INTRODUCTION
An estimated 83 million American adults have one or more types of cardiovascular diseases. Of these, more than 5 million have cardiac heart failure, and the prevalence is rising.Reference Go, Mozaffarian and Roger 1 In 2009, there were more than 1 million U.S. primary heart failure hospitalizations and another 3 million with heart failure as the secondary diagnosis.Reference Blecker, Paul and Taksler 2 Heart failure is the second most common reason for hospitalization with an average length of stay being 12.9 days and accounting for 1.4 million hospital days.Reference Tsuyuki, Shibata and Nilsson 3 Similarly, in Canada, heart failure is a common and serious condition that affects 500,000 people.Reference Ross, Howlett and Arnold 4
Readmissions within 30 days following heart failure hospitalization approach 25%.Reference Keenan, Normand and Lin 5 Relapses that result in return visits to the emergency department (ED) represent important adverse health outcomes for heart failure patients and result in important costs to the health care system.Reference Chun, Tu and Wijeysundera 6 Moreover, a reduction in hospital readmissions has been identified as one of the pillars of Medicare reform in the United States. Whereas many studies are related to readmission rates among patients with an initial admission for heart failure, little is known about the issue of the return to the ED for patients initially treated and released by the ED for acute heart failure (AHF).
The objective of this study was to document relapse events and factors associated with return to the ED in the 14-day period following release by the ED for patients with AHF.
MATERIALS AND METHODS
Study design and setting
The Respiratory Admission (RAD) studies were conducted in Canada to develop risk scales for ED patients with AHF and acute exacerbation of chronic obstructive pulmonary disease. We pooled data related to only patients with AHF from two prospective cohort studiesReference Stiell, Clement and Brison 7 , Reference Stiell, Clement and Aaron 8 of the RAD researches. This study is a secondary analysis of two studiesReference Stiell, Clement and Brison 7 , Reference Stiell, Clement and Aaron 8 conducted from September 2007 to September 2014 in six Canadian teaching hospitals in Ottawa, Ontario (two sites); Toronto, Ontario; Kingston, Ontario; Montréal, Quebec; and Edmonton, Alberta. These hospitals have a combined annual ED volume of approximately 350,000 patient visits. These studies were approved by the research ethics boards at each centre. The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.
Population
We did not enrol patients who were obviously too ill to be considered for discharge within the 2- to 15-hour ED treatment study window or who were otherwise unsuitable for the study for the following reasons: 1) resting oxygen saturation (SaO2) < 85% on room air or after being on their usual home oxygen setting for 20 minutes after ED arrival; 2) heart rate greater than or equal to 120 beats/minute on arrival; 3) systolic blood pressure <85 mm Hg on arrival; 4) ischemic chest pain requiring treatment with nitrates on arrival; 5) acute ST-segment elevation on electrocardiogram (ECG) on arrival; 6) terminal status – death expected within weeks from chronic illness; 7) patient was from nursing home or chronic care facility; 8) patient was enrolled into the study in the previous 2 months; or 9) patient was on chronic hemodialysis.
We included a convenience sample of adults above 50 years of age who presented with acute shortness of breath secondary to exacerbations of chronic heart failure or new-onset AHF and subsequently release by the ED after this initial visit. We did not include patients who experienced an inpatient admission during the initial AHF hospitalization. We used pragmatic criteria for the diagnosis of AHF as recommended by the working group on heart failure of the European Society of Cardiology.Reference Cowie, Wood and Coats 9 – Reference Ranasinghe, Wang and Dharmarajan 11 If doubt remained, a beneficial response to treatment (for example, a brisk diuresis accompanied by substantial improvement in breathlessness) was also considered.
Measurements
Patient assessments were made by emergency physicians, registered respiratory therapists, or registered nurses. There was ongoing evaluation of the quality of the patient assessments by a central study nurse coordinator who provided regular feedback to the sites. Blood samples in each of the two cohorts were collected at the time of the study enrolment.
Outcome measures
The primary outcome in this substudy was the number of return visits to the ED for patients who were released by the ED after the initial visit, for any related medical problem within 14 days of the visit. Assessment of the primary outcome measure was made by the investigators, blinded to the patient status for the predictor variables, from these source documents: 1) ED health records, 2) hospital health records, 3) computerized hospital patient tracking and record system, and 4) review of provincial death records. Patients were not contacted by telephone.
Data analysis
We described patient characteristics using percentages for qualitative variables and using means and standard deviation, or median with interquartile range (IQR), depending on the type of distribution, for quantitative variables. Variable distributions were tested with the Shapiro-Wilk normality test. Comparisons between groups were performed using the chi-square test and t-test for parametric distributions, Fisher exact test, and Mann-Whitney-Wilcoxon test for nonparametric distributions. Despite the large number of univariate tests performed, no correction was applied because the goal was to detect associations, not conclude significance. Binary logistic regression with backward stepwise selection was conducted for variables found to be associated with return to the ED on univariate analysis with a p value of < 0.2. For the different models, identification of each covariate was adjudicated by the empiric association with the primary outcome using Akaike’s information criterion. Overall model fit was assessed using the Hosmer-Lemeshow test. Analyses were performed using R version 3.1.1 (R Core Team 2013, R: A language and environment for statistical computing, R Foundation for Statistical Computing, Vienna, Austria). A p value (two-tailed) below 0.05 was considered to indicate statistical significance.
RESULTS
Characteristics of study subjects
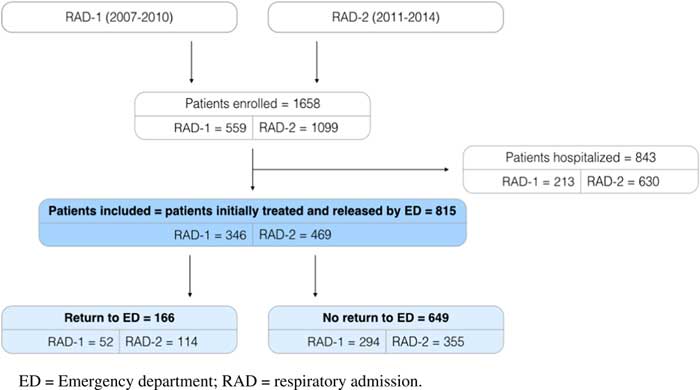
Patient visits totalling 815 were included from September 2007 to May 2014 (Figure 1). Overall, 56% patients were male. Patients had a mean (± SD) age of 76.1 (10.5) years. Return to the EDs occurred in 166 (20%) patients. The main documented reason was worsening dyspnea (71%). Of all patients who returned to the ED within the 14-day period, 77 (47%) were secondarily admitted to the hospital. Table 1 shows the characteristics and the outcomes of the patients.

Figure 1 Patient flow diagram.
Table 1 Patient characteristics and outcomes

ACE=angiotensin-converting enzyme; CABG=coronary artery bypass graft; COPD=chronic obstructive pulmonary disease; CXR=chest X-ray; ECG=electrocardiogram; NT-proBNP=N-terminal prohormone of brain natriuretic peptide; PCI=percutaneous coronary intervention; pCO2=partial pressure of CO2; SaO2=oxygen saturation; TIA=transient ischemic attack; URL=upper reference limit.
Univariate analysis
Patients who return to EDs had a lower systolic blood pressure (134.3±27.5 v. 144.4±28; p < 0.001) and a higher heart rate (85±20.1 v. 80±18.6; p=0.005). Overall, 22 of the univariate associations between hemodynamic profiles and prespecified risk factors were statistically significant with a p value of < 0.2. Among them, 16 variables were considered for the multivariate analysis. Because of high Pearson correlation coefficients and missing values, six variables were not included in the final model. Table 2 shows the univariate analysis between return to the ED and the characteristics of the 815 patients released by the ED after management of AHF.
Table 2 Univariate association with return to ED for 815 heart failure patient visits then discharged

ACE=angiotensin-converting enzyme; CABG=coronary artery bypass graft; COPD=chronic obstructive pulmonary disease; CXR=chest X-ray; ECG=electrocardiogram; NT-proBNP=N-terminal prohormone of brain natriuretic peptide; PCI=percutaneous coronary intervention; pCO2=partial pressure of CO2; SaO2=oxygen saturation; TIA=transient ischemic attack; URL=upper reference limit.
Multivariate analysis
Multivariable analysis indicated that the following factors were independently associated with return to the ED (Table 3): past medical history of percutaneous coronary intervention (PCI) or coronary artery bypass graft (CABG) (aOR=1.51; 95% CIs [1.01-2.24]); current use of antiarrhythmics medications (aOR=1.96; 95% CIs [1.05-3.55]); heart rate above 80/minute (aOR=1.89; 95% CIs [1.28-2.80]); systolic blood pressure below 140 mm Hg (aOR=1.67; 95% CIs [1.14-2.47]); SaO2 above 96% (aOR=1.58; 95% CIs [1.08-2.31]); troponin above the upper reference limit of normal (aOR=1.68; 95% CIs [1.15-2.45]); and chest X-ray with pleural effusion (aOR=1.52; 95% CIs [1.04-2.23]). This model was developed on a data set of 730 cases without missing values. This model had a nonsignificant Hosmer-Lemeshow chi-square goodness-of-fit (GOF) statistic (GOF=0.66), and the area under the receiver operating characteristic curve was 0.69 (95% CIs [0.65-0.73]).
Table 3 Independent predictors of return to ED as determined by stepwise logistic regression analysis for acute heart failure patientsFootnote *

Hosmer-Lemeshow goodness-of-fit p value=0.66; area under ROC curve=0.69 (95% CI [0.65-0.73]).
* Model developed for 730 patients without missing values. CABG=coronary artery bypass graft; CXR=chest X-ray; PCI=percutaneous coronary intervention; SaO2=oxygen saturation; URL=upper reference limit.
DISCUSSION
Interpretation
The patients in our study were relatively older in age (median [IQR]=77 years [69-84]). They had important medical comorbidities and cardiovascular risk factors (72% with heart failure; 66% with hypertension). They well represent patients presenting in the EDs in Organisation for Economic Co-operation and Development (OECD) countries. Because of these significant morbidities, patients in our study were often treated inconsistently (55% beta blockers; 74% diuretics). In our study, half of the AHF patients who presented for the first time were released by the ED. Yet, among these patients, 20% returned to the ED within 14 days, most commonly for dyspnea (71%). This is a relatively high rate of returns to the ED (i.e., one in five patients). We are concerned by this disturbingly high rate. Indeed, it exposes patients to potential harms such as hospital acquired infection. Moreover, it leaves an important overwork on EDs and acute care resources. As a consequence of this overwork, EDs and hospital crowding adversely impact patient care. Of these patients who returned, nearly half of the patients were subsequently hospitalized (47%).
To prevent the ED returns of these patients, we identified several independent variables associated with this return. The two clinical variables most strongly associated with returns to the ED were initial high heart rate and low systolic blood pressure. These two parameters can be interpreted as a reflection of a hemodynamic stress. However, these differences were of minimal clinical significance. We also assume that these parameters reflect an already low extracellular volume while the patient has congestive symptoms, reflecting a sign of acuteness. Other variables independently associated with a return to the ED reflect the important comorbidities of patients and reflect their fragility. Indeed, patients with a medical history of PCI or CABG were more likely to return to the ED.
Review of previous literature
Our study confirms the frequent returns in ED for AHF patients and the issue of the initial care provided to patients.Reference Calder, Tierney and Jiang 12 In our study, the hospitalization rate for AHF patients was 47%. This rate is relatively low compared with other studies that found hospitalization rates between 70% and 80% in the United States.Reference Singer, Skopicki and Thode 13 Nevertheless, this difference between Canada and the United States has been previously described. Indeed, Lai et al. found a striking difference in the admission rates because it appeared that the Mayo Clinic admitted almost twice as many AHF patients compared to The Ottawa Hospital (95% v. 51%), and yet the outcomes of return to the ED and death within 30 days were similar.Reference Lai, Tenpenny and Nestler 14
Our study shows that simple clinical parameters, such as a high heart rate and low systolic blood pressure, enable the detection of patients at risk of return to the ED. In a large retrospective study, Fonarow et al.Reference Fonarow, Adams and Abraham 15 also found an association of these two parameters with mortality. Similarly, Gheorghiade et al.Reference Gheorghiade, Abraham and Albert 16 showed that high blood pressure confers some form of advantage in heart failure patients. Unlike the Fonarow et al. study, in which patients were admitted in the ED, our study validates these results for patients released by the ED. Whereas Fonarow et al. found renal function to be strongly associated with prognosis, our study finds this factor to be true in the univariate analysis only. We found an association between cardiovascular patient medical history and return to the ED. However, medical history of dementia was not associated with more ED returns, whereas Dodson et al.Reference Dodson, Truong and Towle 17 showed an association between dementia and poor prognosis in patients with heart failure. This can be explained by the increased number of cognitively impaired patients in this study (132 patients), whereas in our study we enrolled only 19 patients with dementia. In our study, a higher SaO2 was independently associated with returns to the ED. The mean difference between the two groups was very low (95.2% v. 95.5%). Given the limited clinical relevance of this finding, its interpretation is difficult.
Clinical impact
A recent systematic review showed that returns to the ED deemed potentially avoidable were relatively uncommon, comprising less than 20% of all returns to the ED following hospital discharge.Reference Walraven, Jennings and Taljaard 18 However, Retrum et al. showed that, contrary to prior literature, patient experiences were highly heterogeneous and not easily categorized as preventable versus not preventable.Reference Retrum, Boggs and Hersh 19 These results appear to support a case-by-case assessment to improve the prognosis of patients. In addition, an early follow-up after discharge is critically important.Reference Hernandez, Greiner and Fonarow 20 Several studies have shown that regular monitoring of the patient out of the hospital decreased returns to the ED in the week following the dischargeReference Eastwood, Howlett and King-Shier 21 or later.Reference Feltner, Jones and Cené 22 Identification of factors associated with return to the ED is the first step in developing interventions to reduce these events. Indeed, interventions to prevent these returns can be directly implemented in the ED. In a retrospective study, Hadi et al.Reference Hadi, Hellman and Malik 23 evaluated a very early and dedicated supportive intervention by a specific team to patients readmitted for AHF. The authors showed that such intervention reduced the rate of return to the ED within 30 days, from 23% to 17% (p < 0.05). Future prospective studies,Reference Black, Romano and Sadeghi 24 currently underway at six academic medical centres located throughout the state of California, USA, also aim to evaluate a more active monitoring of returns to the ED for AHF.
CONCLUSION
The aim of our study was to better understand the patients who return to the ED after an initial consultation for AHF. Many heart failure patients (i.e., one in five) are released from the ED and then suffer return to the ED. We show that it is the patients with multiple medical history, and those with a systolic blood pressure of < 140 mm Hg or heart rate > 80 bpm who are associated with returns to the ED. Their identification and monitoring could lead to interventions to reduce this important outcome.
Acknowledgements: The authors are very grateful to the many physicians, nurses, respiratory therapists, and research assistants at the study hospitals for their helpful assistance with patient identification and data collection. Authors confirm that they have read and approved the paper. They also confirm that they have met the criteria for authorship as established by the International Committee of Medical Journal Editors, believe that the paper represents honest work, and are able to verify the validity of the results reported. PGC and IGS conceived the study and wrote the manuscript. IGS was the director of this research project and participated in the writing of the manuscript. PGC was responsible for the statistical analysis. PGC, LAC, IGS, JWY, JJP, and BHR was involved in drafting the manuscript and/or revising it critically for important intellectual content. All authors have given their final approval of the version to be published and agree to be accountable for all aspects of the work and ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Financial support: Canadian Institutes of Health Research (Ottawa, ON) supported this research.
Competing interests: None declared.