1. Introduction
Postpartum depression (PPD) is a common and serious women’s mental health problem that is associated with maternal suffering and numerous negative consequences for offspring. The first six months after childbirth may occur a high-risk time for depression [Reference O’Hara and McCabe1]. According to previous studies, the prevalence of PPD ranged from 0.9% to 25.5% in developed countries, and from 8.2% to 38.2% in developing countries using the screen of the Edinburgh Postnatal Depression Scale (EPDS) [Reference Norhayati, Nik Hazlina, Asrenee and Wan Emilin2]. Estimates of prevalence ranged from 14.3% to 19.3% in China [Reference Gao, Chan, You and Li3, Reference Xie, Liao, Xie, Guo, Walker and Wen4]. PPD has been identified an acknowledged public health problem [Reference Shrivastava, Shrivastava and Ramasamy5].
It could increase the risk for multiple adverse outcomes among themself, their partners, infants and families such as lead to self-negative attitudes, self-harm and even suicidal intention, cause anxiety or depression of partner and even influence the behavioral, cognitive, physical health and social emotional development of their infants and children [Reference O’Hara and McCabe1, Reference Wisner, Sit, McShea, Rizzo, Zoretich and Hughes6–Reference Glavin and Leahy-Warren8]. Until now, the etiology of PPD remains unclear, although several risk factors have been identified [Reference Norhayati, Nik Hazlina, Asrenee and Wan Emilin2, Reference Patel, Bailey, Jabeen, Ali, Barker and Osiezagha9], such as history of depression, lack of social support, cesarean delivery and prenatal smoking and so on [Reference Palumbo, Mirabella and Gigantesco10–Reference Ross and Dennis14]. With the attention of women’s mental health, the influence of violence on mental health has attracted the closely attention of researcher. Violence is increasingly becoming recognized as an important public health problem worldwide [Reference Ludermir, Lewis, Valongueiro, de Araujo and Araya15], which may seriously affect the women’s mental health, lead to anxiety, depression or posttraumatic stress disorder (PTSD) [Reference Dolatian, Hesami, Shams and Majd16, Reference Leung, Kung, Lam, Leung and Ho17]. Previous four systematic reviews and meta-analysis [Reference Wu, Chen and Xu18–Reference Beydoun, Beydoun, Kaufman, Lo and Zonderman21] suggested that maternal violence experiences were significantly associated with the developing of PPD. Of note, these reviews included some case-control studies and cross-sectional studies, which limited the strength and quality of such evidence. Additionally, when exploring the association between violence and PPD, these reviews did insufficient consider the confounding factors and heterogeneity sources, so the risk estimates might be not be precise and robust. Meanwhile, mentioned-above reviews did not given attention to the association between difference types of violence and the risk of PPD.
Furthermore, most of subsequent cohort studies with adequate sample sizes have examined the association in recent years, but the results are inconsistent [Reference Rogathi, Manongi, Mushi, Rasch, Sigalla and Gammeltoft22–Reference Flach, Leese, Heron, Evans, Feder and Sharp32]. If these newer studies could be included in the future meta-analysis, it is bound to increase the statistical power. Moreover, our study will to explore the association between the different types of violence and PPD in the same article. Therefore, given the inconsistency of existing literatures and insufficient evidence of primary studies, further an update meta-analysis based on original cohort studies is evidently required.
2. Methods
2.1. Literature search strategy
We referred to the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) guidelines to conduct this meta-analysis [Reference Moher, Liberati, Tetzlaff and Altman33]. PubMed, Google Scholar, Cochrane Libraries, China Biology Medicine disc, Chinese Scientific Journals Fulltext Database (CQVIP), China National Knowledge Infrastructure (CNKI), and Wanfang Database were searched, with an end date parameter of December 31, 2017, to identify cohort studies assessing maternal violence experiences and risk of PPD. We used and combined the following search terms: “(violence OR abuse OR force OR maltreat OR ill-treat OR tyrannize OR disservice OR negative life event OR adverse event OR traumatic event) AND (postpartum depression OR puerperal depression OR postnatal depression OR depression OR melancholia) AND (cohort study OR prospective study OR follow-up study OR longitudinal study OR incidence study)”. Additionally, we also performed a manual search on the reference lists of retrieved articles and recent reviews.
2.2. Exposure of interest
In the present review, the exposure of interest was maternal violence experiences which were defined as actual violence, including having been slapped, bitten, kicked, hit, beaten, chocked, threatened with a knife or gun, physical and emotional neglect, or had one used against them or forced into sexual activity [Reference Janssen, Heaman, Urquia, O’Campo and Thiessen30, Reference Li, Long, Cao and Cao34]. Maternal violence experiences could be further classified according to the nature, perpetrators and period of violence occurrence. According to the nature of violence, it could be further divided into sexual violence, emotional violence, and physical violence whereas recently of violence is conceptualized as recent (within the past year) or lifetime (incorporates childhood abuse experiences) [Reference Records and Rice35]. Besides, on the basis of perpetrators and period of violence, it could be further divided into domestic violence [Reference Howard, Oram, Galley, Trevillion and Feder19] (i.e. intimate partner violence perpetrated by a current or former partner and/or violence perpetrated by family member) and childhood violence [Reference Malta, McDonald, Hegadoren, Weller and Tough36] (i.e. violence occurred when individuals were younger than 18 years of age), respectively. Because previous studies did not explore the association between the different types of violence and the risk of PPD, our study will attempt to estimate these associations.
2.3. Study selection
We first performed an initial screening of titles or abstracts. A second screening was based on full-text review. Studies were considered eligible if they met the following criteria: (1) had a cohort study design; (2) the exposure of interest was maternal violence experiences; (3) the outcome of interest was PPD; (4) the determination of outcome were based on reliable techniques such as Edinburgh Postnatal Depression Scale (EPDS), Postpartum Depression Screening Scale (PDSS), Beck Depression Inventory (BDI) and so on; (5) reported relative risks (RRs) and odd ratios (ORs), with corresponding 95% confidence intervals (CIs) (or data to calculate them).
2.4. Data extraction and quality assessment
Two independent authors (SMZ and JBQ) extracted data and assessed study quality. Any disagreements were resolved through discussion among the authors until consensus was reached. Data extraction was performed by using a standardized data collection form. Information was recorded as follows: the first author’s name; publication year; geographic region; economic levels (World Bank Income group distribution 2017); study design; number of total samples; assessment method of PPD; PPD assessment time; assessment method of violence; occurrence time of violence (recent vs lifetime); type of violence; reported ORs and their 95%CIs for the risk of PPD associated with maternal violence experiences; whether the confounding factors were adjusted; and quality score.
In our review, we assessed the study quality of included literatures by using the Newcastle-Ottawa Scale (http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp). Using this scale, each study is judged on eight items, categorized into three groups: the selection of the study groups; the comparability of the groups; and the ascertainment of outcome of interest for cohort studies. Stars awarded for each quality item serve as a quick visual assessment. Stars are awarded such that the highest quality studies can be awarded as many as nine stars. When the study gains seven or more stars, it is considered of higher methodological quality.
2.5. Statistical analysis
OR was used as the common measure of association between maternal violence experiences and PPD, and hazard ratios, incidence rate ratios, and RRs were directly considered as OR. The combined ORs and their 95% CIs were calculated using either fixed-effects models or, in the presence of heterogeneity, random-effects models. When multiple outcome of violence was reported in the same study, the effect values of the relationship between different types of violence experiences and the risk of postpartum depression were combined with statistical software (such as Stata version 12.0 and Review Manager version 5.3). Homogeneity of effect size across studies was tested by using the Q statistics (significance level at P < 0.10). The I2 statistic (significance level at I2 > 50%), which is a quantitative measure of inconsistency across studies, was also calculated [Reference Higgins, Thompson, Deeks and Altman37].
Subgroup analyses according to geographic region, economic levels, assessment method of PPD, PPD assessment time, assessment method of violence, occurrence time of violence, whether the confounding factors were adjusted, and quality score were performed, to assess the potential effect modification of these variables on outcomes. We also conducted a sensitivity analysis to investigate the influence of a single study on the overall risk estimate by omitting one study at a time or excluding the low quality studies. Potential publication bias was assessed by Begg's funnel plots and Begg's linear regression test (significance level at P < 0.10) [Reference Egger, Davey, Schneider and Minder38].
All statistical analyses were performed using Stata version 12.0 and Review Manager version 5.3. All reported P values were two-sided and P < 0.05 was considered statistically significant, except where otherwise specified.
3. Results
3.1. Literature search
We initially searched 508 potentially eligible articles from seven databases. Three additional articles were found from reference lists. Most articles (n = 403) were excluded after the first screening based on titles or abstracts because they were duplicates, reviews, or unrelated to our topics. Then, 105 potentially relevant articles were identified, which were carefully assessed by full-text, and 73 articles were further excluded for various reasons. Reasons for not including the other studies were: (i) outcome measures could not be extracted (n = 17); (ii) ineligible study design (n = 29); (iii) outcome lumping PPD and other diseases (n = 15); and (iv) exposed group is inconsistent with our interest (n = 12). Finally, we identified 32 eligible articles [Reference Ludermir, Lewis, Valongueiro, de Araujo and Araya15–Reference Leung, Kung, Lam, Leung and Ho17, Reference Rogathi, Manongi, Mushi, Rasch, Sigalla and Gammeltoft22–Reference Flach, Leese, Heron, Evans, Feder and Sharp32, Reference Li, Long, Cao and Cao34–Reference Malta, McDonald, Hegadoren, Weller and Tough36, Reference Meltzer-Brody, Bledsoe-Mansori, Johnson, Killian, Hamer and Jackson39–Reference Budhathoki, Dahal, Bhusal, Ojha, Pandey and Basnet53] for this meta-analysis (Fig. 1).
3.2. Study characteristics
The characteristics of included literatures, which involved 177,531 participants and were published between 2002 and 2017, were summarized in Table 1. Among the 32 studies, 11 studies (34.4%) were conducted in Asia, 9 (28.1%) in America, 7 (21.9%) in Oceania, 3 (10.3%) in Europe and 2 (6.3%) in Africa. Based on World Bank Income group distribution, 12 studies (37.5%) belonged to middle and low income countries and 20 studies (62.5%) belonged to high income countries.
The Edinburgh Postnatal Depression Scale (EPDS) was the most commonly used assessment instrument of PPD (87.5%), while the Beck Depression Inventory (BDI), the Beck Depression Inventory Fast Screen (BDI-FS), the Patient Health Questionnaire-9 (PHQ-9) and Postpartum Depression Screening Scale (PDSS) only were used in one study respectively. The assessment time of PPD in 20 studies (62.5%) was conducted within 2 months of postpartum. Eight studies (25%) used administered questionnaire to assess maternal violence experiences, 12 studies (37.5%) used standardized/structured questionnaire or interview and 12 studies (37.5%) used the violence assessment scale. Meanwhile, according to violence assessment of period, more than half of studies (53.1%) of violence experiences occurred in recent and other studies (46.9%) of violence experiences occurred in lifetime.
Additionally, 19 studies (59.4%) adjusted some potential confounding factors (such as age, education, parity, social support, history of depression, depression during pregnancy and so on), and the remaining studies did not adjusted any factors when estimating the effect. Twenty-nine studies (90.6%) were considered of higher methodological quality, achieving a quality score ≥7 out of 9; these 29 studies contributed most of study participants. Physical violence experiences in 8 studies were reported, emotional violence experiences in 8 studies, sexual violence experiences in 6 studies, domestic violence experiences in 16 studies, and childhood violence experiences in 5 studies.
3.3. Quantitative synthesis
Fig. 2 shows the results from random-effect models combing the ORs between maternal violence experiences and risk of developing PPD. Overall, women who experienced any violence events compared with those who did not experience any violence events, were at a higher risk of developing PPD (OR = 2.04; 95%CI: 1.72–2.41). However, substantial heterogeneity was found (P = 0.000; I2 = 93.7%).

Fig. 1. Flow chart of literature selection.
Table 1 Characteristics of included studies for the association between violence and risk of PPD.
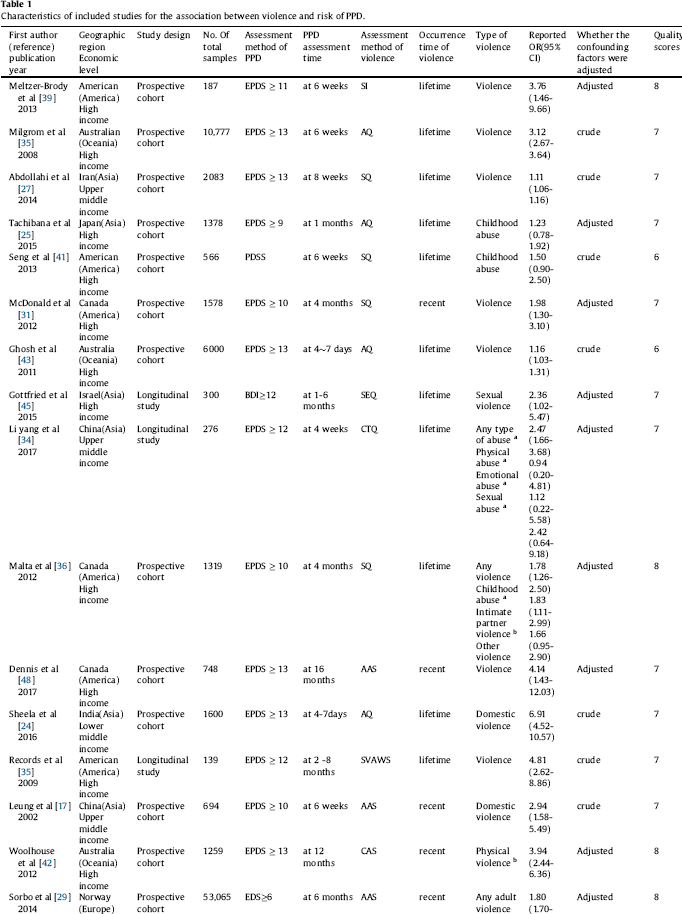


Fig. 3 presents the results of pooled estimates between sexual, psychological and physical violence experiences and risk of developing PPD. Overall, the risk of developing PPD was significantly increased in women who experienced sexual (OR = 1.56; 95%CI: 1.35–1.81), emotional (OR = 1.75; 95%CI: 1.61–1.89) and physical (OR = 1.90; 95%CI: 1.36–2.67) violence events. Nevertheless, there was substantial heterogeneity except for sexual violence experiences (P = 0.303; I2 = 17.1%).
Fig. 4 displays the results of pooled estimates between domestic and childhood violence experiences and risk of developing PPD. Overall, women experiencing domestic violence events (OR = 2.05; 95%CI: 1.50–2.80) or childhood violence events (OR = 1.59; 95%CI: 1.34–1.88) had a significantly higher risk of developing PPD, when compared with those without any violence events. Yet, the evidence heterogeneity was observed for domestic violence experiences (P = 0.000; I2 = 85.4%).
3.4. Subgroup analyses
Subgroup analyses for the association between any violence experiences and risk of developing PPD were summarized in Table 2. Overall, a significantly increased risk of developing PPD was found in most of subgroups. After subgroup analyses, whether the confounding factors were adjusted (test for subgroup differences [TSD]: I2 = 65.6%), assessment method of PPD (TSD: I2 = 57.8%), economic levels (TSD: I2 = 42.9%) quality score (TSD: I2 = 20.7%), and geographic region (TSD: I2 = 19.0%) were identified as the first five of the most relevant heterogeneity moderators. However, the risk of developing PPD was not statistically different across above-mentioned subgroup variables (TSD: all P ≥ 0.09).
3.5. Sensitivity analyses
Sensitivity analyses were conducted to explore potential sources of heterogeneity in the association between maternal violence experiences and PPD, and to examine the influence of various exclusion criteria on the overall risk estimates. Exclusion of 3 studies that were considered of low methodological quality yielded similar results (OR = 2.11; 95%CI: 1.75–2.54), with substantial evidence of heterogeneity (P <0.00001; I2 = 94.0%). Further exclusion of 13 studies in which the confounding factors were not adjusted when assessing the risk of developing PPD associated with maternal violence experiences also yielded similar results (OR = 1.79; 95%CI: 1.52–2.11), yet heterogeneity was still present (P <0.00001; I2 = 72.0%). Additionally, exclusion of any single study at a time did not materially alter the overall pooled estimates (Fig. 5).

Fig. 2. Forest plot for maternal violence experiences and risk of PPD.
3.6. Publication bias
The Begg’s funnel plot did show a little substantial asymmetry (Fig. 6), but the Begg’s rank correlation test did not indicate the evidence of publication bias across studies of maternal violence experiences and risk of developing PPD (P = 0.709).
4. Discussion
PPD is an important part of the spectrum of mood disturbances affecting postpartum women, which can predispose to chronic or recurrent depression, and may affect the mother-infant relationship and child growth and development. Previous studies found that approximately half of new mothers may experience depressive symptoms at some point during the first year birth [Reference Dennis, Merry and Gagnon48].
Our meta-analysis yielded following main findings. First, overall, maternal violence experiences were significantly associated with an increased risk of developing PPD (OR = 2.04); second, different types of violence events such as sexual violence (OR = 1.56), emotional violence (OR = 1.75), physical violence (OR = 1.90), domestic violence (OR = 2.05) or childhood violence (OR = 1.59) were also significantly associated with higher risks of developing PPD; and third, the association between maternal violence experiences and higher risks of developing PPD still existed after subgroup and sensitivity analyses, which indicated our results were stable and credible.
Until now, there are four existing reviews [Reference Wu, Chen and Xu18–Reference Beydoun, Beydoun, Kaufman, Lo and Zonderman21] that evaluated the association of maternal violence experiences with PPD. Our findings are generally consistent with previous reviews. However, our study has important strengths. Our review is the most up to date on this subject. With the accumulating evidence and enlarged sample size, we have enhanced statistical power to provide more precise and reliable risk estimates. In our study, more than half of studies had a large sample size (>1000); nearly 90% of studies were considered of higher methodological quality; and these high-quality studies contributed most of study participants. All included original studies used a cohort study design, which minimizes recall and selection biases. Moreover, compared with previous four meta-analyses, we fully considered the effect of geographic region, economic levels, assessment method of PPD, PPD assessment time, assessment method of violence, occurrence time of violence, whether the confounding factors were adjusted, and quality score. We found that the association between maternal violence experiences and risk of developing PPD persists and remains statistically significant after subgroup and sensitivity analyses. The most relevant heterogeneity moderators have been identified by subgroup analyses. Besides, our study indicated different types of violence experiences such as such as sexual, emotional and physical violence, or domestic or childhood violence, were significantly associated with PPD, which did not be confirmed by previous reviews.
To our knowledge, the underlying mechanisms involved in the association between violence and PPD are unclear. The most probable explanation is stress-related neuroendocrine dysfunctions. Evidence shows that the neuroendocrine channel comprising hypothalamic pituitary adrenal (HPA) axis responds to stress by hormonal secretion. The level a person experiences stress is directly related to the intensity of neuroendocrine response that promote the hormones secretion. Violence is a type of stress. When women experienced various forms of violence events in childhood, adolescence and adulthood, these adverse events could lead to a higher level of stress and activate the axis [Reference O’Hara and McCabe1, Reference Dolatian, Hesami, Shams and Majd16, Reference Records and Rice35, Reference Brummelte and Galea54, Reference Meltzer-Brody55].

Fig. 3. Forest plot for sexual, psychological and physical violence experiences and risk of PPD.
Additionally, there are a few possible explanations for the association between maternal violence experiences and risk of PPD. On the one hand, the association between violence and the risk of PPD may be influenced by cultural, social and behavior aspects of violence. Evidence indicates that violated women may be unwilling to disclose their violence experience because of the effect of self-concept, self-confidence, dignity, competence and even social stigma. Therefore, the expression of depression symptoms may be a reaction to violence and an indirect request for help. In addition, it is widely believed that violence is private matter and should be kept secret, which hinder women to seek for heal and lead to continuation of their problems [Reference Dolatian, Hesami, Shams and Majd16, Reference Records and Rice35, Reference Varma, Chandra, Thomas and Carey56]. On the other hand, they thought that who experienced violence events may lead to psychological trauma and psychological sensitivity, which brings about an increased risk of developing PPD [Reference Leung, Kung, Lam, Leung and Ho17]. In a word, the uncertainty of underlying mechanisms between violence and PPD warrants further research.
Substantial heterogeneity was observed among studies assessing the association of maternal violence experiences with risks of PPD, which was not surprising given the differences in study population and methodology. In our review, subgroup analyses were used to explore heterogeneity sources. Our subgroup analyses have identified main heterogeneity moderators, including whether the confounding factors were adjusted (TSD: I2 = 65.6%), assessment method of PPD (TSD: I2 = 57.8%), economic levels (TSD: I2 = 42.9%), quality score (TSD: I2 = 20.7%), and geographic region (TSD: I2 = 19.0%). However, there were not statistically significantly differences for risks of developing PPD across above-mentioned subgroups, which indicated the reasons leading to heterogeneity among studies may be more perplexing.
Potential limitations of this study should be considered. Firstly, there were some differences for measure methods of exposures and outcomes between studies, which may increase the likelihood of misclassification bias and measurement bias, thereby over- or underestimating the strength of the association. For example, in the present study, for the measure of PPD, nearly 87% of included studies used EPDS, while the remaining studies used other tools. Meanwhile, for the assessment of violence, most of included studies used standardized violence scale and questionnaires to collect the information of maternal violence experiences, while eight studies did not. In particular, when we collect the information of childhood abuse based on recollection of experiences of violence, recall bias was inevitable. Therefore, it is difficult for us to commit to the complete elimination of misclassification bias and measurement bias. But evidence indicated that the memories of violence experiences remain fairly accurate over a long period [Reference Zou and Andersen57]. In addition, the assessment time of PPD and the occurrence time of violence were also different between studies. So it is difficult to precise classify because of the limitation of original data.
Secondly, the substantial heterogeneity among studies for the association between maternal violence experiences and risk of developing PPD were observed. Nevertheless, we were able to detect the major source of heterogeneity through subgroup and sensitivity analyses. The sensitivity analysis that omitted one study at a time and calculated the combined OR for the remaining studies yielded consistent results. After subgroup analysis, the heterogeneity was obviously decreased. However, our estimates have to be viewed with caution because of heterogeneity.

Fig. 4. Forest plot for domestic and childhood violence experiences and risk of PPD.
Table 2 Subgroup analysis of association between violence and the postpartum depression.
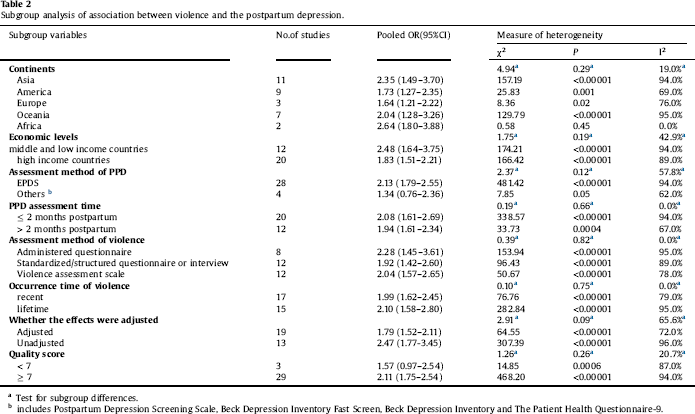
a Test for subgroup differences.
b includes Postpartum Depression Screening Scale, Beck Depression Inventory Fast Screen, Beck Depression Inventory and The Patient Health Questionnaire-9.

Fig. 5. Sensitivity analyses by excluding any single study at a time for maternal violence experiences and risk of PPD.

Fig. 6. Begg’s funnel plot for maternal violence experiences and risk of PPD.
Thirdly, due to limited number of included studies on specific subtypes of violence, we did not perform a subgroup or sensitivity analysis for the association of specific violence events with PPD, so more studies should be included in future reviews, to provide further support for our results. Fourthly, residual confounding is of concern. Uncontrolled or unmeasured risk factors (such as responsibilities of perpetrators, laws, social condition, and the implications for health services or public health) potentially produce biases. Especially, cultural factors also are an important risk to the developing of PPD. Cultural diversity may vary between countries. However, we did not assess the influence of cultural factors on our outcome because the limitation of original data. Although restricting analysis to studies that controlled conventional risk factors of PPD did not materially alter the combined risk estimates, we still cannot eliminate the possibility that residual confounding could affect the results because these factors do not explain all of the risk of PPD. Additionally, although the Begg’s rank correlation test did not indicate the evidence of publication bias, Begg’s funnel plot did show a little substantial asymmetry, which may influence the results. Finally, because our review only included studies published in Chinese or English, additional research in other populations is warranted to generalize the findings.
In conclusion, our study, which includes a large proportion of participants, with sufficient statistical power, aimed at providing an updated evidence to identify the risk of PPD associated with maternal violence experiences by conducting a meta-analysis of cohort studies. Although the role of potential bias and evidence of heterogeneity should be carefully evaluated, the present study indicated that women who experienced any violence events compared with those without experiencing any violence events, had a higher risk of developing PPD. Furthermore, it should be noted that specific subtypes of violence events such as sexual, emotional and physical violence, and domestic and childhood violence, were also associated with an increased risk of developing PPD.
Therefore, a comprehensive law against violence should be enacted, popularized and implemented in different counties. Improving the social and economic status of women, combating gender discrimination, and providing legal, medical as well as psychological services for violated women are very necessary to reduce violence and its outcomes. Meanwhile, early postpartum depression screening also plays an important role in preventing postpartum depression. In addition, the mechanisms involved in the association between violence and PPD are unclear and require further study for elucidation.
Disclosure of interests
The authors declare that they have no conflicts of interest.
Details of ethics approval
Not required.
Funding
JBQ was supported by the Project Funded by Natural Science Foundation of Hunan Province (2018JJ2551), National Natural Science Foundation Program of China (81803313), Hunan Provincial Key Research and Development Program (2018SK2063).
Acknowledgments
The authors would like to thank the editors and reviewers for their suggestions.













Comments
No Comments have been published for this article.