The SARS-Cov-2 pandemic has affected nearly the entire world and has led to considerable loss of life and high rates of physical morbidity. Moreover, the pandemic has seriously affected economies and individual livelihoods. Previous epidemics had tremendous negative consequences on the mental health of various population groups such as health care workers and survivors of the infectious disease (Zürcher et al., Reference Zürcher, Kerksieck, Adamus, Burr, Lehmann, Huber and Richter2020). However, past epidemics have also negatively impacted the mental health of general populations at large (Zürcher et al., Reference Zürcher, Kerksieck, Adamus, Burr, Lehmann, Huber and Richter2020). Therefore, during the first wave of the Coronavirus pandemic and the first phase of lockdowns, there were widespread fears concerning mental health problems beyond population groups that were directly affected by the illness (The Lancet Infectious Diseases, 2020). Some professional societies even feared a ‘tsunami of mental illness’ (Royal College of Psychiatrists, 2020).
Several systematic reviews and meta-analyses have analysed the extent of mental health problems in the general population during the lockdown phase in spring/summer 2020. Pooled prevalence rates for depression, anxiety and distress reached 30–40% (Krishnamoorthy et al., Reference Krishnamoorthy, Nagarajan, Saya and Menon2020; Luo et al., Reference Luo, Guo, Yu, Jiang and Wang2020; Salari et al., Reference Salari, Hosseinian-Far, Jalali, Vaisi-Raygani, Rasoulpoor, Mohammadi, Rasoulpoor and Khaledi-Paveh2020). Although these reviews did not directly compare pre-pandemic and pandemic time points, the prevalence rates suggest an increase in mental health problems during the first months in spring and early summer 2020 compared to pre-pandemic assessments. These prevalence rates, however, should be interpreted with some caution due to methodological and psychopathological issues (Riedel-Heller and Richter, Reference Riedel-Heller and Richter2020). To start with methodological caveats, many studies suffer from problems with sampling and sample size – which is understandable in the circumstances of an immediate outbreak. From a psychopathological perspective, it is unclear to what extent the prevalence rates that are measured with self-report instruments reflect common distress that is to be expected in such public health crises and to what extent this distress will result in increasing rates of mental disorders and health care utilisation demand. Therefore, we have decided to remain cautious and to stick to the terminology of ‘mental health problems’ rather than ‘mental illness’.
Another point that needs to be considered is the research design of most studies in this field. Most studies have utilised either a one-time cross-sectional design or have compared pre-lockdown data to cross-sectional results from data collection during lockdown. As nearly all countries eased their restrictions during summer 2020 and many have already entered the second phase of strict non-pharmacological interventions, we seek to explore the course of mental health problems during and after the first phase of lockdowns that is closely related to the first pandemic wave. A longitudinal perspective can help to solve some of the methodological and psychopathological problems and may inform about possible future developments concerning mental health during the pandemic.
Methods
We have conducted a rapid review of multi-wave studies that gathered data from general populations during and/or after the first lockdown phase in 2020. Rapid reviews are recommended in cases where swift information is needed in order to inform policies and administrative responses to health-related challenges (Tricco et al., Reference Tricco, Langlois and Straus2017). In doing so, rapid reviews waive some characteristics of systematic reviews to facilitate a publication that will be utilised more quickly than is common with systematic review. Our rapid review was registered with PROSPERO CRD42020218640.
We searched PubMed (including preprint servers medRxiv, bioRxiv, arXiv, Research Square and SSRN), PsychInfo and the preprint server PsyArXiv with search terms that have been adapted to the requirements of each database (see details in the Supplementary Material). We also searched the search machine Google Scholar with very broad search terms. Inclusion criteria were as follows: studies that covered at least two time points during the first lockdown phase or at least one time point during lockdown and one time point after easing of public health restrictions. Studies that, for whatever reason, reported additional pre-pandemic data were not excluded. Both repeated cross-sectional surveys and longitudinal panel studies were deemed to be analysed. Included languages were English, French, Dutch, Spanish and German. Publications in other languages were excluded. Further, we included only studies that utilised psychometrically validated instruments for assessing mental health problems. Any reporting modus (means, prevalence rates, regression coefficients) was included as long as data on at least two time points were reported. Exclusion criteria were (a) health care workers, (b) survivors or patients with SARS-CoV-2, (c) vulnerable populations with a risk of being marginalised that live in precarious situations, with poor access to health care services, with chronic physical conditions (e.g. homeless people, people with pre-existing mental illness, indigenous populations, cancer patients), (d) specific subpopulations (e.g. students, young adults, seniors). The search was conducted by DR and randomly checked by SZ.
We extracted the following data: authors, country of data collection, publication status (preprint v. peer-reviewed publication), sampling procedure, sample size, utilised assessment instrument, scale means or prevalence rates at the following time points: pre-lockdown, first and last time points during lockdown, post-lockdown. Results were briefly summarised in a separate column. In the case of non-reporting of means or prevalence data (e.g. when coefficients were reported), we extracted the result as provided by the authors. When only figures were presented, we estimated the exact numbers by measuring the bars. In cases where prevalence rates and scores were reported from the same study, we extracted both indicators. In order to provide a simplified overview of the changes during and after the first lockdown phase, we will display the results in three figures in the Supplementary Material.
Data extraction was conducted by DR and checked by SZ. Quality appraisal was conducted with an adapted instrument (Munn et al., Reference Munn, Moola, Lisy, Riitano and Tufanaru2015). Items were rated on the options: yes, no, unclear. Following criteria were covered: sampling frame, sampling method, sample size, subjects and setting description, coverage, standardised procedures and response rate. Quality appraisal was conducted by SZ and randomly checked by DR. The application of meta-analytical methods was impossible due to the heterogeneity of instruments, time points and measures. There was no funding source for this study.
Results
After study selection (Fig. 1), we included 23 publications into the qualitative and narrative synthesis. Four of these studies covered the USA, another four were from Germany (one jointly with Austria) and three were from the UK. Apart from the two publications from China, the remainder of the studies were single publications from various countries that predominantly covered European populations. Sixteen studies were peer-reviewed, seven were published as preprints.
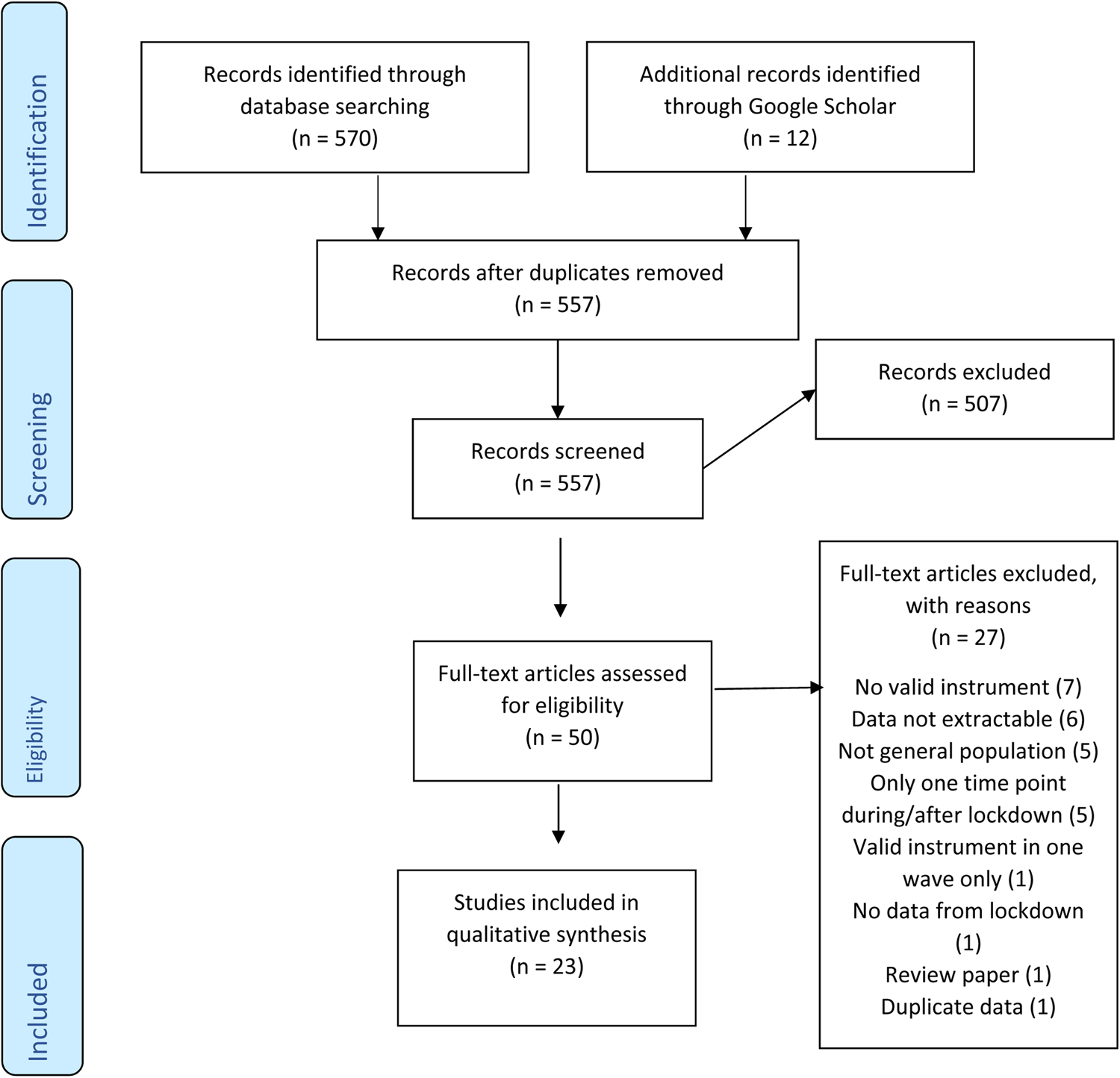
Fig. 1. Flow-chart according to PRISMA.
We identified the following study characteristics (Table 1). The sample sizes ranged from less than 200 to 90 000 per time point. Twelve studies managed to collect data from representative samples while 11 utilised convenience or snowball sampling. The included studies reported results from 56 indicators. This means that many studies utilised two or three instruments simultaneously (e.g. anxiety plus depression). Seven studies reported data from pre-pandemic time points, six from post-lockdown phase. The instrument most utilised was the ‘Depression, Anxiety, and Stress Scales’, followed by the ‘Patient Health Questionnaire’ and the ‘Generalised Anxiety Disorder Assessment’. Different versions of these and other scales were used. Our quality appraisal (Supplementary Material) has shown that many studies have issues with sampling, recruitment and coverage, while the research procedures and the description of subjects and settings were well reported.
Table 1. Characteristics of multi-wave studies reporting on mental health problems for at least two time points (during the first lockdown/pandemic wave or during the first lockdown/pandemic wave and a time point after easing of public health restrictions)
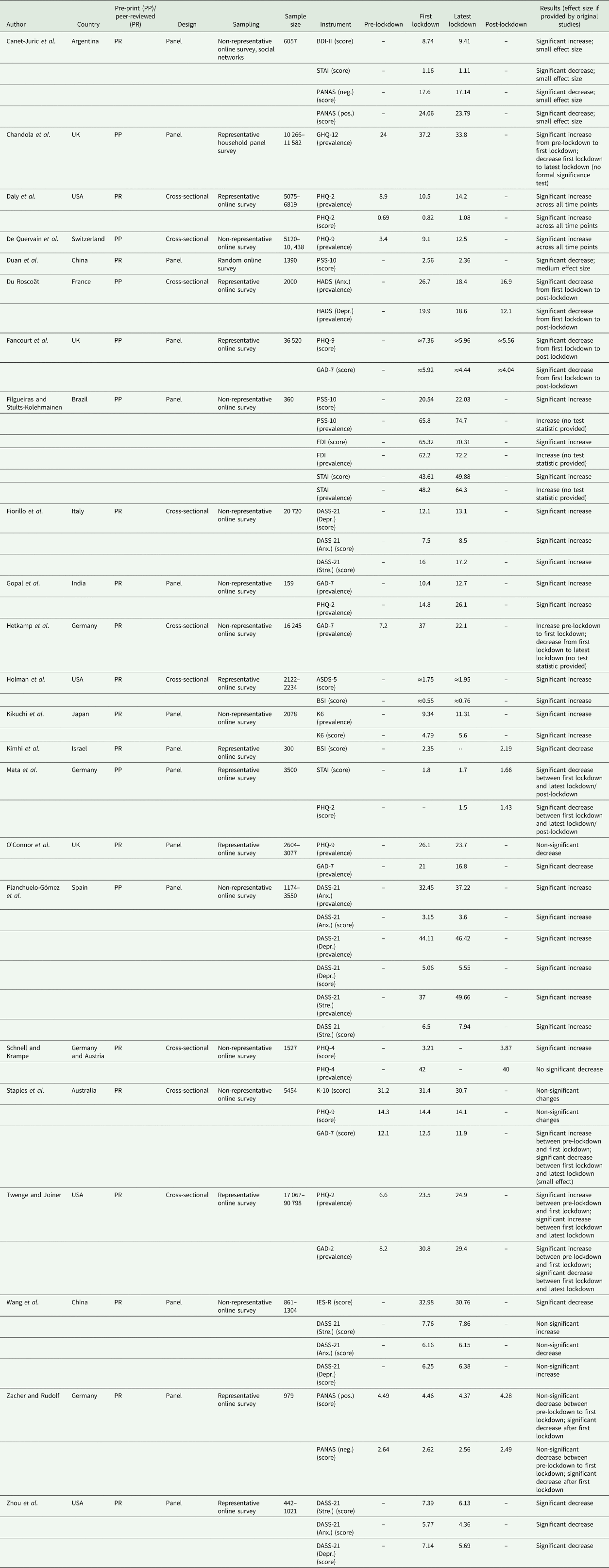
ASDS-5, Acute Stress Disorder Scale-5; BDI-II, Beck Depression Inventory-II; BSI, Brief Symptom Inventory; DASS-21 (Anx.), Depression, Anxiety, Stress Scale – Anxiety; DASS-21 (Depr.), Depression, Anxiety, Stress Scale – Depression; DASS-21 (Stre.), Depression, Anxiety, Stress Scale – Stress; FDI, Filgueiras Depression Inventory; GAD-2, Generalised Anxiety Disorder-2; GAD-7, Generalised Anxiety Disorder-7; GHQ-12, 12-item General Health Questionnaire; HADS (Anx.), Hospital Anxiety and Depression Scale; HADS (Depr.), Hospital Anxiety and Depression Scale; IES-R, Impact of Event Scale-Revised; K-10, Kessler Psychological Distress Scale; K6, Kessler Psychological Distress Scale; NA, text; PANAS (pos.), Positive and Negative Affect Schedule – Positive Affect; PHQ-2, Patient Health Questionnaire-2; PHQ-4, Patient Health Questionnaire-4; PHQ-9, Patient Health Questionnaire-9; PSS-10, Perceived Stress Scale-10; STAI, State-Trait Anxiety Inventory.
≈, results provided in graphical format only.
The changes of means, prevalence rates and coefficients were not uniform across indicators, types of mental health problems and time points (see online Supplementary Figs 2–4). The general impression was as follows: a huge variation during lockdown but no uniform trends and a slight decrease of indicator data after lockdown. We also noted an increase from pre-pandemic times to lockdown.
We also looked for trends in specific types of mental health problems (e.g. anxiety or depression) and for trends in countries with more than two studies. Again, we found no uniform trends across studies.
Discussion
This rapid review has compiled data from multi-wave studies that analysed mental health problems during and after the first lockdown phase of the SARS-Cov-2-pandemic. We did not find a uniform trend of mental health problems and assume – without being able to quantify – a considerable heterogeneity. However, the most likely ‘big picture’ that emerged is as follows: as suggested by previous systematic reviews (Krishnamoorthy et al., Reference Krishnamoorthy, Nagarajan, Saya and Menon2020; Luo et al., Reference Luo, Guo, Yu, Jiang and Wang2020; Salari et al., Reference Salari, Hosseinian-Far, Jalali, Vaisi-Raygani, Rasoulpoor, Mohammadi, Rasoulpoor and Khaledi-Paveh2020), an increase in mental health problems can be seen from pre-pandemic time points to the first phase of the lockdown. During the first phase, we see a diversity of trends, some increasing, some decreasing and some with no changes. After the easing of the restrictions, we mainly find a slight decrease in mental health problems. This decrease, however, does not reach pre-pandemic levels.
Several methodological, psychopathological, pandemic-related, lockdown-related and policy-related issues have to be considered while interpreting this somewhat unclear picture.
(1) Methodologically, we found a diversity of instruments, of versions of the same instrument and sampling approaches that were utilised in the studies. Additionally, we found many studies that used more than one indicator answered by the same respondents. This methodological challenge is known from previous reviews on prevalence changes of mental illness and needs to be accounted for as the effect sizes are dependent (Richter et al., Reference Richter, Wall, Bruen and Whittington2019; Fernandez-Castilla et al., Reference Fernandez-Castilla, Jamshidi, Declercq, Beretvas, Onghena and Van den Noortgate2020).
(2) In terms of psychopathology, we found several mental health problems that were addressed: anxiety, depression and distress among them prominently. While these are negative emotional reactions, it is not clear what kind of problem is most relevant and whether these problems reflect general distress. And again, we did not find a clear trend that emerged in this regard. Additionally, we have seen statistically relevant differences in means and prevalences between time points during and after lockdown that prima facie do not indicate large clinical relevance and effect size.
(3) In many countries, the mental health-related consequences of the pandemic cannot be clearly separated from lockdown effects as lockdowns are commonly implemented when infection rates are high. Nevertheless, we assume that emotional reactions to the infection are a major background of the mental health problems that have emerged. Although consequences from financial hardship will certainly impact emotional states during the pandemic, research has shown that people who received financial support during the pandemic reported less mental health needs than those who did not receive such support (Berkowitz and Basu, Reference Berkowitz and Basu2021). Many countries, even in the developing world (e.g. Brazil), have supported their citizens with financial aid or furlough programmes during the pandemic (Richter, Reference Richter2021).
In this regard, it needs to be considered that the first wave of the pandemic in larger countries did not hit the entire country at the same time. In many countries, the pandemic spread from hotspots (e.g. Lombardy in Italy or the Northeast of the USA) to other areas. Data from the United States Centers for Disease Control suggest that mental health problems are to a certain extent correlated to infection rates (CDC, 2020). Therefore, precise points of time of data collection and actual infection rates in the region where respondents live are crucial information that is commonly missing in the publications.
(4) The implementation of non-pharmacological interventions, summarised as lockdown, was not uniform across countries or sometimes even within countries (e.g. the USA). Some states implemented very strict measures that locked citizens up in their houses, other states ordered curfews at night-time only, and other jurisdictions again adopted a ‘lighter’ approach (Oxford University, 2020). As the rigidity and time length of restrictions is known to be of importance in terms of mental health problems (Huremovic, Reference Huremovic and Huremovic2019; Brooks et al., Reference Brooks, Webster, Smith, Woodland, Wessely, Greenberg and Rubin2020), we assume that those differences need to be accounted for when interpreting data on mental health during and after lockdown. Further, the success of measures in terms of the reduction or even suppression of infection rates needs to be considered.
(5) Alongside differences in the implementation of non-pharmacological intervention, states have also shown a diversity of policy responses. While some political leaders have clearly and consistently communicated the risks of the pandemic and of non-adherence to restrictions, others have denied the public health crisis and have defied recommendations from experts. As empirical research has demonstrated, this clearly had an impact on the general public. In the USA, for example, the politicisation of the pandemic has led to diverse views and behavioural responses according to political camps (Zhao et al., Reference Zhao, Wu, Crimmins and Ailshire2020). We assume that these differences will also impact the emotional response to the pandemic. When people see the virus as non-existent or to be of minor risk, there is no reason to be worried about it. In addition, states have differed to a certain extent in the welfare response that aimed at mitigating the economic and psychosocial consequences of the pandemic. The longer the pandemic is not sufficiently suppressed, the more important the welfare state response in terms of mental health becomes.
As data on other mental health indicators suggest, the first lockdown phase has – in general – not led to an increase in mental health care utilisation. A UK study reported that the demand for mental health care decreased partly due to fears of becoming infected in health care settings (Chen et al., Reference Chen, Jones, Underwood, Moore, Bullmore, Banerjee, Osimo, Deakin, Hatfield, Thompson, Artingstall, Slann, Lewis and Cardinal2020). A large German statutory health insurer published a report that indicated a sharp increase in mental health-related sick leave during the first pandemic peak that had returned to ‘normal’ levels during spring and summer of 2020. This report concluded: ‘It would be inappropriate to derive increasing mental illness rates from these data’ (Techniker Krankenkasse, 2020: 44; our translation). Also, suicide rates and suicide attempt rates in various countries do not seem to have risen compared to pre-pandemic times (e.g. Hernandez-Calle et al., Reference Hernandez-Calle, Martinez-Ales, Mediavilla, Aguirre, Rodriguez-Vega and Bravo-Ortiz2020; John et al., Reference John, Pirkis, Gunnell, Appleby and Morrissey2020; Leske et al., Reference Leske, Kõlves, Crompton, Arensman and de Leo2020). Whether these trends will hold in further infection or lockdown phases remains to be seen. Our assumption that post-lockdown mental health problems have not decreased to pre-pandemic levels is concerning in this regard. Newly imposed restrictions during the second phase of lockdown together with infection rates that are much higher than during the first pandemic wave and increasing economic worries may induce more mental health problems in future weeks and months. This may also result in a higher demand for mental health services.
Conclusions
We conclude from this rapid review that mental health problems in the general population have not essentially changed during the first lockdown after they have risen compared to pre-pandemic times. After easing of lockdown restrictions, they have decreased to a level that is assumingly higher than before the pandemic. As many data sources do not indicate an increasing demand for mental health care utilisation during the first wave of the pandemic, we interpret these mental health problems generally as distress that is to be expected during a global public health crisis. This conclusion, however, does not disregard that some individuals or some population groups have suffered psychologically over and above the commonly to be expected distress in the first half of 2020. Again, studies on people with pre-existing mental disorders, for example, do not generally suggest worse outcomes during the first lockdown phase. While some studies see more distress in this group (Liu et al., Reference Liu, Stevens, Conrad and Hahm2020; O'Connor et al., Reference O'Connor, Wetherall, Cleare, McClelland, Melson, Niedzwiedz, O'Carroll, O'Connor, Platt, Scowcroft, Watson, Zortea, Ferguson and Robb2020), others reject this hypothesis (Pinkham et al., Reference Pinkham, Ackerman, Depp, Harvey and Moore2020; Schutzwohl and Mergel, Reference Schutzwohl and Mergel2020). Our conclusion does not disregard that there is a certain risk for increasing mental illness and demand for mental health care in the general population the longer the pandemic and its economic and psychosocial consequences will last.
In terms of methodology, we caution against the over-interpretation of results from single studies on mental health problems during the pandemic. Similar to meta-analyses of clinical trials which oftentimes provide conflicting results on health care interventions, only aggregate and synthesised data are able to inform on general trends. This is particularly the case during this pandemic as various confounding factors need to be considered when trying to get a clearer perspective on the complexity of mental health problems in such a crisis.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S2045796021000160.
Data
All data are shown in Table 1. No further data have been used for the analyses.
Acknowledgements
None.
Financial Support
None.
Conflict of Interest
None.






