Dear editor
The study presented by Melsew et al., is quite interesting as authors described risk factors for infectiousness of patients with tuberculosis (TB) [Reference Melsew1]. One of the most important risk factor is cavitary lesion. Contacts of TB patients with the cavitary disease were around twice as likely to be infected as contacts of patients without cavitation. In TB endemic countries such as Taiwan, how to prevent the transmission of TB is an important issue and treats as early as possible to these patients who has high probability of pulmonary TB is urgent. However, misdiagnosis will lead to poor outcome.
The global impact of TB is extremely important, considering that an estimated 9.0 million people developed TB in 2013 and 1.5 million died from the disease, according to the World Health Organization (WHO) global TB report 2014. Taiwan is also an endemic country for TB. Generally speaking, the most common radiographic manifestation of post-primary pulmonary TB is focal or patchy heterogeneous, poorly defined consolidation involving the apical and posterior segments of the upper lobes and the superior segments of the lower lobes [Reference Lau2, Reference Nachiappan3]. Cavitary lesions are often seen within areas of consolidation and may be multifocal [Reference Krysl4]. In addition, cavity is always high contagious and easy transmission [Reference Melsew1, Reference Zhang5]. Besides, according to our previous study, diabetes mellitus (DM) was regarded as the most important risk factor for pulmonary TB in Taiwan [Reference Wang6]. Since the slow growth characteristics of Mycobacteria tuberculosis, in order to avoid diseases spreading, many physicians in Taiwan always prescribed empiric anti-TB agents to these patients who had such radiographic presentation in DM patients though negative for acid-fast bacillus (AFB) smear. However, this treatment strategy is not always a right way.
A 70-year-old male smoker with poor controlled DM and hypertension, presented to our chest out-patient department with productive cough and blood tinged sputum for about 2 months in April 2017. The chest radiograph (Fig. 1a) and high-resolution computed tomography (HRCT) both showed two consolidations with cavity lesions over left upper lung. In addition, multiple enlarged lymph nodes over his mediastinum were also noted. No leukocytosis, normal liver and renal function but a very high serum HbA1c level (11.2%) indicated a very poorly controlled DM. Negative for AFB stain from his sputum specimens and bronchoscopy also disclosed negative result for smear of AFB and M. tuberculosis polymerase chain reaction from the bronchoalveolar lavage (BAL). Though lacks microbiology evidence, his clinical presentations and underlying disease strongly indicated pulmonary TB.
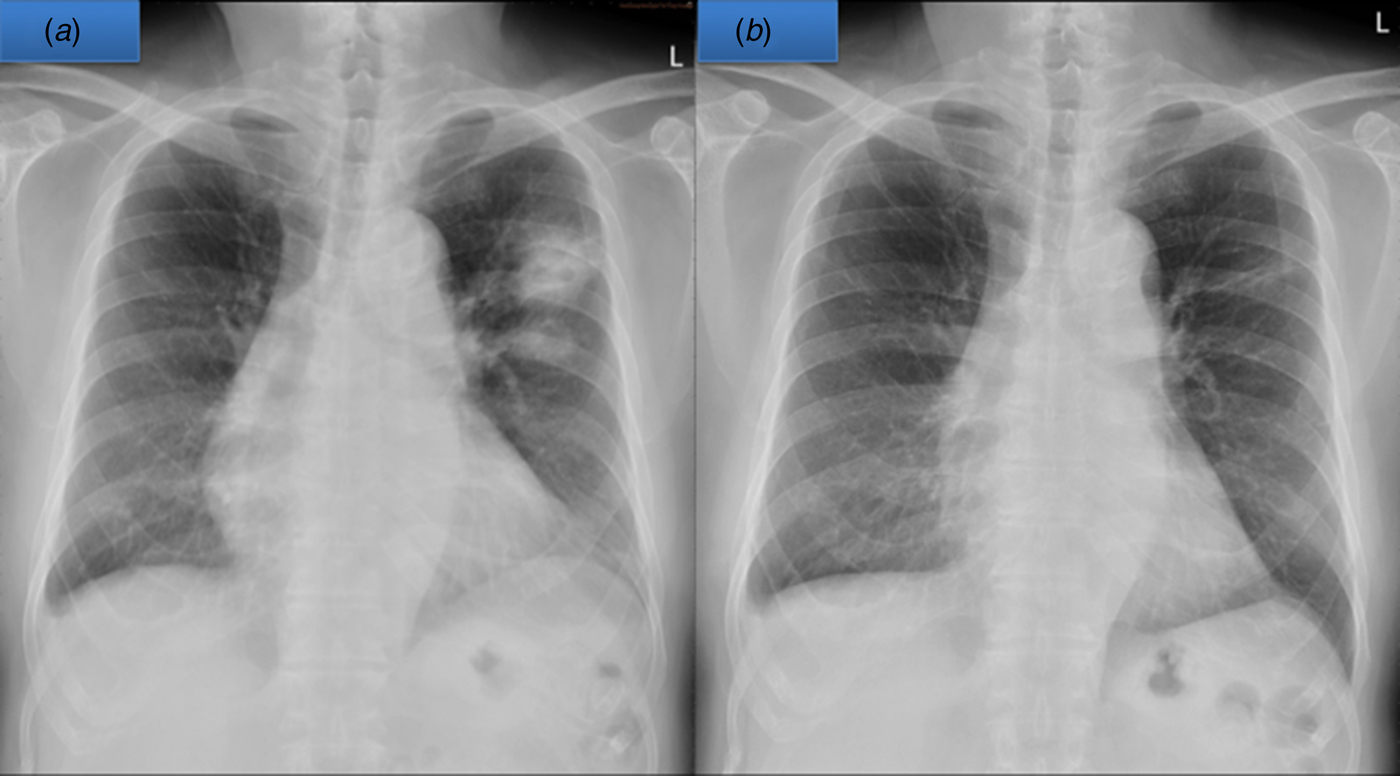
Fig. 1. The chest radiograph (a) showed two consolidations with cavity lesions over left upper lung and dramatically resolved after oral steroid for 2 weeks (b).
In order to get the real aetiology, CT guided biopsy was arranged and the pathology revealed organising pneumonia. We started oral prednisolone 30 mg/day and his pulmonary cavity lesions had been dramatically improved 2 weeks later (Fig. 1b).
Typical upper lobe infiltrates maybe seen in 80% patients [Reference Krysl4]. In addition, Cavitation is the radiological hallmark of post-pulmonary TB and among 20–45% of patients [Reference Lau2–Reference Krysl4]. Accumulated evidences shows pulmonary TB with cavities always has higher contagious characteristic because of high burden of M. tuberculosis, especially in DM cases [Reference Zhang5]. To be concerned, since the subsequent several specimens from sputum and BAL all showed negative results, other possible aetiologies should be clarified instead of prescribed empiric anti-TB agent. Therefore pathological proof is mandatory and misdiagnosis will lead to poor outcome. We present this interesting case and share our experience to physicians in TB endemic countries.
Conflict of interest
The authors declare that they have no competing interests.






