A 50-year-old man with a history of smoking and unspecified drug use suffered an acute ischemic stroke and was transferred to our stroke center for mechanical thrombectomy (MT). He had awoken with a complete right hemispheric syndrome and a right middle cerebral artery (MCA) occlusion of the M1 segment on CT angiogram (CTA) (Figure 1a). He did not receive thrombolysis at the referring center because of the unknown time of onset, although his ASPECTS was favorable (9) on baseline CT. He underwent MT with TICI 2a (Thrombolysis in cerebral infarction) recanalization after one pass with a stent retriever (Figure 1b).
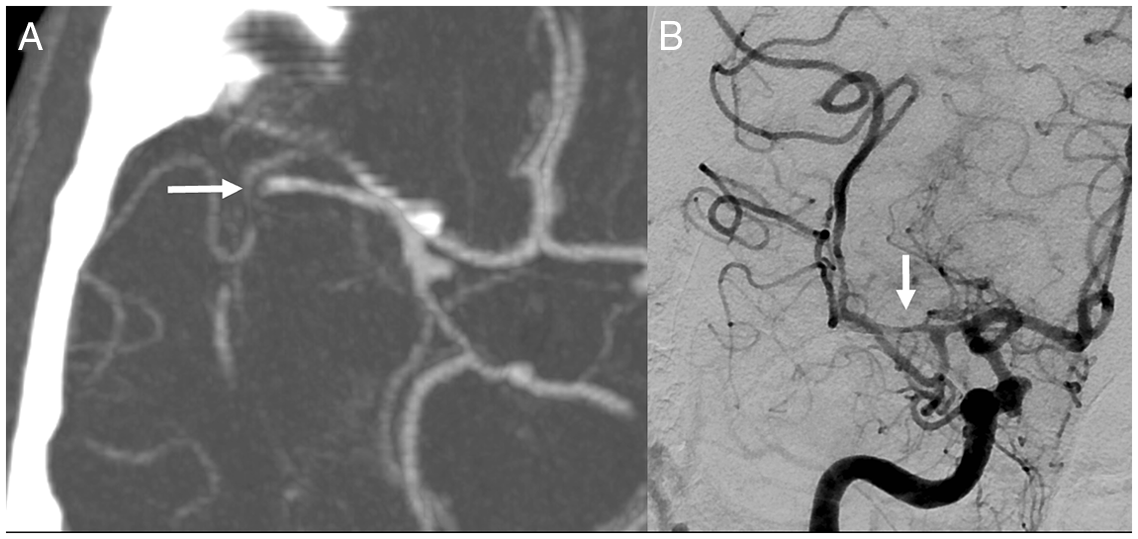
Figure 1: Right middle cerebral artery occlusion and reperfusion.
On Day 1, there was little improvement in his neurological deficit. His CT scan revealed an expected evolution of the right MCA infarct in addition to a left MCA territory subacute infarct, retrospectively visible on the baseline CT (not shown). Aspirin was started. He developed fever the same day, and his blood cultures were positive for gram-positive cocci bacteria, later identified as Streptococcus viridans and Streptococcus oralis. A rapid transthoracic echocardiogram showed a mitral valve vegetation, and intravenous antibiotics were started. When further questioned, he confirmed that he had undergone dental extraction 3 months prior. His urinary toxicology screen was positive for amphetamines and opiates.
A CTA performed on Day 4 revealed a right MCA mycotic aneurysm at the site of the original occlusion (Figure 2a). Additional right MCA cortical branch aneurysms were also identified, one of which was associated with a new temporal intraparenchymal hematoma (Figure 2b).
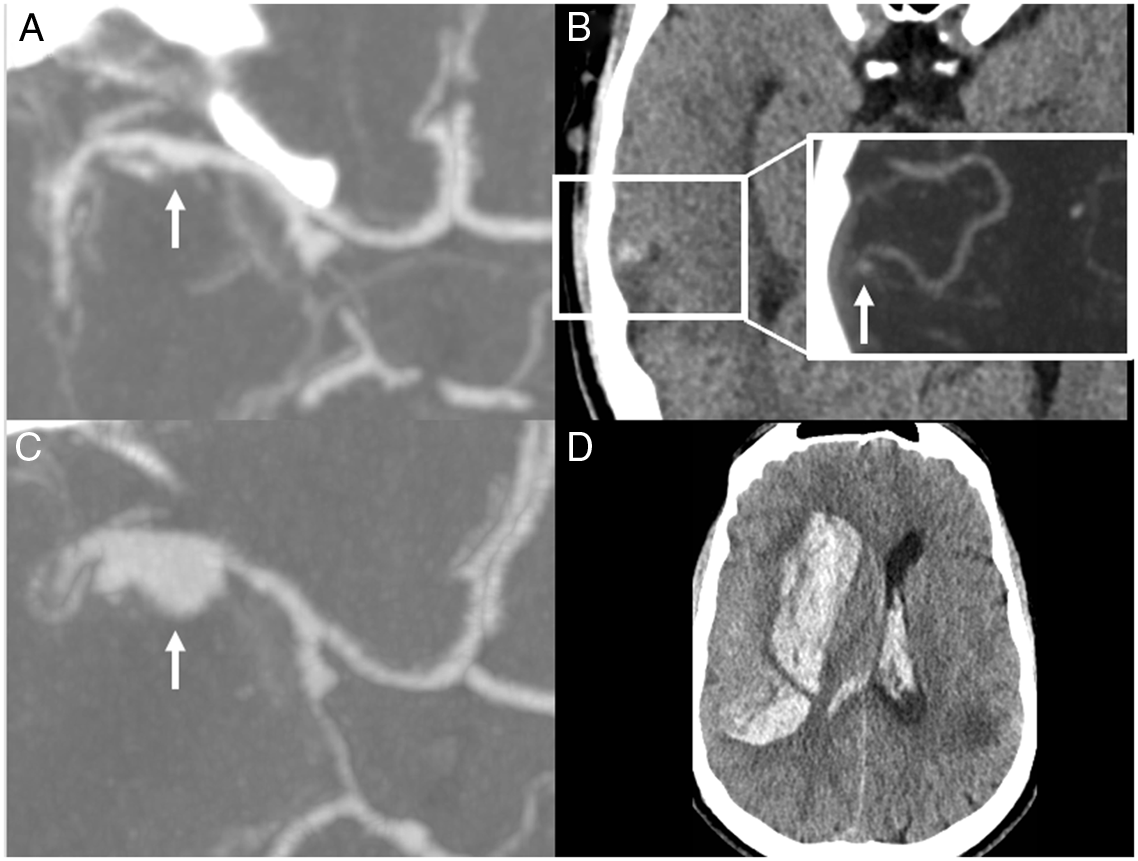
Figure 2: Progression of aneurysm in the right middle cerebral artery, leading to rupture and catastrophic bleeding.
On Day 9, another follow-up CTA showed that the right MCA aneurysm had more than doubled in size (Figure 2c). He also developed a new left MCA aneurysm (6 × 5 mm), and the distal right MCA aneurysm had progressed to 2 mm (not shown). On the same day, he developed a thunderclap headache and sudden coma. Urgent CT showed a large right subinsular intraparenchymal hemorrhage with mass effect and intra-ventricular extension (Figure 2d), most likely secondary to rupture of the right MCA aneurysm. After discussion with his family, conservative management was preferred and the patient was listed as a potential organ donor after confirmation of neurological death.
While it is recommended that thrombolysis be avoided in patients with infectious endocarditis and acute stroke given the high risk of hemorrhagic transformation, Reference Asaithambi, Adil and Qureshi1 the safety of thrombectomy remains less clear. Many case reports suggest successful outcomes, Reference Sloane, Raymond, Rabinov and Singhal2,Reference D’Anna3 but the risk of hemorrhagic complications remains high, Reference Maheshwari, Wardman, Cordato and Bhaskar4 as shown in our patient, in whom the potentially rapid and catastrophic evolution of intracranial mycotic aneurysms is also illustrated. Endothelial injury caused by stent retriever deployment has been described in MRI studies, Reference Kasab, Bathla and Varon5 and we hypothesize that such injury may have favored local bacterial seeding and mycotic aneurysm formation at the site of thrombectomy in our patient. While suspected or confirmed bacterial endocarditis is not an absolute contra-indication to MT, specific risks, including further septic embolization, intraprocedural arterial rupture, and mycotic aneurysm formation, must be key considerations when offering endovascular stroke treatment to this patient population.
Acknowledgements
The Open Access fees of this article were funded through an agreement between Université de Montréal and Cambridge University Press.
Author Contributions
CR performed the literature review and drafted the manuscript.
LCG proposed the case report topic and provided critical review of the manuscript.
LLG reviewed, selected, formatted and described the imaging, and provided critical review of the manuscript.
CO provided critical review of the manuscript.
AYP supervised the project, provided critical review of the manuscript, and helped draft it.
Conflicts of Interest
The authors do not have conflicts of interest to disclose.






