Background
The purpose of translational science is to positively impact population health, with the goal of effective research products (programs, practices, and interventions) being widely implemented in real-world clinical and public health settings. Reference Brownson, Colditz and Proctor1 This process inevitably requires users of research to identify, adopt, and normalize new policies and practices within complex, real-world contexts. Reference May, Mair and Finch2 Implementation science describes this process, identifies the multi-level factors influencing it, and informs efforts to make it happen more readily, more equitably, and on a broader scale. Because of this, implementation science offers a compelling value proposition to translational science, namely, as a tool for accelerating translation and achieving health impact. Reference Lobb and Colditz3,Reference Leppin, Mahoney and Stevens4
The field of implementation science includes both implementation research and practice. Implementation research consists of generating knowledge about how to implement research products in specific settings (e.g., schools, health departments, and clinical settings). Implementation research is primarily the work of implementation researchers and (as in community-based participatory research Reference Wallerstein and Duran5 ) the stakeholders with whom they partner in the process of learning. Implementation practice focuses on applying knowledge about implementation to guide process change. It is primarily the work of implementation practitioners, Reference Albers, Metz and Burke6 a diverse group of non-academic stakeholders (e.g. public health practitioners, healthcare providers, policymakers, leaders from community-based organizations, and other implementation support practitioners Reference Metz, Albers and Burke7 ) Implementation research and practice represent two ends of a “studying-to-doing-implementation continuum” that overlap in important ways. Indeed, research and practice continuously inform and shape one another, and each depend on individuals with common implementation competencies in order to be carried out effectively.
Translational science stakeholders—particularly National Institutes of Health-funded Clinical and Translational Science Award (CTSA) Hubs—are actively seeking to develop and support resources and infrastructures that can optimize both implementation research and practice. Prior efforts have described the rationale and need for this activity broadly and highlighted workforce shortages and lack of implementation science expertise as key barriers to progress. Reference Dolor, Proctor, Stevens, Boone, Meissner and Baldwin8 As such, efforts are underway to recruit, teach, and train an implementation science workforce.
Current educational infrastructures may be well positioned for teaching and training either implementation researchers (e.g., as in degree-granting graduate programs) or practitioners (e.g., as in continuous professional development) in somewhat siloed ways, but few institutions can adequately teach both. Even fewer organizations have the capacity to train researchers and practitioners in a way that prepares them to work together synergistically and as collaborators within the same learning systems and contexts. CTSAs—embedded in academic health centers and comprising cores dedicated to education and community engagement—have this potential.
Leveraging this opportunity, we propose an approach for teaching and training implementation that is specifically targeted to the goals, strengths, and infrastructure of CTSAs. We call this approach Teaching For Implementation (TFI). TFI is grounded in the idea that translational science stakeholders should focus on both equipping a research workforce to generate knowledge about implementation and improving the capacity of learning healthcare systems and other clinical, public health, and community contexts to more effectively implement research in practice. It emphasizes that, as it relates to implementation, both the science and practice are integral to successfully changing the healthcare system and improving care quality and impact. Reference Churruca, Ludlow, Taylor, Long, Best and Braithwaite9
In this paper, we—members of the Advancing Dissemination and Implementation Sciences in CTSAs Workgroup—introduce the TFI Framework and show how teachers for implementation and related educational stakeholders can use it to tailor their educational targets, content, and pedagogy to meet the needs of real-world translational contexts and systems.
Teaching for Implementation
The TFI Framework
TFI is based on the goals of fostering both scientific and practical capacity for implementation and increasing the routine application of research knowledge in real-world systems (see Fig. 1). We believe that it is particularly appropriate for CTSAs or other translational infrastructures—learning healthcare systems, practice-based research networks, professional societies—that reach both researcher and practitioner networks and have and train an existing workforce. Below we demonstrate how to operationalize the TFI framework by articulating ‘who’, ‘what’, and ‘how’, one might teach implementation based on its goals. We also describe ways leaders of educational infrastructures can create environments that support a TFI approach.

Fig. 1. The Teaching For Implementation Framework.
Who to Teach for Implementation
Under a TFI approach, the implementation workforce poised to benefit from training consists of all the people needed to carry out implementation-related tasks within a given system or context. An academic medical center, for example, is one system where implementation of research products is relevant. A community experiencing structural barriers to health and healthcare is another. The implementation needs of these and other systems vary greatly, and thus, it is essential that teachers for implementation be familiar with the settings in which their learners will work and understand the unique needs of these contexts. In some cases, it may be helpful or essential to collaborate with system stakeholders in recruiting learners.
When identifying potential students, traditional predictors of academic success (e.g. publications and grants) may be less relevant, particularly when the candidates have strengths that make them uniquely suited for affecting change on the ground. Recruiting students in this way may result in the inclusion of several “non-traditional” learners, including practitioners or administrative leaders that are not interested in obtaining degrees.
For example, many real-world delivery systems leverage the expertise of external implementation support experts in change efforts. Examples include technical assistance providers, implementation coaches, and consultants who often contract with delivery systems but are not embedded in or employed by the systems on a permanent basis. Reference Metz, Albers and Burke7,Reference Wandersman, Duffy and Flaspohler10 These individuals play a critical role in the day-to-day translation of evidence and serve as an important bridge between implementation research and practice. Yet, few formal training opportunities explicitly focused on equipping people for these roles exist. TFI is well suited to meet this growing workforce demand by producing boundary-spanning experts with understanding of both implementation research and practice.
Effective learners of implementation should be motivated by a passion for and commitment to improving health in the real world. Beyond this core similarity, learners can and will differ in many ways. It is incumbent on teachers for implementation to know their students well and to identify the characteristics, motivations, values, priorities, and capacities that distinguish them. Early in this discovery work, teachers for implementation should get a sense of where learners’ aspirations lie on the research-to-practice continuum so that educational opportunities and methods can be tailored to the needs of each learner.
For example, the Mayo Clinic CTSA is currently developing a course in rural health to support implementation efforts in rural settings. The course will be open to any interested learners, including community members. To assist with expectation setting and meeting learners’ unique needs, all students will be required to describe their goals for the course and their perceived role in affecting change in rural health settings. This helps to guide and inform what and how to teach each learner.
What to Teach for Implementation
Ultimately, TFI takes its cues on “what to teach” from the implementation competencies required to operationalize real world, non-academic systems and contexts. We define an “implementation competency” as the capability to apply or use a set of knowledge, skills, or abilities to successfully carry out or perform an implementation-related task or function (e.g. an implementation research or practice task). Indeed, while several efforts have been made to delineate the competencies of implementation scientists Reference Gonzales, Handley, Ackerman and O’Sullivan11–Reference Tabak, Padek and Kerner13 and practitioners Reference Albers, Metz and Burke6,Reference Albers, Metz and Burke14–Reference Metz, Louison, Ward and Burke16 broadly, the implementation competencies TFI prioritizes are those that map to the expressed implementation-related needs of real-world settings. Many of these needs are generic and common to all systems and settings. For example, it is generally true that implementation practitioners in any context will need to be capable of 1.) identifying the research products (e.g., “evidence-based interventions”) that should be implemented, 2.) identifying and communicating the barriers and facilitators to implementation in a particular context, and 3.) developing and deploying strategies for overcoming those barriers and facilitating implementation.
Often, however, health and healthcare delivery systems have unique implementation needs that demand-specific competencies. For example, a public health system seeking to implement cancer screening protocols in diverse communities may require an implementation workforce that is capable of engaging stakeholders in culturally sensitive and responsive ways and using participatory methods. Conversely, large, integrated health systems may value implementers who can analyze electronic health record-based data sets and who are capable of changing organizational cultures. Given this variation, it may be useful for CTSAs to formally evaluate the implementation training needs of their stakeholders. If CTSAs discover that their learners are predominantly beginners, for example, they can focus on offering introductory training that emphasizes core principles. For more varied levels of experience and expertise, a grant-writing course or tailored speaker series may be appropriate and specific areas of interest or need can be emphasized.
Developing comprehensive curriculum and training resources that address the different needs of such diverse systems and learners can be challenging. Reference Chambers, Proctor, Brownson and Straus17 Perhaps because of this, the implementation workforce is often segmented and, consequently, researchers and practitioners often learn different contents in different ways. A tenet of TFI is that it may be valuable for implementation researchers and practitioners to spend at least some time learning together. Co-learning is possible because the competencies of implementation scientists and practitioners overlap in important ways (see Table 1). By leaning into this area of overlap, teachers for implementation can ensure that all learners have a common language and core understanding of key principles in the field. The expectation is that teaching in this way will pay off in the future when the learners and doers of implementation find themselves working together in the real world.
Table 1. Examples of distributing learning objectives for implementation competencies among implementation researchers and practitioners

For example, the UTHealth CTSA provides training on implementation strategy planning using Implementation Mapping Reference Fernandez, Gill and van Lieshout18 and recruits both researchers and practitioners to participate. The training utilizes a problem-based learning approach in which teams are engaged in both planning implementation strategies and their evaluation. Learning in this way provides an opportunity for researchers to apply implementation science concepts while incorporating principles of community engagement and team science, two concepts central to translational research and a focus of CTSAs. It also provides an opportunity for implementation practice stakeholders to learn and apply similar principles while realizing their pragmatic value.
Similarly, Columbia University’s CTSA integrates and provides training in implementation science as part of their community-based participatory research training course that academic researchers and community partners undergo together, and the University of Colorado’s Dissemination and Implementation Science graduate certificate program welcomes both implementation research- and practice-oriented learners.
While a one-size-fits-all approach is not feasible, there are common elements that can ground a single, accessible curricula. Specifically, our collective experience and the literature suggest that a joint research and practice training curriculum should cover the following foundational pillars: 1) what evidence-based interventions (EBIs) and implementation strategies are and how they differ and relate, 2) the role of theories, models, and frameworks in guiding, describing, and evaluating implementation efforts, and 3) basic methods and approaches to doing implementation research, including basic study designs, stakeholder engagement strategies, and implementation outcomes and measures. Reference Proctor and Chambers19
For each of these curricular pillars, there may be both commonalities and differences in what is taught. For example, it may be useful for all implementation trainees to learn about resources and databases for identifying and assessing existing EBIs that might merit implementation. In teaching researchers, however, one might focus more on increasing the learner’s capacity to evaluate the external and internal validity of evidence for interventions based on the literature. On the other hand, implementation practitioners may be better suited by gaining experience with hands-on tools (like The Hexagon Tool Reference Metz and Louison20 ) that can assist with choosing EBIs for specific contexts.
Similarly, when teaching the foundations of implementation research methods, there is value in all learners being aware of the range of study designs that exist, but the emphasis and depth of understanding may need to vary. For example, it may be useful for all learners of implementation to grasp the role of social networks in influencing change. As it relates to this, researchers may need to know how to conduct social network analyses and use specialized analytic software, whereas practitioners might need to know how to identify social network influencers and opinion leaders via informal methods (e.g., by asking participants to nominate influential stakeholders). For other examples of “what to teach” for implementation and how these competencies are differentially applied across the breadth of implementation learners see Table 1.
How to Teach for Implementation
Embracing the diversity and breadth of implementation competencies that real-world systems demand presents clear challenges. Namely, teachers for implementation must grapple with how to match those needs with the diverse strengths, interests, and aspirations of implementation learners. They must also acknowledge their own scope of expertise and its related strengths and limitations. Indeed, no single teacher for implementation is likely to be able to meet all of the educational needs of every learner. Similarly, few learners of implementation will be well-suited by any single training curriculum.
For these reasons, TFI suggests that education be tailored to the unique needs of individual learners. Because few centers have the capacity to meet the diverse needs of all implementation learners, it also requires that students receive help in selecting from existing and external educational offerings. Mentorship is key in this regard and is critical to the effective training of both implementation researchers and practitioners. Reference Padek, Mir and Jacob21–Reference Jacob, Gacad and Pfund23 As it relates to TFI specifically, mentors are often ideally positioned to foster skill development and practical knowledge that are essential to competency attainment. As such, we recommend all learners of implementation have mentors with connections to and experience in the contexts and fields where they intend to work.
Learners should work with these mentors and other teachers for implementation to structure a personalized curriculum that is robust and feasible and that will address key competency gaps. Efforts are underway to catalog and categorize the many educational resources and opportunities that currently exist for both implementation science and practice, which will aid in this process. Here, we present only archetypes of existing training options Reference Chambers, Proctor, Brownson and Straus17,Reference Davis and D’Lima24 to show how they can be used as part of a tailored training plan for different learners (see Table 2).
Table 2. Archetype training options for incorporation in tailored implementation science training plans

Of course, TFI is more than simply making existing training options available to learners. It is also ensuring that those options are delivered in a way that is effective. For some existing training options, it can be difficult to know their target audience, competencies addressed, and methods of teaching. In these situations, it is best to contact and directly inquire of program coordinators. An alternative approach where feasible is to develop and deliver all core implementation curriculum in house and to supplement learners’ specialized and additional needs with focused, external training options. This approach gives teachers for implementation more control over equipping their workforce and ensuring specific needs are met. With that approach in mind, we recommend teachers for implementation develop curricula and programs that are built on contemporary educational philosophy and theory. Especially relevant bodies of work to draw from include those centered on competency-based education, Reference Padek, Colditz and Dobbins12,Reference Cate and Carraccio25–Reference Bloom27 interprofessional education and collaboration, Reference Boon, van Baalen and Groenier28 and online learning strategies. Reference Goodsett29
Teachers for implementation should be strategic but generous with co-learning opportunities for implementation researchers and practitioners. Such opportunities may advance both the science of implementation and its application in practice. For example, while various implementation frameworks describe contextual factors that influence implementation outcomes, the relationships between these factors are not well explicated and an important area of new research. Practitioner–researcher co-learning in this area can help generate hypotheses about these relationships as well as identify leverage points for intervention. As mentioned above, a core curriculum based on the foundations of implementation science is well suited for teaching in a way that will stimulate discovery. Additionally, surveys of implementation scientists and practitioners suggest that several of the most important professional skills they have learned were learned “on-the-job” and after their formal education. Reference Schultes, Aijaz, Klug and Fixsen30 As such, it will only benefit implementation learners to structure educational opportunities that emulate the real world and that allow each member of the interprofessional implementation team to learn and practice their roles.
For example, to teach implementation research methods in a problem-based and multi-professional way, a teacher for implementation might convene a stakeholder panel to speak and answer questions about a key health problem with all learners. Small multidisciplinary groups might then break up to discuss the problem and suggest ways to address it. Researchers may need to draft a protocol or proposal for an implementation study, while practitioners select and pilot pragmatic tools for measuring the impact. The group could then demonstrate what they learned in a shared presentation.
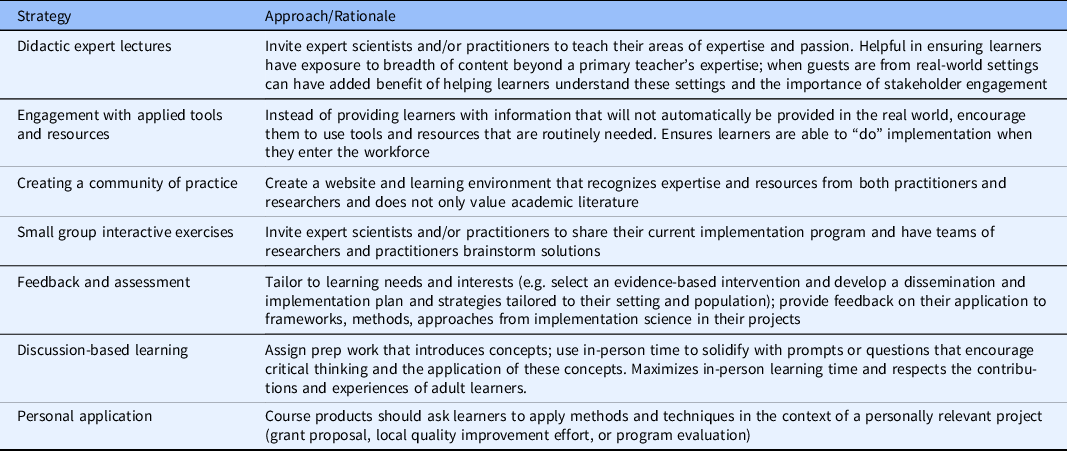
Brief, interactive modules to convey content and teach key principles (e.g., brief videos, “ignite” sessions from experts) may be especially helpful when they are followed by activities that allow learners to apply the material to their own settings and contexts. Existing modules and toolkits that can be used in this way are also available from CTSAs (see https://sites.wustl.edu/wudandi/di-toolkits/ and https://www.youtube.com/channel/UCJhGTpULmVIENeYHPDy-jLg/videos). Other methods and approaches to teaching for implementation based on these principles are presented in Table 3.
Table 3. Example strategies to support teaching for implementation
Supporting Teachers for Implementation
The TFI Framework offers educational direction to stakeholders seeking to hasten implementation of research products in real-world settings. To support a TFI approach CTSAs and similar structures will need to innovate. Innovations may include strategies for making implementation training more consistent and accessible. This may mean offering “courses” that are open to learners that are not formally enrolled in a degree-granting program. These courses could be organized as a certificate program based on a TFI core curriculum while also awarding credit toward researchers’ degrees. Cross-CTSA learning, collaboration, and sharing of resources would be invaluable in developing such a curriculum. Specifically, only a handful of training options explicitly focused on implementation practice currently exist. Reference Proctor and Chambers19 CTSAs are well positioned to address this training gap through collaboration with related disciplines and efforts, such as those centered on healthcare quality improvement.
Finally, work is needed to develop educational models and structures that get learners of implementation out of the classroom and into real-world delivery systems during training. Indeed, it is natural and expected for basic science learners to spend time working in laboratories. The concept of implementation laboratories as avenues for conducting rapid-cycle implementation research would provide training opportunities for researchers and practitioners alike. Extending from learning healthcare systems, implementation laboratories Reference Grimshaw, Ivers and Linklater31 are explicitly focused on conducting pragmatic studies that can generate readily applicable, real-world evidence. From a training perspective, learning laboratories for implementation can provide opportunities for internships and clerkships that would, ideally, be central to a TFI approach. For example, researchers at Mayo Clinic, with pilot funding from its CTSA, partnered with the local Area Agency on Aging and other regional non-profits to develop a collaboration focused on healthy aging program implementation. Reference Leppin, Schaepe and Egginton32,Reference Leppin, Okamoto and Organick33 To foster learning within this “collaboratory,” Doctorate of Nursing Practice students from a local university work with stakeholders to conduct small implementation research studies as part of their capstone projects. CTSAs are well positioned to provide consultations and “match-making” services that make these sorts of learning opportunities possible.
Discussion
CTSAs and other translational science stakeholders recognize the strong potential of implementation science as a tool for facilitating research translation. As such, many institutions are working to build implementation science capacity. In this paper, we introduced the TFI framework as a guide for educational stakeholders and teachers of translational research. The framework orients educational efforts toward the end goal of facilitating the implementation of research products in real-world systems and settings and demonstrates the implications of this orientation on who, what, and how to teach.
TFI builds on an existing and growing knowledge base about how to teach learners of implementation but makes explicit some key challenges and considerations for CTSAs. Specifically, TFI describes how CTSAs and the translational science infrastructure may be ideally positioned to advance teaching and training for implementation in key ways. To that end, we see many potential uses for the TFI framework. First, teachers for implementation can translate its principles in the classroom and in curricular development. Second, directors of KL2 programs and other educational infrastructures may find the framework useful for thinking through the recruitment of learners and the designing of educational offerings. Finally, the larger community of implementation teachers and trainers within the CTSA consortium may use the framework to coordinate the creation and sharing of key resources.
Strengths of the framework relate to its value as a synthesis of several disparate bodies of work, its unique relevance to translational science teachers and stakeholders, and the diverse experience and perspectives of the authors from whom it is drawn. Important limitations include the framework’s limited empirical basis. Indeed, future efforts should focus on using the framework; assessing its value; and refining, confirming, or refuting it.
In conclusion, we emphasize that teaching for implementation is not the same as teaching for the acquisition of knowledge. Related to this, affecting change in real-world systems may benefit from teaching and training a workforce that is uniquely equipped for implementing research products. We hope that the TFI framework offers a helpful guide for thinking through how to facilitate such an effort.
Acknowledgments
ALL’s contribution was made possible by CTSA grant UL1TR002377 from the National Center for Advancing Translational Science, a component of the National Institutes of Health (NIH). AAB’s contribution was made possible by the following NIH grants: UL1TR002345, 5U24HL136790, P50 CA-244431, 3D43TW011541-01S1, 1U24HL154426-01, 5U01HL133994-05, and 3R01HD091218. MEF’s contribution was made possible by the following NIH grans: 5UL1TR003167-02, 5T32CA057712-28, and 1U48DP006408-01-00. KRS’ contribution was made possible by CTSA grant UL1TR002645. BMK’ contribution was made possible by Colorado CTSA Grant UL1 TR002535. RCS’ contribution was made possible by CTSA grant UL1TR001873 to Columbia University. The content is solely the responsibility of the authors and does not necessarily represent the official views of NIH.
Disclosures
The authors have no conflicts of interest to declare.








