Article contents
Ultracellular Imaging of Bronchoalveolar Lavage from Young COVID-19 Patients with Comorbidities Showed Greater SARS-COV-2 Infection but Lesser Ultrastructural Damage Than the Older Patients
Published online by Cambridge University Press: 06 September 2022
Abstract
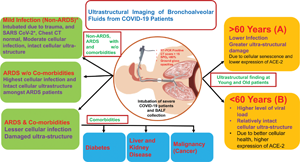
In this study, we examined the cellular infectivity and ultrastructural changes due to severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection in the various cells of bronchoalveolar fluid (BALF) from intubated patients of different age groups (≥60 years and <60 years) and with common comorbidities such as diabetes, liver and kidney diseases, and malignancies. BALF of 79 patients (38 cases >60 and 41 cases <60 years) were studied by light microscopy, immunofluorescence, scanning, and transmission electron microscopy to evaluate the ultrastructural changes in the ciliated epithelium, type II pneumocytes, macrophages, neutrophils, eosinophils, lymphocytes, and anucleated granulocytes. This study demonstrated relatively a greater infection and better preservation of subcellular structures in these cells from BALF of younger patients (<60 years compared with the older patients (≥60 years). The different cells of BALF from the patients without comorbidities showed higher viral load compared with the patients with comorbidities. Diabetic patients showed maximum ultrastructural damage in BALF cells in the comorbid group. This study highlights the comparative effect of SARS-CoV-2 infection on the different airway and inflammatory cells of BALF at the subcellular levels among older and younger patients and in patients with comorbid conditions.
- Type
- Biological Applications
- Information
- Copyright
- Copyright © The Author(s), 2022. Published by Cambridge University Press on behalf of the Microscopy Society of America
References
- 2
- Cited by





