The dehumanising sexual violence against women in Bosnia, Ruanda or against those facing Islamic State of Iraq and Syria (ISIS) terror in Iraq and Syria has shown us how cruelly humans can treat their fellow humans.Reference Kizilhan and Noll-Hussong1–Reference Schaal and Elbert3 As a result, victims and the collective they belong to can be traumatised for decades.Reference Schaal and Elbert3 This violence can take the form of coercion, human trafficking, mutilation, rape, slavery and murder.Reference Kizilhan4 Rape is an extreme attack on the intimate self; it triggers massive feelings of humiliation, abasement and shame.Reference Fontenelle, Cocchi, Harrison, Shavitt, do Rosario and Ferrao5
Studies related to sexual violence against women who have survived war situations have identified a number of mental disorders, such as anxiety, depressive and addictive disorders, post-traumatic stress disorder (PTSD), and suicide attempts.Reference Pagotto, Mendlowicz, Coutinho, Figueira, Luz and Araujo6–Reference Darves-Bornoz10 Frequently, the clinical characteristics of a sexual traumatisation only come to light during the course of psychological treatments.Reference Kizilhan and Noll-Hussong11,Reference Gerdau, Kizilhan and Noll-Hussong12 This is often because those affected tend to conceal their traumata because of shame and feelings of guilt, but also out of fear of being ostracised by their native community.Reference Kizilhan13,Reference Budden14 Among individuals who have experienced trauma with body contact, especially in the area of sexual violence, shame plays a particular role in the development of peritraumatic or post-traumatic symptoms,Reference Dorahy and Clearwater15–Reference Dyer, Dorahy, Hamilton, Corry, Shannon and MacSherry17 and is linked to prolonged clinical problems.Reference Herman, Dearing and Tangney18
Emphasising the central affective role of shame,Reference Talbot, Talbot and Tu19 it has been suggested that PTSD, which often results from repetitive victimisation, especially sexual violence, can be conceptualised as both trauma disorder and shame disorder. It has been demonstrated that individuals feel fear when being threatened with violence or even when experiencing violence. Moreover, individuals feel shame when experiencing social isolation or boundary violation, or when being degraded by fellow human beings.Reference Talbot, Talbot and Tu19 Such a degradation of one's own person can lead to feelings of humiliation and rejection by the community.Reference Kim, Talbot and Cicchetti20
Shame and dissociative seizures
Shame by its nature is a relational affect, as it is intimately linked to how an individual perceives themselves, using the real or imagined perspective of internal or external others as a reference point.Reference De Hooge, Zeelenberg and Breugelmans21,Reference Harder, Lewis, Spielberger and Butcher22 On the basis of the social function of shame and its maintenance, this can amplify severe PTSD symptoms and can negatively influence the development of familial and social relationships.Reference Kluft, Vermetten, Dorahy and Spiegel23 Against this background, Yazidi women experience ostracism when having any intimate contact with non-Yazidi – even coerced sexual contact – because, according to their religion, any sexual contact with non-Yazidi is synonymous with an action of exclusion from the Yazidi community.Reference Budden14,Reference Hoffman, Grossman, Shrira, Kedar, Ben-Ezra and Dinnayi24
Local reports have emphasised that dissociative seizures (ICD-10 code F44.5)Reference Wolf, Seiffer, Hautzinger, Othman and Kizilhan25,26 and PTSD (ICD-10 code F43.1) are widespread among female Yazidi who experienced sexual violence in ISIS captivity and are now residing in refugee camps.Reference Wolf, Seiffer, Hautzinger, Othman and Kizilhan25 To the best of our knowledge, there has not been any study examining the potential connection between mentioned violent experiences, shame, post-traumatic symptoms and dissociative convulsions among Yazidi women in a post-ISIS captivity context.Reference Dyer, Dorahy, Hamilton, Corry, Shannon and MacSherry17 The aim of this study is to examine a potential role of dissociation in the overall characteristics of post-traumatic psychopathology. For this purpose, we compared female patients with PTSD who were raped and held hostage by ISIS with those suffering from PTSD who did not experience rape and captivity.
Method
Ethical considerations
The Institute of Psychotherapy and Psychotraumatology at the University of Duhok in Iraq organised and implemented the examination, obtaining permission from the University Ethical Review Board and following ethical principles stated in the Declaration of Helsinki. We confirm that all the research meets the ethical guidelines, including adherence to the legal requirements of the country in the study. Written, informed consent was obtained from the patients for publication of this manuscript and any accompanying information or images.
Participants
The age of the women in the investigation group ranged from 18 to 34 years (n = 64, mean 25.61, s.d. 2.61). The women came from the area of Sinjar in Northern Iraq. They were held captive by ISIS in Iraq and Syria for at least 1 year between August 2014 and September 2018. While being held captive, they repeatedly experienced different forms of sexual violence, such as rape. The control group ranged from 18 to 36 years (n = 60, mean 26.24, s.d. 2.46) and met the following criteria: they were Yazidi women who came from the same region and were living in the same refugee camps. However, they were neither held captive by ISIS nor were they raped. At the time of the investigation, all participants were residing in refugee camps in Northern Iraq.
The first author contacted both the investigation group and the control group, communicating with licensed physicians and psychologists in the refugee camps that they knew from earlier joint projects. Before data were collected, a first visit to the participants was made, which pursued the following goals: the participants were given a description of the study and were informed about its purpose, to obtain informed consent. Moreover, they were informed about how the anonymised data was going to be used.
All participants were examined by a licensed physician from the refugee camps within the 3 days before the interview. There were not any clinically relevant medical records or findings. The data collection was carried out by professional psychologists trained by J.I.K. from 15 October 2018 to 20 May 2019; continuous supervision was provided by J.I.K. Each examination lasted approximately 1.5 hours on average.
Measures
In addition to measures mentioned below we used self-report tools to collect demographic data. Moreover, we incorporated questions that allowed us to obtain information about the kind and extent of support the Yazidi women received at any point during the 4 years after their liberation from ISIS, e.g., ‘Who provided help?’ or ‘Did others help in emotional, social or material terms?’
The Structured Clinical Interview (SCID) for the DSM-IVRReference First, Spitzer, Gibbon and Williams27 is a widely used, semi-structured interview intended to determine whether an individual meets criteria for any DSM-IV disorder.28
The Event Scale by Horowitz et al Reference Horowitz, Wilner and Alvarez29 is a 15-item scale designed to assess the nature and extent of exposure to various war events.Reference Dyregrov, Gupta, Gjestad and Mukanoheli30 Thus, the answers indicate whether an event occurred before, during or after captivity (multiple answers possible), and whether the respondent witnessed the event or experienced it personally.
The 22-item PTSD standardized instrumentReference Øktedalen, Hagtvet, Hoffart, Langkaas and Smucker31 is based on DSM-IV criteria.28 Frequencies of PTSD standardized instrument item responses were determined, and the prevalence of probable PTSD was calculated according to a cut-off score of 50 (diagnostic efficiency 0.91, sensitivity 0.73, specificity 0.88).
The Multiscale Dissociation Inventory (MDI) is a 30-item scale measuring a range of dissociative symptoms on six subscales: (a) disengagement: cognitive and/or emotional detachment from the immediate situation and stimuli; (b) depersonalisation: feeling separated from or alien to one's own body or self; (c) derealisation: feeling as if the environment and the stimuli within it are unreal or dream-like; (d) emotional constriction: a marked reduction in awareness and experience of emotions (positive or negative); (e) memory disturbance: experiencing memory lapses (without specific known organic causes) and (f) identity dissociation: unstable identity states, experiencing more than one ‘self’.Reference Brière32 Scores on each subscale range from 5 to 21. Raw scores are converted to t scores. For subscales a–f, t scores >80 are considered clinically significant. For subscale f, a t score >95 suggests clinical relevance; Cronbach alpha ranges from 0.77 to 0.92.
The Somatoform Dissociation Questionnaire by Nijenhuis et al Reference Nijenhuis, Spinhoven, van Dyck, van der Hart and Vanderlinden33 is a 20-item self-report instrument that evaluates the severity of somatoform dissociations. The assessment has satisfactory internal consistency (Cronbach alpha = 0.94, test-retest coefficient r = 0.95)
The Trauma-Related Shame InventoryReference Øktedalen, Hagtvet, Hoffart, Langkaas and Smucker31 is a 24-item questionnaire that assesses shame-related to sexual trauma across items of internal and external shame and condemnation and affective behavioural facets. Responses are rated on a 4-point Likert scale ranging from 0 (not true of me) to 3 (completely true of me), and the total scale score ranges from 0–72. The measurement demonstrated high reliability as the G-coefficient was 0.87 and the index of dependability was 0.87, with self-judgement correlations of r = 0.52 (P < 0.001), suggesting adequate convergent validity.Reference Goldstein, Drew, Mellers, Mitchell-O'Malley and Oakley34 In this study, the TRSI demonstrated an internal consistency of alpha = 0.97.
All questionnaires were used according to DSM-V, translated in Kurdish and translated back into English, reviewed, analysed and corrected. Maintenance of the original meaning was evaluated by four assessors. Questionnaires in Kurdish were read by female interviewers who were trained by the research team.
Statistical analyses
Statistical analyses were performed using SPSS for Windows, version 22.0, and SAS for Windows, version 17. The values of the clinical diagnostic tests were analysed, using the total and scale values described in the respective manuals. The comparison of all other procedures was based on the raw values of the investigations.
The data distribution was evaluated with non-parametric statistical methods. The multiple comparisons of the groups were undertaken by means of the Mann–Whitney U test, considering the statistical significance adjusted according to Bonferroni.Reference Fontenelle, Cocchi, Harrison, Shavitt, do Rosario and Ferrao5 A P-value of <0.05 was considered statistically significant.
Results
Psychological disorders
All participants were initially diagnosed with PTSD according to DSM-V criteria. With regards to the severity of the PTSD symptoms there were no significant differences between the two groups.
On diagnostic examination by trained physicians and psychotherapists, the highest comorbidity was detected in the investigation group in the affective disorders (75%, χ2 = 1.75, P < 0.42), followed by anxiety disorders (62.5%, χ2 = 1.45, P < 0.44) and somatisation disorder (38.7%, P < 0.02). In addition, eating disorders (9.7%, χ2 = 0.42, P < 0.45) and personality disorders (22.5%, χ2 = 0.76, P < 0.53) were also diagnosed in the investigation group. Dissociation disorders were detected among the investigation group (40.6%, χ2 = 0.18, P < 0.36), and among the survivors who were not in captivity (19.4%). Dissociative seizures were found in 43.7% (P < 0.02) of survivors who were held captive and raped by ISIS (Table 1).
Table 1 Comorbidity among patients with post-traumatic stress disorder (PTSD) overall and with regard to dissociative disorder status
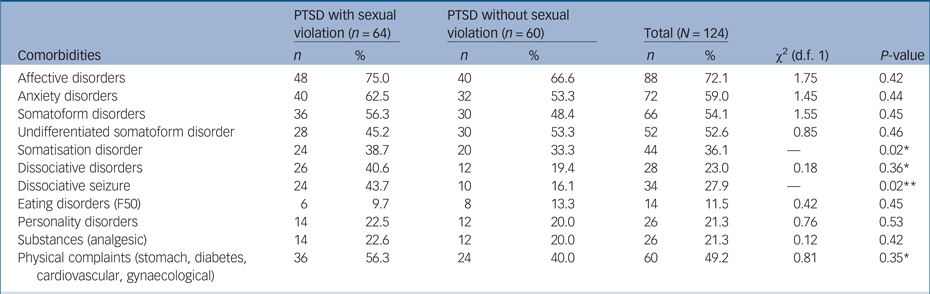
* P < 0.05, **P < 0.01.
Dissociation disorder
The difference in age was significant (t = 1.35, d.f. 120, P > 0.002). There was a correlation between younger age and dissociative seizure (mean 19.9 years, s.d. 8.7), whereas older participants did not suffer from such convulsions (mean 26.5 years, s.d. 11.7). More importantly, symptoms of a major depression and panic disorder were only found among individuals who had suffered from dissociative seizure, whereas those without seizures did not display correlated symptoms. Moreover, there was evidence for a connection between somatoform disorders and dissociative disorders: the objective evaluation using the SCID revealed that the symptoms that displayed the highest mean score were depersonalisation and derealisation (Table 2).
Table 2 Clinician- and self-rated dissociation among female survivors of Islamic State of Iraq and Syria captivity
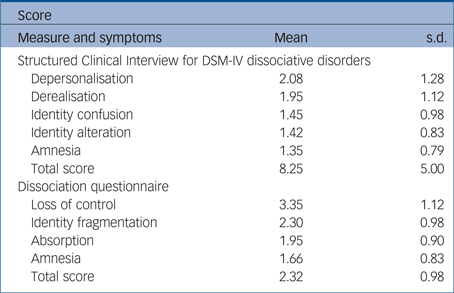
In terms of self-rated symptoms, loss of control displayed the highest score. Participants with dissociative seizures endorsed somatoform disorders as well as shame criteria. Concurrently, they displayed SCID diagnoses more frequently than patients with PTSD who were not raped (Table 3).
Table 3 Psychiatric comorbidity among patients with post-traumatic stress disorder (PTSD) overall and with regards to somatoform disorder and shame
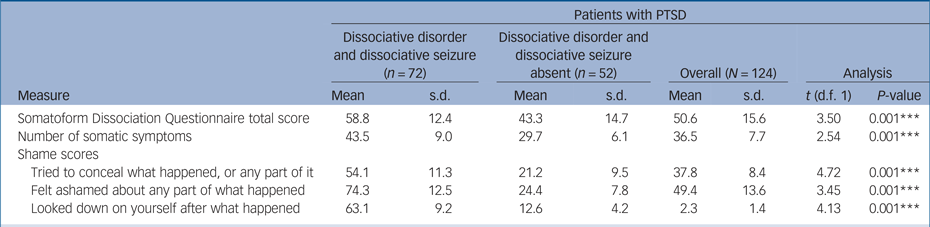
* P < 0.05, **P < 0.01, ***P < 0.001.
Fourteen (22.5%) patients were diagnosed with borderline personality disorder. PTSD participants who were held captive frequently showed striking self-destructive behaviour and continued to report flashbacks, intrusion and avoidance after captivity, and sexual abuse or rape. Speaking about the time when they were held captive, patients with dissociative disorders reported symptoms of a sleeping disorder as well as suicide ideations. Moreover, they said that they had been reminded of physical neglect and sexual abuse (rape) when being held captive. Data (Table 4) has confirmed their reports. With the exception of a high total captivity trauma score, considerably high scores for all sorts of abuse and neglect were also displayed by all of these women.
Table 4 Post-traumatic stress disorder (PTSD) related shame among patients with PTSD overall and by dissociative disorder status
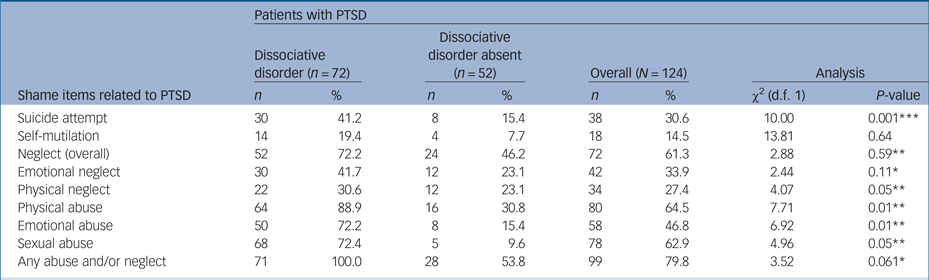
* P < 0.05, **P < 0.01, ***P < 0.001.
Patients who suffered from PTSD but did not suffer from dissociative seizures were more likely to reduce their post-traumatic experience from the time they were held captive and from the time they were fleeing from ISIS. The analysis was conducted with MDI score as the criterion variable and PTSD derived from the TRSI as predictor variables. Sexual abuse (rape) (72.4%, χ2 = 4.96, P < 0.05), emotional abuse 72.2%, χ2 = 6.92, P < 0.01) and suicide attempt (41.2%, χ2 = 10.0, P < 0.001) had a statistically significant effect on dissociation scores.
Discussion
This study primary aimed at measuring shame, somatoform disorders and seizure symptoms reported by women diagnosed with PTSD after they had been held captive by ISIS. These victims were compared with women who had not been held captive and sexually abused by ISIS. Additionally, connections between these factors and the currently reported dissociative symptoms were explored.
Participants who were held captive and sexually abused by ISIS and suffered from PTSD display a high prevalence in affective (75%), anxiety (62.5%), somatoform (56.3%) and dissociation disorders (50.6%), especially dissociative seizures (43.7%).
Despite the fact that individuals examined in this study endorsed dissociation questionnaire scores (mean 2.6) and somatoform scores (mean 58.8) close to that of dissociative disorder patients with PTSD in other studies,Reference Pic, Mellers and Goldstein35,Reference Simeon, Guralnik, Schmeidler, Sirof and Knutelska36 this study has indicated a significant connection between somatoform disorder, shame and dissociative seizure among traumatised raped women, using a variety of validated diagnostic instruments, under the conditions of a refugee camp.
In contrast to earlier epidemiologic examinations,Reference Pic, Mellers and Goldstein35,Reference Baslet37,Reference Hendrickson, Popescu, Ghearing and Bagic38 this study is characterised by high rates of recounted physical (88.9%) and sexual (72.4%) violence. In contrast to individuals who do not suffer from dissociative disorders or dissociative seizures, individuals who do suffer from these disorders recount emotional mistreatment and physical neglect more often. Quantitative data analysed through a stepwise multiple regression analysis reveals that dissociation scores are statistically significantly affected by sexual abuse, e.g. rape and emotional abuse.
In this context, a recent study on individuals with depersonalisation disorder demonstrated that emotional abuse is the most significant predictor of depersonalisation, but not of general dissociation scores, which were better predicted by a combination of emotional and sexual abuse.Reference Simeon, Guralnik, Schmeidler, Sirof and Knutelska36 Patients with dissociative disorder reported more suicidal thoughts than the patient with PTSD without dissociative disorder.
This study provides additional evidence that dissociative seizures are strikingly connected with traumatic life events, especially rape in ISIS captivity, their relation to shame, which further adds a high biopsychosocial pressure, and their connection with severe mental disorders like somatisation disorders. Thus, our results especially support previous findings on the relationship between dissociative symptoms and traumatic experiences.Reference Gershuny and Thayer39,Reference Lanius, Vermetten, Loewenstein, Brand, Schmahl and Bremner40
Furthermore, this study has revealed that the percentage of prior sexual and physical abuse is significantly higher in the investigation group than in the control group. Other studiesReference Fiszman, Alves-Leon, Nunes, D'Andrea and Figueira41,Reference Nicholson, Aybek, Craig, Harris, Wojcik and David42 have emphasised that prior sexual and physical abuse can be considered significant risk factors for the development of dissociative disorders like dissociative seizures, and for other comorbidities. This observation applies to a significant percentage of the patients. Regression analyses are frequently used to gain further insights into the recounted history of sexual violence. In this case, the recounted history of sexual abuse correlated with a higher likelihood of a dissociative diagnosis. Thus, this study and its observation that sexual mistreatment leads to a higher probability of dissociative disorders emphasises what other studies have concluded:Reference Sharpe and Faye43 These studies revealed a positive correlation between sexual mistreatment and dissociation scores, concluding that individuals who reported a history of sexual violence are more prone to have symptoms of dissociative disorders or dissociative seizures.Reference Nicholson, Aybek, Craig, Harris, Wojcik and David42
Moreover, results of this study suggest that there is a relationship between a history of sexual abuse, PTSD and somatisation.Reference Salmon, Al-Marzooqi, Baker and Reilly44 PTSD and especially sexual abuse (rape) may lead to dissociative phenomena through a process characterised by an increasing tendency of ‘resomatisation’ or toward culturally influenced somatic manifestations of emotional distress: emotional stress combined with a culturally shaped perception of deep shame, ‘loss of face’ and fear of being excluded from the community can lead to increased propensity and the diagnosis of dissociative seizures.
As there is a significant relationship between dissociation and shame, there is also a significant relationship between somatisation and dissociative seizures in response to shame, with regards to rape and trauma. This latter finding might reflect a proposed process in which shame both evokes a physical withdrawal from cues eliciting and a psychological withdrawal (i.e. dissociation) from the painful affect.Reference Goldstein, Drew, Mellers, Mitchell-O'Malley and Oakley34 Among the women raped while being held captive by ISIS, all shame items related to PTSD show a higher rate linked to dissociative disorder. Our results highlight the central role of dissociative disorders or dissociative seizures and shame in connection to PTSD, not least considering the construct of ‘complex PTSD’.Reference Talbot, Talbot and Tu19
From a clinical point of view, our findings emphasise the potential importance of addressing shame and somatisation in treatments for patients with PTSD with dissociation disorders. Approaches that focus on ‘shame-trauma-somatic awareness’ might be an effective tool to address these aspects.
Psychotherapeutically, a treatment extension for patients with PTSD who have experienced heavily traumatic events and suffer from symptoms of a dissociative disorders like dissociative seizures might be considered. This extension should coincide with the therapeutic use of proven techniques focusing on processes related to trauma (e.g. prolonged exposure, eye-movement desensitisation and reprocessing, narrative exposure therapy). At the same time, this study emphasises that there is a lack of evidence in optimal treatment procedures for this patient group. At present, a clinical trialReference Øktedalen, Hagtvet, Hoffart, Langkaas and Smucker31 proposes paying early attention to dissociative seizure symptoms with cognitive–behavioural therapy. This view focuses on enabling patients to establish some control over their seizures before undertaking any trauma-related work. As the evidence for robustly effective treatments for dissociative seizures is still at an early stage,Reference Rosenberg, Rosenberg, Williamson and Wolford45,Reference Martlew, Pulman and Marson46 it is currently not possible to indicate conclusively how trauma-related shame interventions considering and respecting the cultural background of the patients might be integrated best while using existing treatment approaches – a possible area for future treatment studies.
The extent to what psychotherapeutic procedures or treatments are possible and helpful depends heavily on the way societies deal with sexuality, sexual violence, rape and trauma. High moral standards, sociocultural limits and internalised attitudes to the issues of ‘honour’ and ‘violation of honour’ can hinder patients from accessing treatment.Reference Kizilhan47
In this respect, the role of shame should not be underestimated, especially in traditional cultures, which are often also characterised by a ‘culture of shame’. Professionals who sufficiently know about how sociocultural influences significantly shape the patients individuality, and who take this into account, are particularly important.
Limitations
Self-report measures may result in potential biases arising from self-presentation concerns and/or retrospective reporting. In addition, the seizure symptom questionnaire used in this study was developed with the aim of examining subjective/psychological seizure symptoms only, rather than the full range of motor and behavioural manifestations often observed during dissociative seizures. Given the importance of the interplay between shame, trauma and dissociative seizure revealed by this study, further research may seek to explore possible relationships between measures of dissociation with ictal motor and/or behavioural symptoms in this population. Future studies may also include larger patient groups of trauma-related shame with and without PTSD in relation to dissociative seizures.
Author contributions
J.I.K. examined the patients and analysed the clinical and psychometric data in Iraq. F.S. and M.N.-H. helped to analyse the clinical and psychometric data. J.I.K., F.S. and M.N.-H. contributed equally to the writing of the manuscript. All authors read and approved the final manuscript.









eLetters
No eLetters have been published for this article.