Introduction
Stroke prevention, treatment, and recovery have completely transformed over the past several decades due to research breakthroughs, increased awareness, and improvements to systems of care. Canada continues to be a world leader in driving innovation and change across the stroke continuum of care. In Canada, in 2017, there were 108,707 hospital visits for an acute stroke event, Reference Holodinsky, Lindsay, Yu, Ganesh, Joundi and Hill2 and stroke remains a leading cause of adult disability with over 878,000 people living in Canada with the consequences of stroke. Reference Krueger, Koot, Hall, O’Callaghan, Bayley and Corbett3 In Canada, stroke systems of care have been growing since the late 1990s when acute thrombolysis became available. Currently, 232 hospitals (35%) are capable of providing acute thrombolysis, and this number now includes 155 hospitals with dedicated stroke teams and 95 acute stroke units. Twenty-five hospitals in Canada provide endovascular thrombectomy (EVT). Reference Lindsay4 The global pandemic caused by the COVID-19 virus brought increased risk and worse outcomes for people with stroke and impacted response times by both the public and healthcare providers. Reference Nogueira, Abdalkader and Qureshi5–Reference Ntaios, Michel and Georgiopoulos8
The 7th update of the Canadian Stroke Best Practice Recommendations (CSBPR) for Acute Stroke Management is a timely opportunity to reassess current processes to ensure efficient access to acute stroke diagnostics, treatments, and management strategies, which have proven to reduce mortality and morbidity. The topics covered include those related to prehospital care, emergency department (ED) care, acute treatments with intravenous thrombolysis and EVT, the prevention and management in hospital complications, vascular risk factor reduction strategies, early rehabilitation, and end-of-life care. The theme of the 7th edition of this CSBPR is building connections to optimize individual outcomes. Following an acute stroke, persons often present with multiple comorbid conditions, some of which may have contributed to their stroke, some that are the consequence of their stroke, and some which are unrelated. In many cases, comorbidities such as hypertension, carotid stenosis, and patent foramen ovale (PFO) may be first detected at the time of stroke. Regardless of the etiology, persons presenting with stroke and multiple comorbidities are more complex and are at risk of worse outcomes. These comorbid conditions must be considered within the treatment and care planning process to ensure effective and person-centered care.
The CSBPRs are intended to provide up-to-date evidence-based guidelines for the prevention and management of stroke and to promote optimal recovery and reintegration for people who have experienced stroke, including patients, families, and caregivers. The goal of disseminating and implementing these recommendations is to optimize evidence-based stroke care across Canada to reduce practice variations in care delivery and to narrow the gap between current knowledge and clinical practice. These recommendations have been developed in collaboration with the Canadian Stroke Consortium, Canada’s national organization of stroke physicians. The recommendations are applicable to all healthcare providers, health system leaders and planners, and people living with stroke. The CSBPR Acute Stroke Management 2022, 7th edition supersedes all recommendations contained in the 2018 CSBPR 6th edition of Acute Stroke Management. Reference Boulanger, Lindsay and Gubitz9
Guideline Development Methodology
The CSBPR development and update process follows a rigorous framework Reference Graham, Harrison, Brouwers, Davies and Dunn10,Reference Vernooij, Alonso-Coello, Brouwers and Martinez Garcia11 and addresses all criteria defined within the Appraisal of Guidelines for Research and Evaluation II (AGREE II) Instrument components. Reference Brouwers, Kho and Browman12 The methodology for development and updates to the CSBPR has been previously published, Reference Gladstone, Lindsay and Douketis13 and detailed methodology can be found on our Canadian Stroke Best Practices website at www.strokebestpractices.ca. An interdisciplinary group of experts was convened and participated in reviewing, drafting, and revising all recommendation statements. Eight people with lived experience of stroke (seven people with stroke and one caregiver) also actively participated in the review and update process as part of our acute stroke community consultation and review panel. Reference Lindsay, Gierman and Harris14
Searches were conducted by experienced personnel to identify peer-reviewed literature that examined each topic area addressed in the current module. Systematic reviews, meta-analyses, randomized controlled trials, and observational studies were included, as available. The literature for this module was current to September 2022. Following a standardized abstraction format, evidence tables were constructed including content from selected studies and provided to the writing group for review. The writing group discussed and debated the strength, importance, clinical relevance, and applicability of the evidence and, through consensus, developed a draft set of proposed recommendations. During this process, additional literature may have been identified and used to develop a final set of proposed recommendations. Evidence levels were assigned based on the quality of available evidence, using the Grading of Recommendations, Assessment, Development and Evaluations (GRADE) system. Reference Guyatt, Oxman and Akl15–Reference Guyatt, Oxman and Vist17 Expert opinion was used to formulate recommendations in the absence of evidence. These guidelines have undergone extensive internal and external review, and consensus was achieved for all content. For additional details of the methodology and additional materials to support these recommendations, including rationales, system implications, performance measures, knowledge translation and implementation tools, evidence tables, and an extended summary of the evidence, please visit: www.strokebestpractices.ca. Supplemental online materials are available with this publication to support many of the recommendations included.
Summary of Changes and Updates in the Acute Stroke Management Stroke, 7th Edition, 2022
Significant updates and new additions to the CSBPR for Acute Stroke Management, 7th edition 2022 are based, in part, on the results from several new, important clinical trials. Notable changes in the 7th edition include recommendations pertaining the use of tenecteplase, thrombolysis as a bridging therapy prior to mechanical thrombectomy, dual antiplatelet therapy (DAPT) for stroke prevention, Reference Johnston, Amarenco and Denison1 the management of symptomatic intracerebral hemorrhage (ICH) following thrombolysis, acute stroke imaging (Section 4), pre- and post-op care of patients undergoing EVT (Section 5), medical assistance in dying (MAiD) (Section 11), and virtual stroke care in the ED and inpatient care (Sections 4 and 8). An explicit effort was made to address sex and gender differences wherever possible. The first four sections of this guideline pertain to all people presenting with signs of acute stroke or TIA. The remaining sections pertain largely to the management of acute ischemic stroke and TIA. Guidelines for the management of patients with ICH were released in 2020, Reference Shoamanesh, Patrice Lindsay and Castellucci18 while those for subarachnoid hemorrhage and cerebral venous thrombosis are in development.
Acute Stroke Management Recommendations, 7th Edition, Update 2022
Note, please refer to online Supplemental Material accompanying these recommendations for additional definitions, information, inclusion criteria, and other implementation content. This manuscript has been translated into French and is also available as an online supplement.
Section 1: Stroke Awareness, Recognition, and Response
Many members of the general public are unable to recognize the signs and symptoms of a stroke, or they attribute them to a less serious health issue. Reference Naguib, Fayed, AlFadhliah, AlMansour, AlDakheel and AlQahtani19–Reference Metias, Eisenberg and Clemente21 While 61% of the population in Canada knows at least one sign of stroke, only 33% know at least two and only 10% know all three, based on the FAST (Face, Arms, Speech, Time) mnemonic. 22 The failure to recognize the signs of an acute stroke, either by the persons witnessing one or the person experiencing one, can delay contact with emergency services, which may in turn decrease a patient’s opportunity to receive time-sensitive treatments. The number of public health campaigns designed to increase recognition of the signs and symptoms of stroke has increased over the past decade. One of the best recognized programs in the healthcare community is FAST. The results of a systematic review Reference Tan, Ramazanu, Liaw and Chua23 suggest that stroke education using mass media campaigns can increase the likelihood of symptom recognition by 20% and increase the likelihood that persons would call emergency services by 19%. Mass media campaigns have also been shown to be associated with increases in the use of thrombolytic agents following acute stroke. Reference Advani, Naess and Kurz24

Section 2: Triage and Initial Diagnostic Evaluation of Transient Ischemic Attack (TIA) and Non-Disabling Stroke
People experiencing signs of stroke require rapid assessment, diagnosis, and determination of risk for a recurrent stroke. Patients diagnosed to have TIA, or subacute, non-disabling ischemic strokes who are not candidates for hyperacute treatment with intravenous thrombolysis and/or EVT still require timely assessment and management, which can often be provided in an outpatient setting. The goal of outpatient management is to rapidly identify neurovascular risk factors, which may have precipitated the index event, and to initiate treatments to reduce the risk of recurrent events. The increased use and availability of sensitive neuroimaging to identify minor events as well as the increased use of antiplatelet agents, anticoagulants, antihypertensive agents, lipid-lowering agents, and carotid revascularization has been shown to significantly reduce the risk of major stroke after an initial minor event in recent years. In the TIARegistry.Org group study, 78.4% of patients were seen by a stroke specialist within 24 h of the event. Reference Amarenco, Lavallee and Labreuche25 Most patients received key urgent investigations before discharge, and appropriate treatments were initiated. For example, 5.0% of patients received a new diagnosis of atrial fibrillation, of which 66.8% received anticoagulant therapy before discharge. Carotid stenosis of ≥50% was found in 15.5% of patients, of which 26.9% underwent carotid revascularization before discharge. The 1-year estimate of risk of the primary outcome, a composite of death from cardiovascular causes, nonfatal stroke, and nonfatal acute coronary syndrome, was 6.2% (95% confidence interval [CI] 5.5–7.0%). Estimates of stroke at days 2, 7, 30, 90, and 365 were 1.5%, 2.1%, 2.8%, 3.7%, and 5.1%, respectively. These estimates were almost half of those compared with historical cohorts, possibly reflecting faster access to preventive care in the contemporary cohort. The availability of TIA outpatient clinics appears to be increasing. Based on the results of a geospatial analysis, there were 123 secondary prevention clinics in Canada, as of 2016. Reference Jewett, Harroud and Hill26 While over 87% of the population had access to such a clinic within a 1-h drive, only 69.2% has access to a service that operates 5–7 days a week.

Section 3: Emergency Medical Services
Emergency medical services (EMS) play a critical role in prehospital assessment and management of patients with suspected stroke. Patients arriving to hospital using EMS following a stroke experience fewer delays in receiving appropriate diagnostic tests, and are more likely to receive revascularization treatments, if eligible. In 2020, 69.0% of patients with stroke admitted to hospital in Canada were transported by EMS. Reference Eswaradass, Swartz, Rosen, Hill and Lindsay30 The odds of a patient receiving treatment with intravenous thrombolysis were increased by 52% if the patient was transported by EMS and increased by 75% if a system of hospital prenotification was employed. Reference Nielsen, DeJoie-Stanton, Song, Christie, Guo and Zachrison31 Given the time-sensitive nature of acute stroke treatment, it is imperative that patients who may be candidates for these therapies be transported directly to comprehensive stroke centers as quickly as possible and whenever possible. The 90-day outcomes of patients who received EVT following direct transport have been shown to be better than those who were first transported to a primary stroke center. Reference Ismail, Armoiry and Tau32,Reference Mohamed, Fatima, Shuaib and Saqqur33 However, in a recent cluster-randomized trial Reference Price, Shaw and Islam34 in which paramedics transporting patients with ischemic stroke were randomized to the PASTA pathway (including structured prehospital information collection, prompted prenotification, and structured handover of information) or standard care, there was no significant difference between groups in the proportion of patients who received thrombolysis (49.7% [PASTA] vs. 52.6% [standard care], adjusted odds ratio [OR]=0.84, 95% CI 0.60–1.17). Paramedics in the PASTA group took an average of 13.4 min longer to clear a care episode.
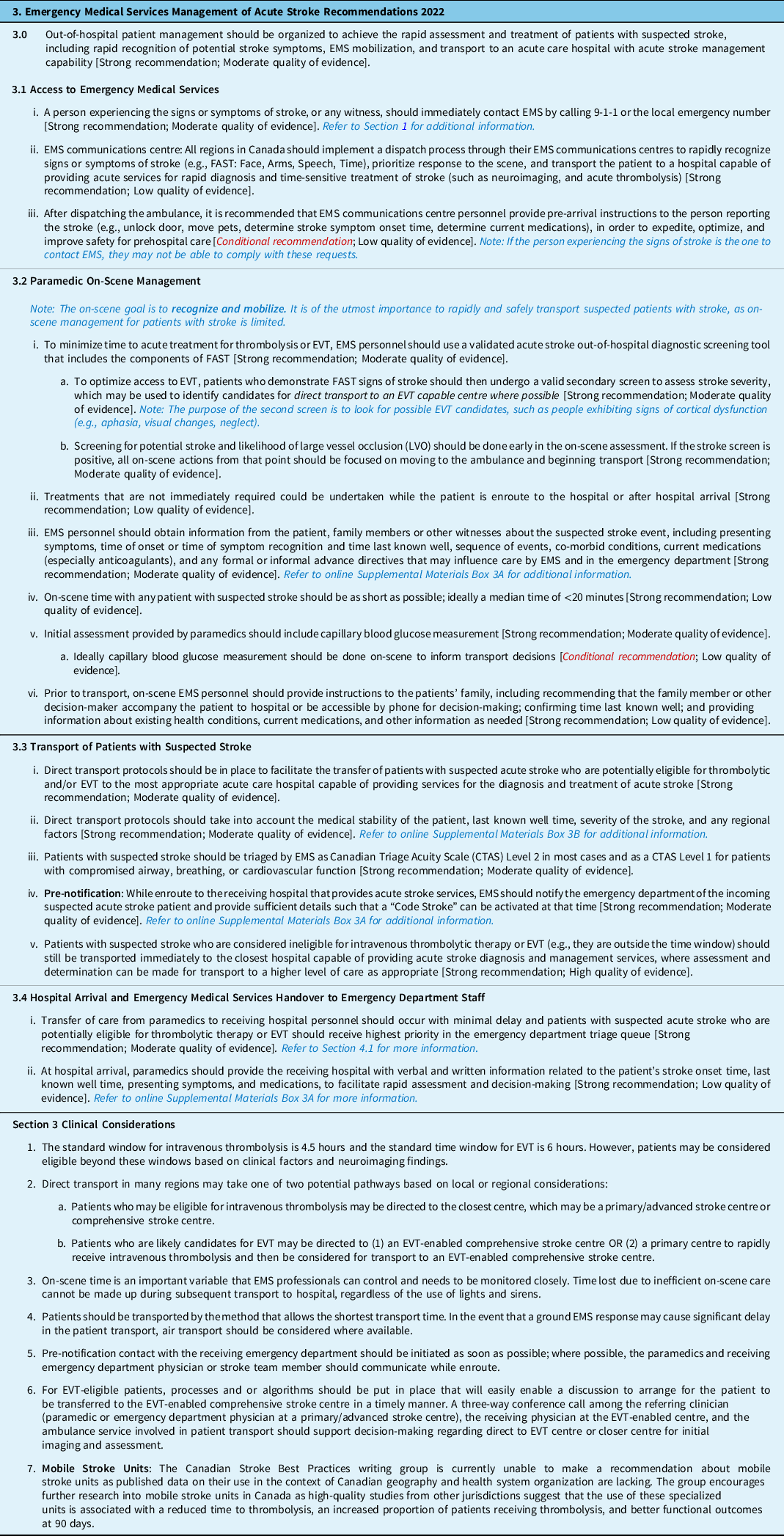
After completing a brief screen tool to confirm signs and symptoms of a stroke, using an instrument such as FAST Reference Harbison, Hossain, Jenkinson, Davis, Louw and Ford35 or the Cincinnati Prehospital Stroke Scale, Reference Kothari, Pancioli, Liu, Brott and Broderick36 EMS personnel should then conduct a subsequent screen to identify potential patients with large vessel occlusions (LVOs) in the anterior circulation who may be potential candidates for EVT. While several validated scales are currently available, most of which are derived from 3–6 components of the National Institutes of Health Stroke Scale (NIHSS), the sensitivities and specificities of these scales are not ideal Reference Smith, Kent and Bulsara37 and most have not been externally validated in the field.
Section 4: Emergency Department Evaluation
Standard assessments for patients with suspected acute stroke presenting to the ED include a rapid neurological examination and urgent brain and vascular imaging, followed by monitoring of vital signs, blood work, cardiovascular investigations, blood pressure management, glucose control, dysphagia screening, and seizure assessment. Given that some acute stroke symptoms including fatigue, anxiety, and dizziness may overlap with other cardiovascular and general medical conditions, Reference Jurgens, Lee and Aycock38 it is important to identify patients who are experiencing stroke “mimics” and to avoid unnecessary and expensive investigations and inappropriate long-term prevention treatments. Patients presenting with stroke symptoms may ultimately be diagnosed with other conditions such as migraine headache, vertigo, metabolic disturbances, brain tumors, or presyncope/syncope. Reference Karliński, Gluszkiewicz and Członkowska39 The NIHSS can be used to quickly screen for stroke-specific symptoms. For all patients arriving to hospital with suspected stroke or TIA, immediate brain and vascular imaging is the highest priority investigation once any life-threatening issues with respiration and circulation have been ruled out or addressed. A non-contrast CT scan is considered to be the imaging standard and the most cost-effective method to be used initially to identify acute ischemic stroke and to rule out intracranial hemorrhage. Reference Wardlaw, Seymour, Cairns, Keir, Lewis and Sandercock40 While MRI with DWIs may be more sensitive in detecting early changes associated with ischemia, especially in patients with small infarcts, this technology may be not immediately available in many centers. Reference Brazzelli, Sandercock and Chappell41 In the year 2019/20, there were 288 MRI machines in 378 facilities across Canada, equating to an availability of 10 units per million population. Reference Chao, Sinclair, Morrison, Hafizi and Pyke42 Combined multimodal vascular imaging is extremely important, and in highly selected cases, perfusion scans with CT or MRI has the potential to identify patients with an ischemic penumbra and potentially viable brain tissue who may be appropriate for acute reperfusion therapies. Perfusion scans can be especially useful in selecting patient eligible for endovascular therapy in the 6-to-24-h window whereas in the 0-to-6-h time frame, and most cases can be selected with the use of CT and CTA alone.

Section 5: Acute Ischemic Stroke Treatment
While the weight of evidence clearly indicates that treatment with intravenous alteplase, administered within 4.5 h of symptom onset, improves functional outcomes and reduces the risks of death or disability, Reference Hacke, Lyden and Emberson44,Reference Lees, Emberson and Blackwell45 there are limited data on the benefit of treatment beyond this window. The most recent trials of thrombolytic therapy in the extended time window include EXTEND Reference Ma, Campbell and Parsons46 and WAKE-UP, Reference Thomalla, Simonsen and Boutitie47 in which patients presenting with symptoms beyond 4.5 h or with unknown time of onset were selected for treatment on the basis of advanced imaging. In both trials, patients receiving alteplase were more likely to achieve an excellent outcome (mRS 0–1) at 90 days, relative increase 44% Reference Ma, Campbell and Parsons46 % and 61%, Reference Thomalla, Simonsen and Boutitie47 symptomatic ICH and death were higher in the intervention group.
The results from several recent trials indicate that tenecteplase, a newer thrombolytic agent that has pharmacokinetic advantages over alteplase, is non-inferior to alteplase. Among the completed trials to date, the AcT trial Reference Menon, Buck and Singh48 was the first to report that tenecteplase at a dose of 0.25 mg/kg (maximum 25 mg) is non-inferior to standard dose alteplase. At 90 days, 36.9% of patients in the tenecteplase group achieved the primary outcome (mRS score of 0–1) versus 34.8% in the alteplase group (unadjusted difference = 2.1%, 95% CI -2.6% to 6.9%; adjusted relative risk [RR] = 1·1, 95% CI 1·0 to 1·2), meeting the non-inferiority threshold (the lower bound 95% CI of which was set at greater than -5%). There was no significant difference between groups in terms of mortality at 90 days (15.3% vs. 15.4%), or in the proportion with symptomatic ICH at 24 h (3.4% vs. 3.2%). In contrast to these findings, the NOR-TEST 2 Reference Kvistad, Næss and Helleberg49 trial of alteplase versus tenecteplase 0.4 mg/kg was halted early due to safety concerns, which included an increased risk of intracranial hemorrhage and mortality; however, the dose in the tenecteplase group was higher (0.4 mg/kg) than is currently recommended (0.25 mg/kg). In the EXTEND-IA TNK, Reference Campbell, Mitchell and Churilov50 where patients with LVO received treatment with both thrombolysis and EVT, a significantly higher number of patients receiving tenecteplase 0.25 mg/kg achieved substantial reperfusion (22% vs. 10%, p = 0.02 for superiority), although the percentage of patients who were functionally independent at 90 days or who had achieved an excellent outcome did not differ between groups. Several clinical trials comparing tenecteplase with alteplase (ATTEST2 NCT0281440) and tenecteplase with placebo, or best medical management (TIMELESS NCT03785678, TWIST NCT03181360, and TEMPO-2 NCT02398656) are ongoing.
A 2021 Cochrane review Reference Roaldsen, Jusufovic, Berge and Lindekleiv51 that included the results of 19 trials adds to the growing body of evidence indicating that EVT performed within 6 h of symptom onset is an extremely effective treatment for patients with LVO in the anterior circulation. Treatment with EVT was associated with a significantly higher likelihood of favorable outcome (RR = 1.61, 95% CI 1.42 to 1.82) with a high certainty of evidence, without a significantly increased risk of symptomatic intracranial hemorrhage (RR = 1.46, 95% CI 0.91 to 2.36) compared with usual care, which in many cases included the use of alteplase. For selected patients, the treatment window for EVT may be even longer. A pooled analysis of six randomized controlled trials Reference Jovin, Nogueira and Lansberg52 including patients who received treatment between 6 and 24 h after the onset of symptoms also found significantly better outcomes in patients in the intervention group. There was a significant shift in the ordinal analysis of mRS scores favoring less disability in the thrombectomy group (adjusted OR =2·54, 95% CI 1·83–3·54). The odds of achieving an mRS score of 0–1 or 0–2 at 90 days were both significantly higher in the EVT group (adjusted OR = 2·41, 95% CI 1·07–5·43 and adjusted OR = 3·88, 95% CI 1·94–7·78, respectively). The number needed to treat for one more patient to be independent with EVT was 2.6.

Section 6: Acute Antiplatelet Therapy
Early antiplatelet therapy, provided soon after ischemic stroke, is known to improve outcomes. Acetylsalicylic acid (ASA) is the most commonly used agent. Results from two of the largest trials of ASA from several decades ago, the Chinese Acute Stroke Trial (CAST) 54 and the International Stroke Trial (IST) 55 represent the majority of the evidence base. In CAST, there were 5.4 fewer deaths and 4.7 fewer recurrent strokes per 1000 patients treated with daily aspirin of 160 mg after 4 weeks. In the aspirin arm of the factorial IST, patients with a suspected acute ischemic stroke received 300 mg/day of aspirin and a similar number avoided aspirin for 14 days. The risk of recurrent ischemic stroke was significantly lower in the aspirin arm, with a number needed to treat of 91, with no significant difference between groups in the frequency of symptomatic ICH.
Short-term DAPT, for up to 21 days following ischemic stroke, with either clopidogrel or ticagrelor is more effective than ASA alone in reducing the risk of recurrent ischemic stroke in selected patients. In the POINT trial, Johnston et al. Reference Johnston, Easton and Farrant56 estimated that for every 1,000 patients treated with 75 mg clopidogrel plus 81 mg aspirin for 90 days, 15 ischemic strokes would be prevented but 5 major hemorrhages would result. The greatest protection from treatment was seen in the first 21 days during which the risk of a major ischemic event was lowered by 35%. Although the antiplatelet regimen in the CHANCE trial Reference Wang, Wang and Zhao57 was slightly different than in the POINT trial, the results were similar, in that the risk of recurrent ischemic stroke was reduced by 33% in the DAPT group. In the THALES trial, Reference Johnston, Amarenco and Denison1 patients with minor acute ischemic stroke treated with 90 mg ticagrelor twice a day + 75–100 aspirin mg/day also experienced fewer recurrent strokes and death within 30 days (5.5% vs. 6.6%, HR = 0.83, 95% CI 0.71–0.96, number needed to treat =92), compared with patients treated with aspirin alone. Reference Johnston, Amarenco and Denison1 However, these benefits were accompanied by a 3.5 to 4 times increased risk of severe or fatal bleeding and intracranial hemorrhage.

Section 7: Hemicraniectomy
Due to higher risks of cerebral edema, increased intracranial pressure, and subsequent cerebral herniation, mortality is higher for patients with malignant MCA stroke. For these patients, decompressive hemicraniectomy may be a surgical option. In persons under the age of 60 years, early decompressive hemicraniectomy increases the odds of a reasonable functional outcome (mRS score of 0–3) at 1 year. Reference Hofmeijer, Kappelle, Algra, Amelink, van Gijn and van der Worp58–Reference Vahedi, Vicaut and Mateo60 The data are limited for patients over the age of 60 years. In the DESTINY 2 trial, Reference Jüttler, Unterberg and Woitzik61 82 patients with a median age of 70 years were randomized to hemicraniectomy or standard care: a significantly higher proportion of patients in the surgical group were alive and living without severe disability (mRS score of 0–4) at 6 months (38% vs.18%, OR = 2.91, 95% CI 1.06–7.49) compared with patients in the medical management group. However, no patients in either the surgical or medical care groups had overall good outcomes (mRS score of 0–2) at 6 or 12 months and most of the survivors required assistance with most bodily needs. In a recent systematic review, which included the results from seven trials, including DESTINY 2, as well as six trials of patients aged <60 years (DESTINY, Reference Jüttler, Schwab and Schmiedek59 DESTINY II, Reference Jüttler, Unterberg and Woitzik61 DECIMAL, Reference Vahedi, Vicaut and Mateo60 and HAMLET), Reference Reinink, Jüttler and Hacke62 the odds of a favorable outcome (mRS 0–3) at 1 year were significantly higher in the surgical group (adjusted OR = 2.95, 95% CI 1.55–5.60) and the odds of death at 1 year were significantly lower (adjusted OR = 0.16; 95% CI 0.10–0.24).

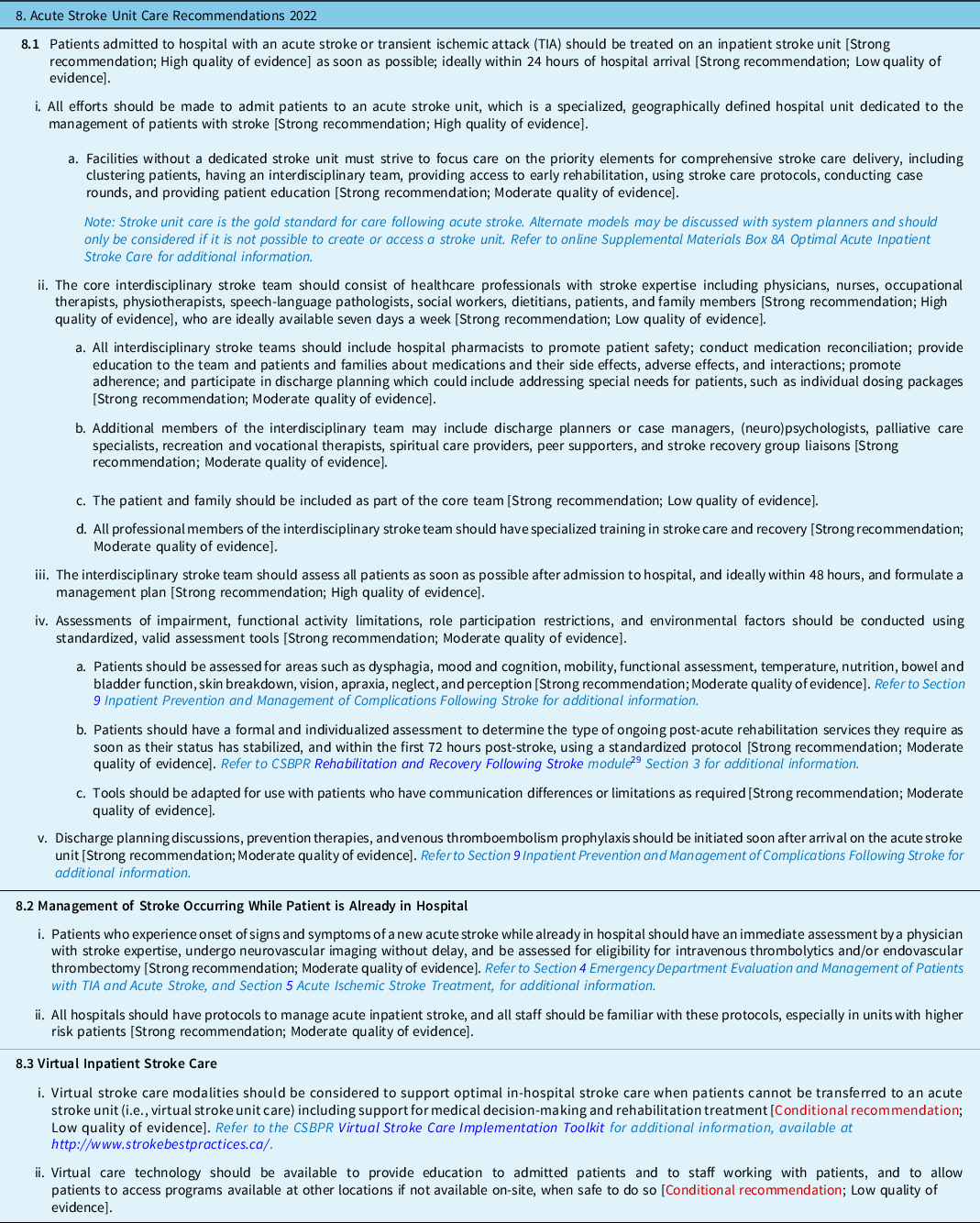
Section 8: Acute Stroke Unit Care
Patients who are admitted to stroke units are more likely to survive, return home, and regain their independence compared to patients who are admitted to non-specialized units. The most recent update of the Stroke Unit Trialists’ Collaboration Reference Langhorne and Ramachandra63 identified 29 randomized and quasi-randomized trials, including 5,902 participants, comparing stroke unit care with alternative, less organized care (e.g., an acute medical ward). Compared to less organized forms of care, stroke unit care was associated with a significant reduction in the odds of death (OR = 0.76, 95% CI 0.66 to 0.88), a poor outcome (OR = 0.77, 95% CI 0.69 to 0.87), and death or dependency (OR = 0.75, 95% CI 0.66 to 0.85) at a median follow-up of 1 year. These results were based on moderate quality evidence. Stroke unit care was superior regardless of age, sex, initial stroke severity, stroke type, trial quality, and duration of follow-up. In Canada, access to stroke unit care varies by region. A survey conducted in 2013/14 identified 32 stroke units within the province of Ontario, of which 21 were acute stroke units, 10 were integrated stroke units, and 1 which was classified as a rehabilitation stroke unit. Reference Rac, Sahakyan and Fan64 The estimated average number of stroke patients served per stroke unit was 604 with large variation across centers.
Section 9: Inpatient Prevention and Management of Complications Following Stroke 2022
Medical complications are relatively common following stroke and may negatively impact the recovery process, with the potential to result in poorer outcomes. Reference Johnston, Li and Lyden65 Estimates of the percentage of patients who experience at least one medical complication during hospitalization vary widely from 25% Reference Ingeman, Andersen, Hundborg, Svendsen and Johnsen66 to 85%. Reference Langhorne, Stott and Robertson67 Some of the most commonly cited complications include urinary tract infections, fever, pneumonia, and deep vein thrombosis (DVT). Examples of measures that can be taken to reduce the risks of these complications include pharmacological venous thromboembolism prophylaxis, Reference Sandercock and Leong68 and the use of thigh-high intermittent pneumatic compression (IPC) devices, Reference Dennis, Sandercock, Reid, Graham, Forbes and Murray69 to prevent thromboembolism, dysphagia screening to reduce the risk of pneumonia, Reference Titsworth, Abram and Fullerton70 and the avoidance of the use of indwelling catheters to prevent urinary tract infections. Reference Ersoz, Ulusoy, Oktar and Akyuz71 Early mobilization post-stroke can reduce the length of hospitalization and is associated with greater ability to perform activities of daily living at 3 months. Reference Langhorne, Collier, Bate, Thuy and Bernhardt72 Cardiac investigations should also be conducted to identify previously undetected or paroxysmal atrial fibrillation, or other cardiac abnormalities. Reference Haeusler, Kirchhof and Kunze73,Reference Wachter, Gröschel and Gelbrich74

Section 10: Advance Care Planning
Advance care planning (ACP) is a process of reflection and communication in which individuals reflect on their wishes and values to make decisions regarding their healthcare in consultation with healthcare providers, should they become incapable of participating in decision-making at a later date. 76 While there is evidence supporting ACP in the primary care setting, there are limited data on ACP in acute care in general, and even less following stroke. Green et al. Reference Green, Gandhi, Kleissen, Simon, Raffin-Bouchal and Ryckborst77 used participant observation and semi-structured interviews to gather information related to the communication process regarding ACP from 14 patients, recruited from an acute stroke unit and 2 rehabilitation units, and 4 HCPs. Four key themes emerged as to why or why not participants engaged in the ACP process. First, there was a perceived lack of urgency by participants, many of whom felt the physician and/or family members would make decisions in accordance with their wishes; second, there was a lack of initiation by HCPs to discuss issues around ACP; third, HCPs expressed hesitation about initiating discussions related to ACP, and uncertainty as the best timing for such discussions. Fourth, there was also a lack of understanding of ACP, especially as compared to advance directives, designation of care, and living wills.
Although no stroke-specific studies have been published that examine the effectiveness of ACP, several studies included patients with stroke. Results from a small number of studies suggest that interventions aimed at increasing ACP have been successful in significantly increasing the likelihood that end-of-life wishes are known and respected. Reference Detering, Hancock, Reade and Silvester78,Reference Kirchhoff, Hammes, Kehl, Briggs and Brown79

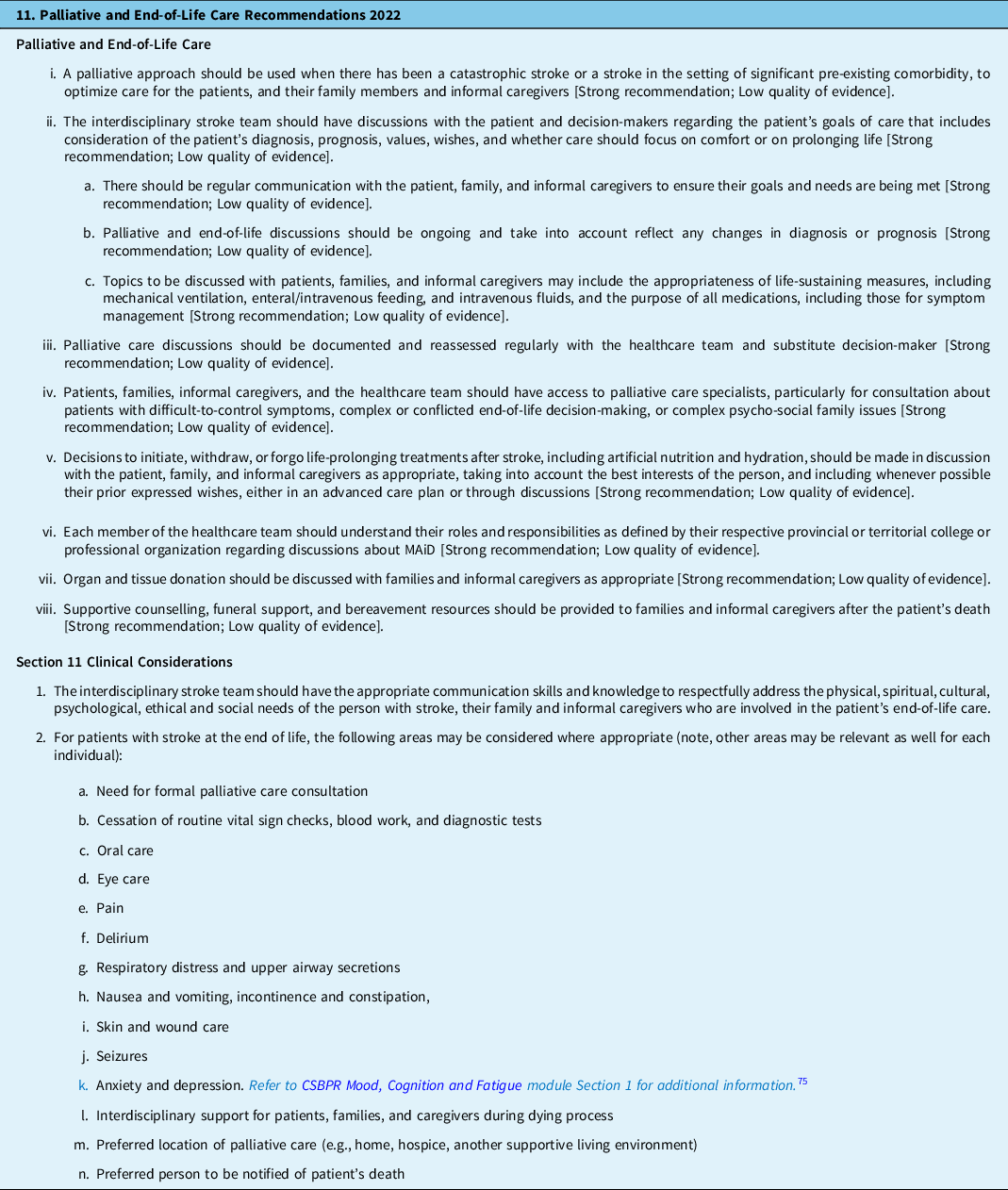
Section 11: Palliative and End-of-Life Care
Palliative care is an approach that aims to reduce suffering and improve the quality of life for people who are living with life-limiting illness through the provision of pain and symptom management, psychological, social, emotional, spiritual, and practical support, and support for caregivers during the illness and after the death of the person they are caring for. 80 Palliative care provides comprehensive care throughout a person’s illness trajectory and is not solely limited to end-of-life care. The role of palliative care may be complicated as prognosis in the earliest phase of stroke can be unclear. Reference Holloway, Arnold and Creutzfeldt81 There is currently no integrated model of palliative care in stroke care addressing the appropriate moment to initiate palliative care discussions Reference Steigleder, Kollmar and Ostgathe82 or which healthcare provider(s) should raise the topic; however, there is agreement that the approach should be interdisciplinary and patient- and family-centered. The palliative care needs of patients following stroke are typically related to the management of common symptoms such as dyspnea, pain, and xerostomia. Reference Mazzocato, Michel-Nemitz, Anwar and Michel83 While palliative care pathways have been developed to ensure that patients receive the most appropriate care possible in the last days of life, there is an absence of high-quality evidence to suggest that current pathways are effective, highlighting the need for additional research in this area. Reference Chan, Webster and Bowers84 In terms of specific interventions designed to address many common palliative care issues, a systematic review by Cowey et al. Reference Cowey, Schichtel and Cheyne85 concluded that there was insufficient evidence to recommend the best and most effective approaches to this important and essential component of care.
Challenges and Future Directions
The 7th update of the Canadian Stroke Best Practice Recommendations for Acute Stroke Management provides a detailed series of recommendations applicable to the care of all adults in Canada who have sustained an ischemic stroke or TIA. These guidelines have been developed through a rigorous process; efforts must now turn to their rapid implementation, especially of the new recommendations, based on emerging high-quality evidence, so as to increase equitable access to timely acute stroke care for all people in Canada.
This edition of the guidelines has incorporated Tenecteplase 0.25 mg/kg as an alternate thrombolytic for acute ischemic stroke based on the landmark Canadian AcT trial. It is expected that the knowledge of the clinical applications of tenecteplase will continue to advance, particularly as it pertains to its use in the setting of patients with intracranial arterial occlusions who may or may not be candidates for thrombectomy.
Thrombectomy with or without thrombolysis is the topic of several recent randomized trials; this issue will likely be settled by the time the next edition of these guidelines is ready for publication. At present, trials that most closely reflect Canadian practice suggest that thrombolysis should NOT be withheld for patients who are also candidates for thrombectomy; all eligible patients should receive thrombolysis, regardless of whether they also may receive thrombectomy. We acknowledge the possibility that further refinement in the understanding of the risks and benefits of combination therapy could alter these recommendations. Specifically, it is anticipated that further experience with tenecteplase may impact this calculus in important ways.
We are also excited about the prospect of further developments in the evidence to support EVT for patients with acute ischemic stroke of the posterior circulation. These patients were excluded from the landmark thrombectomy trials published between 2014 and 2018, and upon which current recommendations are based. With the advent of data from high-quality randomized trials, we expect to be able to provide more specific recommendations about thrombectomy for patients suffering strokes of the posterior circulation in the next edition of these guidelines.
The field of neuroprotection is also likely to advance in the coming years. The ESCAPE NA-1 trial suggested that nerinetide could be an effective neuroprotectant in patients with acute ischemic stroke not receiving thrombolysis, and that hypothesis is currently being tested in the Canadian-led ESCAPE NEXT trial. If that trial should be successful, it will be the first instance in the history of clinical neuroscience that a neuroprotectant agent has been found to be clinically effective in humans. Such a discovery could have significant ramifications for the management of acute ischemic stroke and may also influence the care of patients with ICH, subarachnoid hemorrhage, traumatic brain injury, and cardiac arrest.
The advent of mobile stroke units suggests radical change in the way acute stroke care could be delivered, at least for some people in Canada. While high-quality randomized trials in the USA, Germany, and Australia have suggested that mobile stroke units reduce time to treatment, increase treatment eligibility, and lead to better outcomes, we do not feel able to provide specific recommendations for Canadian practice until real-world research addresses our political, economic, and geographic realities. We hope that further research will help to address the question of how mobile stroke units may contribute to the further optimization of stroke care in Canada.
Lastly, at this time, our knowledge of sex and gender differences in acute stroke is evolving. In addition to pregnancy and hormone therapy, the prevalence of risk factors such as hypertension and atrial fibrillation are higher in women. Stroke symptom severity, presentation, and treatment effectiveness are areas that require further research.
The focus throughout these guidelines and stroke systems development in Canada and globally has been on an integrated system to provide seamless care to the patient with vascular risk factors and multimorbidity. Such an approach requires coordinated systems to be in place in all regions of Canada; a challenge given its vast geographical area with many smaller isolated communities. Quality monitoring and efforts to improve care are ongoing, and these recommendations will be updated within the next several years as new evidence emerges.
Supplementary material
To view supplementary material for this article, please visit https://doi.org/10.1017/cjn.2022.344.
Acknowledgments
Heart & Stroke gratefully acknowledges the Acute Stroke Management writing group leaders and members, all of whom have volunteered their time and expertise to the update of these recommendations. Members of the Canadian Stroke Consortium were involved in all aspects of the development of these recommendations. The recommendations underwent external review by: Philip A Barber, Treena Bilous, Renee Denise Cashin, Luciana Catanese, Seemant Chaturvedi, Michael Chow, Adam A. Dmytriw, Ian Drennan, Claire Dyason, Barb Field, Romayne Gallagher, Peter A. Gooderham, M. Shazam Hussain, Ebru Kaya, Katie Lin, Gordon McDonald, Stefan Pagliuso, Trudy Robertson, Julie Savoie, Joanna Schaafsma, Brenda Semenko, Ravinder Jeet Singh, Sean William Taylor, Aleksander Tkatch, Jenny P. Tsai, Gregory Brett Walker, and Hope Weisenberg.
We thank the Canadian Stroke Best Practices and Quality Advisory Committee members: Eric E. Smith (Co-Chair), Anita Mountain (Co-Chair), Aline Bourgoin, Gord Gubitz, Dar Dowlatshahi, Dylan Blacquiere, Margie Burns, Louise Clement, Thalia Field, Farrell Leibovitch, Christine Papoushek, Jeffrey Habert, Joyce Fung, Michael D Hill, Eddy Lang, Pascale Lavoie, Beth Linkewich, Colleen O’Connell, Jai Shankar, Debbie Timpson, Theodore Wein, and Katie White. The performance measures were reviewed and updated by the Heart & Stroke health systems quality council including Amy Yu (Chair), Michael Hill, Aravind Ganesh, Sacha Arsenault, Christine Hawkes, Jessalyn Holodinsky, Raed Joundi, Laura Gioia, Noreen Kamal, Shannon MacDonald, Katharine Mckeen, Kathryn Yearwood, Leigh Botly, and Laura Holder.
We acknowledge and thank Norine Foley and the evidence analysis team at workHORSE; Shelley Sharp and Trish Helm-Neima for the review of Acute Stroke Management Performance Measures; Adrian Salonga for writing group participation and contributions, Laurie Charest of Heart & Stroke for her coordination of the CSBPR teams and processes; and Francine Forget Marin and the Heart & Stroke internal teams who contributed to the development and publication of these recommendations (Translation, Communications, Knowledge Translation, Engagement, Health Policy, and Digital Solutions).
Heart & Stroke is especially grateful to the members of the Community Consultation and Review Panel who reviewed this module and shared their personal experiences and insights on what made or could have made their journey easier. CCRP members included Ashley Voth, Sarah Blanchard-Eng, Allan Morrison, Patricia Pollock, Heather Purvis, Donna Sharman, Andy Sharman, and Louise Nichol.
Funding
The development of the CSBPR is funded by Heart & Stroke. No funds for the development of these recommendations come from commercial interests, including pharmaceutical and device companies. Writing group members and external reviewers are volunteers who do not receive any remuneration for their participation. All participants complete a conflict of interest declaration prior to participating.
Conflicts of Interest
The following authors have identified actual or potential conflicts of interest which have been mitigated through the design of a multidisciplinary writing group model and additional measures by the advisory committee as required. Michel Shamy holds a CIHR SPOR Grant, New Frontiers in Research Fund Grant, participation on a Data Safety Monitoring Board or Advisory Board for the FRONTIER Trial. Patrice Lindsay is a voluntary member of the March of Dimes After Stroke Advisory Board. Gord Gubitz is Site Investigator for AcT, ESCAPE-NEXT, and ECSC-2. Amy Yu holds a National New Investigator Award from the Heart & Stroke Foundation of Canada. Aravind Ganesh received funding from Canadian Institutes of Health Research and Alberta Innovates (paid directly to the Institution), received research funding from the Canadian Institutes of Health Research, Canadian Cardiovascular Society, Alberta Innovates, Campus Alberta Neuroscience, Sunnybrook Research Institute INOVAIT, Government of Canada – New Frontiers in Research Fund, Microvention, Alzheimer Society of Canada, received consulting fees from MD Analytics, My Medical Panel, Figure 1, CTC Communications Corp, Atheneum, Deep Bench, Research on Mind, Creative Research Designs, received payment or honoraria for lectures, presentations, speakers bureaus, manuscript writing or educational events from Figure 1, Alexion, Biogen, has a patent filed for a system for patient monitoring and delivery of remote ischemic conditioning or other cuff-based therapies, is Member of editorial board of Neurology: Clinical Practice, Neurology, Stroke, Frontiers in Neurology, and holds stock options for SnapDx, Advanced Health Analytics (AHA Health Ltd), TheRounds.com, Collavidence. Sacha Arsenault is a voluntary member of the March of Dimes After Stroke Advisory Board. Devin Harris received research funding from the Canadian Institutes of Health Research and Brain Canada (paid directly to institution), participated on a Data Safety Monitoring Board or Advisory Board for PulsePoint Randomized Controlled Trial (DSMB), and is Council Chair, B.C. Patient Safety and Quality Council. Eric Kaplovitch is an External consultant for the Canadian government through RCGT re: vaccine safety and holds Leadership or fiduciary roles in the Canadian Society of Vascular Medicine (unpaid). Zachary Liederman received an honoraria for presentation at annual Thrombosis Canada conference (warfarin in 2022) as well as creation of patient education pamphlet (cancer associated thrombosis), participated on Advisory board work with SOBI regarding ITP treatment (Avatrombopag), and participated on CanVECTOR Training, Mentoring, & Early Career Development Platform (unpaid). Shauna Martiniuk is a member of the MSH Emergency Associates and received hourly funding for time spent in meetings. Genevieve Milot participated on a Data Safety Monitoring Board or Advisory Board, is a Royal College of Canada council member, and holds a role on the Fellowship affair board. Jeffrey Minuk provides medical expertise for CMPA cases for McCarthy-Tetreault and received payment for expert testimony – McCarthy-Tetreault – written expertise only. Erica Otto is a member of Canadian Society of Hospital Pharmacists (CSHP) and Canadian Pharmacists Association (CPhA), received speaker honoraria from CSHP, received review honoraria from CPhA for reviewing neurology topic chapters, received peer-reviewed salary support grant from the Ontario Heart and Stroke Foundation, and received peer-reviewed grant funding from the Canadian Institutes of Health Research. Jeffrey Perry holds a Heart and Stroke Foundation Mid-Career award (paid to institution). David Volders received a donation from Medtronic Inc for organizing an EVT training day for radiologists from Newfoundland. Eric E. Smith holds research funding from the Canadian Institutes of Health Research, Brain Canada, Weston Brain Institute. Weston Family Foundation (Payments made to University of Calgary) holds a Grant from UpToDate; Royalties/Licenses for Alnylam, Bayer, Biogen, Cyclerion, Javelin, Eli Lilly (topics not related to manuscript), received consulting fees from the US National Institutes of Health, and is an Associate Editor of American Heart Association. Dar Dowlatshahi holds a CIHR grant as co-PI, received consulting fee for advisory board on anticoagulation reversal from Astra Zeneca Canada, honoraria for ICH lecture by the Castle Stroke Course, received travel support for ESCAPE-NEXT investigator meeting at the 5T conference 2022, and holds the position of Vice Chair for the Canadian Stroke Consortium. The following authors have no conflicts of interest to declare: Manraj Heran, Rebecca Lund, Doug Bickford, Donnita Derbyshire, Shannon Doucette, Esseddeeg Ghrooda, Nick Kanya-Forstner, Chelsy Martin, Marie McClelland, Anita Mountain, Rob Schlamp, Donatella Tampieri, Brian van Adel, Ruth Whelan, Samuel Yip, and Norine Foley.
Statement of Authorship
Manraj Heran (First Author) and Michel Shamy (Senior Author) are cochairs of the Acute Stroke Management expert writing group and lead authors contributing to all aspects of the development, data analysis, writing, editing, and final approval of this manuscript; Amy Yu, Aravind Ganesh, Sacha Arsenault, Doug Bickford, Donnita Derbyshire, Shannon Doucett, Esseddeeg Ghrooda, Devin Harris, Nick Kanya-Forstner, Eric Kaplovitch, Zachary Liederman, Shauna Martiniuk, Marie McClelland, Genevieve Milot, Jeffrey Minuk, Erica Otto, Jeffrey Perry, Rob Schlamp, Donatella Tampieri, Brian van Adel, David Volders, Ruth Whelan, and Samuel Yip are all members of the Acute Stroke Management expert writing group and contributed by reviewing, analyzing, and discussing the evidence and collectively finalizing the wording of all included recommendations and contributed to additional supporting content. M. Patrice Lindsay is corresponding author, senior editor of the guidelines and this manuscript, involved in all aspects of scientific literature review, writing group deliberations, external review process, manuscript preparation, and a writer of supplementary documentation. Gord Gubitz, Dar Dowlatshahi, and Michael Hill are senior advisors to this writing group and quality committee and contributed significantly to the methodology and recommendation development and provided review and edits to the overall documents. Eric E. Smith and Anita Mountain are cochairs and senior leaders of the stroke best practices advisory committee and oversee all guideline development and participate in ongoing review and feedback of the content. Norine Foley conducted the evidence searches and completed the evidence tables and evidence summaries supporting this guideline update and contributed to the writing of this manuscript. Rebecca Lund and Chelsy Martin are the Heart and Stroke Foundation stroke best practice project leads and supported the internal and external review process and the final revisions of the guidelines and manuscript and are writers of supplementary documentation.





