INTRODUCTION
Psychogenic non-epileptic seizures (PNES) are a common phenomenon and there is no absolute consensus in defining this condition, so several terms have been used to describe these events over the years.Reference Brigo, Igwe and Ausserer 1 A well-accepted notion is that they represent a sudden event characterized by paroxysmal changes in consciousness, movement and/or behavior that are similar to the ones seen in epileptic seizures. However, they are not associated with epileptiform activity as detected through video electroencephalography (VEEG)Reference Reuber and Mayor 2 and there are psychologic underpinnings and causes that lead to the seizure.Reference LaFrance, Baker, Duncan, Goldstein and Reuber 3
The term pseudo-seizures has been frequently used in the pastReference Glaser 4 but because it implies that the individual is “faking” it, alternative descriptors have been suggested. Accepted by someReference Bodde, van der Kruijs and Ijff 5 , Reference Wadwekar, Nair and Murgai 6 and adopted more widelyReference Brigo, Igwe and Ausserer 1 , Reference Tannemaat and van Dijk 7 the term PNES has been chosen as we feel it best describes these events.
The incidence of PNES has been estimated in 4.9/100,000/yearReference Duncan, Razvi and Mulhern 8 and its prevalence varies widely between 2 and 33/ 100,000 population,Reference Benbadis and Allen Hauser 9 , Reference Sahaya, Dholakia, Lardizabal and Sahota 10 probably due to variation in diagnostic criteria, the inherent complexity of PNES and misdiagnosis perhaps due to lack of proper training in this area. Although in the majority of cases the distinction between PNES and epileptic seizures can be made,Reference Asadi-Pooya and Emami 11 to add more intricacy, PNES can be present in some patients with epilepsy. Some authorsReference Reuber and Mayor 2 , Reference Asadi-Pooya and Emami 11 , Reference Benbadis, Agrawal and Tatum 12 have reported that 5% to 15% of out-patient populations referred to epilepsy clinics and between 20% and 40% of in-patient populations admitted at epilepsy centers have PNES. In a recent retrospective studyReference Wadwekar, Nair and Murgai 6 it was found that from 65 patients diagnosed with PNES, 11.1% also had epileptic seizures. In previous reports it has been described that 75%–80% of the patients with PNES are female.Reference Bodde, Brooks and Baker 13 Although this disorder can occur at any age, Duncan et al.Reference Duncan, Graham, Oto and Russell 14 reported that the mean age of onset is 30.5 years (SD ±13.7 years) (see Table 2).
PNES have been known for at least 2,500 years,Reference Veith 15 however, it continues to be a poorly understood disorder. The diagnosis of PNES is controversial and there is no definitive treatment approach. The overall prognosis of this condition is poorReference Tannemaat and van Dijk 7 and it is associated with a high level of disability and reduced quality of life (QOL).Reference Myers, Lancman and Laban-Grant 16
As far as we know, there is no data regarding the prevalence and incidence of this disorder in Canada; therefore, a database including the characteristics and outcomes of PNES would help clinicians to develop guidelines for the management of patients suffering from this condition (see Table 1 for the key points of this review).
METHODS
We present a comprehensive narrative review of PNES. To cover a wide range of topics related with PNES and add value to our manuscript we reviewed different sources including Pubmed, MEDLINE and EMBASE databases using OVID with literature pertaining PNES from the year 2000 and up to August 2017. We used the terms “PNES” as well as “pseudoseizures” and “psychogenic non-epileptic attacks” with the different following medical subheadings to identify relevant articles: “prevalence”, “diagnosis”, “management,” “prognosis” and “outcomes”.
The abstracts and bibliographies of relevant studies were reviewed to identify additional articles. We included only articles written in English and the evidence ranged from expert opinion to clinical trials, systematic reviews, meta-analyses and a Cochrane review was also included in this paper.
PSYCHOPATHOLOGY OF PNES
Various risk factors have been described in adults and children with PNES. In a study evaluating psychiatric comorbidities encountered in epilepsy monitoring units at Veterans Affairs Medical Centers in the USA,Reference Salinsky, Evrard, Storzbach and Pugh 17 post-traumatic stress disorder (PTSD) preceded the diagnosis of PNES in 58% of the patients. Major depression and alcohol abuse were common diagnoses in PNES and there is a well-documented association between chronic pain, psychiatric illness (especially depression, anxiety and personality disorders) and PNES (see Table 3).Reference Benbadis 18 , Reference Bowman and Markand 19 In children and adolescents parental discord or divorce, sexual or physical abuse, trauma, school difficulties, having epilepsy or family history of epilepsy among others are significantly associated factors.Reference Benbadis and Allen Hauser 9 , Reference Asadi-Pooya and Emami 11 , Reference Say, Tasdemir and Akbas 20 , Reference Vincentiis, Valente and Thomé-Souza 21
In a more comprehensive systematic reviewReference Brown and Reuber 22 authors described different theoretical models of PNES: (1) PNES as a dissociative phenomenon, reflecting a defensive process that prevents individual from becoming overwhelmed by emotional adversity (seen for instance, as a somatic flashback in PTSD); (2) PNES as a “hard-wired” reflex (tendency to have a defensive reflex as occur in other animals); (3) PNES as a learned behavior (maintained by positive and negative reinforcement); and (4) PNES as a disturbance of cognitive control (resulting and maintained by factors that increase activation of seizure programs). PNES has been classified in the Diagnostic and Statistical Manual of Mental Disorders, third revised edition (DSM-III-R), as a dissociative disorder.Reference Bowman and Markand 19 However, according to the DSM-5 and International Statistical Classification of Diseases and Related Health Problems (ICD)-10 manual, PNES is generally considered a conversion type of somatoform disorder. 23 , 24 In a recent published study analyzing dissociative symptoms experienced by patients suffering from PNES;Reference Pick, Mellers and Goldstein 25 those with PNES compared with controls reported significantly more psychological and somatoform dissociative symptoms, trauma, perceived impact of trauma and post-traumatic symptoms. The relationship between traumatic brain injury and PNES has also been described,Reference Salinsky, Storzbach, Goy and Evrard 26 but the causality of this association should be further evaluated in prospective studies.
In addition, other disorders such as psychogenic movements disorders (PMD) have shown to share common risk factors (e.g. similar age and sex distribution; relatively frequent co-occurrence of psychiatric disorders or similar psychological profiles and high rates of chronic pain and other somatization disorders),Reference Erro, Brigo, Trinka, Turri, Edwards and Tinazzi 27 complicating the understanding of the psychopathological process in PNES further. PNES and PMD may represent two ends of a continuum, where different clinical presentations explain referral to either the epilepsy or movement disorder specialists.Reference Erro, Brigo, Trinka, Turri, Edwards and Tinazzi 27
DIAGNOSIS
The diagnosis of PNES is challenging and misdiagnosis of PNES as epilepsy can have deleterious consequences.Reference Seneviratne, Ding and Bower 28 Syncope, panic/anxiety, hyperventilation attacks, parasomnias, migraine with aura and transient ischemic attacks are some of the conditions that may give the appearance of both epileptic and non-epileptic seizures.Reference Brodtkorb 29 , Reference Baslet, Seshadri and Bermeo-Ovalle 30 Sometimes accurate diagnosis is not established until 7-10 years or more after the onset of the disorder.Reference Seneviratne, Ding and Bower 28 Reasons that can contribute to this are a lack of knowledge by physicians with regards to PNES, negative connotation, and a lack of necessary diagnostic facilities.Reference MacDonald, Hill and Phan 31 , Reference Bodde, Brooks and Baker 32
Some studies have noted that many signs that have been considered typical for PNES appear not to be specific as they can also be found in epileptic seizures, especially those which originate in the frontal lobe.Reference Pillai and Haut 33 Conversely, many features characteristic of epileptic seizures can also be present in PNES (i.e. tongue biting, urinary incontinence or eye closure).Reference Brigo, Ausserer and Nardone 34 Therefore, in primary care settings PNES should be suspected when a patient presents with seizures-like symptoms with resistance to antiepileptic drugs (AEDs) (though pharmacoresistant epilepsy is the other common cause of persistence seizures and reason for referral to an epilepsy center). 35 The presence of some triggers may suggest also PNES. For instance, emotional or stress triggers, or if these events occur in special circumstances (in the presence of family members or physician’s office). Patients who suffer from PNES usually have psychiatric comorbidities accompanying the syndrome (i.e. personality disorder, PTSD or depression/anxiety).Reference Bowman and Markand 19 , Reference Say, Tasdemir and Akbas 20 However, it should be noted that the diagnosis of PNES cannot be made at this stage as no single clinical feature is pathognomonic of PNES. The International League Against Epilepsy (ILAE) Commission on Neuropsychobiology Non-epileptic Seizures Task Force was charged with developing a consensus on minimal requirements for diagnosis of non-epileptic events.Reference LaFrance, Baker, Duncan, Goldstein and Reuber 3 They proposed a diagnostic level of certainty for PNES based in witnessed event, history and electroencephalogram (EEG) findings. Therefore, the level of certainty can be divided in: (1) Possible (if the event is self-reported by the patient or a witness and there is no epileptiform activity in a routine or sleep deprived EEG); (2) Probable (the event is described by a clinician who reviewed video recording and there is no epileptiform activity in the routine or sleep deprived EEG); (3) Clinically established (if the event is witnessed by a clinician experienced in diagnosis of seizure disorders and there is no epileptiform activity in the EEG during a typical event in which the semiology would make ictal epileptiform EEG activity expectable during equivalent epileptic seizure); and lastly, (4) Documented (when the event is witnessed by an experienced clinician in seizure disorders while on video EEG and there is no epileptiform activity immediately before, during or after the event captured on ictal video EEG with typical PNES semiology).Reference LaFrance, Baker, Duncan, Goldstein and Reuber 3
Similar classification like the proposed by the ILAE for PNES, may be applicable to other psychogenic disorders such as psychogenic movement disorders. PNES has been labeled “psychogenic”, implying that psychological factors lead to these events. However, it is not always easy to pinpoint the psychogenic mechanism involved as PNES is a complex disorder that requires a biopsychosocial conceptualization.Reference Drane, LaRoche and Ganesh 36 Therefore, patient history, semiology and the use of other investigations such as neuroimaging may be needed in some cases.
Patients suspected of PNES should be referred to a neurologist who may perform further investigations, including a VEEG, which is considered the gold standard for the diagnosis of PNES.Reference Reuber and Mayor 2 Although VEEG evaluation needs to be performed by an experienced clinician, recent studies have explored the use of artificial neural networks in the scoring of video recordings based on the signs and symptoms displayed (e.g. hypermotor versus akinetic or subjective symptoms). According to the authors, this technique may afford a measure of objectivity, in the differential diagnosis of PNES.Reference Magaudda, Laganà and Calamuneri 37
Some criticisms have been made regarding the value of VEEG. For instance, events characterized by subjective sensory or autonomic manifestations require more comprehensive diagnostic procedures and the VEEG might be less sensitive in these cases.Reference Erba, Giussani and Juersivich 38 In one study evaluating the accuracy of epileptologists diagnosing PNES based on the video recording alone,Reference Erba, Giussani and Juersivich 38 authors found that there were some important factors affecting the rater’s decision. For instance, the video or audio quality, as well as lack of intervention by bystanders, which were the most common reasons for considering the video below the minimum desirable standard to make a diagnosis. All five raters involved in this study were correct in predicting the diagnosis in 7 (30.4%) of 23 cases. Of these, three had epileptic seizures and four PNES. However, for the diagnosis of other non-epileptic seizures, in addition to video and EEG data information about the prodromal symptoms and the results of monitoring other physiologic parameter, such as vital signs and ECG, might be necessary.
Another study evaluated the accuracy of discrimination between epileptic seizures and PNES before and after targeted video training among medical students.Reference Seneviratne, Ding and Bower 28 Authors showed that at 3 and 6 months after training the students achieved results similar to that of emergency medicine trainees, which suggest that video-based training is an effective tool to improve the accuracy of PNES diagnosis.Reference Seneviratne, Ding and Bower 28
Controversy also exists in the use of suggestive seizure induction as there is no unified protocol, definitive ethical agreement and no consensus on diagnostic utility.Reference Popkirov, Grönheit and Wellmer 39 Hypnosis, intravenous application of saline, or even applying additional EEG-electrodes or photic stimulation could induce a psychogenic seizure as long as its effects are explained or implied convincingly.Reference Popkirov, Grönheit and Wellmer 39 In a recent retrospective study including 122 patients with PNES,Reference Popkirov, Jungilligens, Grönheit and Wellmer 40 authors described that in about a quarter of all patients, no spontaneous PNES was recorded during VEEG, but one could be elicited during suggestive seizure induction. Therefore, the authors support the role of suggestive seizure induction in the diagnostic workup when PNES are suspected and no spontaneous events occur in the epilepsy monitoring unit.
A psychiatric and/or psychological evaluation is paramount as part of a comprehensive assessment strategy as well as to improve the outcomes.Reference Brown and Reuber 22 , Reference Drane, LaRoche and Ganesh 36 Interestingly, language-based techniques evaluating patient/physician interaction by conversation analysis may also be a useful tool in the differential diagnosis of PNES, especially when VEEG is not available.Reference Cornaggia, Gugliotta, Magaudda, Alfa, Beghi and Polita 41
Laboratory studies might be helpful but are usually performed to exclude metabolic or toxic causes of seizures. Serum prolactin, creatine kinase and neuron-specific enolase have been evaluated in PNES; however, their limited discriminative power makes them unreliable.Reference Willert, Spitzer, Kusserow and Runge 42 , Reference Nass, Sassen, Elger and Surges 43 A recent pilot study analyzing EEG spectral power in patients with PNESReference Meppelink, Pareés and Beudel 44 showed that desynchronization of β power might be a marker of an upcoming non-epileptic attack. However, this needs to be reproduced in larger studies. In a systematic review evaluating biomarkers in the diagnosis of PNES (including neuroimaging findings, serum enzymes and hormones among others) authors concluded that no single biomarker successfully differentiates PNES from epileptic seizures.Reference Sundararajan, Tesar and Jimenez 45
A prospective study analyzed the neuroanatomical correlates of PNES by using morphologic brain MRI measurements.Reference Labate, Cerasa and Mula 46 Authors demonstrated that voxel-based morphometry and cortical thickness analyses in PNES patients were abnormal. They showed cortical atrophy of the motor and premotor regions in the right hemisphere and the cerebellum bilaterally. This observation was more pronounced in those with higher scores of depression, which favor the hypothesis of adaptive cortical-subcortical plasticity within these regions, giving rise to PNES (where PNES phenomenology is driven by the psychological factor interacting with specific biologic abnormalities). However, further studies are needed to clarify whether these changes are related to depression, other conversion disorders or to PNES per se.
Another study using positron emission tomography (PET) as functional neuroimaging, supported specific neurobiological dysfunction in patients with PNES.Reference Arthuis, Micoulaud-Franchi and Bartolomei 47 These patients exhibited significant hypometabolism within the right inferior parietal and central regions, and within the bilateral anterior cingulate cortex compared with controls. However, authors could not exclude that these observed changes may be related to patient’s comorbidities, and these biomarkers are only used for research purposes at the moment.
Such studies may help in understanding the pathophysiology and refine the diagnosis of PNES in the future. Otherwise, incidental abnormalities can be occasionally seen on imaging, but they should not confound the diagnosis of PNES if this is established with the VEEG. We have proposed a diagnostic and management algorithm suggesting a multidisciplinary approach (see Figure 1).
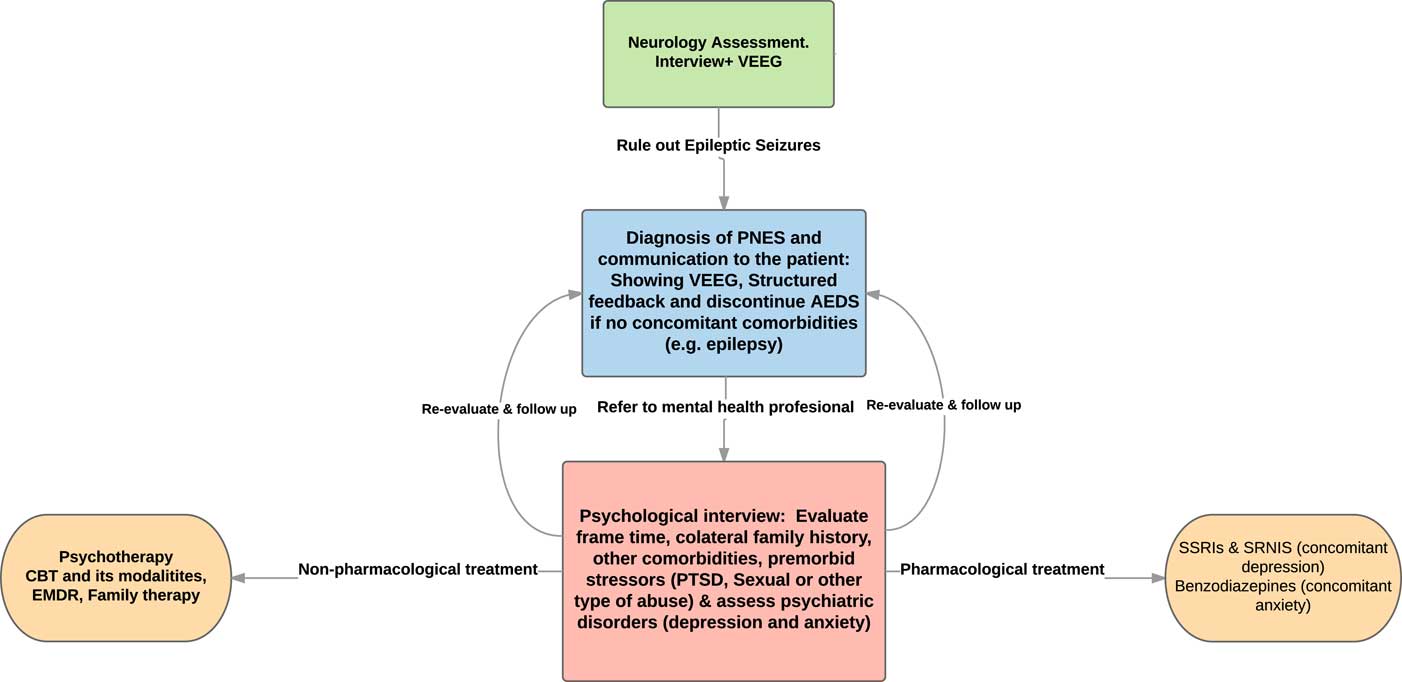
Figure 1 Diagnostic and Management Algorithm for psychogenic non-epileptic seizures (PNES). VEEG, video electroencephalogram; AEDS, antiepileptic drugs; PTSD, post-traumatic stress disorder; CBT, cognitive behavioral neurology; EMDR, eye movement desensitization and reprocessing; SSRIs, selective serotonin reuptake inhibitors; SRNIs, selective serotonin-norepinephrine reuptake inhibitors.
MANAGEMENT
There is no standardized treatment strategy for PNES. Treatment recommendations are therefore based on case studies, small case series or anecdotal experience.Reference Bodde, Brooks and Baker 13 Ideally, a team approach should be utilized to formulate a comprehensive treatment strategy.Reference Bodde, Brooks and Baker 13 Patients with a suspicion of PNES should be referred by the family doctor to a neurologist who specializes in epilepsy for confirmation. These patients may be discharged from the care of the neurologist if there is no coexisting epilepsy. However, it is important that before discharge, patients have accepted their diagnosis and a transition to psychiatry has been established.Reference Reuber and Elger 48 This is the first step in the treatment pathway. Possible strategies for communicating the diagnosis of PNES include showing the patient a video-recording of the seizure, presenting the diagnosis as good news (i.e. the absence of epilepsy) and establishing that these seizures are not deliberate.Reference Marie Gillig 49 However, one needs to be cautious as the diagnosis of PNES predicts a poor prognosis in many of the cases, so follow-ups and early interventions need to be put in place. Structured feedback and psychiatric consultation appears adequate to significantly reduce PNES frequency and improve aspects of QOL.Reference Drane, LaRoche and Ganesh 36 A clinical trial published recently showed that structured feedback interventions, which may contribute to better acceptance of the PNES diagnosis, led to a greater likelihood of seeking formal mental health intervention, reduction in PNES events and improvements in QOL. Furthermore, the addition of weekly phone contact also led to mood improvement.Reference Drane, LaRoche and Ganesh 36
Current treatments include the use of cognitive behavioral therapy (CBT) by using desensitization, and exposure plus response prevention to modify anxiety and allow adaptive responses.Reference Baslet, Seshadri and Bermeo-Ovalle 30 Other special forms of CBT such as hypnotic abreaction to try to discover how the patients feel during seizures have been also recommended.Reference Bodde, Brooks and Baker 32 Prolonged exposure (PE) therapy is also another form of CBT that specifically targets the effects of PTSD and was used in a trial of 16 patients with PNES and PTSD.Reference Myers, Vaidya-Mathur and Lancman 50 In this trial authors showed that although a diagnois of PTSD does not explain the development of PNES in all patients, applying a disorder-specific treatment (PE therapy for PTSD) can be an effective way of treating PNES in patients who have been traumatized and carry a diagnosis of PTSD.
In an open pilot trial, CBT was found to reduce PNES frequency and improve psychosocial functioning after 12 sessions of treatment.Reference Goldstein, Deale and Mitchell-O’Malley 51 A meta-analysis evaluating the prevalence of seizure reduction in psychological treatments for PNES, authors showed that 82% of those completing psychotherapy reported a reduction in seizure frequency of ≥50%.Reference Carlson and Nicholson Perry 52 Goldstein et al.Reference Goldstein, Mellers and Landau 53 proposed a multicenter randomized controlled trial of CBT for PNES evaluating the cost effectiveness of this intervention and its generalizability which could help us to make further recommendations in the management of patients with PNES. Furthermore, we need to take into account that mental health resources as well as specific protocols approaching the diagnosis and management of PNES might not be available in all neurology centers where the diagnosis of PNES is made.Reference Valente, De Paola and Palmini 54
A recent meta-analysis reviewing 13 studies that included CBT, psychodynamic therapy, paradoxical intention therapy, mindfulness, psychoeducation and eclectic interventions in patients with PNES, highlighted the potential for psychological interventions as a favorable alternative to the current lack of treatment options offered to people with PNES.Reference Carlson and Nicholson Perry 52 However, in a Cochrane review that included 12 randomized clinical trials of CBT in patients suffering from PNES,Reference Martlew, Pulman and Marson 55 authors showed that many of these studies have multiple biases and the overall evidence for the main outcome of reducing seizures as a result of treatment was not considered reliable. Therefore, further research in this field needs to be done.
Pharmacotherapy should be considered especially when major mood disorders such as depression, panic disorder or psychosis are presentReference Baslet, Seshadri and Bermeo-Ovalle 30 . LaFrance et al.Reference LaFrance, Baird and Barry 56 suggested that a selective serotonin reuptake inhibitor or related compounds may be useful. However, there is insufficient evidence to recommend routine treatment with antidepressant medication as a method of reducing PNES.Reference Bravo, Hoffman-Snyder and Wellik 57 An open-label prospective study evaluated patients with PNES and anxious-depressive symptoms treated with venlafaxine for 5 months.Reference Pintor, Baillés and Matrai 58 The authors showed that venlafaxine reduced by 50% the number of seizure like events as well as depressive and anxiety symptoms based on different scales.
In the absence of epilepsy, an important first step once the diagnosis of PNES is made is to discontinue the AEDs as they may have associated side effects.Reference Duncan 59 However, many patients with PNES in whom epilepsy has been excluded remain on AEDs.Reference Duncan 59 In a study cohort was shown that a baseline history of psychological trauma was a predictor for continuation of AED prescription 5-10 years after the diagnosis of PNES was made.Reference Duncan, Graham, Oto and Russell 14 Of note, the continuation of AEDs might be considered to manage other comorbidities (e.g. neuropathic pain and psychiatric disorders such as depression or bipolar disorder).Reference Asadi-Pooya and Emami 11 , Reference Benbadis, Agrawal and Tatum 12 Part of PNES management is to have further neurology follow up visits to assess the overall progress of this condition as well as if necessary to explain again the diagnosis and supervise the AED withdrawal in the transition to mental health professional evaluation.
PROGNOSIS
As commented above, communicating the diagnosis to the patient may impact upon the outcomes of this condition and it has been shown that a standardized diagnostic approach and feedback process may reduce event frequency.Reference Drane, LaRoche and Ganesh 36 Other factors such as educational status and being accompanied to the first clinic visit have also been described as favorable predictors of outcomes.Reference Arain, Hamadani, Islam and Abou-Khalil 60 However, prospective studies evaluating the prognosis of these patients are controversial and some had shown poor outcomes despite an effective communication strategy.Reference Mayor, Brown and Cock 61 , Reference Salinsky, Storzbach, Goy, Kellogg and Boudreau 62 In a recent study assessing standard medical care for PNES across Brazilian epilepsy centers, none of the centers had a particular protocol with rigorous guidelines to provide the diagnosis and treat PNES.Reference Valente, De Paola and Palmini 63 This probably represents just an example of the need for guidelines regarding management of PNES in different countries. The physician presenting the diagnosis must be compassionate and remember that most of the patients with this problem are not intentionally faking. Patients who accept their diagnosis and follow through with therapy are more likely to experience a successful outcome. However, at least 50%-70% of the patients will have some improvement but will not be seizure freeReference Iriarte, Parra, Urrestarazu and Kuyk 64 and about one-quarter of the patients develop chronic PNES.Reference Bodde, Brooks and Baker 13
Psychological factors (including anxiety, depression and illness perceptions) are a stronger predictor of health-related QoL than condition-related and demographic variables in epilepsy and PNES. Therefore, different studies have shown the importance of addressing patients’ beliefs about their condition.Reference Rawlings, Brown and Reuber 65
Unfortunately, those patients with only improvement, but not cessation of PNES, continue to experience significant difficulties. Some of these difficulties include unemployment, depression, persistent visits to the emergency department and reduced QOL in both, patients and caregivers.Reference Karakis, Montouris and Piperidou 66 Karakis et al.Reference Karakis, Montouris and Piperidou 66 showed that QOL scores were significantly worse for PNES than for patients with epileptic seizures and were mainly linked to depression levels. In addition to the social and psychological impact, the financial burden of this disorder is high.Reference Sahaya, Dholakia, Lardizabal and Sahota 10 It is reported that over 50% of PNES patients are disabled.Reference Reuber and Mayor 2 An observational study suggested increased mortality in these patients.Reference Duncan, Oto and Wainman-Lefley 67 Although the overall outcome is poor in PNES,Reference Iriarte, Parra, Urrestarazu and Kuyk 64 some factors are associated with worse prognosis. Some examples are delay in the diagnosis, psychiatric hospitalizations, PTSD, sexual and/or physical abuse and psychiatric comorbidities such as depression or anxiety. Moreover, being single, specific coping strategies (escape-avoidance coping style), family functioning (unsupportive or uninterested family environment) and low socio-economic status also impact negatively the prognosis of PNES.Reference Myers, Lancman and Laban-Grant 16 , Reference Baslet and Prensky 68 , Reference Jones, Reuber and Norman 69 On the other hand, there are some factors that can predict treatment adherence and therefore improve the outcomes of these patients. A retrospective observational study showed that PNES patients who are married or have a live-in partner and subjects without cognitive impairment were more likely to be adherent.Reference Baslet, Seshadri and Bermeo-Ovalle 30
The prognosis in children with PNES might be better, with close to 70% achieving remission.Reference Irwin, Edwards and Robinson 70 , Reference Yi, Kim, Lee, Cheon and Kang 71 However, this needs to be read with caution as the results are based in small retrospective studies, so bigger cohorts and prospective research studies are needed in this population. Psychiatric illness (especially depression) has been shown to be frequent in this population.Reference Vincentiis, Valente and Thomé-Souza 21 A delay in the diagnosis may result in iatrogenic complications. Therefore, identifying PNES in childhood and adolescence should be considered of the utmost importance.Reference Say, Tasdemir and Akbas 20
DISCUSSION
PNES continues to be both a diagnostic and treatment challenge. It is associated with significant morbidity that it is comparable with a population with epilepsy and according to some authors may even be associated with a worse outcome. Furthermore, at this time there is no consensus on the management of PNES; overall strategies are based on small case series. A significant percentage of patients with PNES continue to manifest symptoms which profoundly affect the individual.
We have proposed a diagnostic and treatment algorithm suggesting a multidisciplinary approach to probably improve the outcomes of patients suffering from PNES. A national registry of patients with PNES, their treatment and outcomes may help improve the understanding of this entity and establish more effective treatment strategies and guidelines through coordinated research and “big data” collaborations across the country (see Table 4 for unanswered questions and future directions).
The coexistence of epilepsy and PNES poses special challenges and requires the coordinated efforts of the psychiatrist and the neurologist, particularly when seizure threshold-lowering drugs need to be administered. The use of CBT and other modalities of psychotherapy should be further evaluated in bigger cohort of patients.
Table 1 Key points
Table 2 Epidemiology of psychogenic non-epileptic seizures (PNES)
Table 3 Common factors and comorbidities in psychogenic non-epileptic seizures (PNES)
Table 4 Unanswered questions and possible future directions
PNES, psychogenic non-epileptic seizures.
Acknowledgments
ÁM-T acknowledges the financial support received by Dr. KF and Dr. CMS for her research fellowship in sleep medicine at the psychiatry department in Toronto Western Hospital. ÁM-T also thanks Dr. KF, Dr. CMS, Dr. MD, and MP for their intellectual input, writing assistance, language editing, and proofreading.
Disclosures
ÁM-T, MP, MdC, CMS and KF do not have any disclosures.
Statement of Authorship
Authors contributed equally to this work.









