Prior studies have shown that catheter-associated urinary tract infections (CAUTIs) are common and that they prolong hospital stays and increase overall healthcare costs.Reference Scott 1 , Reference Yi, Baggs, Gould, Scott and Jernigan 2 The importance of this issue is reflected in the mandate to publicly report CAUTI rates to National Health and Safety Network (NHSN) to participate in the Centers for Medicaid and Medicare Services payment system and the inclusion of intensive care unit (ICU) CAUTI rates in an institution’s value-based purchasing score.
In contradistinction, there is increasing recognition that most positive urine cultures in patients with a bladder catheter are asymptomatic and should not be treated.Reference Tambyah and Maki 3 – Reference Cope, Cevallos, Cadle, Darouiche, Musher and Trautner 5 The American College of Critical Care Medicine (ACCCM) and the Infectious Diseases Society of America (IDSA) note that catheter-associated bacteriuria is typically indicative of colonization, is rarely symptomatic, and is an infrequent cause of fever or secondary bloodstream infection. Their joint guidance recommends that when evaluating fever in the critically ill, urine cultures should only be evaluated in patient populations at high risk of invasive infection: (1) those who are kidney transplantation recipients, (2) those who are neutropenic, (3) those who have recently had genitourinary surgery, and (4) those who demonstrate evidence of obstruction.Reference O’Grady, Barie and Bartlett 6
In this report, we describe efforts to decrease CAUTIs by combining best practices for bladder catheter use with guidance-based “stewardship of culturing.”
METHODS
A team representing all intensive care unit (ICU) disciplines (ie, pediatric, medical, surgical, neurologic, cardiac, heart failure, and cardiothoracic surgery) and infection prevention (IP) was assembled in 2013 to address the institutional goal of reducing CAUTI rates. Interventions implemented in 2013 included the following: (1)an assessment of competency with catheter insertion and maintenance, (2) maintaining a closed system, (3) initiation of a nursing driven protocol for catheter removal, (4) improved fidelity of electronic documentation of catheters, (5) implementation of preservative tubes for specimen collection, and (6) periodic maintenance audits of catheters.
In 2014, consensus was obtained through discussions at a standing monthly ICU operations meeting to consider recommended guidance for evaluating a new fever in the critically ill.Reference O’Grady, Barie and Bartlett 6 This approach was adopted by all ICU disciplines over the course of the intervention period. Decisions regarding the use of urinalysis and changing catheters remained at the discretion of each division. Autonomous approaches to adopting culturing guidelines were accepted.
The described observation period was January 1, 2013, through December 31, 2014. Data were compiled from all ICUs and comprised 215 adult and 25 pediatric ICU beds of a 1,268-bed tertiary-care academic medical center. Surveillance for CAUTI and hospital-acquired bloodstream infection (HABSI) according to the NHSN definition was conducted routinely, and results were prospectively recorded in an IP database. 7 Patient days were obtained from an administrative source and device days were counted manually according to NHSN guidelines. Rates of CAUTI, HABSI, and HABSI due to Enterobacteriaceae species were calculated and compared. Device utilization ratios (DURs) were calculated. Urine culture orders were tracked by service. All analyses were performed using Open Source Epidemiologic Statistics for Public Health via JAVA software. The χ2 test was used to evaluate differences between rates.
RESULTS
There were 11,117 ICU admissions in 2013, resulting in 74,705 patient days; there were 11,589 admissions in 2014, resulting in 75,569 patient days. The DURs were 0.7 in 2013 and 0.68 in 2014. The number of urine specimens cultured decreased from 4,749 in 2013 to 2,479 in 2014. The CAUTI rate decreased from 3.0 per 1,000 catheter days in 2013 to 1.9 in 2014 (P=.0003; rate ratio, 0.6291; 95% confidence interval [CI], 0.49–0.81) (Figure 1). Table 1 provides the specific per-unit breakdown of the numbers of urine cultures and CAUTI rates over the preintervention and intervention periods. The HABSI rates per 1,000 patient days decreased from 2.8 in 2013 to 2.4 in 2014 (P=.15). The rates of HABSI secondary to Enterobacteriaceae per 1,000 patient days decreased from 0.71 in 2013 to 0.66 in 2014 (P=.72; rate ratio, 1.1; 95% CI, 0.73–1.60).
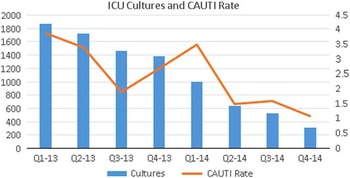
FIGURE 1 Catheter-associated urinary tract infection (CAUTI) rate (by quarter) during the pre-intervention period (2013) and intervention period (2014) associated with number of urine cultures collected.
TABLE 1 Number of Cultures and CAUTI Rates per 1,000 Urinary Catheter Days in Each Intensive Care Unit (by Quarter) in the Preintervention Period (2013) Versus the Postintervention Period (2014)
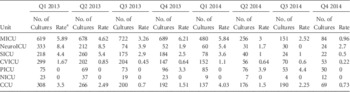
NOTE. MICU, medical intensive care unit; NeuroICU, neurological intensive care unit; SICU, surgical intensive care unit; CVICU, cardiovascular intensive care unit; PICU, pediatric intensive care unit; NICU, neonatal intensive care unit; CCU, cardiac care unit.
a Rate per 1,000 catheter days.
DISCUSSION
In this report, we describe a multifaceted intervention to decrease CAUTIs. Our approach began with attention to best practice for insertion, maintenance, and removal of Foley catheters. Subsequently, we emphasized “stewardship of testing” by following published guidance for evaluation of a fever prior to ordering a urine culture in a critically ill patient. The culmination of these efforts was a significant reduction in CAUTIs.
Beyond recommending against screening for asymptomatic bacteriuria, there is no mention of testing in published guidance for CAUTI prevention.Reference Lo, Nicolle and Coffin 8 Other reports have provided examples of “postculture” interventions, including withholding results of low-colony-count urine cultures or restricting release of positive results unless specifically requested from microbiology.Reference Leis, Rebick and Daneman 9 , Reference Kwon, Fausone, Du, Robicsek and Peterson 10 Our approach focuses on the decision to test, a “preculture” strategy of applying stewardship to diagnostics.
The CAUTI event is an artificial construct designed to reflect clinical events for surveillance purposes. However, this metric cannot distinguish a true signal (ie, a symptomatic infection) from “noise” (ie, an asymptomatic culture) because it is based on a culture from a nonsterile site. By including the decision to test in our prevention efforts, we sought to fully clarify this metric by decreasing the associated noise. This procedure had an immediately tangible effect of decreasing our CAUTI rate by 33%. No increase in overall HABSI or HABSI was attributed to Enterobacteraciae, making it unlikely that bacteremic urinary tract infections went unrecognized.
Consideration of testing also reinforced best bedside practice. Inherently, parsimony of culturing can only be clinically successful in the setting of continuous adherence to established guidance on device management. Best practice necessitates that appropriate insertion, maintenance, and removal of catheters is the rule rather than the exception. In addition, the results of this study indicate the limited utility of a hospital-onset, positive urine culture in an ICU patient. Future studies could investigate whether stewardship of testing in the ICU has downstream benefits on antibiotics use, the development of resistance, and/or resource utilization throughout the remainder of a patient’s hospital stay.
This report has several limitations. First, it includes interventions at a single institution with a high complexity of care, which potentially limits the generalizability of the results. Also, aggregate data collected from the ICUs were evaluated rather than patient-level data. Finally, the approach to culturing was a recommendation and did not mandate the start of the postintervention period. This is reflected in the gradual as opposed to steep decline in both of the number of cultures sent and CAUTI over the duration of the postintervention year.
Campaigns to reduce HAIs such as CAUTIs are often undertaken as IP efforts divorced from everyday clinical care and other safety initiatives. This initiative ensured appropriate clinical care utilizing established best practice while implementing a stewardship of resources model. This combination allows for clarification of a currently problematically defined but necessarily monitored patient quality and safety event. Going forward, the most effective quality initiatives will link best practice at the bedside with optimal stewardship of all resources including testing, imaging, and medication use.
ACKNOWLEDGMENTS
Financial support: No financial support was provided relevant to this article.
Potential conflicts of interest: All authors report no conflicts of interest relevant to this article.






