Given the unprecedented trend in population ageing, outcomes such as health-related quality of life (HRQoL) have become increasingly important(Reference May, Struijk and Fransen1). Although life expectancy is increasing, people who live longer are not necessarily in good health(Reference Murray, Vos and Lozano2). Modifiable risk factors which promote unhealthy lifestyles such as physical inactivity, smoking and poor dietary behaviours are among the leading contributors to overall morbidity and mortality(Reference Zaccardi, Franks and Dudbridge3–Reference Krokstad, Ding and Grunseit5). Data from the Global Burden of Disease study revealed that one-fifth of all non-communicable disease deaths were attributable to dietary risk factors(Reference Melaku, Renzaho and Gill6). Specifically, a low dietary intake of nutrient-dense foods, such as fruits, vegetables, nuts, seeds and wholegrain cereals, coupled with an excessive intake of dietary Na were the primary dietary contributors to both non-communicable disease deaths and disability-adjusted life years(Reference Melaku, Renzaho and Gill6).
There are several physiological changes that occur throughout the ageing process, including reductions in lean body mass and a concurrent accumulation of fat mass(Reference Newman, Lee and Visser7,Reference Janssen, Heymsfield and Wang8) . Among the older adult population, secular trends in obesity have steadily increased over recent decades(Reference Ng, Fleming and Robinson9,Reference Batsis and Villareal10) . Further, the prevalence of type 2 diabetes mellitus (T2DM) has escalated in recent times; as such, older adults with T2DM represent one of the fastest-growing segments of the diabetic population(Reference Sinclair, Abdelhafiz and Forbes11) and this increased surge is expected to continue over the next few decades(Reference Cho, Shaw and Karuranga12). Obesity and its associated co-morbidities are predictive of declines in HRQoL(Reference Busutil, Espallardo and Torres13). Moreover, ageing itself is associated with a sequela of poor health, including multiple co-morbidities, frequent hospitalisations, physical disability and functional decline(Reference Beard, Officer and de Carvalho14,Reference Figaro, Kritchevsky and Resnick15) , all of which threaten the HRQoL of older adults.
HRQoL is an important patient-reported outcome, and a measure of the impact disease and treatment have across a range of subscales related to functioning and well-being, including physical, psychological, social and somatic(Reference May, Struijk and Fransen1,Reference Beaudart, Biver and Bruyère16) . Moreover, HRQoL is a relevant outcome among researchers, clinicians and policymakers, where the focus is to improve quality of life rather than prolong life. The relationship between nutritional adequacy and HRQoL has previously been investigated in older adults, including those with T2DM(Reference Alfonso-Rosa, del Pozo-Cruz and Del Pozo-Cruz17–Reference Amarantos, Martinez and Dwyer19). Furthermore, the paradigm of assessing diet quality and dietary patterns as opposed to individual nutrients as a determinant of overall health has been recognised for some time(Reference Hu20). In a cross-sectional analysis of > 5000 older adults aged ≥ 60 years from the National Health and Nutrition Examination Survey, a healthy diet, as defined by a healthy eating index score, was associated with HRQoL(Reference Xu, Cohen and Lofgren21). Dietary patterns can be defined by two main approaches: (1) a posteriori, which define dietary patterns via statistical approaches such as factor or cluster analysis, and (2) a priori, which are scoring systems informed by guidelines and recommendations, and are often referred to as diet quality indices(Reference McNaughton, Ball and Crawford22,Reference Milte and McNaughton23) . As such, diet quality indices can assess adherence to dietary guidelines(Reference McNaughton, Ball and Crawford22) or particular dietary patterns such as the Mediterranean diet (MedDiet)(Reference Martínez-González, García-Arellano and Toledo24,Reference Trichopoulou, Costacou and Bamia25) .
The MedDiet is used to describe the traditional dietary pattern among the people of the olive-growing regions of the Mediterranean basin(Reference Mantzioris and Villani26). Moreover, the MedDiet has been widely investigated and promoted over several decades as one of the ‘healthiest’ dietary patterns with respect to reductions in chronic disease risk and healthy ageing(Reference García-Fernández, Rico-Cabanas and Rosgaard27,Reference Dinu, Pagliai and Casini28) . Analysis from the SUN (Seguimiento Universidad de Navarra) Project, a longitudinal cohort study of 11 015 men and women from Spain(Reference Henríquez Sánchez, Ruano and de Irala29), showed a linear association between adherence to a MedDiet and four physical domains related to HRQoL. However, this observation has not always been reported(Reference Pérez-Tasigchana, León-Muñoz and López-García30). Moreover, there is a paucity of published literature investigating the relationship between adherence to a MedDiet and HRQoL, particularly in overweight and obese middle-aged and older adults with chronic disease from multi-ethnic, non-Mediterranean populations.
Therefore, we explored the association between adherence to a MedDiet and the various subscales related to HRQoL in community-dwelling overweight and obese middle-aged to older adults with and without T2DM.
Methods
Study design, setting and participants
This was a cross-sectional analysis performed by merging two separate cohorts of community-dwelling middle-aged to older adults recruited from two independent studies conducted by our group(Reference Villani, Wright and Slater31,Reference McClure and Villani32) . The first cohort were overweight and obese older adults aged ≥ 60 years, free from multiple co-morbidities and recruited as part of a 12-week randomised control trial(Reference Villani, Wright and Slater31). For the purpose of the present study, baseline data from this cohort will be reported and referred to as the non-T2DM cohort. This trial was registered with the Australian and New Zealand Clinical Trials Registry (reg. no: ACTRN12616001400459). The second cohort were overweight, middle-aged to older adults aged ≥ 50 years, with a confirmed diagnosis of T2DM(Reference McClure and Villani32). Participants from both cohorts were included with a BMI ≥ 25 kg/m2. In both cohorts, participants were excluded based on the presence of cancer, respiratory, neurological and renal diseases, physical disability, poor cognition/unable to provide informed consent, current or recent use of anti-inflammatory drugs, corticosteroid agents or sex steroid compounds. All participants were recruited from the Sunshine Coast, Queensland, Australia via local flyers, newspaper advertisements and social media platforms. Both studies were conducted in accordance with the guidelines described in the Declaration of Helsinki, and all procedures involving human subjects were approved by the Human Research Ethics Committee (A/16/801) (S/171/123), University of the Sunshine Coast, Queensland, Australia. Written informed consent was obtained from all participants. Furthermore, the present study has been reported according to the STROBE-nut checklist(Reference Lachat, Hawwash and Ocké33).
Outcome measures
Details related to the outcome measures presented in this study have been published elsewhere(Reference Villani, Wright and Slater31,Reference McClure and Villani32) . In brief, key outcome assessments included appendicular lean mass (ALM), functional markers including hand-grip strength and physical performance, adherence to a MedDiet and the assessment of HRQoL. In the present study, outcome assessments related to ALM and functional markers of sarcopenia were used as important covariates in the adjusted multiple regression models for the assessment of adherence to a MedDiet and HRQoL subscales.
Anthropometry and body composition
A calibrated digital scale (AND weighing; HW-KGL) was used to record body mass to the nearest 0·1 kg, with participants barefoot and wearing light, figure-hugging clothing. Height was measured to the nearest 0·1 cm while barefoot using a wall-mounted stadiometer (Holtain Ltd.), with the participant’s head positioned in the Frankfort plane. BMI was calculated as weight (kg) divided by the square of height (m2).
Dual-energy X-ray absorptiometry (Lunar iDXA: GE Healthcare) was used to estimate the whole and regional body composition with analysis performed using the GE encore bone densitometry software (version 16: GE Healthcare). Estimates of fat-free mass, fat mass and lean soft tissue for total body, both arms and legs and the torso were determined. The sum of lean soft tissue mass in both arms and legs was used to determine the total ALM. The ALM index was calculated using the formula, ALM/height2 (kg/m2)(Reference Baumgartner, Koehler and Gallagher34). All dual-energy X-ray absorptiometry scans were performed and analysed by the same trained technician, according to the Nana et al. (Reference Nana, Slater and Hopkins35) protocol.
Functional markers
Hand-grip strength of the dominant hand was assessed as a proxy for muscle strength using a calibrated hand-held hydraulic dynamometer (Smedley). Participants were instructed to exert maximal force to the hydraulic dynamometer on three consecutive test measures, with ˜60-s rest breaks between each measure. All measures were recorded to the nearest 0·5 kg with the mean of the three measures used for the purpose of analysis.
The Short Physical Performance Battery was used to assess functional status and physical performance by evaluating lower body function through the assessment of three functional tests which mimic activities of daily living, including (1) lower body strength (chair stands); (2) balance (side by side, semi-tandem and tandem); and (3) usual gait speed(Reference Guralnik, Simonsick and Ferrucci36).
Mediterranean diet adherence
Adherence to a MedDiet was assessed using the previously validated 14-item Mediterranean diet Adherence Screener (MEDAS), used in the Prevención con Dieta Mediterránea (PREDIMED) study(Reference Martínez-González, García-Arellano and Toledo24). The MEDAS assesses habitual dietary adherence according to pre-defined normative criteria based on the frequency of consumption of twelve main dietary elements and two food habits related to a MedDiet pattern(Reference Martínez-González, García-Arellano and Toledo24). The fourteen questions in the adherence tool were scored as either 0 or 1, generating a maximum score of 14. A higher score is reflective of greater adherence to a MedDiet. Specifically, a MEDAS score ≥ 10 indicated high adherence, a score between 6 and 9 suggests moderate adherence and a MEDAS score ≤ 5 is considered low adherence to a MedDiet.
Health-related quality of life
HRQoL was assessed using an Australian adapted version of the 36-item short-form health survey(Reference Brazier, Harper and Jones37–Reference Lyons, Perry and Littlepage39). The survey instrument is a 36-item validated tool designed to provide aggregated physical component and mental component scores based on eight subscales associated with overall quality of life including physical functioning, social functioning, role limitations due to physical functioning, role limitations due to emotional health, emotional well-being, vitality, bodily pain and general health. Scoring values for each subscale ranged from 0 to 100, with higher scores reflective of a higher perceived HRQoL. To minimise the ambiguity of the questions, the 36-item short-form health survey questionnaire was administered by a member of the research team and further checked for error and missing responses following administration. In the present study, we examined the relationship between adherence to a MedDiet and each of the eight subscales associated with HRQoL as continuous variables.
Statistical analysis
All continuous variables are expressed as means and standard deviations with categorical data presented as frequencies and percentages. Pearson’s correlation coefficients were used to identify associations between adherence to a MedDiet and each of the eight subscales related to HRQoL in both the pooled data and independently by cohort. Similarly, multiple regression analysis was also used in both the pooled data and independently by cohort to examine the association between adherence to a MedDiet and HRQoL subscales, adjusted for age, sex, hand-grip strength, gait speed and ALM index. Multiple regression analysis was powered using the predictor variables established in each of the multivariable models and performed using G × Power. Assuming an α of 0·05, with 80 % power to detect a medium effect size (Cohen’s f2 = 0·15) for HRQoL subscales as the primary outcome, the estimated target sample size was 158 participants. However, to control for the potential inflation of a type I error as a result of multiple comparisons, a Bonferroni-adjusted α was considered for all post hoc comparisons, with statistical significance set at a P < 0·003 a priori. Analyses were performed using the Statistical Package for the Social Sciences for Windows 26.0 software (IDM Corp.), with statistical significance set a P < 0·05.
Results
A total of 152 community-dwelling middle-aged and older adults (70·2 (sd 7·3) years; male n 80 (52·6 %); female n 72 (47·4 %)) were included in the final analyses. Differences in participant characteristics across the two study cohorts are presented in Table 1. When applying the MEDAS adherence tool, pooled adherence scores for the entire cohort were 5·3 (sd 2·2) (range 1–11) with adherence scores greater among middle-aged to older adults with T2DM (T2DM cohort: 5·6 (sd 2·3); non-T2DM cohort: 4·9 (sd 2·0)).
Table 1. Participant characteristics according to the two study cohorts of overweight and obese middle-aged and older adults (T2DM v. non-T2DM)
(Mean values and standard deviations)
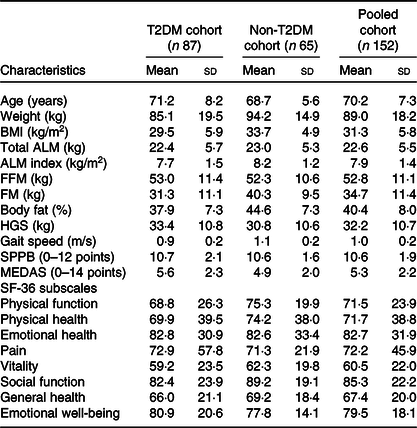
T2DM, type 2 diabetes mellitus; ALM, appendicular lean muscle; FFM, fat-free mass; FM, fat mass; HGS, hand-grip strength; SPPB, Short Physical Performance Battery; MEDAS, Mediterranean Diet Adherence Screener; SF-36, short-form health survey.
Using the pooled data from both study cohorts, Pearson’s correlation coefficients for adherence to a MedDiet and HRQoL subscales showed a small, yet positive association for physical functioning (r 0·263; P = 0·01), role limitations due to emotional health (r 0·166; P = 0·04), vitality (r 0·253; P = 0·02) and general health (r 0·251; P = 0·02). However, when applying the Bonferroni-adjusted correction, these findings were non-significant. Similar non-significant findings were also observed when examining this relationship independently in the T2DM cohort (physical functioning: r 0·286; P = 0·007; vitality: r 0·282; P = 0·008; general health: r 0·277; P = 0·009) and non-T2DM cohort (physical functioning: r 0·297; P = 0·01; general health subscales: r 0·249; P = 0·04).
Standardised β-coefficients reported from multiple regression analysis for associations between adherence to a MedDiet and HRQoL subscales are highlighted in Table 2. Using the pooled data from both study cohorts, adherence to a MedDiet was positively associated with physical function (β = 0·263; 95 % CI 0·010, 0·038; P = 0·001), vitality (β = 0·253; 95 % CI 0·010, 0·041; P = 0·002) and general health (β = 0·251; 95 % CI 0·010, 0·045; P = 0·002). However, this level of significance was only maintained for the general health subscale in the fully adjusted model when the Bonferroni-adjusted correction was applied general health (β = 0·223; 95 % CI 0·006, 0·044; P = 0·001).
Table 2. Multiple regression coefficients expressing associations between adherence to a Mediterranean diet and subscales of HRQoL by cohort
(standardised β-coefficients)*
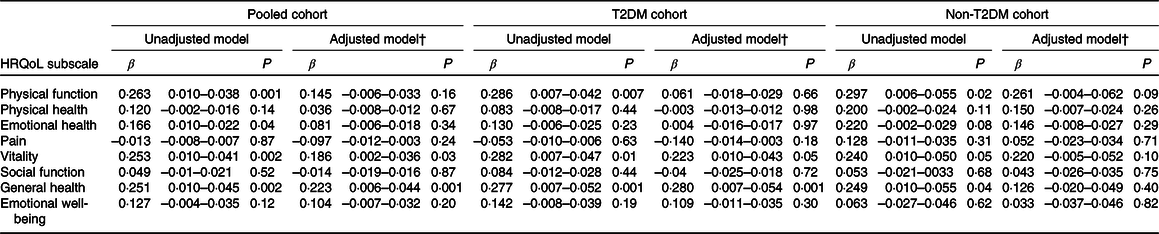
HRQoL, health-related quality of life; T2DM, type 2 diabetes mellitus.
P refers to significant associations between adherence to a Mediterranean diet and various subscales of health-related quality of life.
* β-coefficient represents a 1-unit increase in the MEDAS score per change in outcome measure (subscale of health-related quality of life).
† Adjusted for age, sex, hand-grip strength, gait speed and ALM index.
When multiple regression was applied independently by cohort, after adjustment for potential confounders, adherence to a MedDiet was positively associated with general health in the T2DM cohort only (β = 0·280; 95 % CI 0·007, 0·054; P = 0·001) (Table 2). When the Bonferroni-adjusted correction was applied, no additional significant associations between adherence to a MedDiet and HRQoL subscales were observed in both the T2DM and non-T2DM cohorts.
Discussion
In the present study, we showed that adherence to a MedDiet was positively associated with the general health subscale of HRQoL, which was most apparent in middle-aged to older adults with T2DM. However, these findings should be treated with caution given our small sample size and the lack of high adherence to a MedDiet within the study cohort.
Our findings are consistent with previous literature supporting an association between adherence to a MedDiet and subscales of HRQoL(Reference Henríquez Sánchez, Ruano and de Irala29,Reference Bonaccio, Di Castelnuovo and Bonanni40–Reference Galilea-Zabalza, Buil-Cosiales and Salas-Salvadó42) . Unlike our findings, cross-sectional analysis of the PREDIMED-Plus study(Reference Galilea-Zabalza, Buil-Cosiales and Salas-Salvadó42) showed that greater adherence to a MedDiet was independently associated with HRQoL across all eight subscales in overweight and obese males and females at high risk of CVD. Furthermore, cross-sectional analysis from two independent population-based surveys from Spain(Reference Muñoz, Fíto and Marrugat41) showed that adherence to a MedDiet was significantly associated with the aggregated mental component score of HRQoL. Similar findings were also reported in a population-based cohort of 16 937 Italian men and women(Reference Bonaccio, Di Castelnuovo and Bonanni40). However, unlike the aforementioned studies, we examined the relationship between adherence to a MedDiet and each individual subscales of HRQoL, rather than the two aggregated physical and mental component scores.
To date, most of these positive associations are limited to Mediterranean populations. Nevertheless, Perez-Tasigchana et al. (Reference Pérez-Tasigchana, León-Muñoz and López-García30) reported no clinically relevant association between adherence to a MedDiet and better HRQoL after 2 years of follow-up in two independent cohorts of community-dwelling older adults from Spain. Additional studies on older adults from non-Mediterranean populations are limited. In a cohort of 2457 community-dwelling Australian adults aged between 55 and 65 years, Milte et al. (Reference Milte, Thorpe and Crawford43) reported few associations between MedDiet adherence and HRQoL. Although this may be due to lower adherence scores, reflecting the difficulties of adopting a Mediterranean-style diet in non-Mediterranean populations, making comparisons among the available literature is somewhat challenging due to the heterogeneity in the dietary adherence scores applied across different studies. All of the aforementioned studies assessed adherence to a MedDiet using either the Mediterranean Diet Score developed by Trichopoulou et al. (Reference Trichopoulou, Costacou and Bamia25) or the MEDAS, which was used in the present study. Unlike the MEDAS tool, which is based on normative criteria and reflective of a Mediterranean-style diet, assessing adherence using the Mediterranean Diet Score is dependent on the usual dietary characteristics of the studied population and may not reflect true adherence to a MedDiet, particularly in non-Mediterranean populations(Reference Martínez-González, Hershey and Zazpe44).
Despite the current evidence suggesting a positive association between adherence to a MedDiet and self-perceived HRQoL, the exact mechanisms in support of such findings are poorly understood. Akin with previous research on the proposed health benefits of the MedDiet, the most coherent theory relates to the potential synergistic relationship of nutrients within the dietary pattern, and the inverse relationship with chronic disease risk through the attenuation of oxidative stress and inflammation(Reference Dinu, Pagliai and Casini28,Reference Galbete, Schwingshackl and Schwedhelm45,Reference Tosti, Bertozzi and Fontana46) . The MedDiet is recognisable by a high intake of vegetables, fruits, nuts, legumes, wholegrains and the daily use of extra-virgin olive oil; a moderate intake of fish, shellfish, wine and fermented dairy products; and low consumption of meat and meat products, processed cereals, sweets, vegetable oils and butter(Reference Mantzioris and Villani26,Reference Willett, Sacks and Trichopoulou47,Reference Davis, Bryan and Hodgson48) . Being predominately plant based, the MedDiet is naturally low in saturated fat and rich in several functional components, including, vitamins and minerals, carotenoids, unsaturated fatty acids and phenolic compounds, depicted by antioxidant and anti-inflammatory properties(Reference Trichopoulou, Martínez-González and Tong49). Moreover, the efficacy of the MedDiet has also been linked with improved depressive symptomology(Reference Jacka, O’Neil and Opie50,Reference Parletta, Zarnowiecki and Cho51) , cognitive function(Reference Wade, Davis and Dyer52,Reference Martínez-Lapiscina, Clavero and Toledo53) and inversely associated with central adiposity(Reference Bendall, Mayr and Opie54), frailty and functional decline(Reference McClure and Villani55,Reference Kojima, Avgerinou and Iliffe56) , all of which can negatively impact HRQoL in middle-aged and older adults. Therefore, it is plausible that any observed relationship between adherence to a MedDiet and HRQoL is secondary to a reduction in disease risk or improvements in the management of clinical perturbations. Nevertheless, many of these effects, including reductions in blood pressure, cholesterol and improved glycaemic control, are indeed asymptomatic, and their impact on HRQoL may not be clinically significant(Reference Pérez-Tasigchana, León-Muñoz and López-García30).
Although our results support that adherence to a MedDiet in middle-aged and older adults with T2DM is associated with self-perceived general health, these results may indeed be overstated. Specifically, reverse causation is plausible; as such, participants with a better HRQoL may indeed have healthier dietary patterns. As of consequence, the association that we report might be bi-directional. Furthermore, our results should be treated with caution given that a decline HRQoL in vulnerable older adults, such as those with T2DM, is intuitively evident. Therefore, the use of generic HRQoL instruments, such as the 36-item short-form health survey, may not identify the true consequences that are unique to older adults with chronic disease on individual quality of life subscales. Nevertheless, an important strength of this study is that we adjusted for important covariates including functional markers (hand-grip strength and gait speed) and ALM index. This is an important consideration given that there is previous evidence of an increased risk of mobility disability and poor muscle quality in older adults with T2DM(Reference Volpato, Bianchi and Lauretani57), thus increasing the risk of falls and fractures(Reference Scott, Seibel and Cumming58,Reference Yeung, Reijnierse and Pham59) , hospitalisation(Reference Beaudart, Zaaria and Pasleau60,Reference Zhao, Zhang and Hao61) and ultimately poor HRQoL(Reference Beaudart, Locquet and Reginster62,Reference Manrique-Espinoza, Salinas-Rodríguez and Rosas-Carrasco63) .
The main limitation of our study is the cross-sectional nature of our research, which therefore limits the establishment of causality. Specifically, it is plausible that participants altered their dietary behaviour towards a more healthful dietary pattern following a diagnosis of T2DM; although non-significant, in the present study the T2DM cohort reported greater adherence to a MedDiet compared with the non-T2DM cohort. Nevertheless, adherence scores in the present study were considered low-to-moderate at best. As such, this limits the generalisability of our findings given the lack of high adherents to a MedDiet. Furthermore, although our multiple regression analysis was indeed adjusted, residual confounding cannot be ruled out, including physical activity levels, level of education and socio-economic status, all of which can impact HRQoL. Moreover, our sample was small and not generalisable to the wider population of older adults with and without chronic disease. Lastly, dietary intake data and the 36-item short-form health survey instrument were self-reported. Despite all questionnaires being administered by a member of the research team, recall or social desirability bias may still exist.
In conclusion, in community-dwelling middle-aged and older adults with T2DM, we showed that adherence to a MedDiet was positively associated with the general health subscale of HRQoL. Although we are unable to rule out reverse causation, regardless of its effects on HRQoL, a Mediterranean-style diet should be promoted among older adults to support healthy ageing due to its efficacy on reducing the risks associated with multiple chronic diseases. Nevertheless, these findings should be further evaluated using larger cohorts of older participants with a wider range of adherence scores, particularly higher adherence, using a longitudinal study design while controlling for important confounders to ascertain the direction of the relationship.
Acknowledgements
The authors thank our participants for their time and efforts that made this study possible. The authors are also grateful to Michelle Barrett for her valuable contribution towards the data collection.
This work was supported by funding from the School of Health and Behavioural Sciences at the University of the Sunshine Coast and a stipend awarded to RM from the Sunshine Coast Local Medical Association.
A. V. and R. M. were responsible for the study conception, design and data collection. A. C. was responsible for statistical analysis, interpretation of the findings and drafting the final manuscript. A. V. was responsible for statistical analysis, interpretation of the findings and drafting the final manuscript. R. M. was responsible for the interpretation of the findings and drafting the final manuscript. All authors have read and approved the final manuscript.
There are no conflicts of interest.







