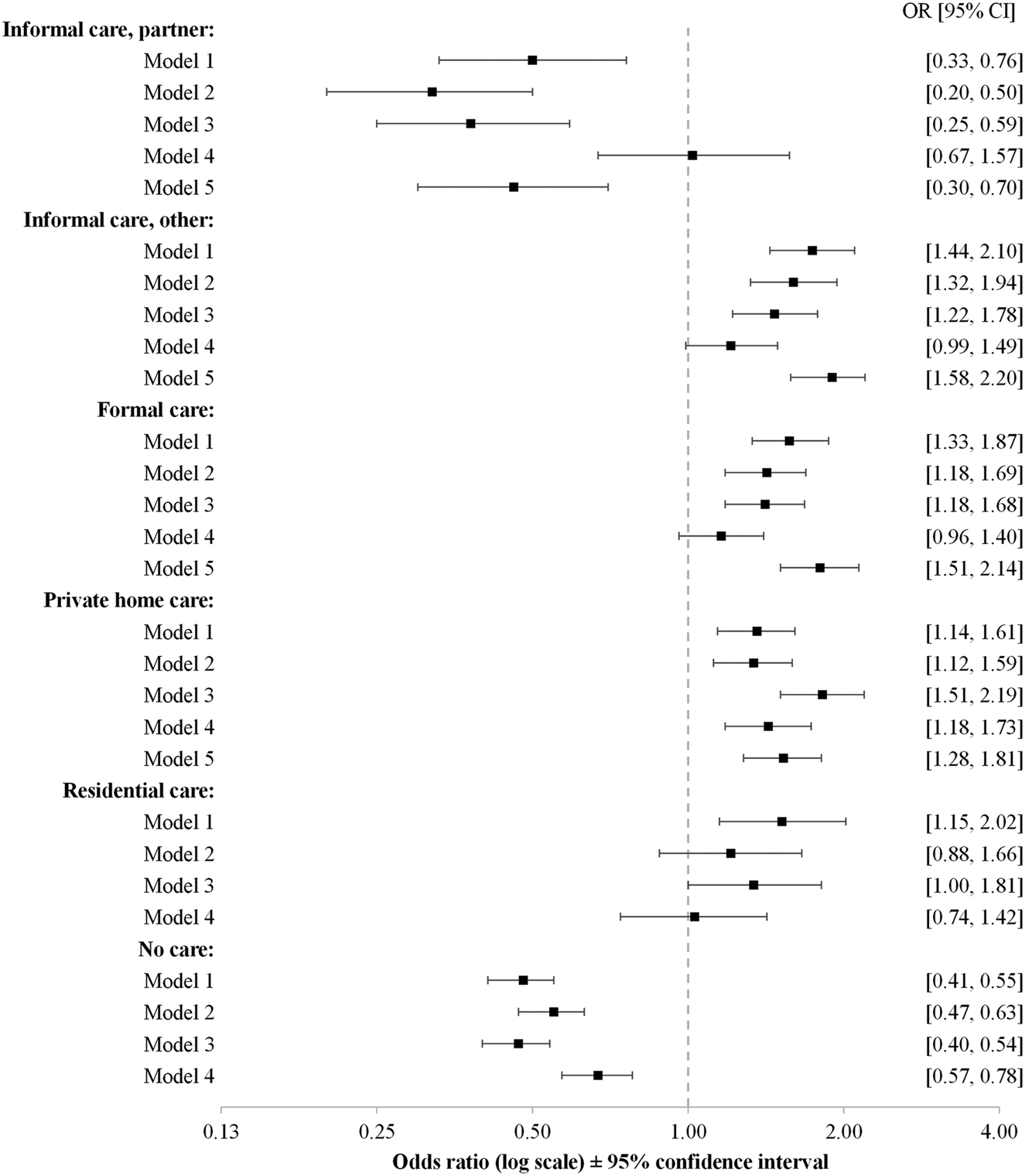
Figure 2. The odds for women to use different types of care when different explanatory factors are included in the models.
Notes: Model 1: sex, age, the year of observation. Model 2: Model 1 plus the health variables including the number of chronic conditions, the number of functional limitations and Mini-Mental State Examination score. Model 3: Model 1 plus education and mastery. Model 4: Model 1 plus social resources including information on living with a partner and the number of children. Model 5: the use of other types of home care. Model 5 applies only in different types of home care use, excluding residential care and non-users. Odds ratios and 95 per cent confidence intervals for generalised estimating equations for logistic regression.
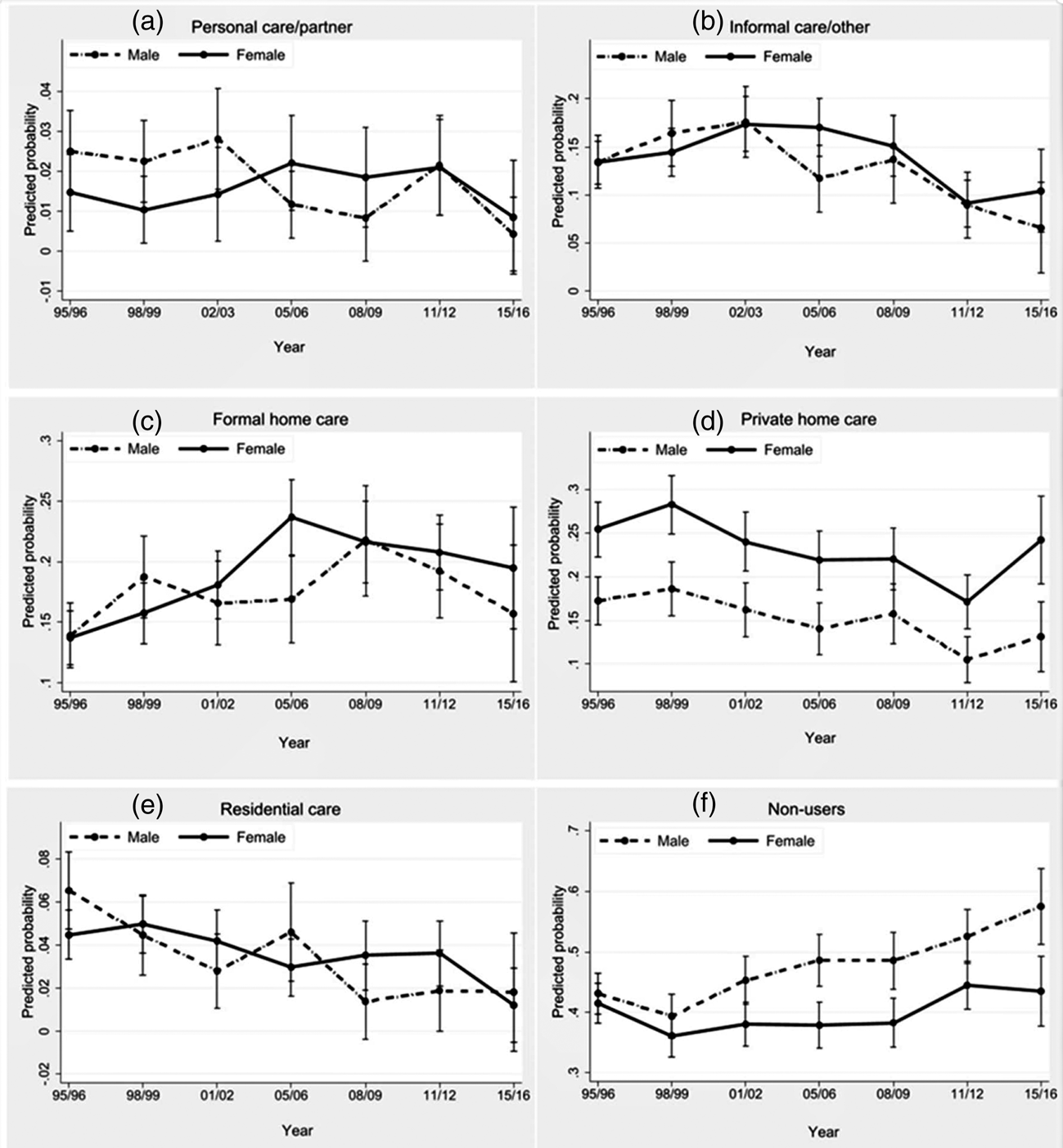
Figure 3. The gender gap in care use from 1995/96 to 2015/16.
Notes: Predictive margins of interaction term sex × year. Logistic regression analyses. Analyses are adjusted for the explanatory variables. The gender differences at each year of observation in the graphs are not fully comparable to the gender × year of observation effects in the logistic regressions (Table 3). The interaction term compares the difference between men and women in a given year with the reference year. Thus, the gender gap may narrow, remain the same or increase in relation to the reference year. The graphs illustrate the gender-specific change in care use and the 95 per cent confidence intervals for women and men separately at each time-point.
Table 3. Changes in gender differences in the use of different care types in 1995–2016. Figures marked in bold indicate a statistically significant difference.
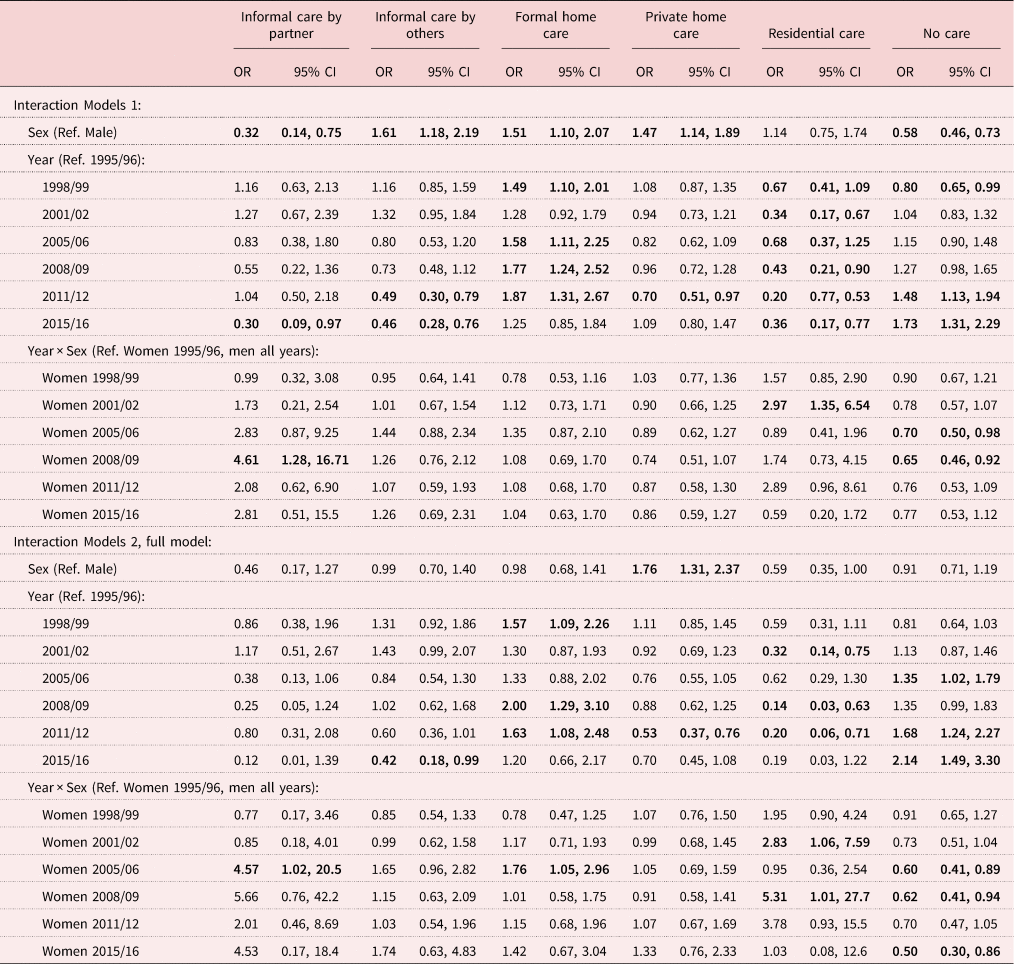
Notes: Generalised estimating equations for logistic regression with interaction term sex × year of observation. Model 1 includes age, sex, year of observation. Model 2 is adjusted for education, partner status, children, Mini-Mental State Examination score, mastery, number of chronic conditions and functional limitations, use of formal home care, private home care or informal care provided by partner/other than partner. OR: odds ratio. CI: confidence interval. Ref.: reference category.
Informal care provided by someone other than a partner
Women received informal care from someone other than their partner more often than men (Table 2). The statistically significant difference became non-significant only when social resources were added to Model 4 (Figure 2). The interaction term is not significant (Table 3), which implies that the changes in care use are similar for both sexes. Figure 3b shows the similar, mainly decreasing trends of informal care provided by someone other than a partner in both men and women.
Formal home care
Women's odds of using formal home care were higher than men's (Table 2; Figure 2). However, the addition of social resources (Figure 2, Model 4) again rendered the gender effect non-significant. Other explanatory variables did not remove the statistically significant gender difference. Table 3 shows a non-significant interaction effect, except in 2005/06 (compared to 1995/96) when the increase in formal home care use was larger for women than for men. However, the mostly non-significant interaction effects imply that the change in care use over the years was rather similar for men and women. For both, the use of formal care was higher in the later than in the earlier years when health, education, mastery and social resources were taken into account (Figure 3c).
Privately paid care
Privately purchased home care use was higher among women than men and adding the explanatory variables to the model did not remove the statistically significant gender difference (Table 2; Figure 2). The interaction effects were not significant (Table 3), suggesting a rather consistent gender gap over time. Adjusted for the individual determinants, Figure 3d shows both the large gender differences for each year of observation and the mainly decreasing trend in privately paid home care use in both genders when all individual factors are included in the model.
Residential care
Women had higher odds of residential care use than men (Table 2; Figure 2). Adding the explanatory variables to Models 2–4 shows that both the health variables (Figure 2, Model 2) and social resources (Figure 2, Model 4) explained the gender difference in residential care use. The gender effect changed in the earlier years as the gender gap was greater in 2001/02 and 2008/09 (compared to 1995/96) in favour of women (Table 3). The use of residential care declined over time, but less so for women. Figure 3e shows that women's residential care use in 2001/02 and 2008/09 decreased less than men's when all individual factors are taken into account, resulting in a greater gender difference in those years.
Non-use
Men had higher odds of the non-use of care than women (Table 2; Figure 2), and taking account of health, education, mastery and social resources did not remove the gender difference (Figure 2, Models 2–4). As the increase in non-use of care was less steep for women than men, the gender difference in non-use increased over time (Table 3). The increase in the gender difference over the study period is illustrated in Figure 3f.
Discussion
In this study, we examined gender differences in the use of several sources of care and how these differences may have changed over time. Three conclusions are derived. First, a gender gap was found in the use of all sources of care as men used more personal care provided by the partner, and women used more of all other sources of care. Second, social resources had a substantial association with gender differences in care use. Differences in social resources between men and women explained the gender gap in informal care and formal home care use, and together with health factors, the gender difference in residential care use. On the other hand, individual factors did not explain the gender gap in the use of private home care and non-use of care. Third, the inclusion of explanatory factors revealed several changes in the gender gap over time. Women were more likely than men to use informal care by a partner in 2005/06 versus 1998/99, formal home care in 2005/06 versus 1998/99, and residential care in 2001/02 and 2008/09 versus 1998/99, while non-use increased especially in men (in 2005/06, 2008/09, 2015/16 versus 1998/99). In both genders, overall trends in care use showed an increase in the use of formal home care and a decrease in the use of other care types. Although health and dispositional factors (education and mastery) explained only little of the gender differences in care use, their contribution was not insubstantial regarding informal and formal care use, and they helped gain a better understanding of the gender gap in these types of care.
Our result that gender differences in partner care, other informal care and formal home care were largely due to gender differences in social resources support earlier findings. The importance of partner help is also illustrated by how changes in family structure are linked to the use of LTC: continuously married adults had a similar risk of LTC use to remarried and partnered adults, and lower risk than widowed, divorced/separated and never married adults (Thomeer et al., Reference Thomeer, Mudrazija and Angel2018). In Germany, women often receive help from several informal sources and formal care services, while men rely mainly on their wives for help (Dorin et al., Reference Dorin, Krupa, Metzing and Büscher2016). This is also reflected in the study by Schmidt (Reference Schmidt2017), who found prevailing gender roles in caregiving and care use in Austria. Our data confirmed our assumption that in recent study years women had a co-habitant partner more often than in earlier years, yet the gender difference in having a co-habitant partner remained in favour of men. This result suggests that gender differences in partner care were largely due to the lack of a co-habiting partner among women. The share of those having a partner outside the household increased slightly during the study years. When in poor health, those with a partner living apart are less likely to receive daily care from their partner than co-habiting partners (Broese van Groenou et al., Reference Broese van Groenou, Te Riele and de Jong Gierveld2019). This implies that partners living apart may not be as available for late-life care as partners in co-habiting relationships. However, as the increase in partners living apart was only around six percentage points, its possible effect on our results is minor. Furthermore, adult children are major providers of informal care. In the case of remarriage and stepchildren, stepchildren are less likely to provide care to stepparents in later life (Coleman et al., Reference Coleman, Ganong, Hans, Sharp and Rothrauff2005). The link between changing family structures and the use of informal care is one possible explanatory factor for the decline in informal care use, but unfortunately our data do not allow more detailed research on the subject.
Over the two decades under study, the Netherlands moved towards more restrictive LTC policies. Our findings show an increased use of formal home care and lower use of residential care over time, corresponding with the stricter eligibility criteria, especially after 2005 (De Meijer et al., Reference Deeg, Comijs, Hoogendijk, Van der Noordt and Huisman2015). These changes were not explained by the various individual factors taken into account in our analysis, which supports the attribution of these changes to factors beyond individual characteristics. In fact, our findings of a decrease in residential care use and an increase in formal home care use in both men and women reflect the ‘ageing-in-place’ policy. We expected that the well-known gender gap whereby women use formal care services more often than men (Bird et al., Reference Bird, Shugarman and Lynn2002; Algera et al., Reference Algera, Francke, Kerkstra and Van Der Zee2004) would be reduced as the restrictions should have affected women – the more frequent formal care users – to a greater extent than men. This appeared not to be the case. In fact, the gender gap increased in some, albeit not in all years of observation, after individual health, dispositional factors and social resources were taken into account. This suggests that, although the allocation of formal and residential care is largely based on care needs and the presence of a partner and/or children, there was also a gender bias in the allocation of formal home care and residential care in some but clearly not all years of observation.
Given that formal home care allocation became less generous over the years, one would have expected to see an increase in the use of alternative sources of care, such as informal care and privately paid care. However, it seems that the opposite has been the case as the use of these sources of care declined over time, contributing to the decrease in care use in both genders. Moreover, non-use increased significantly, even when health and social resources were taken into account. Thus, this increase was not driven by possible improvements in health and social resources. This suggests that a more restrictive LTC policy left older people without care even when they had health conditions that would have contributed to care use in earlier years. There is, for example, evidence that over time, the decline in admissions to LTC institutions is not only the result of changes in need (De Meijer et al., Reference Deeg, Comijs, Hoogendijk, Van der Noordt and Huisman2015; Alders et al., Reference Alders, Comijs and Deeg2017), but also of changes in needs-based LTC eligibility criteria. In all, changes in LTC policies are complex and very difficult to grasp into empirical variables. It would be essential to study further to what extent and how the eligibility criteria for access to public formal home care and the related guidelines explain variations in care use over time.
Our findings show that the availability of both a co-resident partner and informal care by someone other than the partner was associated with a lower level of formal care use. This substitution effect suggests that restricting LTC will increase informal care use, but the matter is more complicated: both individual characteristics and family structures, and cultural norms, steer the need for and the use of informal care (Haberkern and Szydlik, Reference Haberkern and Szydlik2010). In countries with a weaker public care service system, people may feel obligated to care for their family members (Cooney and Dykstra, Reference Cooney and Dykstra2011; Verbeek-Oudijk et al., Reference Verbeek-Oudijk, Woittiez, Eggink and Putman2014). Instead, countries with strong national health-care infrastructures are less likely to prefer family-based care (Mair et al., Reference Mair, Quiñones and Pasha2016). In traditional gender roles, women are expected to adopt the role of a caregiver (Sharma et al., Reference Sharma, Chakrabarti and Grover2016), which may make informal care an option considered as a priority. According to Cooney and Dykstra (Reference Cooney and Dykstra2011), also the logistics matter: the shorter living distance between family members may contribute to higher use of informal help. Some people experience receiving help from family or friends instead of formal carers as an expression of independence (Hillcoat-Nallétamby, Reference Hillcoat-Nallétamby2014). It is possible that when care and caring remain ‘in the family’, people feel more independent, and the care is more manageable when compared to formal care service providers, who follow their own work schedule and priorities. Moreover, preference towards informal care is also dependent on the care receiver's level of disability (Mair et al., Reference Mair, Quiñones and Pasha2016); informal care substitutes for formal home care, but the substitution effect disappears as the level of disability of the older person increases (Bonsang, Reference Bonsang2009).
While we started out from the assumption that older women are more affected by societal changes, including LTC policies, than older men, it appears that older men may be affected more than older women by a decrease in the supply of informal and formal care, as the use of care decreased more slowly for women. In men, the increased frequency of non-use may be attributed to cutbacks in formal LTC coupled with a decline in the availability of non-spousal informal care. Women may be more active and persistent in care-seeking (Thompson et al., Reference Thompson, Anisimowicz, Miedema, Hogg, Wodchis and Aubrey-Bassler2016). We observed that women were more likely to use privately paid care than men, and this gender gap remained stable throughout the study years. Hence, it seems that women were more able – or willing – to purchase care from private home care providers. The growing gender gap in not using any care raises concerns especially regarding the possible increase in unmet care needs of older men. Many chronic diseases have become much more manageable over time, and especially men who have survived these previously fatal diseases may have an increased need for care. Research on older men's and women's care trajectories, particularly after widowhood, may help to shed light on whether and why older men use less care than older women.
This study was subject to some limitations. First, the data included only those persons who were able to participate in interviews, which means those in the poorest health were excluded. However, this allowed us to consider important factors contributing to care use such as cognitive functioning (MMSE) and sense of mastery – measures that cannot be provided by proxies. Second, we were able to detect gender differences in care use and changes in care use over time but had only limited possibilities to investigate the underlying causes. In particular, changes in the supply of informal and formal care were unobserved measures in our study and were only reflected in the year of observation variable. The inclusion of more direct measures (e.g. number of LTC beds per year) has proved useful in cross-national comparisons (Suanet et al., Reference Suanet, Broese van Groenou and van Tilburg2012; Wagner and Brandt, Reference Wagner and Brandt2018), but they have limited empirical value in within-country studies due to the lack of variation (e.g. Rostgaard and Szebehely, Reference Rostgaard and Szebehely2012). Third, our focus in this study was on people aged 70–88. Over the years, it is possible that the amount of time lived with severe health problems has increasingly shifted towards the older population, even older than 88 (Deeg et al., Reference De Meijer, Bakx, Van Doorslaer and Koopmanschap2018). The majority of those who live to old age experience a period of chronic illness and an increased need for care, especially when the end of life is approaching (e.g. Forma et al., Reference Forma, Rissanen, Aaltonen, Raitanen and Jylhä2009; Pot et al., Reference Pot, Portrait, Visser, Puts, Broese van Groenou and Deeg2009). As age at death is continuing to rise, older ages are of ever-greater interest as far as studying care use is concerned. It may, therefore, be considered a limitation that we did not include people older than 88 in our study. Fourth, as our sample excludes the most disadvantaged individuals such as those with severe dementia, who make up a significant proportion of residential care users, the share of residential care users in this study is an underestimation. However, we felt that the inclusion of residential care is important to see how the gender gap changes over time when a comprehensive definition of care is used. Fifth, a specific concern for studies on ageing is the high rate of attrition. However, we do not consider attrition a major problem for the reliability of our findings. In LASA, attrition can for the largest part be attributed to mortality and, to a much lesser extent, to refusal or other reasons; attrition due to mortality does not affect sample representativeness because high mortality is characteristic of all older populations. To avoid the negative effects of attrition on sample size, men and the oldest participants were oversampled in LASA (Huisman et al., Reference Huisman, Poppelaars, van der Horst, Beekman, Brug, van Tilburg and Deeg2011). Sixth, this study focuses on the changes in the gender gap in care use in the Netherlands. However, as shown in the theoretical part of this study, studies from different countries show similar gender differences in care use. In addition, the changes in care policies are roughly similar – ageing-in-place and informal care are emphasised in public debate and policy recommendations in many Western countries. The study design we used could be extended to other countries to see if the changes and the explanations for the possible changes are similar.
Conclusions
The use of care in general showed a tendency to decline in both genders from 1995 to 2016, resulting in an increased share of persons who did not use any care. Although health, dispositional factors and especially social resources explained most of the gender differences in care use, they did not explain the difference in private care or in non-use of care. This study increases our insight into how individual- and societal-level developments intertwine. Given the persistent and even increasing gender differences in care use, it is important to explore further the role of gender in seeking care and access to care, and to examine the role of specific LTC policies from a gender perspective.
Acknowledgements
This work is part of research conducted at the Center of Excellence in Research on Ageing and Care (CoEAgeCare), funded by the Academy of Finland (326567).
Author contributions
MA and MBvG conceptualised the study. MA conducted the analyses and wrote the first draft of the manuscript. MA, MBvG and DD interpreted the data. MBvG and DD provided critical feedback on the manuscript. MA was the main author responsible for writing the manuscript. All authors approved the final manuscript.
Financial support
This work was supported by the Academy of Finland (MA, grant number 318985). The Longitudinal Aging Study Amsterdam is supported by a grant from the Netherlands Ministry of Health Welfare and Sports, Directorate of Long-Term Care.
Conflict of interest
The authors declare no conflicts of interest.
Ethical standards
The Longitudinal Aging Study Amsterdam (LASA) has received approval by the Medical Ethics Committee of the VU University Medical Center. Appropriate informed consent was obtained from all study participants. For the present study, the permission to use data was obtained from the LASA steering group using the official analysis proposal form (http://www.lasa-vu.nl/data/availability_data/availability_data.htm).










