Introduction
People with severe mental illness (SMI) have poorer physical health (Launders, Hayes, Price, & Osborn, Reference Launders, Hayes, Price and Osborn2022), a higher rate of non-mental health hospitalisations (Germack, Caron, Solomon, & Hanrahan, Reference Germack, Caron, Solomon and Hanrahan2018; Jansen, van Schijndel, van Waarde, & van Busschbach, Reference Jansen, van Schijndel, van Waarde and van Busschbach2018), and a higher risk of mortality than the general population (Hayes, Marston, Walters, King, & Osborn, Reference Hayes, Marston, Walters, King and Osborn2017; Walker, McGee, & Druss, Reference Walker, McGee and Druss2015). A recent meta-analysis found elevated rates of non-mental health admissions in people with SMI, even when controlling for underlying physical health (Ronaldson et al., Reference Ronaldson, Elton, Jayakumar, Jieman, Halvorsrud and Bhui2020), suggesting that increased prevalence of physical health conditions is not the only driver of elevated non-mental health admissions in those with SMI.
Barriers to timely preventative care and to services aimed at the management of chronic disease, may lead to increased emergency admissions. Barriers to appropriate physical health care for those with SMI include healthcare-related factors such as diagnostic overshadowing resulting in delayed diagnosis of physical health conditions, and fragmented healthcare systems hampering a patient's ability to access appropriate and timely care, as well as patient-level factors such as cognitive impairment, reduced motivation or social isolation reducing healthcare access. There is also evidence that patients with SMI are at increased risk of 30-day readmissions for physical health conditions (Germack et al., Reference Germack, Caron, Solomon and Hanrahan2018; Jansen et al., Reference Jansen, van Schijndel, van Waarde and van Busschbach2018), suggesting treatment failure and suboptimal follow-up care and management may be responsible for some of the increased emergency hospital use in this population. Understanding the use of planned and emergency hospitalisation is therefore important to implement appropriate actions, aimed at providing accessible physical health services, reducing emergency admissions with the aim of reducing premature mortality in people living with SMI.
A subset of emergency admissions is thought to be avoidable if appropriate disease management services are in place (Purdy, Griffin, Salisbury, & Sharp, Reference Purdy, Griffin, Salisbury and Sharp2009). In the general population, analyses of these admissions have been used to identify subsets of patients for whom interventions in primary care may impact their emergency hospital use (Orlowski et al., Reference Orlowski, Snow, Humphreys, Smith, Jones, Ashton and Bottle2021). In the context of people with SMI, previous studies have found elevated rates of avoidable admissions (Davydow et al., Reference Davydow, Ribe, Pedersen, Fenger-Grøn, Cerimele, Vedsted and Vestergaard2016; Lin, Huang, Chen, & Chen, Reference Lin, Huang, Chen and Chen2011), but few if any have put this in the context of emergency admissions for other causes.
While there is evidence that non-mental health admissions are elevated in those with SMI, there is a need to investigate the contribution of physical health admissions separately from accident and injury admissions, and avoidable admissions in comparison to emergency admissions for other causes. Furthermore, there is a paucity of evidence on the impact of having SMI on planned v. emergency physical health admissions. The objective of this cohort study was to determine the rate of emergency and planned physical health hospitalisations in those with SMI, compared to matched comparators, and to investigate how these rates differ by SMI diagnosis.
Methods
Population
We identified a cohort of patients with SMI, and a comparator cohort without SMI, who were registered with a primary care practice in England from the Clinical Practice Research Datalink (CPRD) Aurum and Gold databases (Herrett et al., Reference Herrett, Gallagher, Bhaskaran, Forbes, Mathur, van Staa and Smeeth2015; Wolf et al., Reference Wolf, Dedman, Campbell, Booth, Lunn, Chapman and Myles2019). At the time of this study, these databases held deidentified primary care medical records for over 39 million patients in the UK. We defined patients with a diagnosis of SMI using medical codes for schizophrenia, bipolar disorder, or other non-affective psychotic illnesses (online Supplementary Table S1). Patients with SMI were matched to individuals who had never had a diagnosis of SMI on sex, five-year age band, primary care practice and year of primary care practice registration to comparators. Exact matching was performed by CPRD prior to receipt of the dataset and comparators were matched at least 1:1 and up to 1:4 based on the availability of comparators. Hospitalisation data were available from 1 April 2000 to 31 March 2017, we therefore included patients with a first diagnosis of SMI between 1 April 2000 and 31 March 2016 to allow for at least one year's follow up. The index date was the date of diagnosis, or for comparators, the date that their matched patient with SMI was diagnosed. We excluded patients under the age of 18 or over 100 with less than one year of active follow up at index. Ethical approval for this study was obtained from the Independent Scientific Advisory Committee of CPRD (protocol no. 18_288).
Data linkage
We linked data from CPRD to Hospital Episode Statistics (HES) Admitted Patient Care (APC) data for hospital activity HES APC contains details of admissions to hospitals in England where care is paid for by the National Health Service (NHS). The main purpose of HES is to inform service provision and to manage reimbursements within the NHS system (Herbert, Wijlaars, Zylbersztejn, Cromwell, & Hardelid, Reference Herbert, Wijlaars, Zylbersztejn, Cromwell and Hardelid2017). We also linked data from the Office for National Statistics to obtain the 2015 Index of Multiple Deprivation (IMD) (Office for National Statistics, 2015). The 2015 IMD provides a relative measure of deprivation across small areas in England as calculated in 2015. The IMD quintile was then determined for patients in CPRD based on patient postcode. We compared patients eligible for linkage to those who were not eligible to assess linkage bias.
Study follow up
For the cohort of patients with SMI, follow up began the day following the first diagnosis of SMI received in primary care. For the comparator population, we used the same start date as their matched case. Patients were followed up from this date until their CPRD record ended or to the end of HES data; 31 March 2017.
Outcomes
The primary outcomes were planned and emergency hospital admissions for physical health conditions. Secondary outcomes were emergency admissions for accidents, injuries, and substance misuse, and for avoidable admissions, due to ambulatory care sensitive conditions (ACSC), a list of conditions deemed potentially preventable with appropriate primary care (Purdy et al., Reference Purdy, Griffin, Salisbury and Sharp2009). We defined admissions as spells of continuous hospitalisation in a single hospital. We excluded hospital spells where a patient was transferred from another hospital (1.8% of admissions) or where the source of admission was not given (0.1%). The reason for admission was identified based on ICD-10 codes for the primary diagnosis of the first episode of care within a spell. We excluded maternity admissions, and admissions that were regular repeat attendances, for example for regular cancer treatment or renal dialysis, or admissions where the primary diagnosis was related to mental health, or due to congenital conditions. We classified remaining admissions as due to ‘physical health’, ‘accident, injury and substance misuse’, or ‘other cause’ (online Supplementary Table S2).
Covariates
Covariates were derived from primary care and LSOA data. We included age, sex, ethnicity, region and IMD as potential confounders based on previous literature (Busby, Purdy, & Hollingworth, Reference Busby, Purdy and Hollingworth2017b; Cournane et al., Reference Cournane, Byrne, Conway, O'Riordan, Coveney and Silke2015; Huntley et al., Reference Huntley, Lasserson, Wye, Morris, Checkland, England and Purdy2014; Petersen, Kandt, & Longley, Reference Petersen, Kandt and Longley2021). We defined age as age at index based on year of birth as a continuous variable. Sex and ethnicity were reported as recorded in the patient's primary care medical records. Ethnicity was grouped based on the UK 2011 Census Ethnic Group categories (Office for National Statistics, 2014): ‘Asian’, ‘Black’, ‘Mixed’, ‘White’ or ‘Other’. Where multiple ethnicities existed for an individual, we selected the most frequent, and where frequencies were equal, the most recent ever recorded. Region was based on primary care practice postcode, and IMD was based on patient postcode and, where this was missing, the primary care practice postcode.
We also investigated physical health, substance misuse, smoking and obesity as potential confounders. Underlying physical health conditions and multimorbidity are key drivers of admissions, while substance misuse, obesity and smoking may increase the severity or result in poor self-management of physical health conditions and may be precursors to physical disease. We included a count of 24 physical health conditions, defined from code lists for the Elixhauser and Charlson Comorbidity Index (Launders et al., Reference Launders, Hayes, Price and Osborn2022; Metcalfe et al., Reference Metcalfe, Masters, Delmestri, Judge, Perry, Zogg and Costa2019). For investigation of avoidable admissions, angina was also included, defined using the Caliber code list (https://www.caliberresearch.org/portal/codelists). We defined alcohol and drug misuse using the code lists for the Elixhauser comorbidity index (Metcalfe et al., Reference Metcalfe, Masters, Delmestri, Judge, Perry, Zogg and Costa2019). We categorised smoking status as never-smoker, ex-smoker, or current smoker using medical code lists, taking the most recent category prior to index, and recording any never-smokers with a historical code for smoking as ex-smokers. We took the most recent BMI prior to index, categorised as obese (BMI ⩾ 30), overweight (BMI 25 to 29.9), healthy weight (BMI 18.5 to 24.9) or underweight (BMI < 18.5), derived from the recording of obesity, BMI, and BMI calculated from weight and height recording.
Missing data
We coded patients with missing smoking or BMI data as never-smoker and normal range BMI respectively, as general practitioners are less likely to record values that are within the normal range (Hippisley-Cox & Coupland, Reference Hippisley-Cox and Coupland2013; Marston, Nazareth, Petersen, Walters, & Osborn, Reference Marston, Nazareth, Petersen, Walters and Osborn2014). We coded ethnicity as White ethnic group where this variable was missing. This approach is in line with previous research using primary care data, which suggests that more than 93% of individuals without ethnicity recorded are from a white ethnic group (Hippisley-Cox et al., Reference Hippisley-Cox, Coupland, Vinogradova, Robson, Minhas, Sheikh and Brindle2008). Furthermore, sensitivity analyses comparing physical health outcomes using this method found similar effect estimates as using multiple imputations (Launders et al., Reference Launders, Hayes, Price and Osborn2022).
Analysis
As the distribution of admissions within the study population was ‘over dispersed’, with many zero counts, we considered the use of Poisson, negative binomial and zero-inflated models in the analysis. We found little improvement between negative binomial and zero-inflated negative binomial models (online Supplementary Table S3) and therefore used negative binomial regression for all outcomes, with sandwich standard errors to account for clustering by primary care practice.
We calculated crude incidence rate ratios (IRR) of all hospital outcomes stratified by SMI diagnosis (schizophrenia, bipolar disorder, other psychoses), then calculated adjusted IRR (aIRR), first adjusting for demographic variables (age, sex, ethnicity, region, IMD quintile, calendar year); then health risk factor variables (BMI category, smoking, alcohol misuse, drug misuse) and a count of physical health conditions as recorded in primary care.
For the analysis of avoidable admissions, we additionally adjusted for diagnosis of each separate chronic condition in the ACSC definition (angina, asthma, COPD, congestive heart failure, deficiency anaemia, hypertension, diabetes, and neurological disease) as recorded in primary care and a count of the remaining physical health conditions not included in the ACSC definition.
For all outcomes, we calculated E values to assess the potential for residual confounding (VanderWeele & Ding, Reference VanderWeele and Ding2017). We reported this study according to the Strengthening the Reporting of Observational Studies in Epidemiology checklist (Strobe Checklist) (von Elm et al., Reference von Elm, Altman, Egger, Pocock, Gotzsche, Vandenbroucke and Initiative2007).
Sensitivity analyses
We conducted five sensitivity analyses which were defined a priori. We investigated admissions in the first year post SMI diagnosis, due to the potential for different healthcare use due to increased physical health monitoring or less stable mental health compared to other time points. We investigated the effect of covariates updated at one-year post-diagnosis, to account for potential increased capture of physical health conditions around the time of SMI diagnosis. We limited the population to those with at least one year of registration prior to the start date, to investigate the impact of possible incomplete baseline data, and reran the main analysis with individual physical health conditions rather than a count to investigate the potential of residual confounding. Finally, we ran the models to account for the use of primary (online Supplementary Table S4), and secondary (planned and emergency non-mental health admissions) care use in the year prior to the start date. A final post-hoc sensitivity analysis was performed to assess the impact of using a zero-inflated negative binomial model for the primary outcomes.
Results
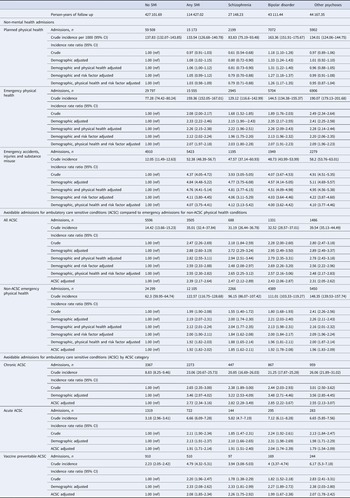
We identified 118468 patients eligible for linkage with HES, of which 23415 did not meet our inclusion/exclusion criteria. A further 108 had multiple records in CPRD for one HES record and 2996 could not be matched at least 1:1 (online Supplementary Fig. S1). The final cohort consisted of 20568 people with SMI and 71 381 matched comparators (Table 1). Patients eligible for HES linkage were similar in respect to SMI diagnosis, age at start of follow up, sex, BMI, smoking and multimorbidity to those which were ineligible (online Supplementary Table S5). A total of 67.58% of patients could be matched 1:4, 25.79% 1:3, 5.49% 1:2 and 1.14% 1:1.
Table 1. Demographic and clinical variables in those with and without SMI
a Index is date of SMI diagnosis or, for patients without SMI, the diagnosis date of the matched patient with SMI.
b Ethnicity: missing coded as white [SMI: 7886 (38.34%); comparators: 30 922 (43.32%)].
c Index of multiple deprivation: missing patient IMD coded as primary care practice IMD [SMI: 44 (0.21%); comparators: 102 (0.14%)].
d BMI: missing coded as normal range [SMI: 5216 (25.36%); comparators: 18 178 (25.47%)].
e Smoking: missing coded as never smoker [SMI: 2467 (11.99%); comparators: 9233 (12.93%)].
Demographic and clinical factors
A higher proportion of patients with SMI were identified as Black ethnic group (4.85% v. 3.00%) and from the most deprived IMD quintile (26.50% v. 19.90%) compared to comparators. Patients with SMI had a higher prevalence of physical health conditions and multimorbidity than comparators and were more likely to have a recording of obesity, current smoking, substance misuse recorded in their primary care record (Table 1) and used primary care more frequently in the year prior to and following SMI diagnosis than comparators (online Supplementary Table S6).
Primary outcomes: admissions for physical health
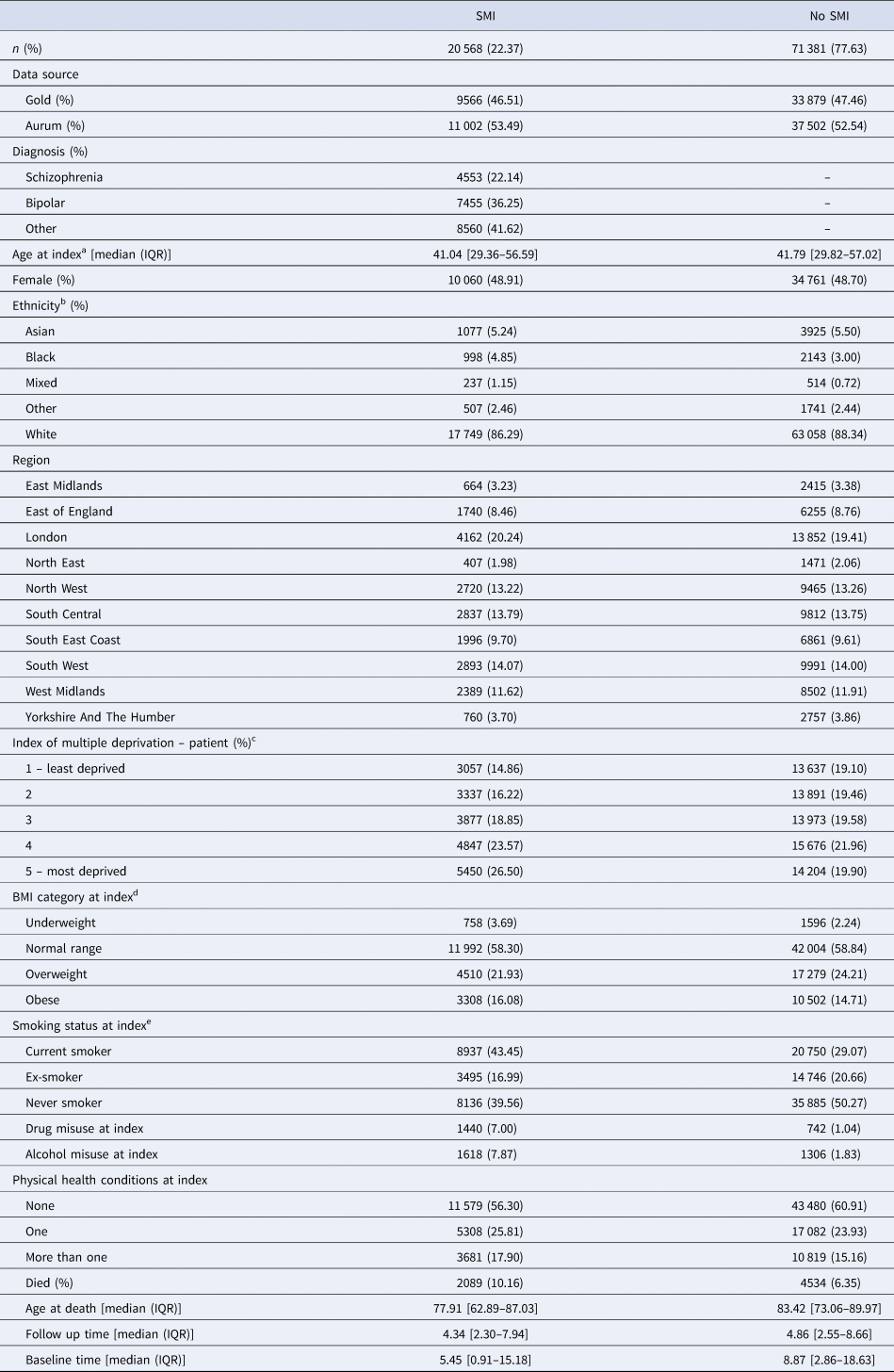
The crude incidence of emergency and planned physical health admissions was higher than other non-mental health emergency causes, for patients with and without a diagnosis of SMI (Fig. 1, Table 2). Patients with a diagnosis of schizophrenia and other psychoses had more emergency physical health admissions than planned physical health admissions, whereas those with bipolar disorder or no SMI diagnosis had fewer (Fig. 1, Table 2). When stratified by SMI diagnosis, the crude incidence of emergency physical health admissions was elevated compared to comparators for all three SMI diagnostic groups (Fig. 1) and there was little difference in aIRRs across SMI groups (Table 2; Fig. 2). Controlling for physical health conditions increased the aIRR for those with schizophrenia while it decreased it for those with bipolar disorder and other psychoses (Table 2). When all SMI diagnoses were pooled, people with SMI had 2.33 times more admissions than people without SMI (aIRR: 2.33; 95% CI 2.22–2.46) after adjusting for demographic variables (age, sex, region, ethnicity, IMD, year of index). This effect remained even after controlling for health risk factors (BMI, smoking, alcohol, and drug misuse) and underlying physical health conditions (aIRR: 2.07; 95% CI 1.97–2.18, Table 2).
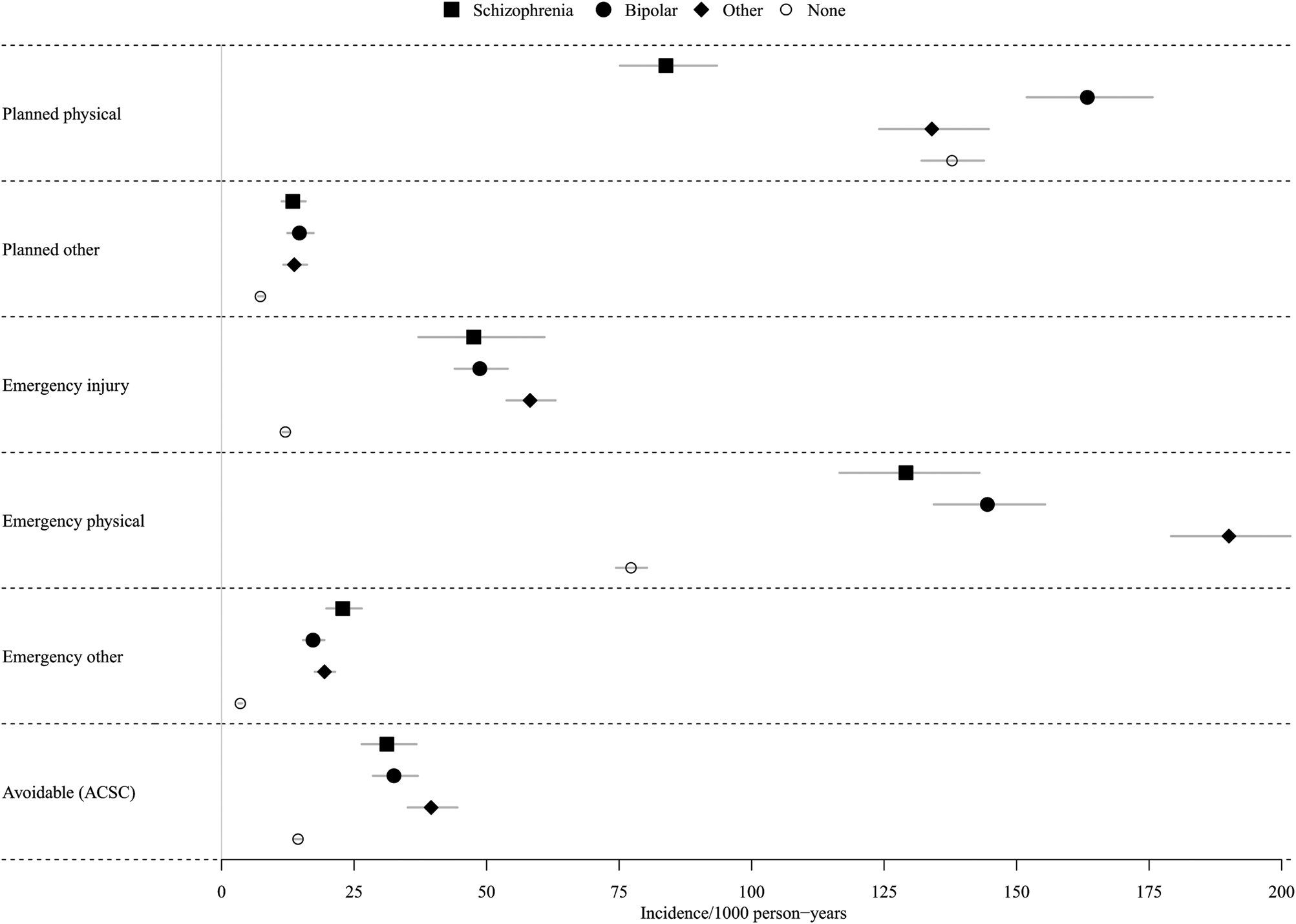
Fig. 1. Unadjusted incidence of hospital admission outcomes per 1000-person years.
Planned physical: Planned admissions for physical health.
Planned other: Planned admissions for other non-mental health causes.
Emergency injury: Emergency admissions for accidents, injuries and substance misuse.
Emergency physical: All emergency physical admissions, including avoidable admissions.
Emergency other: Emergency admissions for other non-mental health causes.
Avoidable (ACSC): Potentially avoidable admissions, defined as ambulatory care-sensitive conditions.
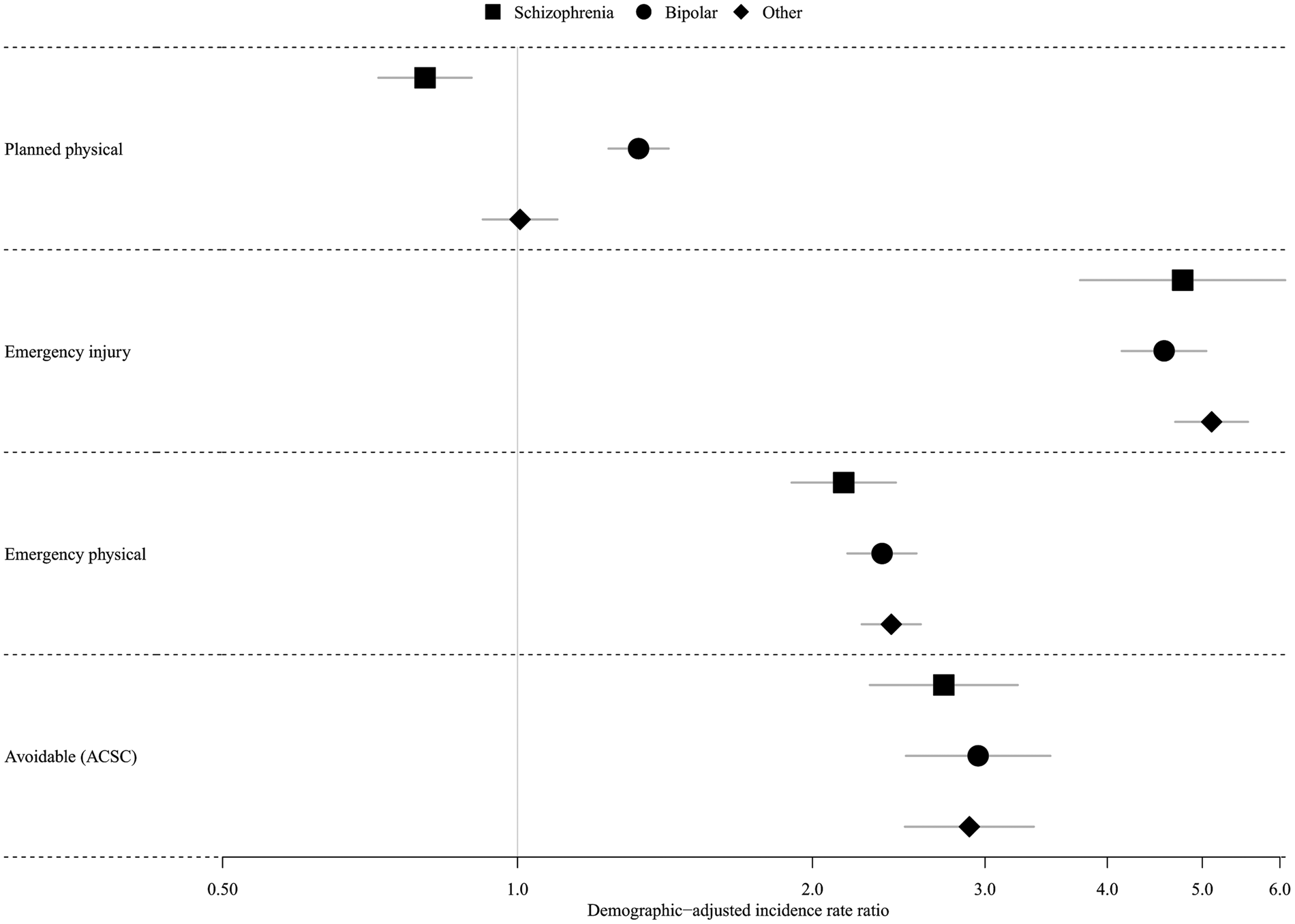
Fig. 2. Demographically adjusted incidence rate ratios (IRR) of hospital admission outcomes in patients with SMI compared to comparators.
Emergency injury: Emergency admissions for accidents, injuries and substance misuse.
Emergency physical: All emergency physical admissions, including avoidable admissions.
ACSC: Avoidable admissions, defined as ambulatory care-sensitive conditions.
Table 2. Crude and adjusted incidence rate ratio of non-mental health hospital admissions in patients with SMI compared to matched comparators
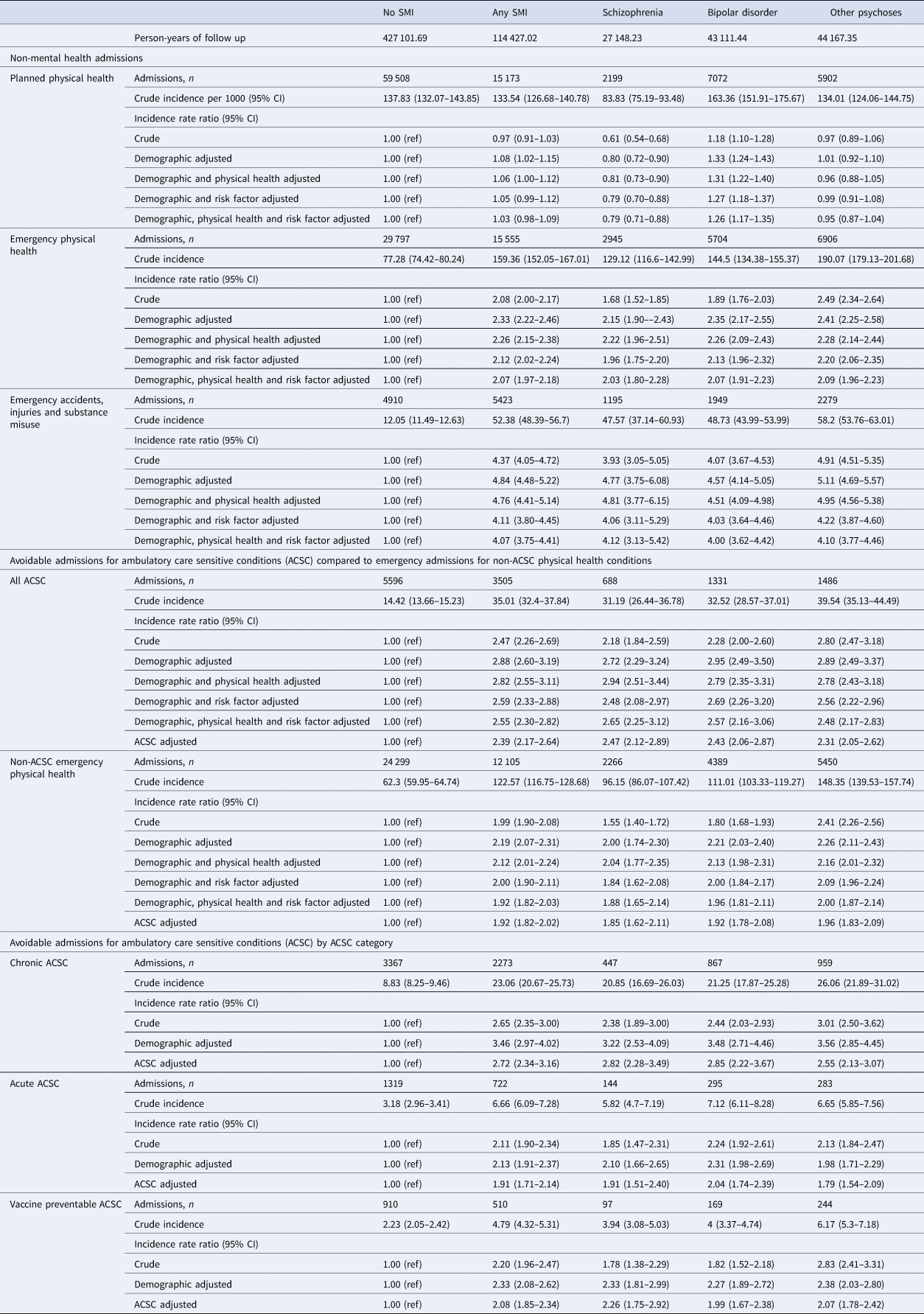
Demographic adjusted: for age at study entry, sex, IMD, ethnicity, region, year of diagnosis.
Risk factor adjusted: BMI, smoking, drug misuse, alcohol misuse.
Physical health adjusted: 24 physical health conditions.
ACSC adjusted: Adjusted for demographic variables, plus risk factors, individual ACSC chronic conditions and a count of non-ACSC physical health conditions.
In contrast, the incidence of planned admissions differed by SMI diagnosis. Patients with schizophrenia had fewer planned admissions compared to comparators (aIRR: 0.80; 95% CI 0.72–0.90), while those with bipolar disorder had more (aIRR: 1.33; 95% CI 1.24–1.43; Table 2 & Fig. 2). As with the emergency physical health admissions, controlling for health risk factors (BMI, smoking, alcohol, and drug misuse) and underlying physical health conditions did not alter the findings, and controlling for physical health decreased the aIRR for patients with bipolar disorder and other psychoses; but increased the aIRR for patients with schizophrenia.
The E value for the fully adjusted IRR of planned physical admissions in people with schizophrenia compared to those without SMI was 1.85, suggesting an unmeasured confounder would need an effect size of 1.85 in relation to both schizophrenia and hospitalisation to confound this finding. For the IRR of emergency physical health admissions in those with SMI v. no SMI, the E value was 3.56.
Secondary outcomes: avoidable admissions and emergency accident, injury, and substance use admissions
The incidence of emergency avoidable admissions compared to those without SMI was similar ion patients with schizophrenia, bipolar disorder and other psychoses (Table 2; Fig. 2). When pooled across diagnoses, patients with SMI had a higher incidence of emergency avoidable admissions than those without SMI (aIRR: 2.88; 95% CI 2.60–3.19). This remained, even after controlling for prior diagnosis of individual physical health conditions included in the ACSC definition and a count of other physical health conditions (aIRR: 2.39; 95% CI 2.17–2.64); and was higher than for emergency physical health admissions not defined as avoidable (Table 2). When stratified by type of avoidable admission, the aIRR was highest for admissions due to chronic physical health conditions (aIRR: 3.46; 95% CI 2.97–4.02; Table 2).
Rates of emergency accident, injury and substance misuse admissions were lower than emergency physical health admissions (Fig. 1), however patients with an SMI had markedly elevated rates of emergency accident, injury and substance misuse admissions compared to the non-SMI comparator population (aIRR: 4.84; 95% CI 4.48–5.22).
The E value for the fully adjusted IRR of emergency avoidable admissions in those with v. without SMI was 4.21, and for admissions for accidents, injuries and substance misuse admissions was 7.60
Sensitivity analyses
Limiting the outcome period to the first year following diagnosis, increased the crude and adjusted IRR for all outcomes, particularly for emergency admissions for accidents, injuries, and substance misuse (sensitivity: aIRR: 6.18; 95% CI 5.46–6.98 v. main model: 4.84; 95% CI 4.48–5.22, online Supplementary Table S7).
Controlling for the number of primary care consultations and emergency and planned non-mental health admissions in the year prior to index attenuated our main findings for all outcomes; the incidence of emergency physical (aIRR: 1.52; 95% CI 1.44–1.59), avoidable admissions (aIRR:1.85, 95% CI 1.67–2.04) and emergency accident, injury, and substance misuse admissions (aIRR: 3.06; 95% CI 2.87–3.27) remained elevated (online Supplementary Table S8). Excluding those patients with less than one year's baseline data (online Supplementary Table S8) and updating physical health and risk factor covariates to account for better capture in the year following diagnosis (online Supplementary Table S9) or controlling for individual physical health conditions (online Supplementary Table S10) did not alter the findings. Using zero-inflated negative binomial regression resulted in a lower aIRR for emergency and planned physical health admissions, though the effect sizes had overlapping confidence intervals with those of the negative binomial model, and it did not alter the findings (online Supplementary Table S11).
Discussion
Physical health admissions in NHS secondary care were the most frequent non-mental health reason for hospital admissions for those with and without SMI. People with SMI were over twice as likely to have an emergency physical health admission during the study period than those without SMI, and the rate of admissions was similar across SMI diagnoses. This remained true after controlling for a wide range of demographic and clinical factors.
Emergency admissions due to chronic avoidable conditions were almost three and a half times the admission rate in patients with SMI compared to those without SMI. Given the high prevalence of diabetes, COPD and neurological disease in people with SMI (Launders et al., Reference Launders, Hayes, Price and Osborn2022), this represents a major burden on the NHS. Controlling for pre-existing physical health conditions did not alter our findings, suggesting that the number of underlying physical health conditions that a patient has recorded in primary care is not the only driver of the high rate of physical health admissions in people with SMI. In contrast, the high rate of avoidable admissions for chronic conditions suggests that severity or control of pre-existing physical health conditions leads to high emergency admissions for physical health. As these conditions are thought to be preventable or can be reduced by actions in primary care or community settings, this suggests that targeted approaches to improving physical health screening, and the monitoring and treatment of chronic physical health conditions in community settings are needed to reduce emergency hospital admissions in this population. While physical health checks are incentivised in primary care in the UK, a previous study found that while care plans reduced avoidable admissions in those with SMI, physical health checks for BMI, blood pressure, cholesterol and glucose did not (Ride et al., Reference Ride, Kasteridis, Gutacker, Kronenberg, Doran, Mason and Jacobs2018). A range of interventions are therefore likely required to reduce avoidable admissions in those with SMI, such as physical health clinics in psychiatric services, more thorough physical health checks and screening, improved uptake of care plans, and personalised care and support to better manage existing physical health conditions.
Furthermore, people with SMI also have a high prevalence of modifiable health risk factors (Launders et al., Reference Launders, Hayes, Price and Osborn2022), which may increase the severity or affect the management of physical health conditions. Interventions aimed at reducing these, such as smoking or alcohol cessation services have been shown to be effective (Gilbody et al., Reference Gilbody, Peckham, Bailey, Arundel, Heron, Crosland and Vickers2019; McDonell et al., Reference McDonell, Leickly, McPherson, Skalisky, Srebnik, Angelo and Ries2017), and may also act to reduce emergency admissions.
The year following SMI diagnosis appears to be a time of high emergency hospital admissions utilisation in people with SMI. We found that people with SMI were over five times as likely to be admitted for accidents, injuries and substance misuse, and almost three times as likely to have an avoidable admission in the year following SMI diagnosis. This suggests that targeted interventions around the time of diagnosis are required, particularly focusing on risk reduction and management of existing physical health conditions.
Excess emergency admissions reduce the quality and length of life for those with SMI and represent a cost burden to the NHS. Using a prevalence of SMI in 2015/2016 of 0.89% (Grigoroglou et al., Reference Grigoroglou, Munford, Webb, Kapur, Ashcroft and Kontopantelis2020), and a population of 43.8 million people aged 18 or over in 2017 in England; this suggests an excess of between 35 000 to 45 000 admissions per year, likely to cost in excess of £55 million (using an average emergency admission cost of £1603 in 2017/2018) (NHS Improvement, 2019).
In contrast to the findings of all emergency admission outcomes, there were marked differences by SMI diagnosis for planned physical health admissions, and we found that pooling results for all SMI diagnoses potentially masks differences in planned healthcare utilisation. People with bipolar disorder had elevated rates of planned physical health admissions, while those with schizophrenia had far lower rates. While low rates of emergency inpatient admissions are usually deemed to be a sign of good preventative and primary care, the lower-than-expected rates of planned admissions for physical health in people with schizophrenia are of concern, and suggest potential barriers to access of planned inpatient care in this population. However, while there has been research into barriers to attending screening and other disease-specific specialist services (Bramberg, Torgerson, Kjellstrom, Welin, & Rusner, Reference Bramberg, Torgerson, Kjellstrom, Welin and Rusner2018; Melamed et al., Reference Melamed, Fernando, Soklaridis, Hahn, LeMessurier and Taylor2019; Murphy et al., Reference Murphy, Stone, Presskreischer, McGinty, Daumit and Pollack2021), as well as primary care (Bramberg et al., Reference Bramberg, Torgerson, Kjellstrom, Welin and Rusner2018; Decoux, Reference Decoux2005; Kohn et al., Reference Kohn, Christiaens, Detraux, De Lepeleire, De Hert, Gillain and Jespers2021; Mitchell et al., Reference Mitchell, Zuraw, Delaney, Twohig, Dolan, Walton and Yousefpour2022), there is less information on barriers to planned inpatient admissions. We need to understand the reasons for reduced rates of planned care specifically in people with schizophrenia as this may contribute to the mortality gap for this group of patients.
Strengths and limitations
To our knowledge, this is the first study to investigate both planned and emergency admissions in people with SMI, and the first longitudinal study based in England investigating admissions in people with SMI compared to matched comparators. While previous studies have found high rates of potentially avoidable admissions in those with SMI (Davydow et al., Reference Davydow, Ribe, Pedersen, Fenger-Grøn, Cerimele, Vedsted and Vestergaard2016; Lin et al., Reference Lin, Huang, Chen and Chen2011; Mai, Holman, Sanfilippo, & Emery, Reference Mai, Holman, Sanfilippo and Emery2011), the size of this cohort allows for stratification by SMI diagnosis and investigation of causes other than avoidable ACSC admissions, furthering the understanding of the differences in hospital utilisation in people with SMI.
The use of linked primary and secondary care records is a major strength of our study. Many studies of hospital admissions use only hospital data and are therefore limited to patients who attend hospital during a baseline period. The longitudinal nature of primary care records in England, and richness of data they contain, allows for a more complete capture of demographic and clinical data and a more accurate comparison of hospital admission rates between those with and without SMI in the general population.
We were able to control for known causes of variation in hospital admissions at the patient level, such as age, sex, ethnicity and deprivation (Busby, Purdy, & Hollingworth, Reference Busby, Purdy and Hollingworth2017a). Patients with SMI were matched with comparators in the same primary care practice, reducing the known variation in hospital admission rates between practices, and regionally in England (Busby et al., Reference Busby, Purdy and Hollingworth2017b). Controlling for pre-existing physical health conditions did not alter our findings, suggesting that the number of underlying physical health conditions that a patient has recorded in primary care is not the only driver of the high rate of physical health admissions in people with SMI. This is supported by a previous study of avoidable ACSC conditions in those with SMI (Davydow et al., Reference Davydow, Ribe, Pedersen, Fenger-Grøn, Cerimele, Vedsted and Vestergaard2016). For those with schizophrenia, controlling for pre-existing physical health conditions did not reduce the IRR of any of the hospital outcomes, possibly due to an under-ascertainment of physical disease in this population (Gabilondo, Alonso-Moran, Nuno-Solinis, Orueta, & Iruin, Reference Gabilondo, Alonso-Moran, Nuno-Solinis, Orueta and Iruin2017; Launders et al., Reference Launders, Hayes, Price and Osborn2022; Smith, Langan, McLean, Guthrie, & Mercer, Reference Smith, Langan, McLean, Guthrie and Mercer2013).
While we controlled for physical health conditions, we did not control for other mental health diagnoses. It is recognised that physical health admissions are elevated in people with anxiety and depression (Guthrie et al., Reference Guthrie, Dickens, Blakemore, Watson, Chew-Graham, Lovell and Tomenson2016) and high rates of these diagnoses in those with SMI may therefore contribute to high admissions. However, whether depression and anxiety is a symptom of SMI or a separate condition may not be clear (Upthegrove, Marwaha, & Birchwood, Reference Upthegrove, Marwaha and Birchwood2017), and therefore the role of other mental health diagnoses on hospitalisations in this population is hard to determine.”
While we were able to control for a range of covariates, the matching strategy of this cohort could have introduced bias. People with SMI were matched to those who did not develop SMI at any time prior to or during follow up. Given those with SMI are known to use more healthcare resources in the years prior to SMI diagnosis (Wallace et al., Reference Wallace, Isenberg, York, Shinde, Barron, Franchino-Elder and Sidovar2020), this could have resulted in the under-estimation of hospital utilisation in the comparator population. However, given that the incidence of SMI is low (Hardoon et al., Reference Hardoon, Hayes, Blackburn, Petersen, Walters, Nazareth and Osborn2013) the probability of matching a person with SMI to a person who will develop SMI in the future is also low, and therefore the impact is probably limited.
In the general population, hospital use in the year prior to outcome period may be the strongest predictor of hospital admissions (Donnan, Dorward, Mutch, & Morris, Reference Donnan, Dorward, Mutch and Morris2008; Hippisley-Cox & Coupland, Reference Hippisley-Cox and Coupland2013), and therefore useful for predicting which individuals will use hospital services. However, in models comparing admissions between groups it may represent over-adjustment, since the same causal factors driving admissions may be present prior to and after index date, particularly in the year prior to SMI diagnosis, where healthcare use may be elevated (Wallace et al., Reference Wallace, Isenberg, York, Shinde, Barron, Franchino-Elder and Sidovar2020). In our study, including these variables attenuated all effect sizes but did not alter the main findings.
While CPRD is broadly representative of England's population (Herrett et al., Reference Herrett, Gallagher, Bhaskaran, Forbes, Mathur, van Staa and Smeeth2015; Wolf et al., Reference Wolf, Dedman, Campbell, Booth, Lunn, Chapman and Myles2019), there may be residual confounding due to missing data or linkage bias. In particular, the capture of physical health diagnoses in primary care may be subject to surveillance bias, whereby those who attend primary care more often have more opportunities to have physical health conditions diagnosed and recorded.
Finally, we did not investigate the length of stay in this study. Previous research has found that people with SMI have longer non-mental health hospital stays than those without SMI (Ronaldson et al., Reference Ronaldson, Elton, Jayakumar, Jieman, Halvorsrud and Bhui2020) and higher hospital costs for avoidable admissions (Sporinova et al., Reference Sporinova, Manns, Tonelli, Hemmelgarn, MacMaster, Mitchell and Quinn2019). These periods of admission and stays in inpatient psychiatric care represent periods of time where the patient is unable to experience admissions and could therefore have lowered the admission rate in those with SMI.
While the average length of stay is elevated, those with SMI may also be at increased risk of discharge against medical advice. While we could find no studies investigating discharge disposition for physical health admissions in people with SMI, this could result in a greater risk of multiple short admissions, and drive some of the high 30-readmission rates observed in this population (Germack et al., Reference Germack, Caron, Solomon and Hanrahan2018; Ronaldson et al., Reference Ronaldson, Elton, Jayakumar, Jieman, Halvorsrud and Bhui2020). The likely complex pattern of the length of stays for physical health admissions, reasons for discharge, and the impact this has on hospital utilisation in those with SMI requires further research.
Conclusions
We found that people with SMI have a markedly increased rate of emergency physical health admissions compared to people without SMI. We also identified an under-utilisation of planned physical health hospital services in those with schizophrenia. Further research is required to determine the drivers of high-frequency admissions in those with underlying physical disease, and potential barriers to optimal use of healthcare services in this population. To reduce physical health admissions in people with SMI, targeted interventions are required in community and psychiatric services, aimed at improving access to appropriate care, ensuring effective physical health screening, and providing support to enable appropriate treatment and control of chronic physical health conditions.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S0033291722002811
Financial support
This study was supported by Public Health England and the Office for Health Improvement and Disparities (PhD2019/002), the Wellcome Trust (211085/Z/18/Z), the Medical Research Council (MC\PC\17216), UKRI Medical Research Council (MR/W014386/1), UKRI (MR/V023373/1), University College London Hospitals NIHR Biomedical Research Centre and the NIHR ARC North Thames Academy.
This report is independent research supported by the National Institute for Health Research ARC North Thames. The views expressed in this publication are those of the author(s) and not necessarily those of the National Institute for Health Research or the Department of Health and Social Care, Public Health England or the Office for Health Improvement and Disparities.
Conflict of interest
JFH has received consultancy fees from Wellcome Trust and Juli Health; the remaining authors declare no conflicts of interest.