2018 US estimates suggest that over 20 million people over the age of 12 years had an alcohol or substance use disorder (SUD)(1). Moreover, the opioid crisis has reached epidemic proportions, with nearly a half million people dying from a drug-related overdose between 2000 and 2014 in the USA(Reference Rudd, Aleshire and Zibbell2). The Affordable Care Act of 2010 expanded Medicaid coverage as well as increased utilisation of private insurance for SUD(Reference Saloner, Antwi and Maclean3). Given that SUD is a chronic relapsing disease(Reference Dennis and Scott4), there is an urgent need for new approaches that improve delivery of treatment and enhance client self-management. Investigators have aimed to understand barriers in the implementation of evidence-based treatments such as medication-assisted treatment (MAT) and motivational interviewing in SUD(Reference Lundgren, Chassler and Amodeo5,Reference Lundgren, Amodeo and Chassler6) . Lack of preparation and hesitation of providers to adopt and implement science-based innovations can be due to (1) limited understanding of potential benefits; (2) insufficient resources or expertise and (3) lack of tolerance/patience necessary for full maturation of payoffs(Reference Simpson7). Other organisational change research has identified the need to reduce cynicism among employees through role modelling by transformational leaders(Reference Bommer, Rich and Rubin8).
The Texas Christian University Treatment Model(Reference Simpson9) and the Organizational Readiness for Change instrument(Reference Lehman, Greener and Simpson10) have been used to conceptualise and assess barriers involved in organisational change among SUD treatment programmes. It has been suggested that programmes with the most reluctance to change are often the ones which would benefit most from new innovations(Reference Simpson11). Roger’s Diffusion of Innovation Theory proposes that the spread of novel concepts in a social system is dependent upon communication channels which rely on human capital(Reference Rogers12). Stage-based approaches include training, adoption and implementation(Reference Simpson and Flynn13) which are influenced by staff attributes/attitudes, and levels of organisational stress(Reference Simpson11). Prior to organisational change, it is critical to increase staff readiness and capacity for collective action(Reference Foster-Fishman, Nowell and Yang14). Innovation is most likely to succeed when it involves expert facilitators leading to staff competence and self-confidence(Reference Kitson15,Reference Austin and Claassen16) . Studies have shown that cultural barriers should be overcome in order for new knowledge to successfully translate into alternative services(Reference Hernández-Mogollon, Cepeda-Carrión and Cegarra-Navarro17). Health promotion interventions require support (e.g. development of a wellness team) to increase capacity for sustainable change(Reference Saunders, Evans and Kenison18).
Organisational culture (as influenced from upper management) and low levels of staff skills have been identified as barriers to the adoption of wellness initiatives among SUD treatment centres in the USA, such as smoking cessation services(Reference Knudsen, Studts and Boyd19). Efforts to convert treatment centres into tobacco-free environments have had mixed success(Reference Jessup20). Traditionally, there exists a culture of ‘first things first’ in SUD treatment, which likely stems from Alcoholics Anonymous (originally published in 1939), suggesting that both smoking and sweets/candy can be helpful in early recovery. On the contrary, studies have shown that stopping smoking by the first year of sobriety positively predicts past-year abstinence(Reference Tsoh, Chi and Mertens21). The Addressing Tobacco through Organizational Change model includes on-site 3-d consultation with a trained expert and the formation of a leadership committee and tobacco work groups(Reference Ziedonis, Zammarelli and Seward22). Usage of the Addressing Tobacco through Organizational Change model has led to more favourable staff beliefs and client attitudes towards treating nicotine dependence and increased use of nicotine replacement therapy in residential treatment settings(Reference Guydish, Ziedonis and Tajima23). In a review of forty-eight empirical studies related to the implementation of smoking cessation in SUD treatment settings, it was suggested that successful organisational change should target local ‘champions’ (persons committed to the implementation process) to work with management on planning and carrying out necessary changes(Reference Knudsen24).
There has been an increasing interest in the role of nutrition in SUD recovery, although to date there are only a handful of intervention studies, using different outcome measures(Reference Sason, Adelson and Herzman-Harari25–Reference Wall-Bassett, Robinson and Knight31). Opioid and alcohol users can be considered at high nutritional risk(Reference Coulbault, Ritz and Vabret32,Reference Richardson and Wiest33) , yet most treatment centres do not offer any nutritional counselling or support(Reference Wiss, Schellenberger and Prelip34). It is well established that SUD is associated with poor nutritional status, including malnutrition, and various forms of disordered eating, reviewed elsewhere(Reference Wiss, Danovitch and Mooney35). Reports from Canada have shown that injection drug use is associated with food insufficiency and food insecurity(Reference Werb, Kerr and Zhang36–Reference Strike, Rudzinski and Patterson38). It is common for individuals in early recovery to report gastrointestinal distress(Reference Leppert39) and a strong preference for highly palatable foods low in fibre and nutrients(Reference Hardy, Fani and Jovanovic40). Poor intake of nutrients like n-3 and dietary fibre has been linked to aggression and overall compromised mental health(Reference Meyer, Byrne and Collier41,Reference Ramin, Mysz and Meyer42) . A recent systematic review and meta-analysis has shown that dietary improvement can reduce depressive symptoms, likely modulated by gastrointestinal microbiota(Reference Firth, Marx and Dash43).
A recent survey showed that less than a third of SUD treatment centres in Los Angeles offer any nutrition services(Reference Wiss, Schellenberger and Prelip34). Some authors have suggested that individualised nutrition interventions may improve opioid treatment outcomes(Reference Cunningham44), yet the role of nutrition in SUD recovery remains understudied. Topics for educational groups in treatment settings have been proposed(Reference Wiss, Schellenberger and Prelip45), and it has been shown that hands-on nutrition and culinary interventions can be done in small residential settings where there are financial constraints(Reference Wall-Bassett, Robinson and Knight31,Reference Moore, Gray and Wiss46) . Considering the growing interest in developing nutrition-related programming for SUD, more research about programme design and implementation is warranted. To date, there are no studies assessing perceived barriers to nutrition-related organisational change in SUD treatment. Exploratory research on staff concerns/attitudes towards provision of novel nutrition interventions may inform future efforts to improve food service environments in SUD treatment centres.
The aim of the current study is to describe staff-reported barriers to organisational change involving implementation of a nutrition program in a setting where the majority of clients’ treatment is publicly funded. Given that nutrition interventions in SUD treatment have been poorly described, very little is known about staff attitudes about nutrition, as well as perceived/actual barriers to institutional change, before and after facility-wide modification. This will be the first study to describe potential barriers to nutrition changes in a multisite non-profit SUD treatment centre. Given the biological plausibility that improving nutrition in early recovery has the potential to improve mental health and overall chances of recovery, the study of barriers to making nutrition-related changes can help to inform future intervention work.
Methods
Facility characteristic
Janus of Santa Cruz (JSC) is a non-profit SUD treatment centre in Northern California that primarily serves Medicaid beneficiaries. Their facilities include several levels of care: Driving Under the Influence services, Intensive Outpatient services, Withdrawal Management (in-patient) and Residential Treatment (with a separate Perinatal Unit for mothers and their custodial children 0–5 years of age), MAT, Sobering Center (short-term jail alternative), Lighthouse Counseling (outpatient therapy), Family Programs and sober living environments. Prior to the conception of the study, JSC received two grants that supported policy and procedural changes, staff training and the implementation of additional practices to support multidimensional wellness during recovery from SUD, including a focus on nutrition. The objectives for JSC organisational changes related to the current study are two-fold: first is the implementation of a customised nutrition curriculum for individuals in SUD treatment, including menu changes; and second is to stimulate change of organisational culture through diffusing new information to staff and clients linking nutrition to both physical and mental health. The broader summary of the nutrition intervention at JSC is described in Fig. 1.

Fig. 1 Logic model for nutrition intervention in substance use disorder treatment
There are approximately 150 staff members at JSC. Baseline characteristics (collected in March 2019 by the human resource department) are: 49 % white, 36 % Hispanic, 10 % mixed, 5 % other; 62 % female; 49 % millennials, 28 % generation X, 23 % baby boomers; 80 % paid hourly (v. salary). There was high staff turnover (34 %) between March and November 2019 during which time the organisational changes began, which is not uncommon in treatment settings. November 2019 staff characteristics are similar with respect to ethnicity and gender but there was a slight increase in millennials (56 %) relative to other generational groupings. Demographic characteristics were not collected due to anonymity concerns; we report this data as an overall description of facility staff but not our final analytic sample.
Description of intervention
A consultant registered dietitian nutritionist (RDN) made site visits in March 2019 to meet with key staff, join the newly formed ‘wellness team’ and conduct a needs assessment on the food service operation. The official beginning of the facility-wide changes was marked by a half-day staff training, where the RDN presented emerging research related to ‘nutrition and mental health’ to the twenty JSC employees in attendance. The RDN facilitated an additional meeting for those staff (less than half) who expressed interest in facilitating nutrition groups (i.e. delivering content to JSC clients in the form of lecture, discussion/activity and hands-on skill building). Electronic curriculum was transferred to JSC, and staff ‘champions’ were identified to take the lead on delivering nutrition education. A separate meeting with two members of the food service team led to several recommendations related to increasing the fibre content of foods served (e.g. fruits, vegetables, whole grains, beans, nuts and seeds) and ways to increase their acceptability, designed to match the content of the curriculum. The RDN conducted a 1 h group with clients at the main residential campus which also included residents from the perinatal unit, intended to prepare them for new menu items and nutrition groups.
A second site visit took place in July 2019, with the goals to (1) discuss successes and challenges; (2) provide additional training to staff on self-care and role modelling; (3) educate staff on how to detect co-occurring eating disorder and use sensitive language about weight and diet; (4) empower staff to encourage self-care with their clients while staying in their scope of practice; (5) deliver additional curriculum content for use at the main campus and perinatal unit; (6) provide perinatal-specific nutrition curriculum and recommendations for community involvement in the construction of a grocery list at the perinatal unit and (7) provide a summary report of recommended facility-wide changes. The RDN also conducted a group with the clients to inform them to the ‘why’ nutrition-related changes were happening, and upcoming changes to expect. Since the initiative began in March 2019, the wellness team continued to meet every 2 weeks to discuss: tobacco cessation, nutrition programme, stress reduction, physical activity and other health-promoting recreational activities.
Recruitment, data collection and analysis
Study participants were recruited through verbal announcements at staff meetings, direct communication with supervisors and internal email communications. The pre-intervention questionnaire was administered at the beginning of the initial staff meeting (March 2019) before the ‘nutrition for mental health’ lecture conducted by the RDN. Completing the questionnaire was voluntary. It contained no identifiable information and was distributed after the study information sheet was read and understood. Attendees at the meeting who consented to complete the questionnaire were given adequate space and time to answer the questions in privacy. Any staff member who did not feel that their privacy was maintained was given the option to not participate. Twenty staff members completed the questionnaire, and over the course of the next 2 days, twenty additional questionnaires were collected from staff unable to attend the meeting through an anonymous online platform (Survey Monkey) with no identifiers (total pretest n 40).
The questionnaire was created specifically for this project because no tool to assess nutrition-related concerns in SUD treatment settings has been previously created or validated. The questions were designed to assess barriers related to the current intervention as well as potential future work, with four questions for each of the five domains: (1) provision of nutrition-related treatment; (2) implementation of nutrition education; (3) screening, detecting and monitoring; (4) facility-wide collaboration and (5) menu changes and client satisfaction. Domain scores were created using the means of the individual questions within that domain, separated by pre and post. Cronbach’s α was used to evaluate internal consistency of the items within each domain, analysed separately by pre and post.
A five-point Likert scale was used to indicate the extent to which staff anticipate difficulty or ease in implementing facility-wide nutrition changes, perceived as organisational barriers: (1) very easy to implement; (2) somewhat easy to implement; (3) neither easy nor difficult to implement; (4) somewhat difficult to implement and (5) very difficult to implement. Seven additional questions on nutrition-related attitudes were also assessed on a Likert scale: (1) strongly disagree; (2) somewhat disagree; (3) neither agree nor disagree; (4) somewhat agree and (5) strongly agree. An open-ended question was included: ‘what do you anticipate will be the greatest benefit of implementing facility-wide nutrition changes?’ Participants were also asked to identify the departments where they work.
The follow-up questionnaire (total post-test n 50) was administered between October and December 2019, 3 months after the second site visit and once implementation had commenced. This post-test was administered through the anonymous online platform and was identical to the pre-test with the exception of changed language from ‘anticipate’ (future tense) to ‘experienced’ (past tense). All quantitative analysis was conducted using STATA version 16(47), and statistical significance was set at P = 0·05 for two-tailed t tests for analysing differences pre and post. Sensitivity analysis for missing data was conducted.
Results
Table 1 shows the different departmental affiliations at pre and post. The proportion of respondents from the main campus nearly doubled by post-test (P = 0·03) which may be attributed to the fact that the post-test was exclusively electronic, several reminders were given, and managers were incentivised to encourage staff to complete the questionnaire. Respondents from the MAT clinic south dropped significantly between pre and post (P = 0·005), which may have been because many MAT counsellors felt it was not relevant to them since they do not have opportunity to discuss nutrition with clients and the MAT clinic does not serve food (data not shown). Other differences by department affiliation of respondents were not significant.
Table 1 Staff department affiliations
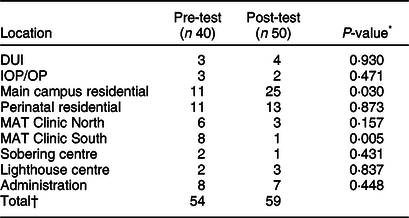
DUI, driving under the influence; IOP, intensive outpatient; OP, outpatient; MAT, medication-assisted treatment.
* Two-tailed t test.
† Totals higher because some employees are at multiple locations.
Staff who were unsure how to answer the question were instructed to leave the question blank. Seventy-four percentage of respondents answered all questions (90 % of staff on the pre-intervention questionnaire, and only 62 % of the post-intervention). Missingness for each question ranged from 2·2 to 12·2 % when combining pre and post (n 90). For example, on the follow-up survey, 20 % (10/50) staff skipped the question related to budgeting for new healthful menu items (q14, Table 2). For sensitivity analysis, mean values were imputed for all missing data and all tests were rerun; it was found that mean imputation did not change the significance of any of our results reported in Table 2 (data not shown). Therefore, our final analysis drops missing data.
Table 2 Staff-perceived barriers to change before and after nutrition-focused wellness initiative
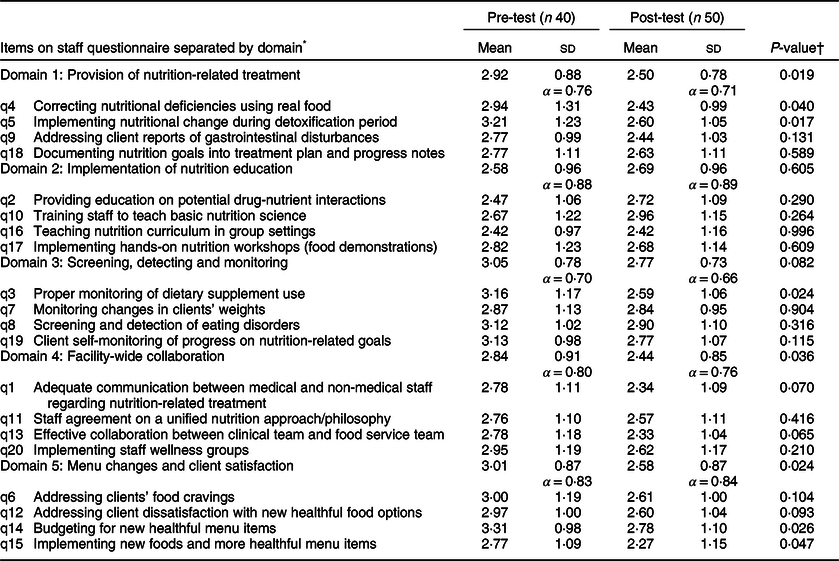
* Means reported from scores regarding implementation on Likert scale: (1) Very easy; (2) Somewhat easy; (3) Neither easy nor difficult; (4) Somewhat difficult and (5) Very difficult.
† Two-tailed t test.
Table 2 summarises our main findings. t Tests were conducted for individual questions as well as for each of the domains. Cronbach’s α demonstrates that all domains belong together based on α ≥ 0·70(Reference Tavakol and Dennick48); however, the post-test for Domain 3 fell just below our threshold (α = 0·66). Domain 1 suggests that perceived barriers related to the provision of nutrition-related treatment decreased from pre to post (P = 0·019). Two of the individual items (q4 and q5, discussed below) were significant in their increase of ease in implementation from before to after organisational change. The difference between pre-test and post-test means for Domain 2 (implementation of nutrition education) was not significant, but it is worth mentioning that it was the only domain to show higher levels of perceived difficulty from pre to post (discussed below). The difference between pre-test and post-test means for Domain 3 (screening, detecting and monitoring) was not significant, but one of the individual items (q3) showed an increase in ease of implementation pre and post (discussed below). The difference between means for Domain 4 (facility-wide collaboration) suggests that perceived barriers related to facility-wide collaboration decreased from pre to post (P = 0·036). None of the individual items was significant, although two of them (q1 and q13) trended towards significance. Data for Domain 5 (menu changes and client satisfaction) suggest that perceived barriers related to menu changes and client satisfaction decreased from pre to post (P = 0·024). Two of the individual items (q14 and q15, discussed below) were significant in their increase of ease in implementation before and after organisational change.
Table 3 summarises the baseline nutrition attitudes at pre-intervention comparing staff members attending training v. those who did not, conducted post hoc. One of the questions (q27) about whether or not ‘investing time and money into nutrition is a waste of precious resources’ had higher levels of disagreement among those who attended training (P = 0·001). While the training was designed to be mandatory for clinical staff, it was difficult to enforce and it is clear that those who attended the training had different attitudes about nutrition compared with those who did not. We found this to be important because in the context of organisational change, the twenty staff members who showed up for the ‘nutrition for mental health’ lecture included our ‘champions’ and those responsible for diffusing these new innovations. This group (in theory) became the vehicle for dissemination and implementation. In other words, our data suggest that the twenty people who attended training may have been valuable as ‘human capital’ in the context of facility-wide nutrition change. Of course, some staff are needed for client care even during mandatory trainings; therefore, those who could not attend were asked to view the recording.
Table 3 Baseline nutrition attitudes by attendance at training*

* Means reported from scores on Likert scale: (1) Strongly disagree; (2) Somewhat disagree; (3) Neither agree nor disagree; (4) Somewhat agree and (5) Strongly agree.
† Two-tailed t test.
Table 4 summarises findings from the qualitative portion of our questionnaire, with verbatim responses to illustrate each theme. We did not observe major thematic changes from pre to post. At baseline staff anticipated the following thematic benefits: (1) improved overall health (‘feel better’); (2) improved brain health and recovery from SUD and co-occurring disorders (‘better cognition’ and ‘emotional stability’); (3) improved understanding and behaviours related to nutrition (‘knowing that we are reaching the highest standards for the clients’) and (4) improved staff health (‘we lead by example’). At post-test, there did appear to more specific knowledge about brain health (‘repair motivation/reward networks’ and ‘restoring good brain activity’) as well as evidence of implementation at the perinatal unit (‘I have heard more talks and discussions from staff and clients. Every week the day after they do the group they talk about what they learned the grocery list has also reflected what they are learning’). Another theme we identified at post-test was ‘access to healthy foods’ where we found more evidence of programme implementation facility-wide (‘people are getting the opportunity to receive healthy food and address a lot of nutritional deficiencies’).
Table 4 Thematic analysis of staff survey responses about anticipated (pre-test) or observed (post-test) greatest benefits of facility-wide nutrition changes (illustrative verbatim responses)

Discussion
Our results show that staff training, food service changes, the use of targeted curriculum for nutrition groups and the encouragement of ‘self-care’ discussion in individual counselling sessions can lead to positive changes about perceived barriers to nutrition-related organisational change among staff. Specifically, staff reported an increase in the ease of addressing nutritional deficiencies using real food and implementing nutritional change during detoxification period, both of which were part of the domain provision of nutrition-related treatment. Increasing collective efficacy about discussing nutrition with clients at JSC might explain these changes. Based on our open-ended questions, it appears that some of the staff were aware that nutrition can lead to ‘positive cognitive change’; however, there are concerns about staying within their scope of practice (data generated from discussion at staff trainings). Our results suggest that organisational change including ‘permission’ to encourage healthful eating (given during staff trainings) can change perception of difficulties in providing nutrition-related treatment.
The staff reported a perceived increase in the ease of implementation of monitoring dietary supplement use; however, the overall domain of screening, detecting and monitoring was not statistically significant, suggesting that the staff perceived low capacity for detecting other changes (e.g. weight status and eating disorder behaviour). It is worth noting that the increase in ease of monitoring supplement use is likely confounded by the requirement for medication counts and discussions among management about the feasibility of continuing to include supplements in those medication counts. Therefore, we interpret these findings with caution. Supplements that were discussed in staff training include multivitamins, n-3 and probiotics; however, these are not typically covered by insurance therefore not implemented facility-wide (B-vitamins are often prescribed by medical staff). Given that SUD have been linked to malnutrition including low levels of micronutrients(Reference Islam, Hossain and Ahsan49–Reference Ross, Wilson and Banks52), multivitamins are common practice in hospital-based detoxification programmes. n-3 in the form of fish oil has been linked to decreased impulsivity and aggression; however, the data linking n-3 to SUD are limited(Reference Bozzatello, Brignolo and Grandi53). Probiotics have shown efficacy in reducing depression, and possibly anxiety(Reference Smith, Greene and Babu54), and have shown promise in the treatment of alcoholic liver disease(Reference Hong, Han and Hong55). Nutrition guidelines including supplement recommendations for different classes of substances have recently been published(Reference Wiss, Danovitch and Mooney35).
The overall domain of facility-wide collaboration was perceived to be easier after intervention; however, none of the individual items was statistically significant. This particular domain appears important based on the published literature, which suggests that identified transformational leaders should work across disciplines and with management in order to effectively carry out changes(Reference Bommer, Rich and Rubin8,Reference Knudsen24) . The domain of ‘menu changes and client satisfaction’ significantly increased in perceived ease of implementation pre and post. Specifically, budgeting for new healthful items and implementing new foods and more healthful menu items were both perceived as easier to implement after the first few months of intervention. This domain is important since client satisfaction with the food appears to be a major barrier. The culture of ‘first things first’ which emphasises client ‘wants’ with respect to food over their long-term health ‘needs’ with respect to health is likely to be challenging trade-offs in future nutrition interventions in SUD settings.
Last, while the domain implementation of nutrition education and all of the items in that domain failed to reach statistical significance, this is the only domain that actually decreased in perceived ease of implementation. This could be related to the difficulty finding qualified staff to teach the nutrition education lessons. In other words, staff reported feeling under-prepared to deliver content. There was also a delay in getting larger televisions to use for the education materials, and the loss of a ‘champion’ staff member who was trained to conduct these groups. It does appear that the job of conducting nutrition education groups would be best filled by an RDN, but unless insurance covers dietitian services in SUD settings, it is unreasonable to expect SUD facilities to have such capacity. A recent article describing the potential role of the RDN in treatment settings has been published(Reference Wiss, Schellenberger and Prelip45). The current study highlights barriers to implementation of nutrition education that may be useful for future intervention studies, where clearly more data are needed.
Limitations and conclusions
The findings of this analysis should be viewed in light of its limitations. To begin, our data were not paired which means our samples were not identical pre and post. Given the amount of staff turnover in these settings, we aimed to capture organisational characteristics rather than individual level data; however, our unmatched samples might have biased our findings. Since the survey was voluntary and staff was not randomly selected, there is potential for selection bias. This approach was our only viable option as this work was conducted in a real-world setting. There was inconsistent implementation of organisational change across the different sites. We had more post-test respondents at the sites where most of the changes took place. There was also more missing data at post-test which may have come from newly hired staff unsure how to answer certain questions. Because of potential anonymity concerns, we did not collect demographic data from staff, which limited our ability to analyse differences by other characteristics, such as age and gender. While the instruments we used was informally pretested, it was created specifically for this research purpose and has not been formally validated.
Despite these limitations, strength of our study is the relatively large size of the facility across its multiple sites. This permitted sufficient power for analysis of staff perceptions before and after organisational change. This is the first study to describe nutrition changes in a large non-profit SUD treatment centre. Despite known barriers to organisational change in SUD settings, nutrition interventions can be implemented and we have provided evidence that some staff-perceived barriers can decrease following organisational change. Specifically, barriers related to providing nutrition-related treatment, collaborating facility-wide and menu changes and client satisfaction all decreased following the wellness initiative. Our description of staff concerns/attitudes towards provision of novel nutrition interventions may inform future efforts to improve food service environments and teach nutrition classes in SUD treatment centres.
Given emerging evidence in the domain of nutritional psychiatry, improving nutrition in early recovery has the potential to improve mental health and overall chances of recovery, although to date there is limited support. Vulnerable populations including those who are food insecure need more attention amidst the addiction crisis. Addressing nutrition-related concerns may be of significant value to both physical and mental health. Empowering staff members as ‘champions’ to lead by example appears critical for diffusion of new knowledge in SUD settings. Future research should examine client barriers as well as satisfaction with nutrition-related changes, in both public and private treatment settings. In addition to documenting changes in biomarkers related to micronutrient status and inflammatory markers, intervention studies should assess changes in depressive symptoms, anxiety, body image, disordered eating, food addiction, self-efficacy with shopping/cooking, and over longer periods of time, abstinence from alcohol and drugs. Nutrition interventions can also be an important part of harm reduction approaches aimed at decreasing food insecurity and increasing quality of life in those who are not abstinent. Overlooking the importance of food in SUD treatment contexts may be a missed opportunity for public health.
Acknowledgements
Acknowledgements: Not applicable. Financial support: The authors would like to recognise sources of financial support for nutrition programme activities: SAMHSA CSAT Residential Treatment for Pregnant and Postpartum Women Grant (En Junto: Mamas y Familias) and California Tobacco Control Program Behavioral Health and Wellness Grant (Janus Tobacco Project). The views of the authors do not necessarily represent those of the funding agencies. Funding agencies had no role in the design, analysis or writing of this article. Conflict of interest: D.A.W. is the founder and owner of Nutrition in Recovery LLC which provides nutrition services to substance use disorder treatment facilities. Such services (e.g. staff training) were rendered to Janus of Santa Cruz during the time this study was conducted. Authorship: All authors participated in the conception of the study and contributed to the final manuscript. D.A.W. formulated the research question and design of the study, L.R. helped with the data collection and M.P. oversaw the project. Ethics of human subject participation: This study was conducted according to the guidelines laid down in the Declaration of Helsinki, and all procedures involving study participants were approved by the Institutional Review Board at the University of California Los Angeles. Written informed consent was obtained from all subjects.










