Successful infection prevention is often a collaboration between healthcare providers, patients, and caregivers. Patient and caregiver education are vital to the dissemination and implementation of infection prevention efforts;Reference Yokoe, Anderson and Berenholtz1
however, research is limited regarding the contribution of language of care to healthcare-associated infection (HAI) risk or infection prevention implementation. As the infection prevention community addresses inequities within HAI,Reference Henderson, Forde and Haessler2
barriers to care associated with patient language must be overcome to protect patients from preventable harm. Here, we detail examples of how language discordance between the healthcare system and patients and caregivers may increase HAI risk and then present strategies to overcome these challenges.
The United States is a multilingual nation. In 2019, the US Census reported that 22.0% of all households spoke a language other than English and 8% endorse limited English proficiency or emerging English proficiency (EEP).Reference Dietrich and Hernandez3
The US Census defines limited English-proficient individuals as those aged ≥5 years who self-identify as speaking English less than “very well.”4
Due to concern that limited English proficiency does not represent English language proficiency accurately, this commentary will use EEP to describe patients and families with a language of care other than English. Individuals with EEP have worse health outcomes compared to patients with English proficiency.Reference Flores and Tomany-Korman5–Reference Rawal, Srighanthan, Vasantharoopan, Hu, Tomlinson and Cheung8
Patients with EEP have longer lengths of stay (LOS) for hospital admissionsReference John-Baptiste, Naglie and Tomlinson9
and higher rates of unplanned readmissions,Reference Rawal, Srighanthan, Vasantharoopan, Hu, Tomlinson and Cheung8
and they are more likely to experience physical harm when adverse events occur during hospitalization.Reference Divi, Koss, Schmaltz and Loeb6
The impact of patient language on HAI risk remains largely unknown; however, growing evidence indicates that rates of HAI vary by race and ethnicity.Reference Chen, Khazanchi, Bearman and Marcelin10
For example, an analysis of Medicare Patient Safety Monitoring System data found that Asian and Hispanic–Latino patients admitted for cardiovascular disease, pneumonia, and surgery had higher rates of HAI than white, non-Hispanic–Latino patients admitted for the same indications.Reference Bakullari, Metersky and Wang11
The healthcare epidemiology community recognizes the importance of health equity in furthering HAI prevention efforts;Reference Henderson, Forde and Haessler2
multilingual patient communication, education and infection prevention interventions are crucial considerations in reducing disparities in preventable infections.
Written and verbal patient education is essential to HAI prevention, but materials and interventions have not been widely studied in languages other than English. Commonly, patients are given educational materials about infection prevention topics, such as invasive device care, the importance of removing unnecessary devices, and empowering patients to remind staff to use standard infection prevention practices.Reference Macewan, Beal, Gaughan, Sieck and McAlearney12
Patient-centered education interventions have improved staff hand hygiene adherenceReference McGuckin, Taylor, Martin, Porten and Salcido13
and have decreased outpatient central-line–associated bloodstream infections (CLABSIs).Reference Moller, Borregaard, Tvede and Adamsen14
In a recent qualitative study of perceptions of infection prevention education of healthcare leaders and staff, widely reported education resources included booklets, handouts, signs, posters, and electronic medical record (EMR) tools.Reference Macewan, Beal, Gaughan, Sieck and McAlearney12
However, this study did not include language-specific resource questions. Spanish language resources to promote infection prevention and antibiotic stewardship are available from the Centers for Disease Control and Prevention (CDC)15,16
and the Agency for Healthcare Research and Quality (AHRQ);17
however, the number of Spanish language resources is limited in comparison to English materials. To our knowledge, no studies have evaluated the efficacy of non-English infection prevention resources nor are data available regarding their use. Evaluating the implementation and efficacy of non-English resources is essential to identifying areas for improvement in infection prevention communication. Expanding the content of resources as well as the number of languages in which such materials are available is also vital to improving healthcare education for all patients.
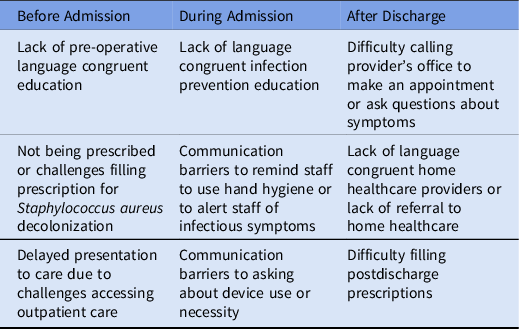
To develop interventions that improve infection prevention for patients with EEP, it is important to address communication barriers and errors throughout preadmission, inpatient, and outpatient care. Communication barriers include lack of access to an interpreter and lack of language congruent healthcare workers. Communication errors include using a family member as an interpreter, not providing written materials in the patient or caregiver’s language of care, and not identifying patients with EEP.Reference Yeheskel and Rawal18
Within infection prevention, communication barriers and errors could affect HAI risk prior to hospitalization, during hospitalization, and after discharge (Table 1). Language incongruent communication between providers and patients may lead to inadequate infection prevention practices, such as not receiving instructions for at-home chlorhexidine bathing or intranasal mupirocin for methicillin-resistant Staphylococcus aureus (MRSA) nasal decolonization. A prior study demonstrated low adherence (62%) to preoperative S. aureus decolonization,Reference Caffrey, Woodmansee and Crandall19
but whether patient language was associated with low decolonization adherence was not assessed. Further research inclusive of multilingual research participants is needed to identify potential barriers to preoperative infection prevention practices.
Table 1. Examples of How Barriers to Communication and Communication Errors Can Impair Infection Prevention Implementation Before, During and After Hospital Admission
During admission to the hospital, patients and families with EEP may be unable to self-advocate (eg, remind a healthcare worker to wash their hands). English language instructions may not effectively prepare patients with EEP for discharge, which could affect self-care for an indwelling device or surgical wound. In a multihospital qualitative study, Latino parents with EEP reported feelings of being underprepared and overwhelmed prior to their child’s neonatal intensive care unit (NICU) discharge.Reference Munoz-Blanco, Boss, DeCamp and Donohue20
Similarly, a multihospital study found that adults with EEP were less likely to report comprehension of discharge follow-up and medication class and purpose than English-proficient patients.Reference Karliner, Auerbach, Nápoles, Schillinger, Nickleach and Pérez-Stable21
In qualitative studies, Spanish-speaking patients frequently cited lack of outpatient language services as a barrier to healthcare.Reference Calo, Cubillos and Breen22,Reference DeCamp, Kieffer and Zickafoose23
The lack of outpatient language support may make it difficult for individuals with EEP to schedule an outpatient follow-up or contact a clinician with questions about a medical device or surgical site issue. Pharmacies frequently cannot provide verbal or written non-English instructions,Reference Bradshaw, Tomany-Korman and Flores24
potentially impeding access to postoperative antibiotics or preoperative mupirocin for S. aureus decolonization, for example. These obstacles to patient education, communication, and care create a cumulative risk for HAI.
The role of language and infection prevention education has received limited attention; however, in small, mostly single-centered studies, patients with EEP have worse infection-related outcomes. Jacobs et alReference Jacobs, Prasad, Fang, Abe-Jones and Kangelaris25
found that non-white and non-Black patients with EEP had an increased risk of mortality from sepsis, after adjusting for demographics, clinical characteristics, and disease severity. In a study of children admitted to the hospital who required intravenous antibiotics, patients with EEP had a longer length of stay and were less likely to have a home healthcare referral.Reference Levas26
In a recent case-controlled study of CLABSIs in critically ill children, Woods-HillReference Woods-Hill, Srinivasan, Schriver, Haj-Hassan, Bezpalko and Sammons27
et al found that non-English language approached significance as an independent risk factor for CLABSI. Kalluri et alReference Kalluri, Melvin, Belfort, Gupta, Cordova-Ramos and Parker28
performed a retrospective cohort study of premature infants admitted to 9 NICUs and found that infants of mothers speaking a language other than English or Spanish had increased risk of late-onset sepsis, after adjusting for hospital, comorbidities, race, and ethnicity. Assuming that multilingual patient education, tools, and interventions were not optimized in these studies, these findings suggest that without supports, individuals with EEP may be at disproportionately higher risk for both infection and morbidity from infection.
Identifying and quantifying the impact of language on HAI is an important first step, but creating solutions to communication barriers is critical. Expanding language services improves quality of care and outcomes for patients with EEP. Access to professional interpreters or bilingual staff improves provider communication,Reference Moreno, Tarn and Morales29,Reference Gutman, Cousins and Gritton30
patient satisfaction with communication,Reference Moreno and Morales31
and patient understanding of their diagnosis and treatment.Reference Moreno, Tarn and Morales29,Reference Baker32
Professional interpreter use is not only mandated for healthcare systems receiving federal aid33,34
but also reduces communication errorsReference Flores, Laws and Mayo35
and decreases unplanned readmissions.Reference Karliner, Pérez-Stable and Gregorich36
Despite being aware of the benefits of professional interpreters, providers report frequent use of ad hoc interpreters.Reference Fox, Godage and Kim37,Reference Diamond, Schenker, Curry, Bradley and Fernandez38
In 2013, only 68% of hospitals in the United States provided interpreter services.Reference Schiaffino, Nara and Mao39
Barriers and solutions to multilingual infection prevention education have not been studied; however, lessons can be learned from prior research. Table 2 cites examples of existing research on language congruent care with examples of how such strategies may reduce HAI risk. Potential interventions include multilingual patient resources, expanded interpreter services, and recruiting multilingual healthcare workers in the inpatient and outpatient environments. These interventions can be accomplished through utilizing existing patient education materials, such as those available through AHRQ17
and the CDC,15
as well as AHRQ guidance for improving interpreter services.40
In addition, patient education tools should be produced in a wide range of languages and there needs to be increased research on the utilization, acceptability, and effectiveness of non-English infection prevention education. Patient- and family-centered teaching methods, such as a question-prompt lists, have been shown to have acceptability and feasibility among Spanish-speaking familiesReference Munoz-Blanco, Boss, DeCamp and Donohue20
and should be evaluated as tools for infection prevention education. Clinicians should partner with patients and families with EEP in developing infection prevention resources and interventions to ensure that these tools are practical and acceptable prior to implementation. To improve care for patients at a diverse range of hospitals, national organizations and government agencies should continue to expand non-English infection prevention resources. Healthcare providers and epidemiologists can also advocate for improved interpreter services, for reimbursement for interpreter services, and for including EEP resources in HAI bundles.
Table 2. Existing Research on Language Congruent Care Outcomes, Quality Improvement and Implementation, With Examples of Similar Strategies to Improve Healthcare-Associated Infection Outcomes
We acknowledge that many factors that we have not addressed in this study contribute to health inequities and infection risk. A growing body of work indicates that antibiotic stewardship is also a critical area of health equity research and intervention. In a retrospective analysis of a single health system’s urgent-care antibiotic prescribing patterns, nonwhite, Hispanic–Latino, and non-English–speaking patients were less likely to receive a prescription for antibiotics compared with white, non-Hispanic/Latino, English-speaking patients.Reference Seibert, Hersh and Patel41
Additional research is needed to identify the impact of patient language on antibiotic prescribing and counselling. There are many barriers to qualified language interpreter use, including financial. Despite the improved healthcare outcomes associated with language congruent care, providers frequently cite cost as a barrier to interpreter use.Reference Shah, Velasquez and Song42
Insurance payments for interpreter services has been a proposed health policy for almost 20 years; nevertheless, very few insurance plans pay for interpreter staff or services.Reference Shah, Velasquez and Song42,Reference Ku and Flores43
Policy changes are required to support provider use of interpreters. Although our proposed strategies may improve patient infection prevention education, a multidisciplinary approach is required to address the many drivers of inequitable care for patients with EEP.
Conducting rigorous research among communities with EEP requires specific skills and experience. As the healthcare epidemiology and infection prevention community begins to examine the impact of language on HAIs, we should engage our colleagues with expertise in health equity and language. Partnering with researchers from a wide range of disciplines, providers, patients and families with EEP is crucial for developing interventions that successfully address any found inequities contributing to HAI risk. Language is an integral component of infection prevention. Providing language congruent care, through educational resources, strengthened interpreter services, and multilingual healthcare workers, is essential to protect all patients from preventable harm.







Successful infection prevention is often a collaboration between healthcare providers, patients, and caregivers. Patient and caregiver education are vital to the dissemination and implementation of infection prevention efforts;Reference Yokoe, Anderson and Berenholtz1 however, research is limited regarding the contribution of language of care to healthcare-associated infection (HAI) risk or infection prevention implementation. As the infection prevention community addresses inequities within HAI,Reference Henderson, Forde and Haessler2 barriers to care associated with patient language must be overcome to protect patients from preventable harm. Here, we detail examples of how language discordance between the healthcare system and patients and caregivers may increase HAI risk and then present strategies to overcome these challenges.
The United States is a multilingual nation. In 2019, the US Census reported that 22.0% of all households spoke a language other than English and 8% endorse limited English proficiency or emerging English proficiency (EEP).Reference Dietrich and Hernandez3 The US Census defines limited English-proficient individuals as those aged ≥5 years who self-identify as speaking English less than “very well.”4 Due to concern that limited English proficiency does not represent English language proficiency accurately, this commentary will use EEP to describe patients and families with a language of care other than English. Individuals with EEP have worse health outcomes compared to patients with English proficiency.Reference Flores and Tomany-Korman5–Reference Rawal, Srighanthan, Vasantharoopan, Hu, Tomlinson and Cheung8 Patients with EEP have longer lengths of stay (LOS) for hospital admissionsReference John-Baptiste, Naglie and Tomlinson9 and higher rates of unplanned readmissions,Reference Rawal, Srighanthan, Vasantharoopan, Hu, Tomlinson and Cheung8 and they are more likely to experience physical harm when adverse events occur during hospitalization.Reference Divi, Koss, Schmaltz and Loeb6 The impact of patient language on HAI risk remains largely unknown; however, growing evidence indicates that rates of HAI vary by race and ethnicity.Reference Chen, Khazanchi, Bearman and Marcelin10 For example, an analysis of Medicare Patient Safety Monitoring System data found that Asian and Hispanic–Latino patients admitted for cardiovascular disease, pneumonia, and surgery had higher rates of HAI than white, non-Hispanic–Latino patients admitted for the same indications.Reference Bakullari, Metersky and Wang11 The healthcare epidemiology community recognizes the importance of health equity in furthering HAI prevention efforts;Reference Henderson, Forde and Haessler2 multilingual patient communication, education and infection prevention interventions are crucial considerations in reducing disparities in preventable infections.
Written and verbal patient education is essential to HAI prevention, but materials and interventions have not been widely studied in languages other than English. Commonly, patients are given educational materials about infection prevention topics, such as invasive device care, the importance of removing unnecessary devices, and empowering patients to remind staff to use standard infection prevention practices.Reference Macewan, Beal, Gaughan, Sieck and McAlearney12 Patient-centered education interventions have improved staff hand hygiene adherenceReference McGuckin, Taylor, Martin, Porten and Salcido13 and have decreased outpatient central-line–associated bloodstream infections (CLABSIs).Reference Moller, Borregaard, Tvede and Adamsen14 In a recent qualitative study of perceptions of infection prevention education of healthcare leaders and staff, widely reported education resources included booklets, handouts, signs, posters, and electronic medical record (EMR) tools.Reference Macewan, Beal, Gaughan, Sieck and McAlearney12 However, this study did not include language-specific resource questions. Spanish language resources to promote infection prevention and antibiotic stewardship are available from the Centers for Disease Control and Prevention (CDC)15,16 and the Agency for Healthcare Research and Quality (AHRQ);17 however, the number of Spanish language resources is limited in comparison to English materials. To our knowledge, no studies have evaluated the efficacy of non-English infection prevention resources nor are data available regarding their use. Evaluating the implementation and efficacy of non-English resources is essential to identifying areas for improvement in infection prevention communication. Expanding the content of resources as well as the number of languages in which such materials are available is also vital to improving healthcare education for all patients.
To develop interventions that improve infection prevention for patients with EEP, it is important to address communication barriers and errors throughout preadmission, inpatient, and outpatient care. Communication barriers include lack of access to an interpreter and lack of language congruent healthcare workers. Communication errors include using a family member as an interpreter, not providing written materials in the patient or caregiver’s language of care, and not identifying patients with EEP.Reference Yeheskel and Rawal18 Within infection prevention, communication barriers and errors could affect HAI risk prior to hospitalization, during hospitalization, and after discharge (Table 1). Language incongruent communication between providers and patients may lead to inadequate infection prevention practices, such as not receiving instructions for at-home chlorhexidine bathing or intranasal mupirocin for methicillin-resistant Staphylococcus aureus (MRSA) nasal decolonization. A prior study demonstrated low adherence (62%) to preoperative S. aureus decolonization,Reference Caffrey, Woodmansee and Crandall19 but whether patient language was associated with low decolonization adherence was not assessed. Further research inclusive of multilingual research participants is needed to identify potential barriers to preoperative infection prevention practices.
Table 1. Examples of How Barriers to Communication and Communication Errors Can Impair Infection Prevention Implementation Before, During and After Hospital Admission
During admission to the hospital, patients and families with EEP may be unable to self-advocate (eg, remind a healthcare worker to wash their hands). English language instructions may not effectively prepare patients with EEP for discharge, which could affect self-care for an indwelling device or surgical wound. In a multihospital qualitative study, Latino parents with EEP reported feelings of being underprepared and overwhelmed prior to their child’s neonatal intensive care unit (NICU) discharge.Reference Munoz-Blanco, Boss, DeCamp and Donohue20 Similarly, a multihospital study found that adults with EEP were less likely to report comprehension of discharge follow-up and medication class and purpose than English-proficient patients.Reference Karliner, Auerbach, Nápoles, Schillinger, Nickleach and Pérez-Stable21 In qualitative studies, Spanish-speaking patients frequently cited lack of outpatient language services as a barrier to healthcare.Reference Calo, Cubillos and Breen22,Reference DeCamp, Kieffer and Zickafoose23 The lack of outpatient language support may make it difficult for individuals with EEP to schedule an outpatient follow-up or contact a clinician with questions about a medical device or surgical site issue. Pharmacies frequently cannot provide verbal or written non-English instructions,Reference Bradshaw, Tomany-Korman and Flores24 potentially impeding access to postoperative antibiotics or preoperative mupirocin for S. aureus decolonization, for example. These obstacles to patient education, communication, and care create a cumulative risk for HAI.
The role of language and infection prevention education has received limited attention; however, in small, mostly single-centered studies, patients with EEP have worse infection-related outcomes. Jacobs et alReference Jacobs, Prasad, Fang, Abe-Jones and Kangelaris25 found that non-white and non-Black patients with EEP had an increased risk of mortality from sepsis, after adjusting for demographics, clinical characteristics, and disease severity. In a study of children admitted to the hospital who required intravenous antibiotics, patients with EEP had a longer length of stay and were less likely to have a home healthcare referral.Reference Levas26 In a recent case-controlled study of CLABSIs in critically ill children, Woods-HillReference Woods-Hill, Srinivasan, Schriver, Haj-Hassan, Bezpalko and Sammons27 et al found that non-English language approached significance as an independent risk factor for CLABSI. Kalluri et alReference Kalluri, Melvin, Belfort, Gupta, Cordova-Ramos and Parker28 performed a retrospective cohort study of premature infants admitted to 9 NICUs and found that infants of mothers speaking a language other than English or Spanish had increased risk of late-onset sepsis, after adjusting for hospital, comorbidities, race, and ethnicity. Assuming that multilingual patient education, tools, and interventions were not optimized in these studies, these findings suggest that without supports, individuals with EEP may be at disproportionately higher risk for both infection and morbidity from infection.
Identifying and quantifying the impact of language on HAI is an important first step, but creating solutions to communication barriers is critical. Expanding language services improves quality of care and outcomes for patients with EEP. Access to professional interpreters or bilingual staff improves provider communication,Reference Moreno, Tarn and Morales29,Reference Gutman, Cousins and Gritton30 patient satisfaction with communication,Reference Moreno and Morales31 and patient understanding of their diagnosis and treatment.Reference Moreno, Tarn and Morales29,Reference Baker32 Professional interpreter use is not only mandated for healthcare systems receiving federal aid33,34 but also reduces communication errorsReference Flores, Laws and Mayo35 and decreases unplanned readmissions.Reference Karliner, Pérez-Stable and Gregorich36 Despite being aware of the benefits of professional interpreters, providers report frequent use of ad hoc interpreters.Reference Fox, Godage and Kim37,Reference Diamond, Schenker, Curry, Bradley and Fernandez38 In 2013, only 68% of hospitals in the United States provided interpreter services.Reference Schiaffino, Nara and Mao39 Barriers and solutions to multilingual infection prevention education have not been studied; however, lessons can be learned from prior research. Table 2 cites examples of existing research on language congruent care with examples of how such strategies may reduce HAI risk. Potential interventions include multilingual patient resources, expanded interpreter services, and recruiting multilingual healthcare workers in the inpatient and outpatient environments. These interventions can be accomplished through utilizing existing patient education materials, such as those available through AHRQ17 and the CDC,15 as well as AHRQ guidance for improving interpreter services.40 In addition, patient education tools should be produced in a wide range of languages and there needs to be increased research on the utilization, acceptability, and effectiveness of non-English infection prevention education. Patient- and family-centered teaching methods, such as a question-prompt lists, have been shown to have acceptability and feasibility among Spanish-speaking familiesReference Munoz-Blanco, Boss, DeCamp and Donohue20 and should be evaluated as tools for infection prevention education. Clinicians should partner with patients and families with EEP in developing infection prevention resources and interventions to ensure that these tools are practical and acceptable prior to implementation. To improve care for patients at a diverse range of hospitals, national organizations and government agencies should continue to expand non-English infection prevention resources. Healthcare providers and epidemiologists can also advocate for improved interpreter services, for reimbursement for interpreter services, and for including EEP resources in HAI bundles.
Table 2. Existing Research on Language Congruent Care Outcomes, Quality Improvement and Implementation, With Examples of Similar Strategies to Improve Healthcare-Associated Infection Outcomes
Note. EEP, emerging English proficiency; HAI, healthcare-acquired infection.
We acknowledge that many factors that we have not addressed in this study contribute to health inequities and infection risk. A growing body of work indicates that antibiotic stewardship is also a critical area of health equity research and intervention. In a retrospective analysis of a single health system’s urgent-care antibiotic prescribing patterns, nonwhite, Hispanic–Latino, and non-English–speaking patients were less likely to receive a prescription for antibiotics compared with white, non-Hispanic/Latino, English-speaking patients.Reference Seibert, Hersh and Patel41 Additional research is needed to identify the impact of patient language on antibiotic prescribing and counselling. There are many barriers to qualified language interpreter use, including financial. Despite the improved healthcare outcomes associated with language congruent care, providers frequently cite cost as a barrier to interpreter use.Reference Shah, Velasquez and Song42 Insurance payments for interpreter services has been a proposed health policy for almost 20 years; nevertheless, very few insurance plans pay for interpreter staff or services.Reference Shah, Velasquez and Song42,Reference Ku and Flores43 Policy changes are required to support provider use of interpreters. Although our proposed strategies may improve patient infection prevention education, a multidisciplinary approach is required to address the many drivers of inequitable care for patients with EEP.
Conducting rigorous research among communities with EEP requires specific skills and experience. As the healthcare epidemiology and infection prevention community begins to examine the impact of language on HAIs, we should engage our colleagues with expertise in health equity and language. Partnering with researchers from a wide range of disciplines, providers, patients and families with EEP is crucial for developing interventions that successfully address any found inequities contributing to HAI risk. Language is an integral component of infection prevention. Providing language congruent care, through educational resources, strengthened interpreter services, and multilingual healthcare workers, is essential to protect all patients from preventable harm.
Acknowledgments
Financial support
This work was supported in part by National Institutes of Health grants (T32 AI052071) to E.P. and (K24 AI141580) to A.M.
Conflicts of interest
All authors report no conflicts of interest relevant to this article.