With rapid economic growth and adverse changes in lifestyle, CVD have ranked highest among the leading cause of death in developed countries and most developing countries as well as in China(Reference Benjamin, Blaha and Chiuve1). For instance, the annual number of deaths owing to CVD increased from 2·51 million to 3·97 million between 1990 and 2016 in China; in 2016, the prevalent cases of CVD reached nearly 94 million with a high disability-adjusted life years attributable to CVD (78·106 million)(Reference Liu, Li and Zeng2). Abnormal lipid levels, as one of the leading causes of atherosclerosis, which are positively linked with the development of CVD(3), are characterised by elevated levels of serum total cholesterol (TC), TAG and LDL-cholesterol, and low levels of HDL-cholesterol. Recently, Chinese adults experienced a high prevalence of abnormal serum lipid levels; the prevalence of high TC, high LDL-cholesterol, low HDL-cholesterol and high TAG was 6·9, 8·1, 20·4 and 13·8 %, respectively(Reference Zhang, Deng and Wang4). There is also accumulating evidence that other lipid measures such as non-HDL-cholesterol and apoB may be more accurate predictors of CVD risk(Reference Kastelein, van der Steeg and Holme5). A serum non-HDL-cholesterol level is a comprehensive measure of atherogenic lipids, which included LDL-cholesterol, lipoprotein (a), intermediate-density lipoprotein and VLDL remnants(Reference Usui, Nagata and Hata6). Growing evidence suggests that elevated serum non-HDL-cholesterol levels are related to an increased risk of CVD events in the general population(Reference Usui, Nagata and Hata6,Reference Verbeek, Hovingh and Boekholdt7) . Many studies show that diet is one of the most important modifiable risk factors for lipid metabolism(Reference Siri-Tarino and Krauss8–Reference Song, Paik and Park10), providing effective means to achieve healthy and nutritious diets is essential for CVD prevention.
Chili is one of the most popular and important spices, used as food flavouring(Reference Nilius and Appendino11). Spiciness or pungency was regarded as one of the basic tastes in ancient India and China(Reference Nilius and Appendino11,Reference Szolcsanyi12) . According to the FAO of United Nations in 2017, the domestic supply quantity of spices in China was up to 253 000 tonnes and the annual food supply quantity per capita was about 0·17 kg(13). In China, more than 30 % of adults eat spicy food, daily(Reference Lv, Qi and Yu14). A lot of studies have been conducted to explore the effects of spicy food and their bioactive ingredients such as capsaicin. Many studies have shown healthy benefits of chili, including antimicrobial, anti-oxidative(Reference Li, Wang and Xiao15), anti-inflammatory, anti-obesity(Reference Janssens, Hursel and Westerterp-Plantenga16) and hypolipidaemic effects(Reference Zhao and Chen17). It is also demonstrated that spicy food has a beneficial effect on supporting weight management(Reference Tremblay, Arguin and Panahi18), controlling hypertension(Reference Li, Cui and Jin19) and both total and certain cause-specific mortality(Reference Lv, Qi and Yu14,Reference Chopan and Littenberg20) . But some studies also have found there are positive associations between spicy food consumption or spicy strength and risk of several health outcomes: a meta-analysis based on evidence from case–control studies (7884 patients with cancer and 10 142 controls) suggested that a higher level of spicy food intake may be associated with an increased incidence of cancer(Reference Chen, Zou and Zheng21); a total of 434 556 adults cross-sectional study indicated that spicy food intake (including frequency, strength and duration of spicy food eating) is a risk factor for obesity in China(Reference Sun, Lv and Chen22); another cross-sectional study conducted among 512 891 Chinese adults found a positive association between the level of spicy food intake and history of fractures(Reference Mei, Fang and Yin23). In addition, although two studies have explored the association between spicy food and lipid profiles in Chinese people(Reference Xue, He and Yu24,Reference Yu, Xue and He25) , however, there were some inconsistent results on lipid measures, and the association of spicy strength with lipids levels has not been examined. For example, Xue et al. (Reference Xue, He and Yu24) have found that spicy food consumption was inversely associated with TC and positively associated with serum TAG in adults, while Yu et al. (Reference Yu, Xue and He25) only observed that women with higher frequency of spicy food consumption had lower TC, LDL-cholesterol and LDL-cholesterol/HDL-cholesterol. Moreover, Almotayri et al. (Reference Almotayri, Jois and Radcliffe26) suggested that the antioxidant and anti-inflammatory properties of spices may play an important role in ameliorating the inflammatory process of some chronic diseases such as abnormal serum lipid levels. However, the epidemiological evidence on the association of spicy food intake with serum lipid levels is limited and needed to be further explored.
Given the context as mentioned above, therefore, the current study aimed to investigate the associations between spicy food flavour or intake frequency and blood lipid levels and risk of abnormal serum lipid levels in a large Chinese rural population from the Henan Rural Cohort Study.
Methods
Study population
Henan province is located in central China, which is an important province in agricultural production, with a rural population accounting for 79 % of the total population (approximately 94 million in 2010)(Reference Liu, Mao and Li27). The rural population of Henan province accounts for 10 % of China’s rural population and is typical of rural areas in China. The study design is cross-sectional, based on the baseline survey of the Henan Rural Cohort Study, which was registered on the Chinese Clinical Trial Register (Registration number: ChiCTR-OOC-15006699). The cohort profile has been described(Reference Liu, Mao and Li27). A multistage, stratified cluster sampling method was used to obtain samples in the general population. Briefly, the baseline survey was carried out in Yuzhou, Suiping, Tongxu, Xinxiang and Yima counties of Henan province in China between July 2015 and September 2017. A total of 39 259 people aged 18–79 years old and with complete information of the questionnaire and physical measurements were recruited into the current study. To better estimate the relationship between spicy food intake and lipid metabolism, participants with incomplete information of spicy food (n 29), missing data about TC, TAG, HDL-cholesterol, LDL-cholesterol (n 197) were excluded. We also excluded those participants who had a self-reported doctor diagnosis of cancer (n 329) or hepatitis (n 466). Finally, 38 238 participants with information of spicy flavour were included in the current analysis, of which 29 034 participants had information on spicy food intake frequency. In addition, information on family history of hyperlipidaemia, CHD and stroke was collected from all participants.
Assessment of spicy food intake and dietary intake
Information about spicy food intake was collected using a two-item questionnaire survey by well-trained staffs through face-to-face interviews. Spicy food flavour and intake frequency were assessed as proxy of spicy food intake. For assessment of the flavour of spicy food, participants were asked ‘How much do you like the spicy flavor in your food?’ (1) no, (2) mild, (3) middle and (4) heavy. Participants were further asked ‘During the past month, how often did you eat spicy foods in one week?’ (1) never, (2) 1–2 d/week, (3) 3–5 d/week and (4) 6 or 7 d/week(Reference Yang, Li and Mao28). The test–retest reliability and the internal consistency of questionnaire were accredited through a pilot study with seventy-six subjects. The internal consistency of Cronbach’s α coefficients was 0·978 for spicy food intake frequency, which indicated that the variable could provide a reasonable estimation of spicy food intake.
Individual dietary intake data were collected by a validated FFQ(Reference Xue, Yang and Wang29). The FFQ consisted of thirteen main food groups, including staple, livestock, poultry, fish, eggs, dairy, fruits, vegetables, beans, nuts, pickles, cereal and animal oil. For each food item, participants were asked to report the quantity and frequency of food they consumed over the past year. The interviewee was required to state the quantity of food consumed (kg, g) according to five frequencies of consumption (never, day, week, month, year). The three consecutive day (1 weekend day and 2 weekdays) 24-h dietary recalls were conducted in a small sample to validate the FFQ, and the results demonstrated that they could be used as a representative tool to conduct a dietary evaluation of a rural population(Reference Xue, Yang and Wang29). For each individual, the mean total daily energy intake and the proportions from protein, fat and carbohydrate were derived from dietary data according to the Chinese Food Composition Table 2004(Reference Yang, Wang and Pan30). In addition, four dietary patterns were identified using factor analysis as described before (dietary pattern I: red meat, white meat and fish; pattern II: vegetables, staple food and fruits; pattern III: grains, nuts, beans, pickles and animal oils; and pattern IV: milk and eggs)(Reference Wang, Liu and Qiao31).
Lipid parameters quantification
After at least 8 h of overnight fasting, venous blood specimen was collected in vacuum tubes without anticoagulation. Serum samples were separated from whole blood through centrifugation for 10 min at 3000 rpm at room temperature, and then were sent to measure TC, TAG, HDL-cholesterol and LDL-cholesterol. TC, HDL-cholesterol, LDL-cholesterol and TAG were measured by enzymatic methods with an automatic chemistry analyser (Cobas C501, Roche Diagnostics GmbH). Serum non-HDL-cholesterol levels were calculated by subtracting HDL-cholesterol from TC values. According to the latest Chinese guidelines on prevention and treatment of dyslipidaemia in adults(Reference Zhu, Gao and Zhao32) and National Cholesterol Education Program Adult Treatment Panel III criteria(33), the cut-off values for abnormal TC, TAG, HDL-cholesterol, LDLC and non-HDL-cholesterol levels (borderline high or low) were 5·18 mmol/l (200 mg/dl), 1·70 mmol/l (150 mg/dl), 1·04 mmol/l (40 mg/dl), 4·14 mmol/l (160 mg/dl) and 4·10 mmol/l (160 mg/dl), respectively.
Assessment and definitions of covariates
The detailed information on demographic characteristics (name, sex, age, marital status, educational level) and lifestyle factors (tobacco use, alcohol use, physical activity, disease history) was collected through face-to-face interview by the trained research staff using a standardised questionnaire. The following variables were included in the current study: age, education (illiterate and elementary, middle school and high school and above), tobacco use (current smoker was defined as smoking at least one cigarette/d for 6 consecutive months), alcohol use (current drinker was defined as alcohol drinking at least twelve times/year as described previously)(Reference Tian, Li and Mao34), physical activity (low, middle and high) and marital status (married/cohabiting and widowed/single/divorced/separated).
Height and weight were obtained by physical examination. Weight and height measurements were converted to BMI-for-age Z-scores for individual aged 18 or 19 years old using the WHO growth reference in 2007(Reference de Onis, Onyango and Borghi35). BMI was calculated as weight (kg) divided height (m) squared for participants over 19 years. Combining the WHO reference standards and criteria recommended by Working Group on Obesity in China(Reference de Onis, Onyango and Borghi35,Reference Liu, Wu and Mao36) , BMI was divided into four groups: underweight, normal, overweight and obese.
Statistical analysis
The basic characteristics of the study participants were described by the spicy flavour (no, mild, middle, heavy) and the frequency of spicy food intake (never, 1–2/week, 3–5 d/week, 6 or 7 d/week), respectively. Continuous variables are presented as means (sd), and categorical variables are expressed as numbers (percentages). The χ 2 test was used to compare basic characteristics across the categorical variables and ANOVA for continuous variables. Tests for linear trend were conducted in all consumers by entering the different categories of spicy food intake (four spicy flavour levels or four spicy food intake frequency levels) as ordinal categorical variables in regression models. Spicy food flavour or intake frequency as an exposure variable was regressed on lipid parameters and covariates in the linear regression models; results are presented as regression coefficients (β) and 95 % CI. Furthermore, multivariable-adjusted logistic regression models were used to investigate associations of spicy food intake with risk of abnormal serum lipid levels, including abnormal TC, TAG, HDL-cholesterol, LDLC and non-HDL-cholesterol levels (borderline high or low); results are presented as OR and corresponding 95 % CI. Same three regression models were selected: model 1 was crude model without any adjustments; model 2 adjusted for age, gender, education level, marital status, smoking status, alcohol drinking, physical activity, BMI and model 3 additionally adjusted for total energy intake. Restricted cubic spline was performed to assess the dose–response relationship between spicy flavour level (no, mild, middle, heavy as first, second, third, fourth level) or intake frequency (0–7d/week) and risk for abnormal, using the first level and 0 d/week as the reference group, respectively.
To examine the robustness of our findings, sensitivity analyses were also conducted by excluding participants with self-reported CHD and stroke (n 3915) and additionally adjusting for dietary pattern and family history of hyperlipidaemia, CHD and stroke.
All statistical analyses were performed using SPSS version 21.0 and STATA version 13.1. All tests were two sided and P values < 0·05 indicated statistical significance.
Results
According to the spicy flavour and the spicy food intake frequency, the general characteristics of the 38 238 participants, aged 18–79 years, are listed in Table 1. Compared with participants who ate no spicy food, those who had preference for heavier spicy flavour were more likely to be younger, male, married/cohabiting, current smoker and consume alcohol, and more likely have higher levels of physical activities and higher BMI (P trend < 0·05). Analogous associations were observed in age, sex, marital status, tobacco use, alcohol use, total energy intake and BMI, with increased frequency of spicy food intake (P trend < 0·05).
Table 1 Demographic characteristics of study participants according to spicy food flavour and intake frequency
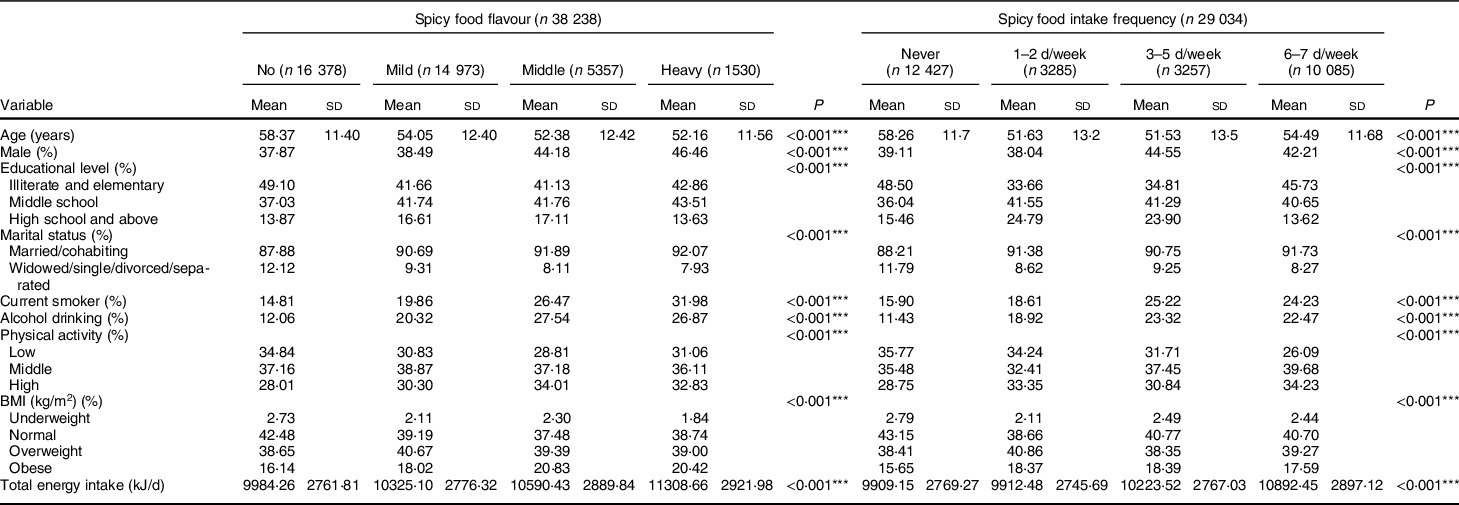
*** P < 0·001.
Multiple linear regression models showed that the heavier flavour of spicy food was positively associated with TAG levels in three models (P trend < 0·001). After adjusting for all covariates, compared with participants who ate no spicy food, the β of mild, middle and heavy spicy flavours was 0·02 (95 % CI −0·01, 0·04), 0·06 (95 % CI 0·02, 0·09) and 0·15 (95 % CI 0·10, 0·21), respectively. However, significant inverse associations were found between spicy food flavour and TC or non-HDL-cholesterol in unadjusted and adjusted models (all P trend < 0·001). Compared with participants who did not eat spicy food, significant lower TC levels in those who ate mild spicy flavour (by 0·07 mmol/l, 95 % CI −0·09, −0·05), middle spicy flavour (by 0·10 mmol/l, 95 % CI −0·13, −0·07) or heavy spicy flavour (by 0·12 mmol/l; 95 % CI −0·17, −0·07) were observed; similarly, those who had mild, middle or heavy spicy flavour also showed a lower non-HDL-cholesterol by 0·07 (95 % CI −0·09, −0·05), 0·10 (95 % CI −0·13, −0·07) or 0·10 (95 % CI −0·15, −0·05), respectively, after adjusting for potential cofounders (Table 2). Further multiple linear analyses according to frequency of spicy food intake were presented in Table 3. Similar to the findings of spicy food flavour, the frequency of spicy food intake was also positively associated with TAG level (P trend < 0·001) and inversely progressively associated with TAG and non-HDL-cholesterol levels in model 3 (P trend < 0·001), although the associations were only found in who consumed spicy food 3–5 d/week or more. In contrast with the flavour of spicy food, compared with participant who never eat spicy food, those who consumed spicy food 6–7 d/week had higher HDL-cholesterol by 0·01 mmol/l (95 % CI 0·01, 0·02) and lower LDL-cholesterol/HDL-cholesterol ratio by 0·02 (95 % CI −0·04, −0·01) after adjusting for confounding factors. Furthermore, there were no significant associations between spicy flavour and LDL-cholesterol level in the fully adjusted model.
Table 2 Associations between spicy food flavour and blood lipid levels
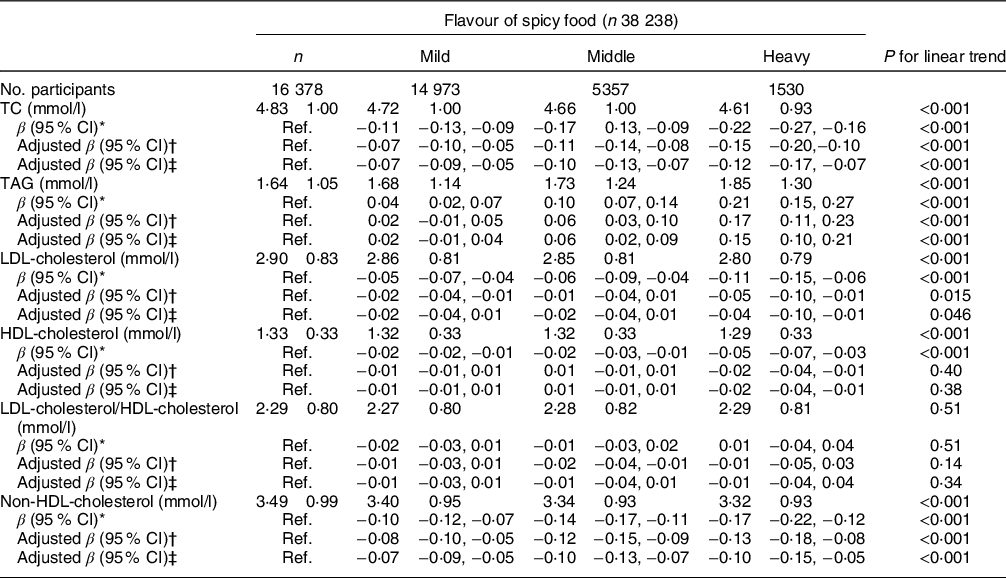
TC, total cholesterol; Ref, reference.
* Model 1: original model without any adjustments.
† Model 2: adjusted for age, gender, education level, marital status, smoking status, alcohol drinking, physical activity and BMI.
‡ Model 3: additionally adjusted for total energy intake based on model 2.
Table 3 Associations between spicy food intake frequency and blood lipid levels
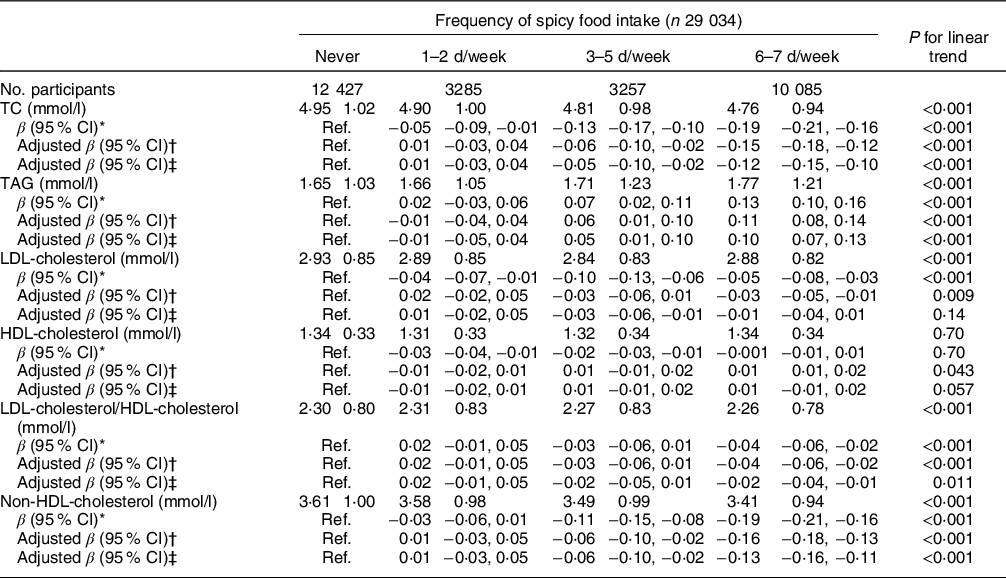
TC, total cholesterol; Ref, reference.
* Model 1: original model without any adjustments
† Model 2: adjusted for age, gender, education level, marital status, smoking status, alcohol drinking, physical activity and BMI.
‡ Model 3: additionally adjusted for total energy intake based on model 2.
The risk of abnormal serum lipid parameters according to the categories of spicy food flavour and intake frequency was further examined in Table 4. After adjusting for potential confounders, multivariate logistic regression analyses showed a significant inverse association between spicy food intake and high TC or non-HDL-cholesterol with elevated level of spicy flavour and frequency of spicy food intake (all P trend < 0·001); the adjusted OR were 0·91 (95 % CI 0·88, 0·93) and 0·88 (95 % CI 0·85, 0·91) for high TC and non-HDL-cholesterol as each level exposure increased in spicy flavour, and 0·92 (95 % CI 0·91, 0·94) and 0·91 (95 % CI 0·89, 0·93) for high TC and non-HDL-cholesterol as 1-d increment in spicy food intake frequency. On the contrary, compared with the reference, there were relatively increasing trends in the prevalence of abnormal TAG level with the elevated spicy flavour or intake frequency (both P trend < 0·001), but significant OR were only observed in middle flavour (by 1·10 (95 % CI 1·02, 1·17)), heavy flavour (by 1·21 (95 % CI 1·08, 1·35)) and who ate 6–7 d/week (by 1·16 (95 % CI 1·09,1·23)). Compared with those who did never eat spicy food, participants who ate spicy food 1–2 d/week significantly associated with increased risk of high LDL-cholesterol level (OR 1·10; 95 % CI 1·01, 1·21). In addition, the restricted cubic splines demonstrated that the risk of high TAG level increased smoothly with continuous spicy flavour level or intake frequency, whereas the risks of high TC and non-HDL-cholesterol decreased gradually with increasing spicy flavour level or intake frequency (Fig. 1) (all P for non-linear trend > 0·05).
Table 4 Multivariate adjusted OR (95 % CI) for abnormal lipid levels according to spicy food flavour and intake frequency*
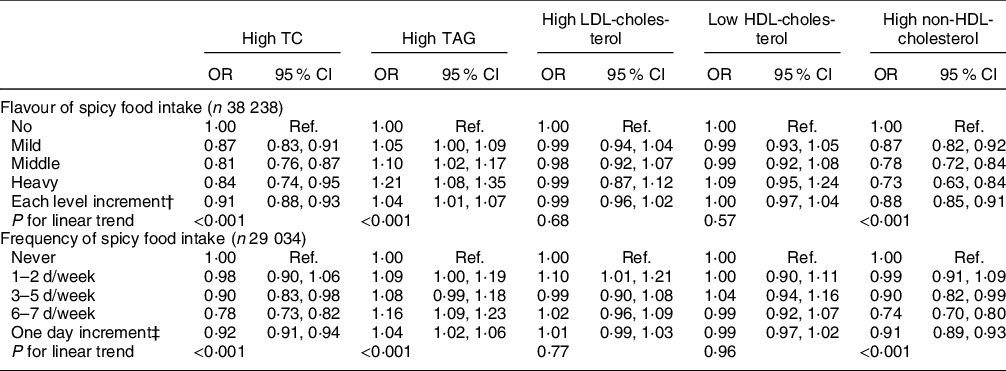
TC, total cholesterol; Ref, reference.
* Adjusted for age, gender, education level, marital status, smoking status, alcohol drinking, physical activity, BMI and total energy intake.
† Effect estimates of per level increment in spicy flavour levels on abnormal lipid levels.
‡ Effect estimates of per day increment in spicy food intake frequency on abnormal lipid levels.
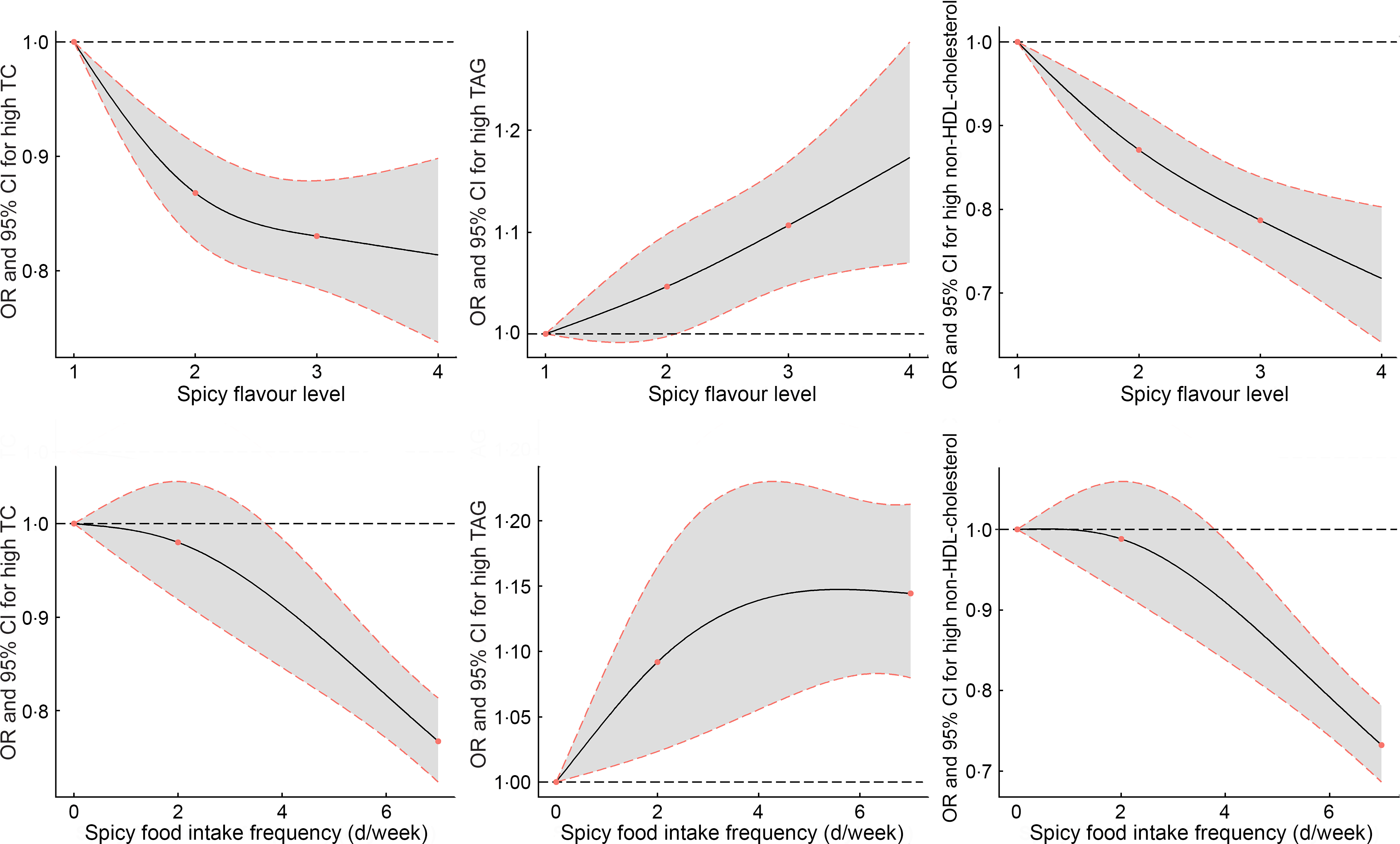
Fig. 1 Dose–response relationships between continuous spicy flavour level or intake frequency and risk for high TC, TAG and non-HDL-cholesterol were estimated by restricted cubic splines. Adjusted for age, gender, education level, marital status, smoking status, alcohol drinking, physical activity, BMI, total energy intake. TC, total cholesterol
The sensitivity analyses showed that associations of spicy food intake with serum lipid levels or abnormal lipid levels did not change appreciably after excluding participants with self-reported CHD and stroke, and additionally adjusting for dietary pattern and family history of hyperlipidaemia, CHD and stroke (online supplementary material, Supplemental Tables 1–4).
Discussion
To our knowledge, this is the first study by far based on large participant population to examine the associations between spicy flavoured food intake and serum lipid levels as well as risk of abnormal lipid levels. Most of the associations suggested beneficial effects of spicy food intake on blood lipid levels (i.e., associated with lower levels of TC, LDL-cholesterol, LDL-cholesterol/HDL-cholesterol, non-HDL-cholesterol and higher HDL-cholesterol levels), though mildly positive associations were detected for TAG levels in participants who had heavy flavours. However, consistent inverse associations were observed between lower risks of abnormal TC, non-HDL-cholesterol levels with elevated level of spicy flavour or frequency of spicy food intake in a dose–response manner.
Our findings on the beneficial association between spicy food intake and the risk of abnormal serum lipid are supported by many population studies as growing evidence indicates that spicy food intake frequency has been associated with obesity(Reference Shi, Riley and Taylor37), hypertension(Reference He, Wang and Tian38), total and certain cause-specific mortality in Chinese population(Reference Lv, Qi and Yu14) or in American(Reference Chopan and Littenberg20), all of which have showed health effects of spicy food consumption on reducing the risk of these chronic diseases. However, few previous studies have investigated the relation between spicy food intake and lipid levels in large population. Recently, two cross-sectional studies have investigated the association between spicy food consumption and lipid profiles in Chinese adults and older people. Xue et al. (Reference Xue, He and Yu24) have found that the frequency of spicy food consumption and the average amount of spicy food intake were inversely associated with LDL-cholesterol, LDL-cholesterol: HDL-cholesterol ratio and positively associated with serum TAG in adults. Yu et al. (Reference Yu, Xue and He25) have also demonstrated that the frequency of spicy food consumption exhibited significant inverse association with lipid parameters including serum LDL-cholesterol, LDL-cholesterol/HDL-cholesterol, LDL-cholesterol/apoB and apoB/apoA1 and was positively associated with apoA1 in older people in China. These findings are somewhat consistent with our results. Compared with these two studies, we have additionally found the inverse association between spicy food intake and non-HDL-cholesterol, which is considered as a more superior predictor than LDL-cholesterol in predicting the severity of coronary atherosclerosis and CVD risk estimation(Reference Moriyama and Takahashi39).
Although the mechanism between spicy food consumption and serum lipid levels is yet to be fully explored, many animal studies focused on Chili pepper and capsaicinoids, the major pungent ingredient in spicy food, have been found potential function on preventing and treating hypercholesterolaemia in cell cultures and animal models(Reference Liang, Tian and Chen40–Reference Chen, Jiao and Ma44). Liang et al. (Reference Liang, Tian and Chen40) reported that capsaicinoids can reduce plasma TC and non-HDL-cholesterol, which is consistent with our study. Capsaicinoids reduced the ratio of plasma campesterol/cholesterol, suggesting that they decreased cholesterol absorption. Zhang et al. (Reference Zhang, Zhou and Fang41) study also found capsaicinoids significantly decreased the plasma TC, LDL-cholesterol and TAG without affecting the HDL-cholesterol in ovariectomised rats. One mechanism underlying the cholesterol-lowering activity of capsaicinoids is that they can stimulate faecal excretion of bile acids. When capsaicinoids were supplemented at a dosage mimicking its regular intake in humans, they significantly reduced blood TC and LDL-cholesterol in hamsters and ovariectomised female rats via upregulating hepatic CYP7A1 gene expression(Reference Zhang, Zhou and Fang41).
In many animal studies, spicy food and its main bioactive ingredients, capsaicinoids, showed TAG-lowering properties(Reference Liang, Tian and Chen40,Reference Zhang, Zhou and Fang41) . But in this large human study, spicy food intake was mildly associated with elevated TAG level. Interestingly, this result was consistent with China Health and Nutrition Survey study(Reference Xue, He and Yu24), which also found the frequency of spicy food consumption and the average amount of spicy food intake were positively associated with serum TAG concentration. There are some potential explanations for the findings different from animal studies. A traditional Asian diet is characterised by higher carbohydrate intake, in contrast with meat-based Western diet. High carbohydrate intake from starchy foods was positively linked with the risk of dyslipidaemia along with increased TAG and reduced HDL-cholesterol levels in the Asian population(Reference Song, Paik and Park10,Reference Feng, Du and Chen45) , so different from those in the USA and Europe, the main types of dyslipidaemias in Asian countries including China manifest as hypertriglyceridaemia and low HDL-cholesterol(Reference Liu, Yu and Mao46). Moreover, the flavour and properties of spices make them important for culinary uses, namely as flavouring agents, colouring agents and preservatives in processed meat in Chinese culinary culture; some evidence indicated that spicy food may increase intakes of carbohydrates, meat with heavy salt or oil, sweet food and beverages to relieve the hot stimulation(Reference Janssens, Hursel and Westerterp-Plantenga16,Reference Sun, Lv and Chen22) . As we previously reported, spicy flavour and spicy food frequency were positively associated with general obesity(Reference Yang, Li and Mao28), which is consistent with the findings in the CKB study(Reference Li, Cui and Jin19). In this regard, excessive carbohydrates, fat and oil intake with spicy food may also increase the risk of abnormal TAG levels. Although the total energy intake (carbohydrate, fat and protein) and dietary pattern have been adjusted in the current study, these mild significant associations still were observed. Because some unmeasured factors such as sweet food intake and beverages cannot be exactly controlled, further study is needed to explore the potential association between spicy food intake and TAG levels.
To the best of our knowledge, this is by far the largest human study to investigate the association between spicy food intake and serum lipid levels in Chinese rural population. The strengths of the current study included a large sample size and available information on a broad range of covariates. Furthermore, the large-scale study population is unique, in resource-limited setting that dyslipidaemia was common with low awareness, treatment and control rates(Reference Liu, Yu and Mao46), which help provide some new evidence in the identification risk factors of the dyslipidaemia and prevention of CVD, especially in low- and middle-income countries like China. Inevitably, there are some limitations in our study. First, the current study was a cross-sectional design, which was unable to reveal a causal association. Second, the information on demographic data, lifestyles and dietary habits was collected by a questionnaire; thus, there may exist recall bias. Third, we did not consider participants who took lipid-lowering drug in the definition of lipid abnormality, which might partially bias our estimates. Fourth, the Henan Rural Cohort Study is not a nutritional survey, although we have collected for many potential confounders, some other unmeasured dietary factors such as chilli and sweet food intake, which were difficult to be accurately assessed by individual dietary recall, because those left in the residue of food was uncertain. In addition, we could not distinguish various food spices such as red chilli, black pepper and garlic, which might limit our study to some extent. Fifth, we did not take into account the survey complex sampling structure with stratification, cluster and sampling weights in our analysis, which may lead to a certain degree of bias. However, given the large sample size and enough number of primary units, there may be a quite limited effect of the sampling plan on variances of estimates (and the P-values). Therefore, the results based on this relatively large rural cross-sectional study, to some extent, could reflect the association of spicy food intake with blood lipid levels in Chinese rural areas. Finally, although the assessment of dietary intake according to the FFQ in current study may be inferior to three consecutive 24-h diaries in some nutrition surveys, which is a common problem with large epidemiological studies, the standardised FFQ has been validated using three consecutive 24-h dietary recalls. It could be used as a representative tool to conduct a dietary evaluation of a rural population and ensure the relatively reliable results(Reference Xue, He and Yu24).
Conclusion
Our findings firstly found that spicy flavoured food intake is associated with altered lipid levels and the risk of abnormal lipid levels in Chinese rural population. Although spicy food was mildly associated with increased TAG level, most of the associations showed favourable effects on blood lipid markers. This suggests that spicy food intake may be contributed to the management of lipid levels and CVD.
Acknowledgements
Acknowledgements: The authors thank all of the participants, coordinators and administrators for their support and help during the research. Financial support: This research was supported by the Foundation of National Key Program of Research and Development of China (grant no: 2016YFC0900803), National Natural Science Foundation of China (grant no: 81573243), Science and Technology Innovation Team Support Plan of Colleges and Universities in Henan Province (grant no: 21IRTSTHN029), Foundation of Medical Science and Technology of Henan province (no: 201702367, 2017T02098), Discipline Key Research and Development Program of Zhengzhou University (grant no: XKZDQY202008, XKZDQY202002). The funders had no role in the study design, data collection and analysis, decision to publish or preparation of the manuscript. Conflicts of interest: There are no conflicts of interest. Authorship: C.W. conceived and designed the study. X.D., Y.L., K.Y., L.Z., Y.X., S.Y., Y.W., D.Q., X.L., Z.L. and W.L. coordinated data collection. X.D., Y.L., X.L. and .R.T. conducted the analyses. X.D. and Y.L. wrote the manuscript. All authors read and approved the final manuscript. Ethics of human subject participation: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Ethics approval was obtained from the ‘Zhengzhou University Life Science Ethics Committee’, and written informed consent was obtained for all participants. Ethic approval code: [2015] MEC (S128).
Supplementary material
For supplementary material accompanying this paper visit https://doi.org/10.1017/S1368980021001853










