Migraine is a primary disorder characterised by periodic and severe headaches, often concurrent with neurological, autonomic and gastrointestinal symptoms(Reference Eren, Dirik and Neşelioğlu1). Migraine affects 10–18 % of the general adult population worldwide, of which approximately 1 % experience a minimum of 24 h of headache per week(Reference Goadsby, Lipton and Ferrari2). The prevalence of migraine varies across populations(Reference Burch, Loder and Loder3). Namely, migraine affects 3 % of men and 10 % of women in Eastern populations. In Western populations, the rates are higher, affecting 5–9 % of men and 12–25 % of women(Reference Burch, Buse and Lipton4). In Iran, 14 % of the adult population is affected by the condition, which is more prevalent than the global projection rates and threefold higher in women than men(Reference Farhadi, Alidoost and Behzadifar5,Reference Vakili, Mirzaei and Zia Kashani6) .
Migraine has staggering public health and economic burden, including psychiatric and mental health disruptions(Reference Bergman-Bock7). Mental health disorders are 2–10 fold higher in individuals with v. without migraine(Reference Minen, De Dhaem and Van Diest8,Reference Jeyagurunathan, Abdin and Vaingankar9) . Moreover, migraine is known to decrease patients’ quality of life and aggravate the financial burden of healthcare services(Reference Lipton, Cohen and Gandhi10). Therefore, implementing novel, safe, effective and affordable therapies to manage this condition should be prioritised.
Accordingly, various dietary interventions have been proposed in the management of migraine, including unique dietary regimens(Reference Barbanti, Fofi and Aurilia11,Reference Di Lorenzo, Pinto and Ienca12) , elimination or restriction of certain foods or nutrients in patients’ usual dietary regimen(Reference Alpay, Ertaş and Orhan13,Reference Zencirci14) and dietary supplementation with specific vitamins or minerals(Reference Shaik and Gan15–Reference Maizels, Blumenfeld and Burchette17). Furthermore, previous reports have suggested a link between some comorbidities and migraine, including elevated blood pressure(Reference Kruszewski, Bieniaszewski and Neubauer18,Reference Cooper, Glover and Hormbrey19) . Therefore, a dietary regimen that modulates blood pressure may have the potential to improve migraine health outcomes. The Dietary Approaches to Stop Hypertension (DASH) eating plan has high amounts of vegetables, fruits, low-fat dairy, lean meat and whole grains and includes low Na intake. The DASH diet was initially designed to reduce blood pressure in patients with hypertension(Reference Sacks20,Reference Blumenthal, Babyak and Hinderliter21) . However, emerging evidence supports the benefits of the DASH diet in migraine(Reference Amer, Woodward and Appel22). Accordingly, a cross-sectional study demonstrated lower migrane severity and duration corresponding to adherence to the DASH diet(Reference Mirzababaei, Khorsha and Togha23), albeit the evidence is sparse and less conclusive(Reference Amer, Woodward and Appel22). As such, we were unable to find published clinical trials evaluating the effects of the DASH diet on migraine health outcomes. To address this knowledge gap, the primary purpose of our study was to examine the effects of the DASH diet on the clinical symptoms of migraine and quality of life in normotensive women. We evaluated the effects of the DASH diet on mental health parameters as our secondary aim. We hypothesised that adherence to the DASH diet would improve the clinical, quality of life and mental health outcomes of women with migraine after 12 weeks of intervention independent of blood-pressure-lowering properties of the dietary regimen.
Materials and methods
Study design and participants
The current study represents a parallel-group randomised controlled trial. Reproductive-aged (20–50 years) women with migraine symptoms referred to the Khorshid and Imam Musa Sadr neurology clinics (medical centres affiliated with Isfahan University of Medical Sciences) from October 2019 to March 2020 were screened for study eligibility. The prevalence of migraine is approximately threefold higher in women v. men(Reference Farhadi, Alidoost and Behzadifar5); therefore, only women were recruited to increase the internal validity of our work. Only reproductive-aged women (20–50 years) were recruited because women in this age range usually present with the highest migraine rates(Reference Spierings and Padamsee24). After confirming the migraine diagnosis by a neurologist (F.K), women with a BMI of 18·5–30 kg/m2 were enrolled in the study. Migraine was diagnosed using the International Classification of Headache Disorders 3 criteria(Reference Olesen25).
Women were excluded if they were (1) pregnant or lactating; (2) had a history of hypertension, CVD, diabetes, cancer, thyroid, hepatic, or renal disease, or other neurological disorders besides migraine; (3) consumed nutritional supplements that are known or are suspected to affect migraine (e.g., feverfew, coenzyme Q10, riboflavin and Mg); (4) changed the type or dosage of their migraine medication during the study and (5) adhered to any specific diet (e.g. energy-restricted) over the past 8 weeks before enrollment.
Ethics
All women provided written informed consents before enrollment, and their participation was voluntary. The study was approved by the research ethics committee at Isfahan University of Medical Sciences on 26 August 2019 (approval number: IR.MUI.RESEARCH.REC.1398·352). All study protocols were conducted according to the Declaration of Helsinki, and results were reported based on the Consolidated Standards of Reporting Trials (CONSORT) guidelines(Reference Bennett26). The trial protocol was registered at the Iranian Registry of Clinical Trials (registration number: IRCT20121216011763N38).
Sample size
We used an equation for parallel design trials to calculate our study sample size(Reference Amer, Woodward and Appel22) using the following parameters: α = 0·05, β = 0·10, Δ (standardised effect size) = 0·70 based on headache frequency and the dropout rate = 10 %. Accordingly, the estimated total sample size was 102 (51 women per group).
Randomisation
Together, 337 women were referred to the neurology clinics, of which 102 women who met all our study inclusion criteria were randomly allocated to the DASH (n 51) or usual dietary advice (control) group (n 51) using computer-generated random numbers using the Excel RAND function. An independent statistician performed the randomisation using a stratified block randomisation method by considering age and BMI at the ratio of 1:1 and randomly permuted block sizes of 4. Randomisation was completed using sealed and opaque coded envelopes that were opened sequentially at participants’ allocation. Participants and researchers were not blinded to group assignment, except a neurologist (F.K) who performed all the clinical assessments.
Protocols of the Dietary Approaches to Stop Hypertension and usual dietary advice (control) diets
Women in the intervention group received a DASH diet for 12 weeks. Women’s daily energy requirement was estimated individually using the validated Livingstone equation(Reference Livingston and Kohlstadt27–Reference Amaro-Gahete, Jurado-Fasoli and De-la-O29). Energy restriction was not part of the protocol design. Therefore, diets were isoenergetic to maintain body weight.
A trained dietitian designed a weekly DASH eating plan using 7-day menu cycles to provide 15–20 % of women’s total daily energy requirements from proteins, 25–30 % from fats and 55–60 % from carbohydrates. The DASH diet was designed to contain higher amounts of vegetables, fruits, whole grains, low-fat dairy, nuts and beans and lower amounts of red meat, sweets, refined grains, saturated fats and cholesterol compared with the control diet. Also, the DASH diet was designed to provide higher amounts of Ca, Mg and K and lower (< 2400 mg/d) amounts of Na(Reference Campbell30).
No dietary menu was provided to women in the control group. Rather, the control group received usual dietary advice consistent with the Healthy Eating Plate recommendations(Reference Saneei, Hashemipour and Kelishadi31) to improve their food choices. These recommendations were provided in oral and written formats.
The number of daily food group servings for a 2000 kcal/d energy intake in the DASH diet and recommendations for the usual dietary advice are provided in Table 1. Both study groups were visited monthly by our study dietitian (A.A) and received a booklet containing the information of foods that are known or suspected to induce or aggravate migraine attacks, including cheese, chocolate, citrus fruits, processed meat, hot dogs, ham, fatty and fried foods and canned foods. Groups were instructed to limit or eliminate consuming these foods(Reference Zencirci14). Our team of researchers contacted women weekly using phone calls to monitor their dietary adherence and resolve any potential issues regarding their compliance with the study protocol. All women had access to our team of researchers through the WhatsApp software, text messaging and phone calls during the study.
Table 1. Number of daily food group servings for a 2000 kcal/d energy intake in the Dietary Approaches to Stop Hypertension (DASH) diet and recommendations for the usual dietary advice

Adherence to the Dietary Approaches to Stop Hypertension diet
Dietary records and serum vitamin C concentrations were used to assess women’s compliance to the DASH diet, as described previously(Reference Saneei, Hashemipour and Kelishadi31,Reference Kwan, Wong and Wang32) . Serum vitamin C concentrations were assessed at baseline and post-intervention. Women in both groups were instructed to complete a 24-h food record at baseline, 4-, 8- and 12-weeks post-intervention. Accordingly, four daily food records were obtained for each study participant during the intervention. Collected food record data were analysed using the Nutritionist-4 software (First Databank, Hearst Corp), modified for Iranian foods.
Study endpoints
The primary outcomes were the clinical symptoms of migraine (i.e., frequency, duration and severity) and quality of life. Secondary outcomes were mental health measures (i.e., depression, anxiety and stress). All outcomes were assessed at baseline and after 12 weeks of intervention.
Socio-demographic, anthropometric, physical activity and blood pressure measures
Face-to-face and structured interviews were conducted by a dietitian (A.A) and a neurologist (F.K) to collect socio-demographic, anthropometric, physical activity and blood pressure data. Briefly, demographic data, including age, education, marital and smoking status, medication use, family history of migraine and time of migraine diagnosis, were obtained using standardised questionnaires. Women’s physical activity levels were assessed using the validated International Physical Activity Questionnaire and were expressed as metabolic equivalent hours per day (METs h/d)(Reference Moghaddam, Aghdam and Jafarabadi33). Weight was measured using a digital scale (Omron BF511; Omron Corp, Kyoto, Japan) to the nearest 100 g and height using an upstretched tape (SECA 206) to the nearest 1 mm with shoulders in a relaxed position without shoes. BMI was calculated using the equation: weight (kg)/height (m2). Blood pressure was measured twice using a mercury sphygmomanometer (Riester, Germany) after sitting for 10 min at each stage with intervals of at least 5 min, and the mean of two measurements was used.
Migraine assessment
The clinical symptoms of migraine, including frequency, duration and severity of headaches, were assessed by a neurologist (F.K). The number of headache attacks per month and the duration of each attack were used to define migraine frequency and duration. The VAS questionnaire(Reference Hajihashemi, Askari and Khorvash34) was used to assess the severity of migraine, wherein a scale system ranging from 0 (no pain) to 10 (worst imaginable pain) was used. The headache impact test (HIT-6) was used to determine the severity of migraine on women’s quality of life. The HIT-6 is a validated questionnaire(Reference Zandifar, Banihashemi and Haghdoost35) containing six questions and five response items per question. This scale ranges from thirty six (no headache) to seventy eight (very severe headache) scores, as described in greater detail previously(Reference Zandifar, Banihashemi and Haghdoost35).
Mental health assessment
Women’s mental health was assessed in three domains of depression, anxiety and stress using the validated Depression, Anxiety, and Stress Scales-21 questionnaire(Reference Samani and Joukar36). Each question was scored from 0 (did not apply to me at all) to 3 (applied to me very much or most of the time) to determine anxiety, stress and depression symptoms. The sum of scores for each domain was multiplied by 2 to re-scale the Depression, Anxiety, and Stress Scales-21 to the original Depression, Anxiety, and Stress Scales-42 (42 items)(Reference Henry and Crawford37). The thresholds used to determine women’s mental status as normal, mild, moderate, severe and extremely severe were (1) 0–9, 10–13, 14–20, 21–27 and ≥ 28 for the depression domain; (2) 0–7, 8–9, 10–14, 15–19 and ≥ 20 for the anxiety domain and, (3) 0–14, 15–18, 19–25, 26–33 and ≥ 34 for the stress domain, respectively(Reference Osman, Wong and Bagge38).
Statistical analysis
All statistical analyses were performed based on the intention-to-treat principle by carrying forward the last observation using the SPSS software (version 21). The normality of quantitative variables was assessed using the Q–Q plots, skewness and Kolmogorov–Smirnov tests. All variables were expressed as mean and standard errors (se) or numbers and percentages, as appropriate. Women’s baseline characteristics and nutrient intakes were compared using the independent samples t test and Pearson’s χ 2 test. A paired samples t test was used to evaluate any changes in these variables over time in groups. The effects of the DASH diet on clinical symptoms, mental health,\ and quality of life outcomes were assessed using the ANCOVA. In the ANCOVA models, baseline data on clinical symptoms, mental health and quality of life, medication use (serotonin-norepinephrine reuptake inhibitors, triptans) and weight change were included as covariates. Also, a binary between-subject variable was added to ANCOVA models to account for any effects of group allocations (0 for the intervention and 1 for the control group). Furthermore, the dependent variable was entered as the post-intervention values of clinical symptoms, mental health and quality of life. Results were considered significant at P < 0·05.
Results
One hundred and two women were enrolled in our work, of which three in the DASH diet group and three in the control group were lost to follow-up (Fig. 1). Briefly, women in the DASH diet group were lost to follow-up due to changes in their medication (n 2) or personal reasons (n 1). Similarly, women in the control group were lost due to changes in their medication regimen (n 1), personal reasons (n 1) or following a special diet (n 1). All the evaluated outcome measures of our interest were normally distributed. Data of all randomised women were included in our analyses consistent with the intention-to-treat principle.

Fig. 1. Patients flow diagram.
Groups’ baseline characteristics were comparable between groups (Table 2), except for the use of triptans (P = 0·041). Similarly, energy, carbohydrate, protein, total fat, saturated fat and Ca intakes were comparable between groups during the intervention (all P > 0·05; Fig. 2). Conversely, the DASH diet group exhibited increased dietary intakes of fibre (20·70 v. 17·36 g/d, P < 0·001), K (3453·26 v. 3128·64 mg/d, P = 0·035), Mg (264·79 v. 226·35 mg/d, P < 0·001) and vitamin C (166·57 v. 140·20 mg/d, P = 0·007) compared with the control group (Fig. 2); however, Na intake was decreased in the DASH diet group (2865·69 v. 3710·08 mg/d, P = 0·005). Furthermore, serum vitamin C concentrations were increased in the DASH diet group v. the control group (36·90 v. 33·59 µg/ml, P = 0·041; Fig. 3). These findings likely indicate a good adherence of the DASH diet group to intervention.
Table 2. Baseline characteristics of women (Mean values and standard errors; numbers and percentages)
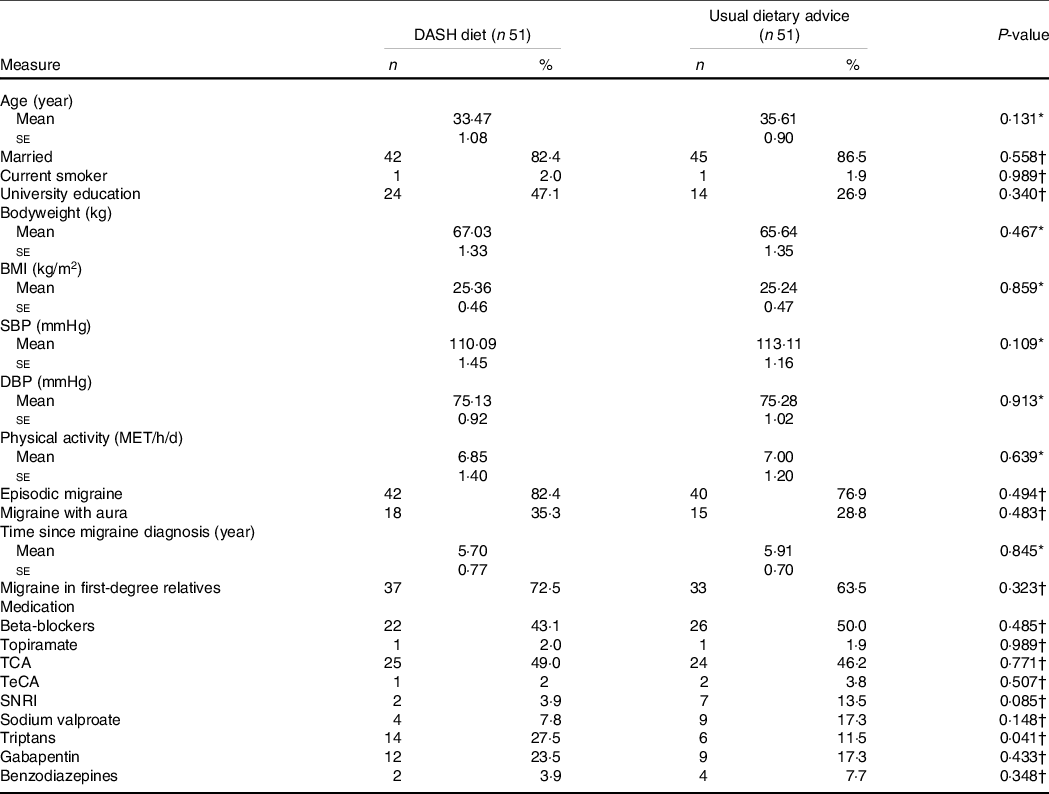
SBP, systolic blood pressure; DBP, diastolic blood pressure; TCA, tricyclic antidepressants; TeCA, tetracyclic antidepressant; SNRI, serotonin-norepinephrine reuptake inhibitor.
* Calculated by independent-samples t test.
† Calculated by χ 2 test.

Fig. 2. Nutrient intakes of the intervention group (IG = 51) and the control group (CG = 51) during the 3-month intervention. Nutrient intakes are presented as means with standard error within bars. *Significant difference (P < 0·05; calculated using the paired samples t test).

Fig. 3. Serum levels of vitamin C at the baseline and following 12-week of intervention in migraine patients who received either DASH diet or usual dietary advice. Data are presented as mean with standard error within bars. * and ** obtained from paired samples t test. *** obtained from analysis of covariance (ANCOVA). *P = 0·004, **P = 0·478, ***P = 0·041. ![]() , DASH diet;
, DASH diet; ![]() , usual dietary advice.
, usual dietary advice.
The DASH diet group exhibited weight loss (–0·64 kg) post-intervention compared with their baseline levels, yet the control group had a tendency to gain weight (0·49 kg; Fig. 4). We detected a significant between-group change in weight in the DASH v. the control group (P = 0·027).

Fig. 4. Body weight at the baseline and following 12-week of intervention in migraine patients who received either DASH diet or usual dietary advice. Data are presented as mean with standard error within bars. * and ** obtained from paired samples t test. ***obtained from analysis of covariance (ANCOVA). *P = 0·057, **P = 0·243, ***P = 0·027. ![]() , DASH diet;
, DASH diet; ![]() , usual dietary advice.
, usual dietary advice.
Also, the DASH diet group exhibited decreases in their frequency, duration and severity of migraine and HIT-6 scores. Similarly, the control group showed decreases in all these markers (all: P < 0·05) except migraine frequency. Our between-group comparisons indicated a significant reduction in the frequency (–3·00 v. −1·40, P = 0·025) and severity (–1·76 v. −0·59, P < 0·001) of migraine only in the DASH diet group, unlike the control group. Furthermore, the duration of migraine tended to be lower in the DASH diet v. the control group (–0·58 v. −0·33 d, P = 0·053).
Table 4 shows the impact of the DASH diet on women’s mental health parameters, including depression, anxiety and stress. The DASH diet group showed decreased scores of depression (–4·50 v. −2·73, P = 0·019) and stress (–5·84 v. −2·98, P = 0·011) v. the control group; however, groups had comparable reductions in their anxiety scores post-intervention (–2·74 v. −1·46, P = 0·077; Table 4). We detected no adverse events during the intervention in groups.
Table 3. Clinical symptoms of migraine and quality of life measures pre-and post-intervention (Mean values and standard errors)

DASH: Dietary Approaches to Stop Hypertension; HIT: Headache Impact Test.
* Calculated by paired-samples t test.
† Calculated by independent-samples t test.
‡ Calculated by ANCOVA, adjusted for taking triptans, SNRI and weight change.
Table 4. Mental health measures pre- and post-intervention (Mean values and standard errors)

DASH: Dietary Approaches to Stop Hypertension.
* Calculated by paired-samples t test.
† Calculated by independent-samples t test.
‡ Calculated by ANCOVA, adjusted for taking triptans, SNRI and weight change.
Discussion
Dietary modification represents a promising therapy for neurological disorders(Reference Hajjarzadeh, Mahdavi and Shalilahmadi39). However, little is known about a unique dietary regimen that can improve the clinical symptoms and associated comorbidities of patients with migraine. In the present work, we examined the effectiveness of the DASH diet, as a dietary approach with a favourable dietary composition, on the clinical, quality of life and mental health outcomes of reproductive-aged women with migraine. Our study revealed that the DASH diet decreases the frequency and severity of migraine after 12 weeks of intervention. Also, women in the DASH diet group exhibited a tendency for greater decreases in migraine duration.
Our observations corroborate a previous population-based study on inverse associations between adherence to the DASH diet and duration and severity of migraine(Reference Mirzababaei, Khorsha and Togha23). Similarly, another observational study revealed that patients with high adherence to healthy dietary patterns (i.e., diets rich in fruits, vegetables and legumes) exhibited fewer migraine attacks(Reference Hajjarzadeh, Mahdavi and Shalilahmadi39). Consistently, the post hoc analyses of results from the DASH-sodium clinical trial showed a link between lower risk of migraine and dietary sodium intakes, albeit the DASH dietary pattern had no beneficial impacts on the risk or severity of headaches(Reference Amer, Woodward and Appel22). However, this study included all primary headaches (tension, cluster and migraine) without delineating patients’ responses based on their headache subtype or subgroup analyses. Additionally, the study included hypertensive patients, making it challenging for us to attribute any positive results on migraine directly to the favourable effects of the DASH diet on modulating blood pressure or indirect improvements mediated by improvements in patients’ metabolic and hypertension status(Reference Gardener, Monteith and Rundek40). Specifically, fewer migraine attacks in hypertensive patients have been attributed to their reduced blood pressure secondary to adherence to the DASH diet, which contains low Na(Reference Amer, Woodward and Appel22). In contrast, our study is unique in evaluating the effectiveness of the DASH diet on otherwise healthy cohorts with migraine headaches, wherein we excluded patients with elevated blood pressure or obesity. These results may be practical if clinical practice as cohorts with obesity present with a higher frequency of headaches v. their lean counterparts(Reference Gelaye, Sacco and Brown41). Also, our findings add a new dimension to current evidence by indicating that the favourable effects of the DASH diet on migraine health outcomes may be independent of blood pressure or adiposity status, albeit further research is required.
The mechanisms underlying associations between the DASH diet and migraine are unclear. The DASH diet has high amounts of K, Mg and Ca but is low in Na. These cations have integral roles in brain function and migraine pathophysiology(Reference Harrington, Fonteh and Cowan42). Namely, elevated Na concentrations in the cerebrospinal fluid(Reference Harrington, Fonteh and Cowan42) and blood(Reference Campbell, Hay and Tonks43), unlike Ca, Mg and K, have been observed in migraine attacks, indicating a role for Na in migraine pathophysiology(Reference Harrington, Fonteh and Cowan42). Increased Na consumption leads to its higher serum concentration and subsequently elevated levels in the cerebrospinal fluid(Reference Harrington, Fonteh and Cowan42,Reference Davson and Pollay44) and brain extracellular fluid(Reference Kawano, Yoshida and Kawamura45) in a short time (< 2 h). These alterations have been proposed to decrease neurons’ resting potential and reduce their threshold for action potentials(Reference Pirahanchi, Jessu and Aeddula46). Conversely, Mg has been proposed to prevent migraine by blocking N-methyl-D-aspartate receptors, inhibiting serotonin-dependent vascular spasm and reducing prostacyclin-dependent vasodilation(Reference Rybicka, Baranowska-Bosiacka and Zyluk47). The DASH diet contains no to low amounts of processed meats, refined grains and fried foods, all of which have been associated with higher migraine complications or frequency(Reference Hindiyeh, Zhang and Farrar48). The diet is rich in fruits and vegetables that are high in anti-inflammatory and antioxidant compounds, known to modulate neurogenic inflammation involved in migraine(Reference Geppetti, Capone and Trevisani49). Moreover, the DASH dietary program in our study was designed to provide more frequent yet smaller portions of meals and snacks to prevent fasting-induced migraine(Reference Hufnagl and Peroutka50).
We observed no differences in the quality of life outcomes between groups post-intervention, as evidenced by the HIT-6 test results; however, both groups showed improvements compared with their baseline levels. Our findings reiterate those of Costa et al., reporting the benefits of nutritional counselling on decreasing HIT-6 scores, albeit the observed decreases were independent of participants’ nutritional status. Moreover, Smith et al. reported that educational and skill-based programmes increased knowledge and improved headache-related quality of life parameters in patients with migraine(Reference Smith, Nicholson and Banks51). Consistently, we hypothesise that dietary education provided by our healthcare team has been effective at improving the quality of life outcomes in both groups.
We showed that adherence to the DASH diet resulted in decreased scores of depression v. a control diet. Specifically, women enrolled in our work were diagnosed with moderate depression and stress levels at baseline. In the DASH diet group, depression and stress levels decreased to mild levels post-intervention, unlike the control group (unchanged). The DASH diet and control groups were diagnosed with moderate and severe anxiety levels, respectively; however, their status did not change during the study. We were unable to detect a study on the effects of the DASH diet on mental health in patients with migraine. However, a study by Torres et al. proposed improvements in mood status outcomes following a DASH diet intervention in non-migraine populations, including postmenopausal(Reference Torres and Nowson52) or hypertensive(Reference Torres, Nowson and Worsley53) cohorts. Furthermore, adherence to the DASH diet has been associated with a lower risk of depression in healthy adults(Reference Valipour, Esmaillzadeh and Azadbakht54), corroborating our findings. Consistently, a large prospective study showed an inverse association between adherence to the DASH diet and depression risk(Reference Perez-Cornago, Sanchez-Villegas and Bes-Rastrollo55).
The mechanisms through which the DASH diet could affect mental health in patients with migraines are not fully elucidated, albeit several dietary factors may contribute. The DASH diet contains high amounts of antioxidant-rich vegetables and fruits, thereby may recover the activity of the antioxidant enzymes in the brain cortex and improve mental health(Reference Arab, Mehrabani and Moradi56). We showed that the DASH diet reduced women’s Na intakes but increased their fibre, K, Mg and vitamin C intakes. A high serum Na/K ratio leads to increased progesterone secretion, which subsequently alters the brain’s neural activity, possibly leading to mood disorders(Reference Arab, Mehrabani and Moradi56). Also, the DASH diet contains a balanced Na to K ratio and is rich in Mg, with antidepressant properties. Namely, the antidepressant activity of Mg is, in part, explained by blocking N-methyl-D-aspartate receptors and increasing the expression of brain-derived neurotrophic factor(Reference Arab, Mehrabani and Moradi56). Similarly, the high vitamin C content in the DASH diet may improve mental health mediated by blocking N-methyl-D-aspartate receptors and regulating the dopaminergic, serotonergic and noradrenergic systems(Reference Arab, Mehrabani and Moradi56).
In the current study, women in the DASH diet group exhibited relatively good compliance to the dietary intervention, as evidenced by their food records and serum vitamin C concentrations. However, their dietary adherence was not perfect, indicating that better compliance would have fostered our observed health benefits. Previous studies have suggested various subjective (e.g. DASH scores, achievement of defined DASH dietary pattern) and objective (serum vitamin C, urinary excretion of Na and/or K) methods for evaluating participants’ adherence to the DASH diet(Reference Kwan, Wong and Wang32). However, the advantages and disadvantages of each approach have been debated. Notably, a systematic review concluded the paucity of consensus on evaluating dietary compliance(Reference Kwan, Wong and Wang32). In the present work, we used subjective and objective approaches to increase the validity of our evaluations. We also acknowledge that dietary compliance may have been higher in feeding trials(Reference Kwan, Wong and Wang32) than in our work, which focused on women’s nutritional education. Also, we assessed the dietary intakes of the women at baseline, 4-, 8- and 12-weeks post-intervention to characterise their dietary intakes. We attribute higher intakes of fibre, K, Mg and vitamin C and lower intakes of Na in women allocated to their adherence to the DASH diet during the intervention. However, we were unable to comment on women’s eating habits or changes in their dietary intake before the intervention, which could affect their response to intervention. Therefore, future work should consider the usual dietary patterns of participants before initiating any dietary intervention.
Overall, we observed minimal differences in the medication use of groups at baseline; however, groups differed in their triptan use (P = 0·041) and exhibited non-significant (P = 0·085) differences in SNRI use. We accounted for these differences in our statistical analyses; however, we acknowledge that any potential impacts of patients’ medication regimens on study outcomes require careful considerations, particularly in the long term. As such, we cannot fully preclude any potential impact of medication use differences between groups on their response to treatment.
Strength and limitation
The study strengths were implementing a DASH diet in women with a migraine for the first time using an interventional design and a relatively large sample size. Furthermore, we accounted for several confounding parameters that could influence our findings, including weight, blood pressure, and medication use. We used dietary records and serum vitamin C levels to assess women’s compliance to the DASH diet. However, we acknowledge a lack of universal consensus regarding an optimal approach for evaluating participants’ compliance to dietary interventions(Reference Kwan, Wong and Wang32).
Our study had some limitations. We were unable to blind women given that the nature of our trial focused on dietary modifications, which is not uncommon in studies of this type, as discussed previously(Reference Staudacher, Irving and Lomer57). We acknowledge that the lack of blinding may introduce a bias to our work as the intervention group may exhibit better outcomes assuming they had received a better treatment v. controls. Our findings may not be generalised to all patients with migraine, as we focused on reproductive-aged women. We provided the DASH diet using a food menu program and written recommendations v. a feeding trial method. We hypothesise that a controlled feeding trial would have improved women’s dietary intakes. Dietary intakes were recorded for 4 d in our study; however, more days of data collection could better capture women’s dietary habits. Finally, we did not assess women’s menstrual cycle status (e.g., regular, irregular). Therefore, we cannot preclude any potential effects of menstrual cyclicity on study outcomes, as menstrual dysfunction may be associated with migraine(Reference Spierings and Padamsee24). Further investigations are required.
Conclusions
Consumption of the DASH diet for 12 weeks may improve the clinical symptoms (severity, frequency) of migrane and mental health outcomes (depression, stress) in reproductive-aged women compared with a control diet. However, no dietary regimen was superior for improving the quality of life and anxiety outcomes. Overall, the DASH diet may be favourable as a complementary treatment for patients with migraine. Further research is needed to confirm our findings.
Acknowledgements
The authors gratefully acknowledge the support of the women who volunteered to participate in the present trial.
This research was supported by the Vice-Chancellor for Research, Isfahan University of Medical Sciences, Isfahan, Iran (Ph.D. thesis grant no. 398360).
Conception and design: A. A., G. A. Acquisition of data: A. A., G. A., F. K. Analysis and interpretation of data: A. A., F. K., M. K. Drafting the manuscript: A. A. Revising it for intellectual content: A. A., F. K., Z. H., G. A., M. K.
There are no conflicts of interest.













