Introduction
According to Crangle (Reference Crangle2010), approximately 500 million people worldwide refuse to fly in an aeroplane, and an even greater number will accept to fly despite experiencing fear. Fear of flying (FoF), also known as aviophobia, is a common psychological condition that affects many individuals. In addition to those diagnosed with FoF, an even larger proportion of the population is either undiagnosed or apprehensive about flying. Multiple studies indicate that 50% of the population exhibit FoF associated with an undiagnosed phobia (Evangelisti, Reference Evangelisti2008; Van Gerwen et al., Reference Van Gerwen, Diekstra, Arondeus and Wolfger2004). The prevalence of aviophobia in the western population is estimated to range from 7 to 40%, with 3% of those affected admitting dependence on alcohol and anxiolytics as their coping strategies (Thompson and Craven, Reference Thompson and Craven2017).
The Diagnostic and Statistical Manual of Mental Disorders (DSM-5) defines FoF as an ‘intense fear or anxiety about flying situations’ (American Psychiatric Association, 2013). Within the framework of this particular situational phobia, there might be various feared agents associated with the act of being on a plane: seeing an aircraft fly, preparing the suitcases, risk of accident that may result in injury or death, being locked in a confined space, erratic movements of the plane, altitude, the sensation of lack of control, panic attack or leaving others unprotected (e.g. young children) in the event of death (Bados López, Reference Bados López2017; Quero et al., Reference Quero, Botella, Guillen, Molés, Nebot, García-Palacios and Baños2012).
Different treatments have been proposed due to the high prevalence and debilitating effects of this disorder. In the 1990s, the treatment of FoF through virtual reality (VR) was studied for the first time (North and North, Reference North and North1994). In vivo exposure therapy (IVET) has proven to be an effective psychological treatment for specific phobias, such as aviophobia. Although there is empirical evidence for the efficacy of exposure therapy, IVET tends to be more expensive (renting or buying a plane ticket) than virtual reality exposure treatment (VRET) (Botella et al., Reference Botella, Fernández-Álvarez and Guillén2017). Apart from that, some studies have found that therapists may be reluctant to provide exposure-based interventions because patients reported that VRET is perceived as more acceptable, helpful and ethical than in vivo exposure-based therapy (Boeldt et al., Reference Boeldt, McMahon, McFaul and Greenleaf2019; García-Palacios et al., Reference García-Palacios, Hoffman, Kwong See, Tsai and Botella2001; Richard and Gloster, Reference Richard and Gloster2007). In fact, IVET could interfere with some ethical considerations as it intentionally evokes anxiety in people, raising ethical issues over its tolerability and humaneness (Olatunji et al., Reference Olatunji, Deacon and Abramowitz2009; Wolitzky-Taylor et al., Reference Wolitzky-Taylor, Viar-Paxton and Olatunji2012). In addition to these disadvantages, there are other issues associated with the individuals’ motivation to implement an appropriate cooperation. It is worth noting that only 7.8% of phobia sufferers seek treatment (MacKenzie et al., Reference Mackenzie, Reynolds, Cairney, Streiner and Sareen2012) and merely 0.8% receive a specific treatment for this disorder (Stinson et al., Reference Stinson, Dawson, Chou, Smith, Goldstein, Ruan and Grant2007). This may be due to long waiting lists or the fact that many therapists do not receive training to administer exposure therapy (Kazdin, Reference Kazdin2015; Kazdin and Blase, Reference Kazdin and Blase2011; Kazdin and Rabbitt, Reference Kazdin and Rabbitt2013).
Over the past several decades, VRET has been gaining popularity becoming an alternative to IVET for FoF (Powers and Emmelkamp, Reference Powers and Emmelkamp2008). Although no clinically significant differences have been demonstrated between VRET and IVET (Morina et al., Reference Morina, Ijntema, Meyerbröker and Emmelkamp2015), it seems that VRET provides better accessibility to the feared stimuli, receives more acceptance among patients compared with other cognitive behavioural interventions and generally results in a lower drop-out rate (Clark et al., Reference Clark, Mayers and Sosa2019). VRET may be cost-effective for both the clinician and the patient, it allows the therapist to perform exposure in the office rather than in vivo environments and, consequently, patients can be treated at the cost of a standard therapy hour as opposed to extended session periods. Besides, VR is conducted within the security and privacy of the therapist’s office offering more confidentiality (Rothbaum et al., Reference Rothbaum, Anderson, Zimand, Hodges, Lang and Wilson2006). Accordingly, it is recognised that offering VRET could contribute to the growth of patients who accept this therapy. In addition, VR offers the benefit that phobic objects and situations can be easily modified for therapeutic purposes. For instance, the therapist can control the type, intensity, duration and repetition of the element or situation to which the person is exposed (Maples-Keller et al., Reference Maples-Keller, Bunnell, Kim and Rothbaum2017) and also can use specific stimuli such as turbulence (Diemer et al., Reference Diemer, Pauli and Mühlberger2015). VR allows the expert to constantly consider what the patient is experiencing, facilitates the location of the relevant situational dimensions, and customises the exposure hierarchies to which the patient can be exposed. To a large extent, the activity is guided by the patients themselves, so it can favour the development of operational thinking by facilitating the exploration of different possibilities. The perceived stigmatisation generated in real situations might be avoided in a controlled VR environment, keeping the subject’s clinical characteristics private (Carl et al., Reference Carl, Stein, Levihn-Coon, Pogue, Rothbaum, Emmelkamp and Powers2019; Wiederhold and Bouchard, Reference Wiederhold and Bouchard2014). Overall, the VR approach for specific phobias could help to increase the number of people who seek exposure therapy, compared with in vivo exposure, providing high possibilities of even surpassing the same reality (Botella et al., Reference Botella, Fernández-Álvarez and Guillén2017; García-Palacios et al., Reference García-Palacios, Botella, Hoffman and Fabregat2007). Actually, when IVET is unavailable or not feasible, the German Clinical Practice Guideline for anxiety disorders recommends VRET for specific phobia (Bandelow et al., Reference Bandelow, Werner, Kopp, Rudolf, Wiltink and Beutel2022).
However, VR has some drawbacks compared with other exposure therapies. Firstly, employing new technologies means that the therapist must acquire specific skills to manipulate the internal and external devices to adapt to the patient’s needs (Bouchard et al., Reference Bouchard, Côté and Richard2007). Secondly, the peripheral components used in this type of intervention are usually expensive. Thirdly, patients may become addicted to the VR scenarios (Park et al., Reference Park, Kim, Lee, Na and Jeon2019). Lastly, there is the possibility that the immersion induces simulator sickness, which is defined as unpleasant adverse effects such as nausea, headache or dizziness, and it has been reported that approximately 5% of individuals immersed in a virtual environment experience significant side-effects (Lawson et al., Reference Lawson, Graeber, Mead, Muth and Stanney2002).
Although several systematic reviews and meta-analyses have been conducted to assess the efficacy of VRET for the treatment of anxiety disorders, as far as it is known, there is only one systematic review (Da Costa et al., Reference Da Costa, Sardinha and Nardi2008) and one meta-analysis (Cardoş et al., Reference Cardoş, David and David2017) focused on aviophobia. Given the specific characteristics of this kind of phobia (e.g. multiple feared agents associated with the act of flying) and considering that the previous systematic research was conducted almost 15 years ago, an update of published research evaluating the efficacy of VRET for FoF is needed. Furthermore, published studies show a wide variability of devices and softwares used for exposure, as well as the characteristics of the VRET setting. Therefore, a deeper review of technical and contextual factors associated with better VRET outputs may help clinicians to design better VR-based interventions.
Taking into consideration the aforementioned, this study aimed to systematically review the research published until December 2021 with four main objectives: (a) determining the efficacy of VRET for FoF, (b) evaluating the methodological quality of reviewed studies, (c) recognising which devices can contribute to the efficacy of VRET in terms of apparatus, virtual environments and sensory cues provided; and (d) distinguishing contextual factors that may have an effect on the efficacy of the VRET in order to determine the optimal setting (e.g. number of sessions, hardware systems, etc.).
Method
The articles included in this systematic review have been carefully selected under the Preferred Reporting Items for Systematic Reviews and Meta Analyses (PRISMA) guidelines, as it consists of an updated and standardised protocol within the scientific community to elaborate a systematic review (Shamseer et al., Reference Shamseer, Moher, Clarke, Ghersi, Liberati, Petticrew, Shekelle and Stewart2015). For the search of the information, three recognised platforms with a wide range of literature related to health, medicine and psychology were selected: PsycInfo, Medline and Web of Science. Although the keywords were modified according to the requirements of each database, the following terms in combination with the Boolean operators ‘AND’ and ‘OR’ were used for the search of scientific articles: (‘virtual environment’ OR ‘virtual reality’) AND (‘intervention’ OR ‘therapy’ OR ‘treatment’) AND (‘flying phobia’ OR ‘aviophobia’ OR ‘fear of flying’ OR ‘FoF’).
The search included papers published until December 2021 and the inclusion criteria were: (1) clinical or subclinical population with FoF, (2) assessment of the efficacy of VRET for the treatment of FoF, and (3) written in English or Spanish. Narrative literature reviews, protocols, congress papers, book chapters, doctoral dissertations and theoretical articles were excluded.
Inclusion and exclusion criteria of the searched papers were assessed by two reviewers (first and last authors). Titles and abstracts were first screened once the search was completed. After that, the full text of the eligible articles was sourced. Additional publications that might have been overlooked in the search, the reference lists of the selected articles, as well as previous systematic reviews were also examined. The reviewers then shared their conclusions on the information provided. In addition to the studies collected by the title and abstract, the complete texts of studies which seemed initially to meet the inclusion criteria were then independently reviewed and screened by the reviewers to determine their relevance. Through discussion and conclusive agreement, any discrepancies between the researchers were resolved.
Results
The search yielded 238 results, of which 137 were excluded as duplicates. Figure 1 depicts the procedure for adhering to PRISMA conventions as well as the reasons for excluding certain studies. After reviewing the titles and abstracts of the remaining articles, 54 papers were selected for inclusion. After a thorough examination of the full text, 33 studies met the inclusion criteria. Notably, the included studies have been conducted in a variety of countries, including Canada, Spain, the United States, Israel, France, Mexico, the Netherlands, Germany and Italy.
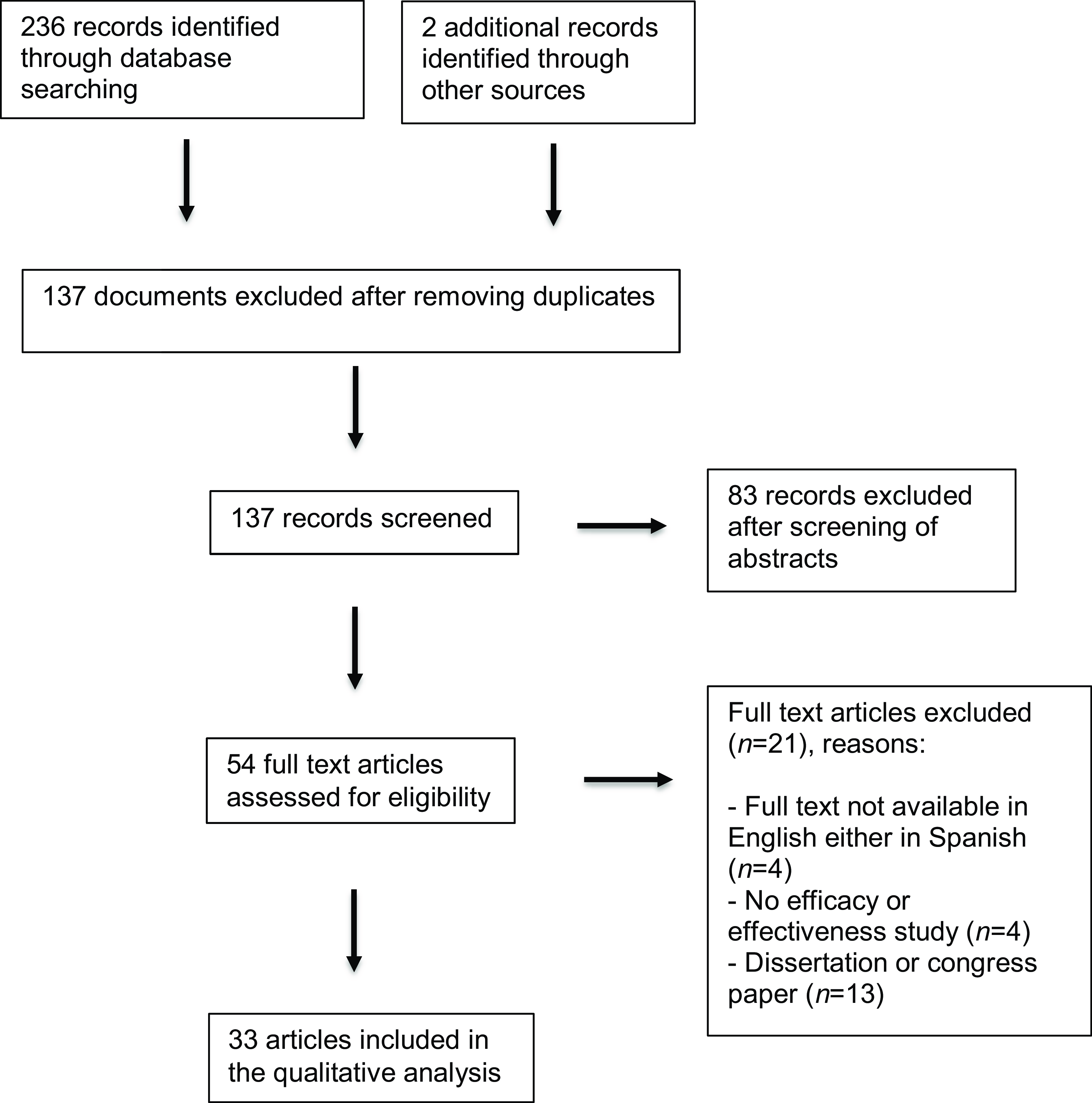
Figure 1. Systematic review flow chart following PRISMA guidelines (Moher et al., Reference Moher, Shamseer, Clarke, Ghersi, Liberati, Petticrew and Stewart2015).
As shown in Table 1, a total of eight case studies (1, 7, 10, 12, 13, 21, 22, 30), seventeen randomised controlled trials (RCTs) (6, 14, 15, 16, 17, 18, 19, 20, 23, 24, 25, 26, 27, 28, 31, 32, 33), and eight articles which used another type of design were examined: four multiple baseline designs (MBDs) (2, 3, 4, 5), two uncontrolled pre–post experiments (8, 29), one retrospective study (9), and one descriptive study (11). Some studies (9, 24, 33) merely followed up on previous studies or VRETs. All of them focused on VR considering either clinical, subclinical or both participant populations. The majority of studies presented experimental conditions comparing VRET with other treatments or waiting list groups (WL).
Table 1. Summary of studies on the application of virtual reality in individuals with FoF
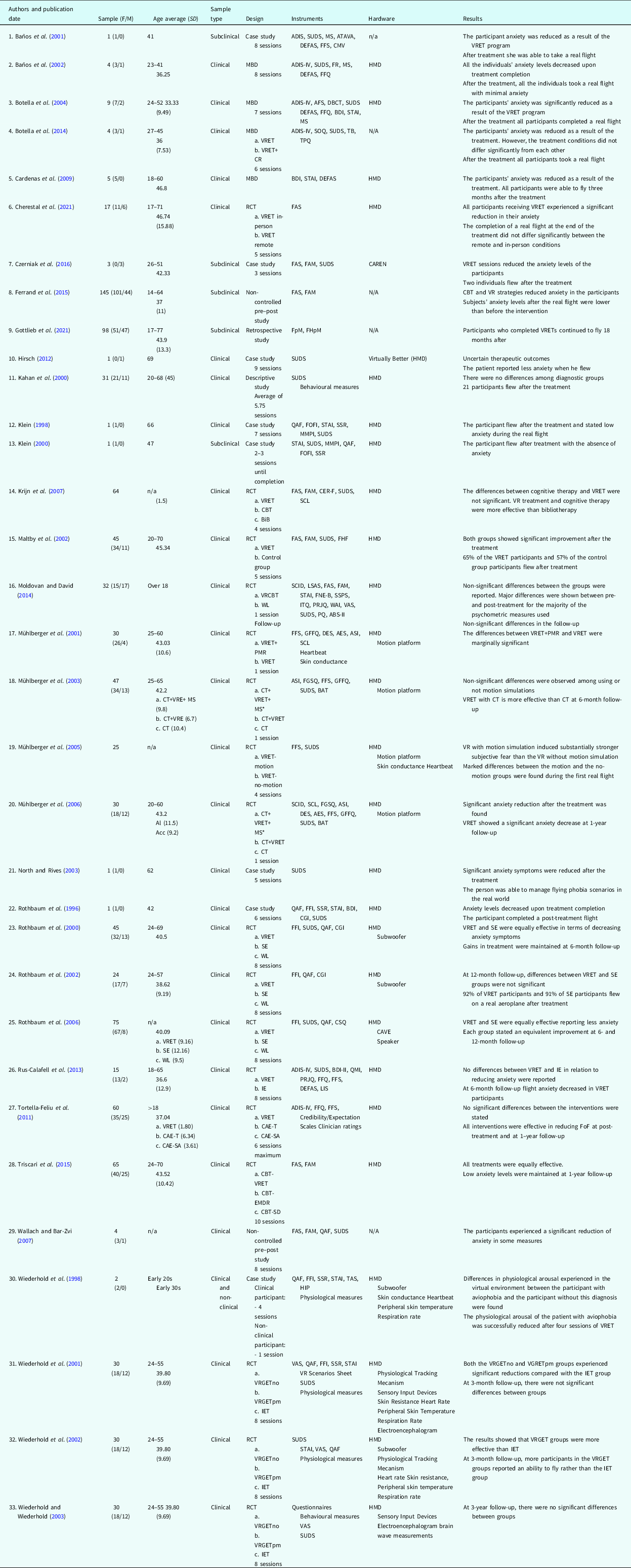
Note. ADIS-IV, Anxiety Disorders Interview Schedule; AES, Anxiety Expectancy Scale; AFS, Avoidance and Fear Scale; ASI, Anxiety Sensitivity Index; ATAVA, Autoinforme sobre Temores a Volar en Avión (in English: Self report about fear of flying); ABS-II, Attitudes and Beliefs Scale II; BAT, Behavior Avoidance Test; BDI, Beck Depression Inventory; BiB, Bibliotherapy; CAE-SA, Self-administered Computer-aided Exposure; CAE-T, Computer-Aided Exposure with Therapist’s assistance throughout exposure sessions; CAREN, Computer Assisted Rehabilitation Environment (Motek Medical©, Amsterdam, the Netherlands); CBT, Cognitive Behavioural Therapy; CCT, Controlled Clinical Trial; CER-F, Cognitive Emotion Regulation Questionnaire Flying; CGI, Clinical Global Improvement; CMV, Cuestionario de Miedo a Volar (in English: Fear of Flying Questionnaire, FFQ); CR, Cognitive Restructuring; CSQ, Client Satisfaction Questionnaire; CT, Cognitive Treatment; DBCT, Degree of Belief in Catastrophic Thoughts; DEFAS, Danger Expectations and Flying Anxiety Scales; DES, Danger Expectancy Scale; EMDR, Eye Movement desensitisation and Reprocessing; FAM, Flight Anxiety Modality Questionnaire; FAS, Flight Anxiety Situations Questionnaire; FFQ, Fear of Flying Questionnaire; FFS, Fear of Flying Scale; FGSQ, Fear and General Symptoms Questionnaire; FHF, Flying History Form; FHpM, Flight Hours per Month; FNE-B, Fear of Negative Evaluation Scale; FOFI, Fear of Flying Interview; FpM, Flights per Month; FR, Fear Record; GFFQ, General Fear of Flying Questionnaire; HIP, Hypnotic Induction Profile; IE, Imaginal Exposure; IET, Imaginal Exposure Therapy; ITQ, Immersive Tendencies Questionnaire; IVE, In Vivo Exposure; LIS, Life Interference Scales; MBD, Multiple Baseline Design; MMPI, Minnesota Multiphasic Personality Interview; *MS, Motion Simulation; MS, Maladjustment Scale; n/a, not available; PQ, Presence Questionnaire; PMR, 1 VR test flight + 1 Progressive Muscular Relaxation; PRJQ, Presence and Reality Judgement Questionnaire; QAF, Questionnaire on Attitudes toward Flying; QMI, Questionnaire Upon Mental Imagery; RCT, Randomised Control Trial; SCID, Structured Clinical Interview for DSM; SCL, Symptom Checklist; SD, Systematic desensitisation; SE, Standard Exposure; SOQ, Session Opinion Questionnaire; SSPS, Self Statements during Public Speaking Scale; SSR, Self-Survey of Stress Responses; STAI, State-Trait Anxiety Inventory; Subwoofer, office chair with a subwoofer mounted underneath to deliver vibrations to participants during the flight experience; SUDS, Subjective Units of Discomfort Scale; TAS, Tellegen Absorption Scale; TB, Target Behaviours; TPQ, Treatment Preferences Questionnaire; VAS, Visual Analogue Scale; VRCBT, Virtual Reality combined with Cognitive Behavioral Therapy; VRET, Virtual Reality Exposure Therapy; VRGETno, Virtual Reality Graded Exposure Therapy without physiological feedback; VRGETpm, Virtual Reality Graded Exposure Therapy with physiological feedback; WAI, Working Alliance Inventory’; WL, Waiting List.
In general, reviewed studies found that flying-related anxiety levels of the participants decreased after being systematically and repeatedly exposed to aeroplane-related virtual scenarios (1, 2, 3, 4, 6, 8, 9, 14, 19, 20, 21, 22, 23, 25, 29, 30). Furthermore, after VRET, the participants were able to take a real flight, experiencing slight or no anxiety at all (1, 2, 3, 4, 7, 9, 11, 13, 15, 23, 24, 25, 26, 27, 28, 30, 31, 32). However, statistically significant differences between VRET and other interventions such as cognitive behavioural therapy, IVET, imaginal exposure, self-administered computer-aided exposure, computer-aided exposure with therapist’s assistance throughout exposure sessions, eye movement desensitisation and reprocessing therapy (EMDR), remote VRET treatment, and systematic desensitisation, were not always found (6, 14, 16, 23, 25, 26, 27, 28).
Three studies (11, 15, 16) considered different criteria to include participants in the experiment, so participants were presenting other phobias or anxiety disorders. Six articles included subclinical individuals and 28 included a clinical sample. The number of VRET sessions ranged from 1 to 4 in six studies, while 24 studies used between 4 and 10 sessions. Two studies could not precisely report the number of sessions because they were based on the favourable evolution in the anxiety levels during the VRET. Most of the studies used eight VRET sessions to carry out the experiment.
Regarding the duration of VR exposure sessions, some lasted under 30 minutes each (12, 13, 16, 17, 18, 19, 20, 33), while others ranged between 30 and 90 minutes (1, 2, 3, 4, 6, 7, 15, 22, 23, 24, 28, 29, 30, 31). Moreover, some treatment sessions were scheduled on a weekly session basis (1, 2, 6, 12, 13, 14, 15, 23, 24, 25, 28, 32). Other studies set three baseline periods (1, 2 and 3 weeks between sessions), where the participants were randomly assigned to them (3, 4, 5). After the pre-treatment assessment session, two studies (26, 27) included participants who had to complete six individual treatment sessions for 3 weeks. In one study (10), the authors designed a 1-day intervention. Patients were assigned between-session homework in order to promote their psychological management during the treatment (3, 12, 17, 23, 24, 25, 26, 31, 32). A limited number of experiments (4, 6, 11, 26, 32) focused the initial sessions on psychoeducation comprising information about anxiety, FoF, aircraft safety, or exposure therapy. Concerning the therapists’ involved experience, some studies included experienced and non-experienced professionals (1, 3, 6, 15, 16, 20, 28), others (2, 5, 8, 11, 12, 18, 19) had only senior therapists. In the research of Mühlberger et al. (Reference Mühlberger, Herrmann, Wiedemann, Ellgring and Pauli2001), only non-experienced therapists were employed. A few papers employed cognitive behavioural therapists (3, 8, 11, 16, 18, 26).
Considering the working alliance reported by the patient between the therapist and the participant during the VRET sessions, it can be said that, on the one hand, this alliance had significantly contributed to reduce anxiety levels in participants (16). On the other hand, two studies (1, 18) showed that the therapist alliance with the participants was not significant. On the contrary, in one study (33) was primarily the therapist’s skills that led to successful therapeutic results. Regarding the treatment experience, participants expressed satisfaction with the procedure (3, 4, 7, 23, 25, 27). The drop-out rate in most studies was between 4 and 10% (15, 17, 18, 23, 25, 31). In two studies, however, it was between 15 and 53% (14, 20). The main causes of participants’ withdrawal were psychological problems, financial issues, and simulation sickness. Motion sickness was a specific cause of drop-outs in VRET groups (14, 15). The rest of the studies identified other reasons that triggered the participants’ withdrawal.
The present study includes articles in which psychometric and psychophysiological assessment measures have been integrated, minimising biases in their results. Most experiments included more than four psychological measures, and behavioural outputs (see Table 1). Some publications (19, 30, 31, 33) repeatedly included psychophysiological monitoring to control the participants’ physiological activation during the experiment. Most studies assessed anxiety levels through subjective psychological questionnaires (see Table 1).
Since the last decade of the 20th century, several studies have been conducted on exposure-based therapies for the treatment of FoF through VR revealing an evident evolution of case studies carried out between the 90s and the beginning of the 21st century. The first decade of the 21st century witnessed an increasing number of RCTs. The scientific community certainly realised the need to continue evaluating the performance of VR in comparison with other cognitive behavioural therapeutic techniques such as systematic desensitisation. In order to expand the knowledge and discriminate the therapeutic effects of VRET, more RCTs were carried out than other types of studies. A remarkable number of studies (2, 3, 4, 5, 6, 14, 15, 16, 17, 18, 19, 20, 23, 24, 25, 26, 27, 28, 31, 32) used randomisation in order to assign participants to the different experimental groups.
According to examined data, there is a relationship between case designs, which employed instruments not technologically developed for the studies’ purposes (sharpness, calibration, visual content display in HMDs) and RCTs. Throughout time, advances in VR hardware and software have enabled fast progress in the devices’ performance, durability and reliability. In general, RCTs use more sophisticated instruments which offer a higher quality of virtual experience than most case studies. A computer-assisted rehabilitation environment (CAREN) and Virtually Better were the pioneer software, used in four studies (7, 10, 23, 32). Furthermore, only one study (25) employed hardware other than a head-mounted display (HMD): a computer automatic virtual environment (CAVE), where the patient and the therapist were surrounded by stereoscopic computer-generated images on four sides of a laboratory room. The rest of the studies used the same device to standardise the methodology and generate experiment reliability: HMDs were convenient because the user could experience visual and auditory synchronised stimuli from the virtual display, making the exposure more realistic. In two studies, the authors considered different devices to increase the patient’s sense of presence in the virtual environment (2, 3). In the paper of Krijn et al. (Reference Krijn, Emmelkamp, Olafsson, Bouwman, Van Gerwen, Spinhoven, Schuemie and van der Mast2007), the virtual environments did not cause anxiety in a substantial number of patients. All experimental studies used 3D virtual scenarios.
Visual and auditory cues were the most common sensory stimuli included in the virtual scenarios of the reviewed studies employed through an HMD or a CAVE. However, some researchers also incorporated motion cues in their virtual scenarios to increase the realism of the virtual experience and, consequently, the sense of presence experienced by the participants during VRET sessions. The following devices were employed to produce vibrotactile or motion stimulation: a motion platform between 2 and 6 degrees of freedom (Symtech Corporation) (17, 18, 19, 20), a specially designed seat with an embedded 100-watt subwoofer and an attached aeroplane seatbelt (23, 24), a bass speaker (25), and a subwoofer mounted under the patient’s chair to add noise and vibrations at appropriate times in the flight (30, 32). Despite the potential effect of adding vibrotactile or motion cues on patients’ anxiety responses, most studies (18, 20, 23, 24, 25, 30, 32) did not specify its contribution to the efficacy of the VRET. Only Mühlberger et al. (Reference Mühlberger, Wiedemann and Pauli2003, Reference Mühlberger, Wiedemann and Pauli2005) addressed this issue, finding mixed results. While no significant anxiety differences were found when using or not motion stimulation in their trials, in one study (18), these authors found a significant increase in heart rate in the VR-motion group compared with the non-motion group, providing support to the capability of vibrotactile stimulation of increasing anxiety during exposure to virtual flying-related environments.
Case studies
All case studies examining the efficacy of VRET (1, 7, 12, 13, 21, 22, 30), except for Hirsch (Reference Hirsch2012) (10), who found inconclusive results, showed lower anxiety levels after the exposure sessions. Wiederhold et al. (Reference Wiederhold, Gervirtz and Wiederhold1998), for example, found a stronger physiological response in a patient with FoF compared with a participant without this diagnostic when exposed for the first time to a flying-related virtual environment. However, the physiological arousal of the patient with aviophobia was successfully reduced after four sessions of VRET (30). In half of the case studies (1, 7, 13, 22), participants with FoF took a real flight after treatment. Interestingly, Czerniak et al. (Reference Czerniak, Caspi, Litvin, Amiaz, Bahat, Baransi and Plotnik2016) reported that one of the three patients that participated in the case studies experienced immersion difficulties in the virtual environment and, consequently, a noticeable and quick decrease in anxiety levels (7). Such a circumstance prevented him from experiencing the necessary anxiety in the virtual scenarios to assure the efficacy of the exposure treatment. In fact, this patient was not able to take a real flight after VRET. Czerniak et al. (Reference Czerniak, Caspi, Litvin, Amiaz, Bahat, Baransi and Plotnik2016) (7) concluded that VRET is not recommended for patients for whom the VR environment does not provoke anxiety.
Case studies examined in this review administrated 3–10 virtual reality exposure sessions, with an average of eight sessions. Two case studies (10, 21) only used the subjective units of distress (SUDs) for assessing anxiety levels. Therefore, there might be biases in the general outcomes.
Randomised controlled trials
Until December 2021, 17 RCTs (6, 14, 15, 16, 17, 18, 19, 20, 23, 24, 25, 26, 27, 28, 31, 32, 33) for assessing VRET for FoF’s treatment have been conducted. Overall, the RCTs indicated that there were significant differences between VRET and non-active control conditions in terms of having better results than the waiting list (23, 24, 25) (see Table 1). Only one study (16) showed that active conditions were as effective as non-active conditions. When it comes to designs that compare VRET with other active conditions, on the one hand, some articles showed slightly more efficacy in VRET rather than the other active conditions (14, 17, 18, 19, 31, 32): progressive muscular relaxation, cognitive therapy, bibliotherapy, motion simulation, and imaginal exposure therapy. On the other hand, VRET did not show significant differences compared with cognitive behavioral therapy (CBT), standard exposure, imaginal exposure therapy (IET), computer-aided exposure with a therapist’s assistance, self-administered computer-aided exposure, eye movement desensitisation and reprocessing (EMDR), and systematic desensitisation (SD) (14, 17, 23, 24, 25, 26, 27, 28). Therefore, it can be concluded that all conditions were equally effective. The study of Mühlberger et al. (Reference Mühlberger, Wiedemann and Pauli2003) showed that virtual reality exposure accompanied by cognitive therapy was more effective than cognitive therapy alone (18). Likewise, according to Triscari et al. (Reference Triscari, Faraci, Catalisano, D’Angelo and Urso2015), the combination of CBT with both EMDR treatment and virtual reality appeared as efficient as CBT combined with systematic desensitisation (28).
Similar results were also found at follow-up. On the one hand, eight studies (15, 16, 23, 24, 25, 27, 28, 33) showed no significant differences at follow-up between VRET and the other comparison groups: control group, waiting list, standard exposure, self-administered computer-aided exposure, computer-aided exposure with the therapist’s assistance throughout exposure sessions, cognitive behavioral therapy, eye movement desensitisation and reprocessing, systematic desensitisation, and imaginal exposure therapy. For example, in Rothbaum et al. (Reference Rothbaum, Hodges, Smith, Lee and Price2000, Reference Rothbaum, Anderson, Zimand, Hodges, Lang and Wilson2006), gains in both standard exposure and VRET were maintained at 6-month follow-up (23, 25), and in Maltby et al. (Reference Maltby, Kirsch, Mayers and Allen2002), most of the differences between VRET and the control group at post-treatment disappeared after a 6-month follow-up (15). On the other hand, some papers reported significant differences (18, 20, 26, 31) between VRET and the rest of the groups: cognitive treatment, motion simulation and imaginal exposure therapy. According to Mühlberger et al. (Reference Mühlberger, Wiedemann and Pauli2003), the VRET was more effective than cognitive therapy at 6-month follow-up (18). In Rus-Calafell et al. (Reference Rus-Calafell, Gutiérrez-Maldonado, Botella and Baños2013), flying anxiety and danger expectations in the VRET group kept decreasing at 6-month follow-up, but not in the IET group, and four of the seven participants in the VRET group took at least one more flight during the follow-up (26). Mühlberger et al. (Reference Mühlberger, Wiedemann and Pauli2003) concluded that taking a flight after treatment might enhance the VRET efficacy (18).
Psychophysiological measures such as heartbeat, skin conductance, peripheral skin temperature or respiration rate show greater reliability when it comes to controlling the emotional responses of participants. Consequently, some studies used these indicators (17, 19, 30, 31, 32) to assess the efficacy of the interventions. Regarding the psychophysiological activation, Wiederhold et al. (Reference Wiederhold, Gevirtz and Spira2001) explored the subjective arousal that emerged from the exposure, and did not find significant differences between participants in the VRET and the IET groups (31). Mühlberger et al. (Reference Mühlberger, Wiedemann and Pauli2005) found stronger psychophysiological responses in participants that were exposed to VR scenarios with motion cues (VR-motion group) than in participants exposed to VR environments without motion cues (VR-non-motion group) (19). However, such differences did not lead to better treatment outcomes in the VR-motion group.
Regarding the sample size of the studies, there were more than 30 participants in most of them (14, 15, 16, 18, 23, 25, 26, 28). However, there were studies (6, 24, 26) that included small samples, ranging from 10 to 20 participants. Concerning nationality, all participants came from western countries.
Other studies
The studies found in this section are distinguished as follows: four MBDs (2, 3, 4, 5), two non-controlled pre–post articles (8, 29), one retrospective study (9), and one descriptive study (11). In general, the sample size of these studies was small. There were only two papers (8, 9) with large sample sizes.
Overall, there were studies (2, 3, 4, 5, 8, 9, 29) examining the efficacy of VRET, which demonstrated lower anxiety levels after the exposure sessions, as in the majority of RCTs. Participants flew after treatment in most studies (2, 3, 4, 5, 9, 11). Only in one study (11) a follow-up was completed, finding that participants could fly despite experiencing anxiety.
In all reviewed studies, more than four virtual reality sessions were administrated during the treatment and several instruments were used to obtain reliable outcomes. Kahan et al. (Reference Kahan, Tanzer, Darvin and Borer2000) also included behavioural measures, so their team could better control the efficacy of the intervention (11).
Discussion and conclusion
The aim of this review was to examine the efficacy of VRET for FoF, to assess the methodological quality of the studies reviewed, and to identify the different devices and other potential elements which contribute to VRET’s efficacy. This review expands on previous systematic reviews and meta-analytic studies (Cardoş et al., Reference Cardoş, David and David2017; Da Costa et al., Reference Da Costa, Sardinha and Nardi2008) by providing an updated synthesis of research on VRET for FoF. The study emphasises the efficacy of VRET and the devices used during its administration, particularly the addition of motion cues to the most common VR systems used in VRET, which only include visual and auditory cues.
Thirty-three studies fulfilled the inclusion criteria and provided significant data about VRET efficacy for FoF. The results indicate that VRET is an effective treatment for FoF that could be conveniently used in the clinical practice. In previous reviews and meta-analyses (Cardoş et al., Reference Cardoş, David and David2017; Carl et al., Reference Carl, Stein, Levihn-Coon, Pogue, Rothbaum, Emmelkamp and Powers2019; Da Costa et al., Reference Da Costa, Sardinha and Nardi2008; Morina et al., Reference Morina, Ijntema, Meyerbröker and Emmelkamp2015), it was already stated that VRET contributed to an effective therapeutic success compared with other exposure-based interventions. Likewise, Price et al. (Reference Price, Anderson and Rothbaum2008) stated that VRET was comparable or even superior to IVET for the treatment of aviophobia. Articles reviewed in this study confirm that VRET is as efficacious as other cognitive and behavioural treatments available for FoF, including progressive muscular relaxation, systematic desensitisation, cognitive therapy and imagery exposure (Opris et al., Reference Opris, Pintea, García-Palacios, Botella, Szamosközi and David2012). Most of the studies that used a strictly VRET-based protocol showed significant differences between VRET and non-active control conditions in reducing clinical symptoms associated with FoF. Furthermore, in the majority of RCTs, all active treatments, including VRET, proved to be equally effective for the treatment of aviophobia. The reviewed articles have also confirmed that the addition of VRET to other cognitive and behavioural evidence-based psychological treatments, such as CBT, could be more effective than cognitive therapy alone.
However, it is important to highlight that for the VRET to be effective, it is essential that patients experience anxiety and sense of presence in the virtual environment (Czerniak et al., Reference Czerniak, Caspi, Litvin, Amiaz, Bahat, Baransi and Plotnik2016). In those cases where the patient does not experience anxiety or does not feel present in the virtual environments, VRET should not be recommended (Weech et al., Reference Weech, Kenny and Barnett-Cowan2019).
Regarding the exposure’s conditions, interventions incorporating cognitive techniques and well-trained therapists improved VRET efficacy (Ferrand et al., Reference Ferrand, Ruffault, Tytelman, Flahault and Négovanska2015). Accordingly, reviewed studies showed that including senior therapists was more appropriate as they hold extensive experience and knowledge about cognitive behavioural techniques. With respect to the working alliance between the therapist and the participant, which has been hypothesised to reduce the participant’s anxiety (Bouchard et al., Reference Bouchard, Dumoulin, Robillard, Guitard, Klinger and Forget2016; Wechsler et al., Reference Wechsler, Kümpers and Mühlberger2019), was not significant in the reviewed studies. Likewise, focusing the first sessions on psychoeducation comprising information about FoF and exposure therapy are all helpful features for the participants’ exposure control (Benbow and Andreson, Reference Benbow and Anderson2019). Additionally, assigning homework between sessions could facilitate psychological management during treatment (Cronin et al., Reference Cronin, Lawrence, Taylor, Norton and Kazantzis2015; Mausbach et al., Reference Mausbach, Moore, Roesch, Cardenas and Patterson2010; Rowland et al., Reference Rowland, Casey, Ganapathy, Cassimatis and Clough2022).
The HMD was the device most frequently used for administrating the VRET. Consequently, HMD might be used to standardise the design and results of future studies in the VR field addressing FoF. Despite being correlated with increasing presence, the use of a CAVE instead of an HMD did not result in greater therapeutic success (Bullinger, 2005). Although the virtual environments provide high levels of logistical comfort, it may be necessary to receive help from a trained technical team to adjust the virtual environment as individualisation might be an effective factor of VRET (Wechsler et al., Reference Wechsler, Kümpers and Mühlberger2019). In addition, the cost of the equipment needed for displaying a virtual environment is high, especially if additional hardware such as vibrational chairs, subwoofers, or motion platforms are needed. Thus, the therapist or health centres require a substantial financial investment. Fortunately, these devices are becoming cheaper now that they are frequently used in various industries (Moro et al., Reference Moro, Stromberga, Birt, Nestel, Reedy, McKenna and Gough2020), making them more affordable for therapists.
The addition of vibrotactile and motion cues have also been proposed to increase the realism of the flying-related virtual environments and the immersion experienced by patients during the exposure (North and North, Reference North and North2016), which may increase the efficacy of the VRET. Previous research has also shown how tactile stimuli could contribute to experiencing more sense of presence during a VRET (Kaul et al., Reference Kaul, Meier and Rohs2017; Luecke and Chai, Reference Luecke and Chai1997; Serrano et al., Reference Serrano, Baños and Botella2016). Several studies (Meyer et al., Reference Meyer, Shao, White, Hopkins and Robotham2013; Ramsamy et al., Reference Ramsamy, Haffegee, Jamieson and Alexandrov2006; Wiederhold et al., Reference Wiederhold, Gervirtz and Wiederhold1998) stated that a VR system implies benefits due to the stimulation of several sensory categories, including auditory, visual, vibrotactile, spatial orientation and motion cues. Thus, multiple sensory categories might better prepare patients for flying as this systematic review shows. There are reasons to believe that such stimuli contribute to the sense of presence and immersion experienced in anxiety-eliciting virtual scenarios (Cooper et al., Reference Cooper, Milella, Pinto, Cant, White and Meyer2018; Marquardt et al., Reference Marquardt, Trepkowski, Maiero, Kruijff and Hinkeniann2018; Marucci et al., Reference Marucci, Di Flumeri, Borghini, Sciaraffa, Scandola, Pavone and Aricò2021; Mühlberger et al., Reference Mühlberger, Herrmann, Wiedemann, Ellgring and Pauli2001, Reference Mühlberger, Weik, Pauli and Wiedemann2006; Rothbaum et al., Reference Rothbaum, Hodges, Smith, Lee and Price2000). In phobias such as spider phobia, studies suggest that adding tactile feedback is helpful for the treatment (Carlin et al., Reference Carlin, Hoffman and Weghorst1997; García-Palacios et al., Reference García-Palacios, Hoffman, Carlin, Furness and Botella2002; Hoffman et al., Reference Hoffman, García-Palacios, Carlin and Botella-Arbona2003). As it is stated in some reviewed studies (Krijn et al., Reference Krijn, Emmelkamp, Olafsson, Bouwman, Van Gerwen, Spinhoven, Schuemie and van der Mast2007; Maltby et al., Reference Maltby, Kirsch, Mayers and Allen2002), when including vibrotactile or motion cues it is necessary to consider the risk of drop-out of participants due to motion during the virtual exposure; thus it is advisable to provide psychoeducation to participants and calibrate motions accurately in order to avoid withdrawals during VRET.
Regarding the use of psychophysiological monitoring and feedback during the treatment of those suffering from FoF, these could provide additional benefits in terms of adjusting their psychophysiological levels based on the virtual content (Diemer et al., Reference Diemer, Mühlberger, Pauli and Zwanzger2014; Wechsler et al., Reference Wechsler, Kümpers and Mühlberger2019; Wiederhold et al., Reference Wiederhold, Jang, Gevirtz, Kim, Kim and Wiederhold2002a, Reference Wiederhold, Jang, Kim and Wiederhold2002b). The visual guidance offered by the physiological monitoring equipment could empower participants to undergo treatment, so they could objectively see their clinical progress over time. In order to better understand the mechanism of transition that happens as the phobic patient becomes desensitised, future studies should provide more sensitive psychophysiological measures such as heart rate variability, blood pressure and cardiac activity. This may assist clinicians in assessing which patients could complete the treatment and which will require further sessions before flying.
The technology world is changing quickly and steadily, and VR is not an exception to the field of technology’s rapid and determined evolution (Muñoz-Saavedra et al., Reference Muñoz-Saavedra, Miró-Amarante and Domínguez-Morales2020). Consequently, there are reasons to exercise caution when adhering to ethical considerations and avoiding iatrogenic effects on the general population. As a result, it would be essential to determine the direction of technological advancement in clinical practice and personalise such VR interventions in order to develop the next generation of VRET (Lindner et al., Reference Lindner, Miloff, Hamilton, Reuterskiöld, Andersson, Powers and Carlbring2017).
Taking the data collected in this review into account, there are specific conditions which could improve the efficacy of VRET for FoF: structure a scheduled treatment of eight sessions lasting approximately 30 minutes each; include psychoeducation in the first two sessions about FoF and cognitive behavioural strategies that favour managing the fears involved in FoF; the participation of well-trained therapists who assign homework between sessions; and the use of HMDs as well as motion feedback synchronised with visual and auditory cues.
Despite the interest of the conclusions of this review, its limitations should be also considered. First, not all available databases were reviewed, so some studies related to the subject of this research may be missed. Moreover, the authors of the articles included in this study were not asked for further information about current and unpublished research. Therefore, there is missing information in some of the reviewed studies (e.g. the characteristics of the sample or the hardware employed during the VRET) that could be important regarding the conclusions of this review. For instance, in Klein (Reference Klein2000), no evidence confirms the presence of a phobia diagnosis despite the presence of phobic symptoms. None of the articles described how the sample size was calculated and, in most of the reviewed studies is small, which leads to a reduction of statistical power and complicates the generalisation of the results found. Concerning the nationality of the participants, reviewed studies included samples of individuals living only in developed countries, a fact that could also interfere with the generalisation of the results, as stated in Rothbaum et al. (Reference Rothbaum, Anderson, Zimand, Hodges, Lang and Wilson2006). Thus, it would be necessary to elaborate with specific research in low- and middle-income countries, where the population presents and maintains more psychological diseases (Rathod et al., Reference Rathod, Pinninti, Irfan, Gorczynski, Rathod, Gega and Naeem2017).
Regarding future research, further studies which use vibrotactile, auditory and visual stimuli in virtual environments are still needed in order to provide more substantial empirical support regarding the comparison between IVET and VRET. Gradually, more healthcare teams are employing VRET due to its demonstrated effectiveness (Muñoz-Saavedra et al., Reference Muñoz-Saavedra, Miró-Amarante and Domínguez-Morales2020). Consequently, it may soon become a necessary tool for the clinical practice of treating anxiety disorders (Krijn et al., Reference Krijn, Emmelkamp, Olafsson and Biemond2004), and particularly aviophobia (Powers and Emmelkamp, Reference Powers and Emmelkamp2008). Therefore, it is important to introduce clear instructions and automatic changes in virtual environments for non-qualified users, so that therapists can easily personalise the environments to which patients will be exposed, taking into consideration their specific fears and, thereby, increasing their sense of control and confidence. As air travel is a necessity of modern life and it is expected to increase as the global economy incorporates more business travel (IATA, 2018), a greater awareness of FoF and a rise of VRET employment is anticipated (Gottlieb et al., Reference Gottlieb, Doniger, Hussein, Noy and Plotnik2021). Consequently, further research and meta-analyses are needed for a more comprehensive understanding of VRET’s effectiveness and to ensure its safe and ethical implementation in clinical practice.
This systematic review provides compelling evidence that VRET is an effective treatment for FoF. However, the impact of motion cues in VRET interventions is currently unknown and more research is needed. These findings have important implications for the clinical practice of treating anxiety disorders, particularly for those with FoF who may struggle with traditional in vivo exposure therapy. By utilising VRET, clinicians can provide a safe and controlled environment for patients to confront their fears and gradually overcome their phobia. This not only enhances patient outcomes but also improves the overall quality of life for those suffering from FoF. As technology continues to advance, VRET has the potential to become an even more valuable tool in the treatment of anxiety disorders, paving the way for more effective and personalised interventions.
Data availability statement
The data used to support the findings of this study are included within the article.
Acknowledgements
We would like to express deep gratitude to Professor Marta Ferrer and José Gutiérrez, research supervisors, for their patient guidance, enthusiastic encouragement and constructive critiques regarding this research work. We also appreciate the involvement of Zahra Zabolipour for her valuable advice and assistance in keeping progress on schedule.
Author contribution
José Ribé Viñes: Conceptualization (lead), Data curation (lead), Formal analysis (lead), Methodology (lead), Writing – original draft (lead), Writing – review & editing (lead); José Gutiérrez-Maldonado: Supervision (lead), Validation (lead), Writing – review & editing (supporting); Zahra Zabolipour: Data curation (supporting), Supervision (supporting), Validation (supporting), Writing – review & editing (supporting); Marta Ferrer–García: Conceptualization (supporting), Methodology (supporting), Supervision (equal), Validation (equal), Visualization (equal), Writing – review & editing (equal).
Financial support
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Competing interests
The authors declare no potential competing interests with respect to the research, authorship, and/or publication of this article.
Ethical standard
This article does not contain any studies with human or animal subjects performed by any of the authors. This systematic review is part of a larger study approved by the bioethics committee of the Universitat de Barcelona (IRB00003099). This study complies with the Declaration of Helsinki.







Comments
No Comments have been published for this article.