Introduction
Suicide is a major public health concern with death by suicide increasing worldwide, especially amongst younger people (Gureje et al., Reference Gureje, Oladeji, Hwang, Chiu, Kessler, Sampson, Alonso, Andrade, Beautrais, Borges, Bromet, Bruffaerts, de Girolamo, de Graaf, Gal, He, Hu, Iwata, Karam, Kovess-Masféty, Matschinger, Moldovan, Posada-Villa, Sagar, Scocco, Seedat, Tomov and Nock2011; World Health Organization, 2014). Approximately 800 000 people die by suicide annually, and it is the leading cause of death for males and females aged 20–34 years in the UK (World Health Organization, 2017; Office for National Statistics, 2020). However, our understanding of factors influencing suicidal behaviours is limited, and it is of vital importance to understand who is most at risk to better target interventions. Mental ill-health is one of the strongest predictors of suicide risk, with approximately 90% of those who attempt or complete suicide meeting diagnostic criteria for a mental disorder (Cavanagh et al., Reference Cavanagh, Carson, Sharpe and Lawrie2003; Bertolote et al., Reference Bertolote, Fleischmann, De Leo and Wasserman2004; Windfuhr and Kapur, Reference Windfuhr and Kapur2011). A recent systematic review concluded that the risk of suicide-related thoughts (SRTs) and suicide-related behaviours (SRBs), including suicide attempts, is significantly increased in those exposed to paternal SRTs and SRBs, or parental suicide (Goodday et al., Reference Goodday, Shuldiner, Bondy and Rhodes2019). Earlier studies of adopted children and twin studies posit that these associations are driven by genetic risk factor transmission (Qin et al., Reference Qin, Agerbo and Mortensen2002; Sørensen et al., Reference Sørensen, Mortensen, Wang, Juel, Silverton and Mednick2009; Gureje et al., Reference Gureje, Oladeji, Hwang, Chiu, Kessler, Sampson, Alonso, Andrade, Beautrais, Borges, Bromet, Bruffaerts, de Girolamo, de Graaf, Gal, He, Hu, Iwata, Karam, Kovess-Masféty, Matschinger, Moldovan, Posada-Villa, Sagar, Scocco, Seedat, Tomov and Nock2011), but more recent evidence highlights the significant role of exposure to adverse childhood experiences including parental psychopathology (Wender et al., Reference Wender, Kety, Rosenthal, Schulsinger, Ortmann and Lunde1986; Glowinski et al., Reference Glowinski, Bucholz, Nelson, Fu, Madden, Reich and Heath2001; Roy and Segal, Reference Roy and Segal2001). However, there is a paucity of research on the association between parental mental health (MH) and death by suicide among offspring.
The World Health Organization's MH surveys suggest that parental mental ill-health increases the risk of offspring suicide, though this was based not only on self-report of five ‘MH’ conditions including major depression, panic disorder and generalised anxiety disorder, but also substance dependence and antisocial behaviour (e.g. illegal behaviour, arrest and imprisonment) (Gureje et al., Reference Gureje, Oladeji, Hwang, Chiu, Kessler, Sampson, Alonso, Andrade, Beautrais, Borges, Bromet, Bruffaerts, de Girolamo, de Graaf, Gal, He, Hu, Iwata, Karam, Kovess-Masféty, Matschinger, Moldovan, Posada-Villa, Sagar, Scocco, Seedat, Tomov and Nock2011). A Danish population cohort study observed a two-fold increase in suicide risk amongst offspring of parents with a history of psychiatric inpatient admissions, with a six-fold increase when both rather than one parent was affected (Webb et al., Reference Webb, Pickles, Appleby, Mortensen and Abel2007). Two other Danish population-based case–control studies also identified parental psychiatric admission or suicide as substantial risk factors for suicide risk in offspring, and a Swedish case–control study showed that the offspring of parents with schizophrenia had a significantly increased risk of suicide, even after accounting for socio-economic status and offspring mental illness (Agerbo et al., Reference Agerbo, Nordentoft and Mortensen2002; Stenager and Qin, Reference Stenager and Qin2008; Ljung et al., Reference Ljung, Lichtenstein, Sandin, D'Onofrio, Runeson, Långström and Larsson2013, Reference Ljung, Lichtenstein, Sandin, D'Onofrio, Runeson, Långström and Larsson2013). However, although the current body of evidence suggests a significant association between parental psychopathology and offspring suicide risk, the derivation of parental MH status from psychiatric inpatient records limits the generalisability of these findings, potentially excluding individuals with less severe mental ill-health conditions and as such, the relationship between more common psychopathologies and offspring MH and suicide risk has yet to be elucidated (Mittendorfer-Rutz et al., Reference Mittendorfer-Rutz, Rasmussen and Wasserman2008).
Aims
The aims of this study were to identify the entire population of parents enumerated in the 2011 Census and examine their MH, and the MH and subsequent suicide risk amongst their offspring. During the study period, Northern Ireland had the highest age-standardised rate of suicide across the UK and Ireland, with 17.8 suicide deaths/100 000 compared to 11.8 and 12.1/100 000, respectively, making it an important setting for targeted suicide research and the advancement of suicide prevention strategies (ONS, 2013; Central Statistics Office, 2014; NISRA, 2017). This is the first population-wide cohort study analysing the risk of poor MH and suicide in offspring given parental MH status in the UK.
Methods
This population-wide cohort study linked 2011 Census returns and mortality records to determine whether living with parents reporting poor MH is linked to offspring's self-reported poor MH, or increased risk of death by suicide.
Data sources
The Northern Ireland Mortality Study (NIMS) links mortality records from the General Register's Office (GRO) to Census returns for the entire enumerated population. The Census is a mandatory questionnaire administered to all households in NI decennially and collects information on household characteristics and individual-level data on the demographics, health, education and employment of residents via self-report. NIMS and the linkage processes are described elsewhere (O'Reilly et al., Reference O'Reilly, Rosato, Catney, Johnston and Brolly2012). For this study the March 2011 Census returns were linked with mortality records from the GRO until the end of 2016, allowing for 69 months of follow-up. The linked data were anonymised, held in a registered secure environment for analysis by the research team. The use of the NIMS for research was approved by the Office for Research Ethics Committees Northern Ireland (ORECNI).
Identifying parents
The Census contains information on both individuals and on household structure enabling the identification of parent-child relationships. We limited the analysis to individuals living with a parent, regardless of age so households containing children and at least one parent were flagged and all other households dropped from the analysis. To clarify the association between MH of parents and children without the potential additional influence of grandparent MH, households in which children were identified as being parents themselves were excluded from the analysis. This resulted in the exclusion of 10 584 individuals.
Cohort attributes
All personal characteristics of parents and children were drawn from the Census, as were other cohort attributes known to be associated with poor MH and suicide risk such as religion (Protestant, Roman Catholic, Other/none), physical illness (‘Are your day to day activities limited because of a health problem or disability which has lasted, or is expected to last, at least 12 months?’ Respondents could identify ‘Yes, limited a lot’, ‘Yes, limited a little’ or ‘No’), and socioeconomic status, which was assessed using a combination of housing tenure and the capital value of the property (Cohen et al., Reference Cohen, Forbes and Garraway1995). Tenure was Census-based (owner occupiers, private renting or social renting); Capital value had been derived by Land and Property Services which determined the level of local tax payable by each household. These data were linked and combined with tenure to produce an eight-fold classification defining tenure/taxable value of the property (private renting; social renting; and for owner-occupiers, five groups ranging from less than £75k to over £250k) (Table 1).
Table 1. Demographic characteristics of individuals who live at home with at least one parent and percentage of those who have ⩾1 parent with poor mental health (n = 618 970)
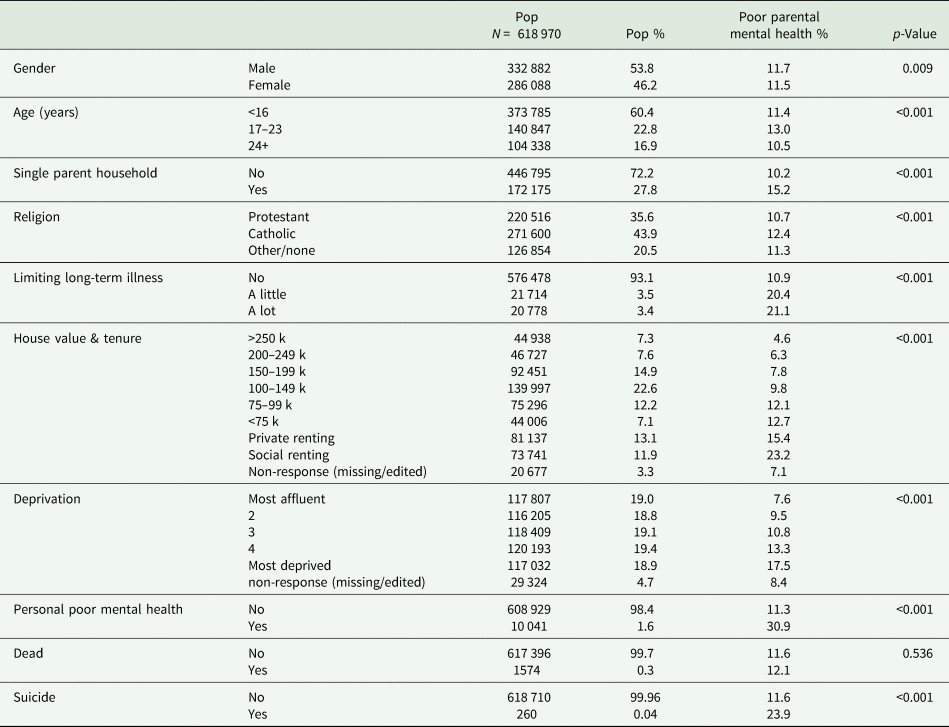
χ 2 test of independence examining the relationship between offspring demographic characteristics and poor parental health.
Area characteristics
Area-level deprivation was assigned using the ‘Income’ domain of the Northern Ireland Index of Multiple Deprivation (NIMDM) which is based on the proportion of residents on means-tested benefits (Northern Ireland Statistics and Research Agency, 2010). Areas were defined as 890 homogenous groups of approximately 2000 individuals and were ranked from least deprived to most deprived, then split into equal quintiles.
MH status
The 2011 Census in Northern Ireland was unique in the UK in that it asked a detailed question on the presence of chronic health conditions. Individuals were asked ‘Do you have any of the following conditions which have lasted, or are expected to last, at least 12 months?’ and asked to tick all of a range of conditions that applied (Wright et al., Reference Wright, Rosato and O'Reilly2017). Those who identified as having ‘An emotional, psychological or MH condition (such as depression or schizophrenia)’ were defined as having poor MH. This indicator has face validity based on its demographic distribution which mirrors known associations with MH, correlational validity as it is associated with receipt of psychotropic medication, and predictive validity as it is a strong predictor of death by suicide (Tseliou et al., Reference Tseliou, Maguire, Donnelly and O'Reilly2015; Rosato et al., Reference Rosato, Tseliou and O'Reilly2019; Onyeka et al., Reference Onyeka, O'Reilly and Maguire2021).
Mortality data
Information on the date and cause of deaths between April 2011 and December 2016 were based on official death records and linked probabilistically to the Census data as described in detail elsewhere (O'Reilly et al., Reference O'Reilly, Rosato and Connolly2008). In keeping with usual practice in the UK, suicide deaths included both deaths recorded as ‘suicide’ and deaths classified as ‘undetermined intent’ (ICD-10 code: X60-X84; Y10-Y34; Y87.0; Y87.2) (Linsley et al., Reference Linsley, Schapira and Kelly2001).
Analysis strategy
The Census identified children residing with their parents and whether 0, 1 or 2 of their parents reported poor MH. Descriptive statistics recorded the socio-demographic characteristics and variations in health status and mortality of individuals stratified according to parental MH. Logistic regression compared the risks associated with both poor MH and suicide given parental MH status. Ordinary Logistic Regression assumes that the residuals are independent. The ‘cluster’ option in Stata 15.1 was used to account for the fact that the observations are clustered into households and may therefore be correlated within households, but independent between. This was enabled by the presence of a unique Census household identifier. Sensitivity analyses were carried out stratifying the children in younger (0–23 years) and older (⩾24 years) age groups to determine if the associations differed given the age of the child resident with their parent. This stratification differentiates between adults (⩾24 years) and children/young people (⩽23years). Whilst there is no universally accepted definition of ‘adolescence’ the United Nations defines adolescence as 15–24 years (United Nations, 2020). For this study it is assumed that by the age 24 years most young people should have completed education and be living independently.
Results
Characteristics of households with at least one parent with poor MH
The final cohort comprised 618 970 offspring living with their parents at the time of the 2011 Census. In total, 71 632 children (11.6%) were living with at least one parent who reported poor MH; 66 936 children (10.8%) were living with only one parent with poor MH, while 4696 (0.76%) were living with two parents with poor MH. The prevalence of parental poor MH was higher in single-parent families (15.2% vs 10.2%) (Table 1). Households affected by poor parental MH were characteristically more socially deprived, and were more than twice as common amongst families living in the more disadvantaged areas (17.5% vs 7.6%) and five times as common for families living in socially rented accommodation compared to those in larger owner-occupied homes (23.2% vs 4.6%).
Offspring MH and relationship to parental MH
Although the majority of children lived in households not affected by poor parental MH, almost 1-in-8 children (11.6%) lived with one or more parents with poor MH. A total of 10 041 (1.6%) children reported poor MH and almost a third also lived with a parent with poor MH. Offspring poor MH was more prevalent in those living with a parent who reported poor MH compared to those who did not report poor MH (4.3% vs 1.3%). However, the majority of children living with a parent with poor mental did not report poor MH (95.7%).
In an unadjusted logistic regression model (Table 2), children living with one parent with poor MH were three-times more likely to report poor MH compared to children of parents not reporting poor MH (OR = 3.36, 95% CI 3.20–3.52). This increased to six-fold where both parents had poor MH (OR = 6.04, 95% CI 5.34–6.83). This association was marginally attenuated with further adjustment for sociodemographic factors and offspring physical illness. In the fully adjusted model, offspring living in households where one parent had poor MH had almost three-times the odds of also having poor MH compared to their peers whose parents who did not report poor MH (OR = 2.79, 95% CI 2.64–2.95), increasing to five-fold when both parents had poor MH (OR = 5.25, 95% CI 4.57–6.02).
Table 2. Logistic regression models determining the odds of poor mental health given parental mental health status
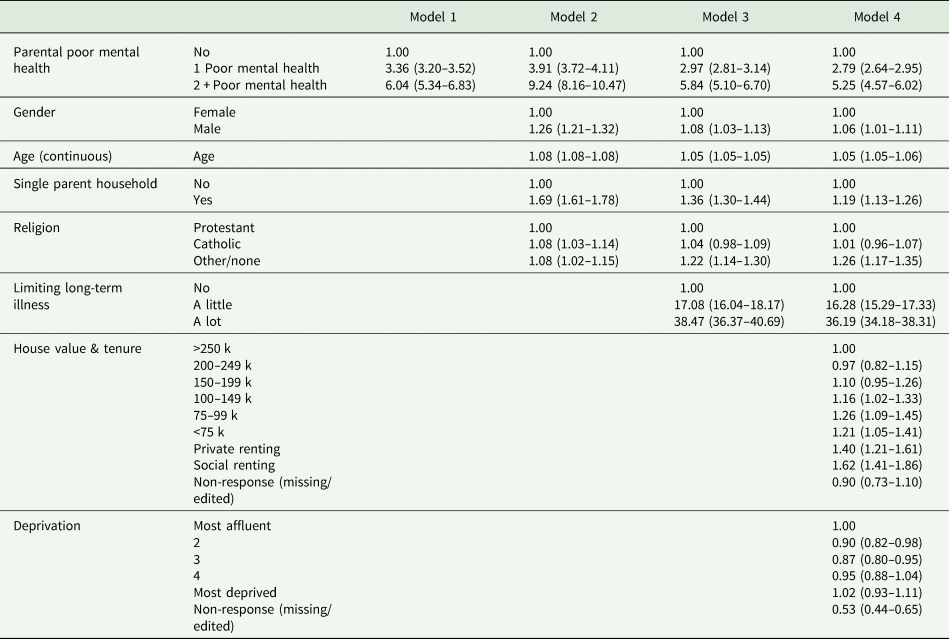
Figures represent odds ratios (95% confidence intervals).
Further examination showed that the association between parental and offspring MH was not related to offspring age (online Supplementary Table 1). The ORs of poor MH for offspring under 24 years were OR = 2.64 (95% CI 2.43–2.86) for those living with one parent with poor MH, and OR = 5.23 (95% CI 4.31–6.36) for those living with two parents with poor MH. For those aged 24 years or over, the ORs were OR = 2.53 (95% CI 2.33–2.74) and OR = 4.90 (95% CI 3.95–6.08), respectively.
Although a stratified analysis revealed slightly increased odds of offspring with poor MH where the mother rather than the father was the parent affected by poor MH (OR = 2.84, 95% CI 2.67–3.03 and OR = 2.63, 95% CI 2.38–2.92 respectively), this difference was not statistically significant (online Supplementary Table 2).
Parental MH and offspring suicide risk
During follow-up, 1574 of our offspring cohort died, 260 (16.5%) by suicide. Of those who died by suicide, 18.5% had reported personal poor MH in the Census and 23.8% had been living in a household where at least one parent had poor MH. The fully adjusted logistic regression model (online Supplementary Table 3) showed that the biggest risk factors for suicide amongst offspring were male sex (ORadj 4.70; 95% CI 3.28–6.73) and having poor personal MH (ORadj 4.31; 95% CI 2.72–6.85). However, there was also a significant association between parental MH and offspring suicide risk. In the unadjusted model (Table 3), the odds of suicide where one parent had poor MH were twice that observed for those living in households who did not report parental poor MH (OR = 2.36, 95% CI 1.75–3.16), and this increased to OR = 2.95 (95% CI 1.21–7.16) where both parents had poor MH. These risks were moderately attenuated with further adjustment for sociodemographic characteristics and physical ill-health, to 1.94 (95% CI 1.45–2.60) and 2.59 (95% CI 1.06–6.32) respectively. The final model shows that the relationship between parental MH and offspring suicide persisted even after adjustment for offspring MH (one parent affected: OR = 1.76, 95% CI 1.31–2.36, two parents affected: OR = 2.18, 95% CI 0.89–5.34).
Table 3. Logistic regression models determining the odds of death by suicide given parental mental health status and sex of affected parent
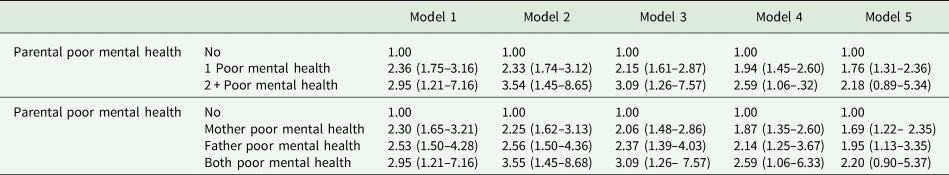
Figures represent odds ratios (95% confidence intervals).
Model 1: unadjusted.
Model 2: + gender, age in years (continuous), single-parent household, and religion.
Model 3: + limiting long-term illness.
Model 4: + house value and tenure, and deprivation quintile.
Model 5: + personal mental health status.
The risk of suicide in offspring did not differ significantly according to which parent was affected, the risk being ORadj = 1.95 (95% CI 1.13–3.35) when the father had poor MH, compared to ORadj = 1.69 (95% CI 1.22–2.35) for those living with a mother with poor MH.
157 deaths by suicide were recorded among the 514 475 (0.03%) individuals aged under 24 years, whilst 103 suicides were reported among the 104 235 (0.1%) individuals aged 24 + years. Further stratification of logistic regression models revealed a differential impact of parental MH on suicide risk by age of offspring (Table 4). Amongst those aged under 24 years, the odds of suicide were increased 1.5-fold (ORadj = 1.54, 95% CI 1.06–2.25) where one parent had poor MH, increasing to ORadj = 2.80 (95% CI 1.02–7.65) where both parents reported poor MH. However, the observed association between poor parental MH and offspring suicide was much lower and not statistically significant in those aged 24+ years (one parent affected: OR = 1.37, 95% CI 0.83–2.26, two parents affected: OR = 0.73, 95% CI 0.10–5.24).
Table 4. Logistic regression models determining the odds ratios of death by suicide given parental mental health status, stratified by age
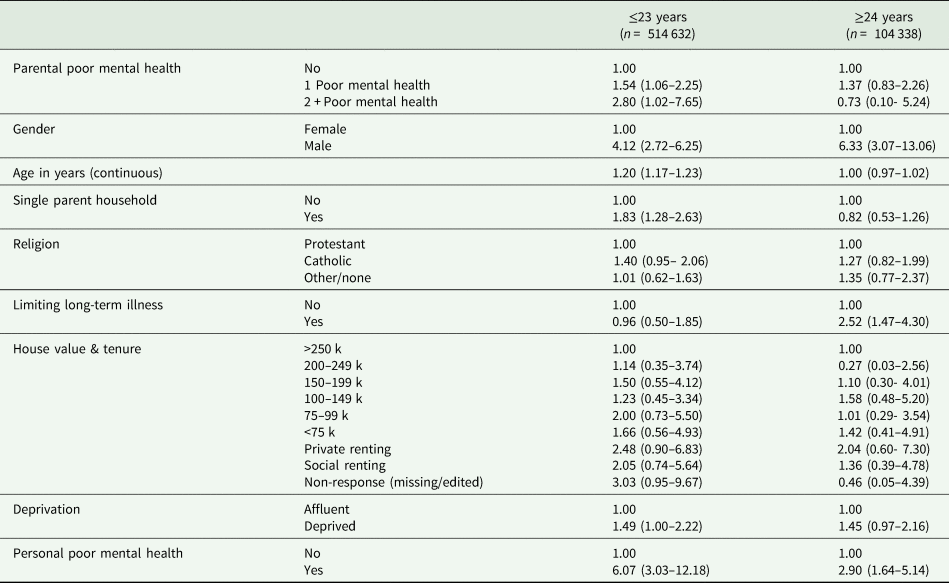
Figures represent odds ratios (95% confidence intervals).
Discussion
This population-wide study demonstrates that living with a parent with poor MH is associated with a significantly increased risk of offspring with poor MH and death by suicide. Almost one-in-eight children in NI were living with at least one parent with poor MH and these individuals were twice as likely to die by suicide, even after accounting for physical health, household socio-economic status and personal MH status.
Effect of parental MH on child MH
Although the aetiology of child psychopathology is multifactorial, the available literature indicates that exposure to parental psychopathology is a key determinant of mental disorders in children (McLaughlin et al., Reference McLaughlin, Gadermann, Hwang, Sampson, Al-Hamzawi, Andrade, Angermeyer, Benjet, Bromet, Bruffaerts, Caldas-de-Almeida, de Girolamo, de Graaf, Florescu, Gureje, Haro, Hinkov, Horiguchi, Hu, Karam and Kessler2012; Rasic et al., Reference Rasic, Hajek, Alda and Uher2014; Bellina et al., Reference Bellina, Grazioli, Garzitto, Mauri, Rosi, Molteni, Brambilla and Nobile2020). In the current study, there was a very strong relationship between the MH of parents and co-resident children, with children almost three-times more likely to report poor MH when one parent had poor MH, increasing to a 5-fold increase when both parents reported poor MH. This compares favourably with the existing body of literature; in a recent meta-analysis, Rasic et al., observed more than a two-fold increase in the risk of mental disorders in offspring of parents with severe mental illness, with even larger estimates observed for offspring with schizophrenia and bipolar disorder (Rasic et al., Reference Rasic, Hajek, Alda and Uher2014). Direct comparison of the current study is however challenging given the methodological heterogeneity across studies, including disparities in the measures used to identify mental illness, the age of offspring examined and the MH condition examined. Many of the previous studies also lacked statistical power or information on the MH status of the second parent.
In the last decade, our understanding of potential mechanisms for the familial transmission of mental illness has advanced with the emergence of genetically informed studies. Systematic reviews provide substantial evidence of the genetic transmission of MH disorders, including schizophrenia and depression (McAdams et al., Reference McAdams, Neiderhiser, Rijsdijk F, Narusyte, Lichtenstein and Eley2014; Jami et al., Reference Jami, Hammerschlag, Bartels and Middeldorp2021), though it is also clear that psychopathology may be transmitted through the shared rearing environment and through unique parent-child interactions. Parenting practices and family functioning have been highlighted as the primary drivers of environmental transmission of psychopathology and these factors are strongly correlated with offspring psychological wellbeing, with healthy offspring development heavily dependent on parental health and wellbeing (Berg-Nielsen et al., Reference Berg-Nielsen, Vikan and Dahl2002; Bradley and Vandell, Reference Bradley and Vandell2007; Bellina et al., Reference Bellina, Grazioli, Garzitto, Mauri, Rosi, Molteni, Brambilla and Nobile2020). In this administrative data-based study we were unable to contribute any insight into whether the increased risk for poor MH is a direct result of a shared genetic susceptibility, or an indirect effect of the impact of parental poor MH on the child's upbringing, from exposure to common stressors, witnessing mental ill-health episodes or the subsequent parenting style or parental involvement.
Effect of parental MH on child suicide
Personal poor MH remained the strongest independent risk factor for death by suicide in offspring even after adjustment for parental MH, contributing to more than a three-fold increase in the odds of suicide compared to those who did not report poor MH. This observation is consistent with findings from Danish studies where an up to 39-fold increase in the risk of suicide in offspring with a personal psychiatric hospitalisation was observed (Stenager and Qin, Reference Stenager and Qin2008; Sørensen et al., Reference Sørensen, Mortensen, Wang, Juel, Silverton and Mednick2009). Although a smaller magnitude of the effect was observed in this study, it is highly plausible that the identification of poor MH from a community-based self-reported measure would capture individuals with a wider range of mental ill-health conditions, including those considered less severe when compared to those requiring psychiatric inpatient admission, as is the case in the majority of studies examining this association. It is universally recognised by the authors of these studies that most cases with mild to moderate mental disorders are diagnosed and treated by general practitioners and will not be observed in such centralised psychiatric registers (Mors et al., Reference Mors, Perto, Preben and Mortensen2011).
The aetiology of the increased risk of mental illness and increased suicide risk in offspring of parents with mental illness are closely interlinked. Support for the implication of genetic transmission of risk for suicidal behaviours has been provided using a variety of study methodologies, including family studies, twin studies and adoptive studies (Mirkovic et al., Reference Mirkovic, Laurent, Podlipski, Frebourg, Cohen and Gerardin2016). Examination of the available evidence indicates significant heritability of suicide, estimated at an aggregated 45%, but this is highly dependent on the presence of psychiatric illness (Mirkovic et al., Reference Mirkovic, Laurent, Podlipski, Frebourg, Cohen and Gerardin2016). In addition, a wide range of environmental factors has been indicated in the development of suicidal behaviours, with the majority of studies attributing the increased risk to a wide range of early adverse experiences including maltreatment, interpersonal loss (e.g. parental death, separation) socio-economic adversity and family dysfunction (e.g. parental mental illness, domestic violence, incarceration) (Sahle et al., Reference Sahle, Reavley, Li, Morgan, Yap, Reupert and Jorm2021). Alterations in family functioning and parenting capacity owing to psychiatric illness may in turn increase exposure to these adverse childhood experiences, conferring a greater risk of internalising and externalising behaviours in exposed offspring(Hughes et al., Reference Hughes, Bellis, Hardcastle, Sethi, Butchart, Mikton, Jones and Dunne2017; Petruccelli et al., Reference Petruccelli, Davis and Berman2019), which are important risk factors for SRTs and behaviours among young people (Goodday et al., Reference Goodday, Shuldiner, Bondy and Rhodes2019).
We observed an elevated risk of suicide where both parents reported poor MH, which corroborates with Webb et al., who noted a 6-fold increase in offspring suicide where two parents had a recorded psychiatric inpatient record, compared to a 2–3-fold increase in those with one affected parent (Webb et al., Reference Webb, Pickles, Appleby, Mortensen and Abel2007). While this may represent increased genetic potential it is also plausible that exposure to two parents with poor MH would also result in greater impairment of parenting capacity and a more dysfunctional family home environment. In order to disentangle this relationship, studies which account for possible genetic influences, such as adoption and children-of-twins designs are necessary. However, suicide is both a rare and sensitive outcome, thus achieving sufficient power to provide robust risk estimates is challenging, even in large population-wide studies.
Whilst the association between parental and offspring MH persisted for both younger and older offspring, the relationship between parental MH and offspring suicide remained significant only for those aged under 24 years. Few studies have examined the impact of parental psychopathology across sensitive life periods in children and adolescents, but this finding, together with those of Niederkotenthaler et al. (Niederkrotenthaler et al., Reference Niederkrotenthaler, Floderus, Alexanderson, Rasmussen and Mittendorfer-Rutz2012) support the hypothesis that early exposure to parental psychopathology during neuro-developmentally sensitive periods may increase risk of suicide. It is also plausible that the impact of environmental influences, including parental psychopathology, on offspring MH and suicidality may decrease with increasing age and independence from the family unit. It is also important to note that these older individuals may have moved out of the family home during follow-up, therefore lessening the observed parental-offspring associations. However, given that the confidence intervals were wide and cross unity, this observation may be the result of insufficient statistical power to detect the true association between the number of parents who reported poor MH and suicide risk among offspring aged 24+ years.
Studies suggest that the risk of suicide varies according to the parent affected. A recent systematic review concluded that the risk of SRBs and death by suicide in children was higher when it was the mother rather than the father who had poor MH though, for death by suicide alone the evidence for a differential impact of parental sex was less conclusive (Goodday et al., Reference Goodday, Shuldiner, Bondy and Rhodes2019). In two case–control studies using national registers in Denmark, maternal psychiatric hospitalisation was associated with a minimally increased risk of offspring suicide compared to those with a record of paternal psychiatric hospitalisation(Webb et al., Reference Webb, Pickles, Appleby, Mortensen and Abel2007; Stenager and Qin, Reference Stenager and Qin2008), and in a Swedish population-based case–control study, maternal schizophrenia was associated with slightly higher odds of offspring suicide than paternal schizophrenia (Ljung et al., Reference Ljung, Lichtenstein, Sandin, D'Onofrio, Runeson, Långström and Larsson2013). However, it is unclear whether the differential risk estimates observed in these studies were statistically significantly different. The current study does not resolve the issue. The elevated risk of offspring with poor MH was marginally greater for individuals living with a mother with poor MH, but conversely, the risk of offspring suicide was greater to in those living with a father with poor MH. Previous research on parenting and child psychopathology suggests that although the quality of paternal-child relationships strongly predicts the emotional and behavioural outcomes of offspring, the impact of maternal influence supersedes that of the father, presumably as the primary burden of parental care is adopted by the mother (Flouri, Reference Flouri2010).
Strengths and limitations
This population-wide cohort study provided a unique opportunity to examine the relationship between parental MH and offspring psychopathology and suicide risk in a typically hard to reach population. The self-reported indicator of poor MH encompassed a wider range of psychopathology than studies based on admission to a psychiatric hospital, making these findings more generalisable to the wider body of individuals with mental ill-health. Although admission data has the benefit of high specificity, it excludes the much larger proportion of psychiatric ill-health that is managed in the community. Additionally, population surveys which use validated diagnostic instruments, though arguably the most accurate measurement of MH, are resource intensive, require a clinical application or specialist interviewer training and cannot cover more than a small proportion of the population. However, as the Census measure used included only those with conditions that had or were expected to last at least twelve months, people with less protracted episodes of poor MH will not have been included. Furthermore, a self-report measure, while democratising the identification process, is subject to reporting bias especially related to the continuing stigma surrounding mental illness. However, this indicator has face validity based on its demographic distribution which mirrors known associations with MH, correlational validity as it is associated with receipt of psychotropic medication, and predictive validity as it is a strong predictor of death by suicide (Tseliou et al., Reference Tseliou, Maguire, Donnelly and O'Reilly2015; Rosato et al., Reference Rosato, Tseliou and O'Reilly2019; Onyeka et al., Reference Onyeka, O'Reilly and Maguire2021).
As parental and offspring MH were measured at the same time point, establishing causal order by accounting for reverse causality was not possible. There is likely some degree of bidirectionality to this association, however, the association persisted with adjustment for person MH status, and only 1.62% of children reported poor MH despite 11.6% living with an affected parent, providing some indication of the direction of the association. This also limited the statistical modelling to logistic regression, however, there is an argument that when the outcome is rare and the follow-up period is short, the regression coefficients obtained through logistic regression approximate those obtained through Cox regression (Green and Symons, Reference Green and Symons1983; Ingram and Kleinman, Reference Ingram and Kleinman1989; Ingram et al., Reference Ingram, Kleinman and Mock1990). Finally, while Census-based studies provide population coverage, they lack depth and additional information on important household factors, such as substance dependencies in parents or exposure to adverse childhood experiences which would have contributed to our understanding of factors that may mediate these associations. Owing to the study design, it was not possible to examine the extent to which the observed parent-offspring associations could be explained by shared genetic factors. As such, further investigation into the mechanisms underpinning these associations is warranted.
Conclusion
Parental poor MH is strongly associated with offspring suicide risk even after adjustment for personal MH status, especially in children aged under 24 years. However, personal MH remains the greatest predictor of suicide risk. Given the high prevalence of parental psychopathology in households in Northern Ireland, early identification of children and families at excess risk is crucial in the treatment of mental ill-health and the prevention of suicide. These findings indicate that the wider household effects of poor MH should be taken into consideration when treating parents with mental illness and treatment plans should consider potential interventions for their children also, particularly in families with children under 24 years.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S2045796022000063.
Data
The de-identified research dataset was made available only to the approved research team within the secure setting at the Northern Ireland Statistics and Research Agency (NISRA).
Acknowledgements
The help provided by the staff of the Northern Ireland Longitudinal Study/Northern Ireland Mortality Study (NILS/NIMS) and the NILS Research Support Unit is acknowledged. The NILS/NIMS is funded by the Health and Social Care Research and Development Division of the Public Health Agency (HSC R&D Division) and NISRA. The NILS-RSU is funded by the ESRC and the Northern Ireland Government. The authors alone are responsible for the interpretation of the data and any views or opinions presented are solely those of the author and do not necessarily represent those of NISRA/NILS.
Financial support
This study was funded by the Administrative Data Research Centre Northern Ireland (ADRC-NI) (Grant ES/S00744X/1).
Conflict of interest
None.
Ethical standards
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.








