On 7 April 1904, 29-year-old May Beecham was admitted to the Gynaecological Department of the Royal Free Hospital under the care of Mary Scharlieb.Footnote 1 Nine days before, she had experienced a ‘flooding’, noticing dark red lumps, which Mrs Beecham described as resembling ‘pieces of liver’, coming away when she passed water. Since this point, she had lost large clots, ‘nearly half a pint at a time’, daily. Sufficiently concerned about her symptoms, May Beecham visited the Out-Patient Department at the RFH on 2 April, and was informed that she must see Ethel Vaughan-Sawyer, Scharlieb's assistant, at Gynaecological Out-Patients, for a more specialist opinion on her condition. At the next relevant opportunity, four days later, Mrs Beecham came back, saw Vaughan-Sawyer and was told she must come in immediately. She became an in-patient the next day. In a little over a week after experiencing any symptoms, and never having suffered any pain stronger than some bearing-down sensations before the floodings, May Beecham was informed she required an urgent operation for a rapidly growing carcinoma of the cervix.
Eight patients admitted to the RFH in 1904 under Scharlieb were suffering from cancer.Footnote 2 Four of these were diagnosed, like Mrs Beecham, with carcinoma of the cervix; one from epithelioma of the vulva and another from malignant disease of the liver. May Beecham was different in a number of ways. Firstly, she was the youngest, by a considerable margin; her nearest contemporary was 41, while the other six were aged between 45 and 77. In a textbook first published in 1908, Johns Hopkins University's Professor of Gynaecological Surgery, Howard Kelly, noted that uterine and cervical carcinomas were diseases of the over-forties, with few of the latter occurring before 40 and after 60. While not impossible, diagnoses in those aged between 20 and 30 were ‘exceptional’.Footnote 3 Secondly, May Beecham's symptoms had been largely painless and extremely recent. This was not unusual for her condition, where pain frequently indicated that the disease had been caught too late.Footnote 4 However, unlike many who suffered similarly, she had sought medical help as soon as her symptoms began, as well as returning promptly for appointments made by the various doctors she saw. Such adherence to life-saving advice would have cheered a profession troubled by patient delay in seeking treatment for suspicious growths, unexpected and intermenstrual bleeding.Footnote 5 Thirdly, and most importantly, the combination of her youthfulness and swift reaction, coupled with the willingness of her surgeon to take a risk on her patient's chance of survival, ensured that she was the only cancer patient who left the RFH's Gynaecological Department in 1904 having undergone surgery for her condition. After initial examination and, in some cases, exploration of the extent of the disease, the other seven were deemed inoperable and sent home.
Mrs Beecham's notes recorded the dilemmas which faced her surgeon when considering the severity of her disease and the debate Vaughan-Sawyer entered into when deciding whether or not to try and save her patient's life surgically. Upon initial examination per vaginam, the whole of Mrs Beecham's cervix was seen to be hard and infiltrated with a large friable mass protruding through it; the vaginal wall was also diseased and the base of the left broad ligament was suspected to be involved too. Contemporary opinion, such as that contained in gynaecological surgeon John Bland-Sutton's second edition of Tumours Innocent and Malignant (Reference Bland-Sutton1901), inclined to the melancholic when faced with the spread of the cancer beyond the confines of the cervix itself. Even if it was not too late for operative interference, which it was in around 90 per cent of cases, recurrence was extremely likely and life expectancy poor.Footnote 6 Four days after admission, Vaughan-Sawyer was inclined to take this perspective, as re-examination pointed to infiltration occurring rapidly, rendering surgery hopeless. Although expressing doubt about whether a panhysterectomy was justifiable, due to the extent of the growth, Vaughan-Sawyer wavered in her decision, concluding finally that the patient's youth made her anxious to give her a chance. May Beecham was operated upon the next day. The growth was curetted and then her uterus, fallopian tubes, ovaries and the upper half of her vagina were removed in a procedure lasting a lengthy two and a quarter hours. Surgery revealed that there was no infiltration of the broad ligaments, and while the posterior and left lateral fornices were affected, the rectal mucous membrane was not involved. Pathological enquiries further confirmed that the growth was a squamous-celled epithelioma, but the glands present and the vaginal wall were healthy. May Beecham recovered well from her procedure, despite a little wound suppuration, and left the RFH on 24 May 1904, barely two months after her first symptoms.
Optimistically, May Beecham was discharged as ‘cured’ and, indeed, did not appear again in Vaughan-Sawyer's case notes, which covered the period between 1904 and 1919, nor those of Mary Scharlieb, which finish in 1909.Footnote 7 As a firm believer in the need to keep track of patients, Vaughan-Sawyer frequently added follow-up comments to the notes or attached letters from the patient's own practitioner informing her of their progress, but no further remarks were made about the future of May Beecham.Footnote 8 Vaughan-Sawyer's response to May Beecham's case and her ‘anxiety’ to do something to help her patient raise a number of questions about women surgeons and their treatment of malignant disease in the first two decades of the twentieth century. Rather than leaving her to die, in similar fashion to the other seven cancer patients who were admitted in 1904, Vaughan-Sawyer insisted on risking a radical surgical procedure – namely, an abdominal hysterectomy and the removal of all appendages – in order to give her patient ‘a chance’ of survival. Recent research by Ilana Löwy and Ornella Moscucci on gender and cancer has offered conflicting interpretations of women's involvement in radical surgical procedures. While Löwy has claimed that ‘[s]upport for hysterectomy as a cancer cure was not limited to male doctors. Women surgeons also actively advocated radical surgical approaches’, Moscucci has focused on the ‘“ineffable freemasonry of sex”’ between women doctors and their patients, which, stimulated by a ‘long history of feminist opposition to gynaecological surgery’, determined to find and support alternative, less ‘“mutilating”’ non-surgical means to treat cancerous growths.Footnote 9 Löwy's article ends in 1910, but both this and A Woman's Disease point to a similar trajectory as Moscucci's, noting that from ‘the 1910s onwards the treatment of cervical cancer was dominated by the rays rather than by the scalpel’.Footnote 10 Both argue that non-surgical treatment appealed from the second decade of the twentieth century to the compassionate nature of women surgeons, keen to speak for their sex and offer less invasive procedures.
Neither Löwy nor Moscucci, however, consider directly the position of the British woman surgeon in the 1910s, seen by both as a key decade of change in attitudes. As this chapter will show, in two different general metropolitan hospitals with prominent female surgeons, the Royal Free and the women-only New Hospital for Women, risky surgery was still performed, and, indeed, was the dominant treatment for cancerous growths throughout this decade. This is not to claim that women surgeons entirely ignored or refused to attempt other forms of contemporary ‘cure’, such as the newly discovered properties of X-ray or radium therapies, but recourse was had to both as a last resort and only for inoperable cases: surgery came first. Moscucci has suggested that it was ‘die-hard’ male surgeons who were keen to ‘preserve the pre-eminence of operative treatment’ for cervical cancer,Footnote 11 but at both these institutions radical abdominal procedures were the norm, carried out, altered and perfected for patients with malignant disease from 1900 to 1919. The wealth of extant case notes at the RFH also makes it possible simultaneously to explore the reactions of female cancer patients to the progress of their disease, as well as their responses to proposed and actual treatment over the first two decades of the twentieth century.Footnote 12
Unlike many of their contemporaries, women surgeons’ confidence in radical operative procedures was supported by their belief in the value of a diagnostic trajectory in which surgery was the end point, but not the only part. Rather than relying solely on clinical skills founded on experience, women took advantage of modern technology, such as pathological reports, to aid judgement and prove diagnosis scientifically. Löwy has remarked that the majority of surgeons and gynaecologists still ‘relied above all on direct observation and reading of clinical signs’, believing that this was more ‘reliable than microscopic observations’.Footnote 13 This was applicable even in the early twentieth century, with some older surgeons denying the usefulness of pathology in solving surgical problems. Indeed, as a leading Professor of Obstetrics and Gynaecology, William Japp Sinclair, declared in an address to the BMA in 1902: ‘What is not surgical is futile – it is hardly knowledge.’Footnote 14 Additionally, as already noted in the case of Vaughan-Sawyer, women surgeons were committed to following the progress of their patients after they had left the hospital through personal correspondence, as well as monitoring the conditions of those who lived nearby through the outpatient system. If, as Moscucci notes, women surgeons wanted to compete professionally with their male counterparts by offering more compassionate forms of cancer care than radical surgery by the 1920s, in the first two decades of the twentieth century such a meticulous programme of affirmation and confirmation of diagnosis, surgical treatment and ultimate results would speak for female skill in operative procedures for malignant disease. Operations for cancer were difficult, dangerous and had to be continually adapted for each patient's particular condition and the extent of the disease.Footnote 15 Yet, as with Vaughan-Sawyer's decision to operate on May Beecham, giving patients a ‘chance’ of survival through the best means available ensured that the women practitioners considered here supported surgical intervention above all else, in spite of the risks involved.
This chapter will ask three key questions about women surgeons and the treatment of malignant disease in the decade and a half between 1904 and 1919. Firstly, what conditions did they treat and how did they operate? Secondly, whom did they treat and why, and, finally, what was the experience of those patients treated? While the first two sections will refer to both hospitals already mentioned, the final analysis will be of the extensive RFH gynaecological case notes, where patients diagnosed between 1904 and 1914 can be followed through to possible five-year ‘cures’. Patient reactions to cancer and its treatment were dominated by lay perception of a disease which was beginning to rival tuberculosis as the era's greatest public health concern.Footnote 16 Why potential sufferers did not request medical advice sooner and the response of the general practitioner to a possible cancer will additionally be considered, alongside the perception of what delayed seeking treatment. However, I will also take into account the professional pessimism towards cancerous growths in the early twentieth century and the initial reluctance to operate on potentially ‘hopeless’ cases by a number of surgeons. This, in turn, fuelled public suspicion of surgical value when faced with this still poorly-understood disease.
Cancer Treatment at the New Hospital for Women, 1900–1919
Although previous research has primarily focused on gynaecological experience,Footnote 17 women surgeons at the RFH and the NHW operated on a variety of cases, as befitted the general status of these institutions. That the latter only admitted women and children (and boys below a certain age) did not mean that it treated exclusively gynaecological nor even female-only malignancies, nor carried out surgery solely on these conditions, as we have already seen, as regards the New, in chapter 1. The NHW, indeed, was compelled to make its general status clear in 1905 to the charitable King Edward's Hospital Fund for London, which had been under the impression that the hospital was ‘solely for Gynaecological cases’ and the ‘diseases of women’.Footnote 18 While the RFH staff dealt primarily with the diseases of women, as their job titles suggested, they were also confronted with other abdominal complaints and disorders, which were not always passed over to colleagues who dealt with surgical cases of both genders. As neither of these institutions were specialist centres and the treatment of cancer in the early twentieth century took place predominantly in general hospitals,Footnote 19 it is helpful to ascertain how frequently women surgeons were confronted with malignancy, as well as how often surgery was performed on those suffering from the disease. The first section of this chapter will go on to focus specifically on rectal surgery at the NHW, both because of its prevalence at this institution and because it was a field in which women, such as the hospital's Senior Surgeon Louisa Aldrich-Blake, were contributing to the development of contemporary surgical procedure.
Public understanding of the increase in cancer cases was stimulated by frightening statistics, which also contributed to medical pessimism about the inability, even in an age of improved antisepsis and asepsis, to halt the progress of this disease surgically. At the BMA Annual Meeting in 1907, Herbert Spencer, of University College Hospital, quoted the Sixty-Eighth Annual Report of the Registrar-General of Births, Deaths, and Marriages in England and Wales to highlight the current state of affairs.Footnote 20 Between 1901 and 1905, there had been just over 73,000 deaths from the most common forms of female cancer. Malignant disease of the uterus, breast, stomach, liver and gallbladder killed over 10,000 women each; uterine cancer killing nearly twice that many. By 1909, deaths ascribed to new malignant growths numbered 34,053 that year alone, and there was a 4 per cent annual increase in cases between 1910 and 1922.Footnote 21 Women, and especially working-class mothers, were seen to be particularly susceptible to cancer. Some medical opinion claimed that with their harsh, poverty-stricken lives, filled with overfrequent strain from childbearing, these women's bodies were rendered fertile ground for the development of malignancy.Footnote 22 As we saw from the previous chapter, it was precisely this type of early twentieth-century patient with whom the Royal Free, and the other hospitals considered here, primarily dealt. It was also the reluctance of this particular group of women to acknowledge the presence of obvious symptoms which medical professionals blamed for consulting too late to improve the rate of cure. Often the disease had spread so that nothing could be done except send patients home to die, as in the case of seven-eighths of the cancer cases under Scharlieb and Vaughan-Sawyer in 1904. While women did not necessarily consult their own sex for ill-health in the first instance, as the previous chapter's study of patients at the RFH revealed, it is vital to consider whether or not female modesty extended to examination and treatment for life-threatening malignant disease by practitioners of the same sex. Whether, indeed, the ‘freemasonry of sex’, as Moscucci has put it, was evident at women-run hospitals or in female-led Gynaecological Departments.
Over the two decades from 1900, the NHW witnessed a steady increase in the number of patients seen. Indeed, twice as many in-patients occupied the hospital in 1919 as they had done in 1900. As noted in chapter 1, the NHW was established and took pride in itself as a primarily surgical institution and this continued to be reflected in the number of operations carried out in the first two decades of the twentieth century (Figure 3.1). While in 1900, just over 50 per cent of in-patient cases were surgical, by 1919, this had increased to over 65 per cent, with a peak in numbers rising to around 70 per cent consecutively between 1911 and 1915. Although the 1910s have been considered a key decade in the gradual replacement of radical surgery with other, less invasive modes of treatment, the New actually saw a rise in the numbers of major operations being carried out.
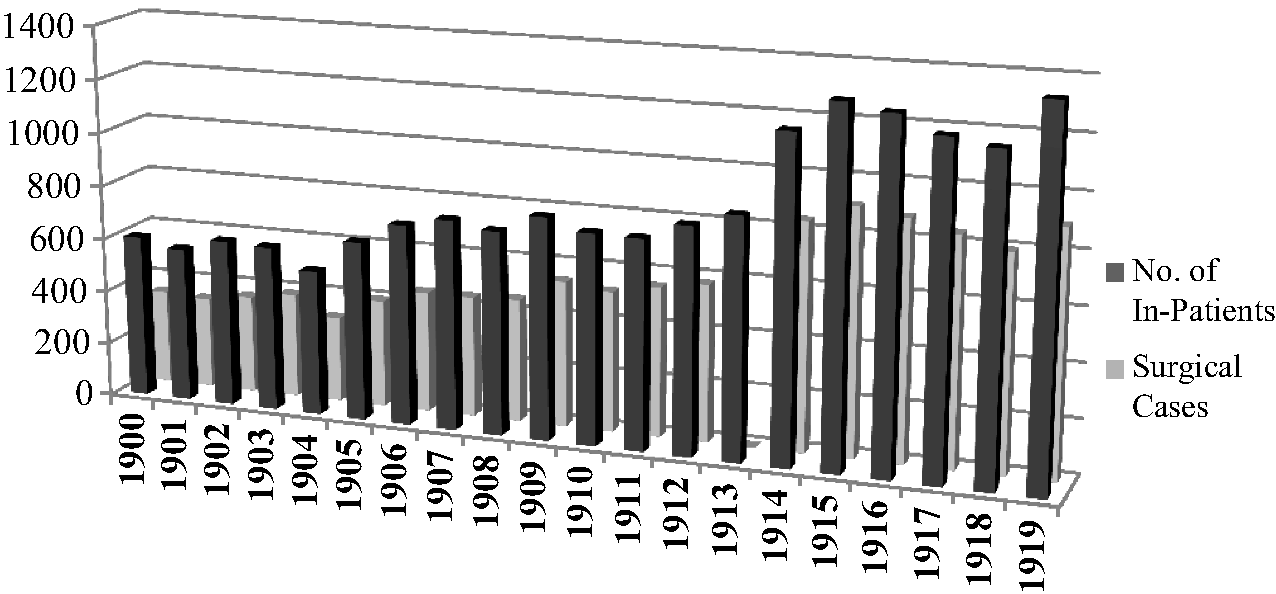
Figure 3.1 Number of In-Patients and Surgical Cases: NHW.Footnote 23
Similarly, the Annual Reports of the hospital from 1906 make reference to the numbers frequenting the newly established Electrical, or X-Ray, Department, with the patients divided into those attending for diagnosis and those for treatment (Figure 3.2).
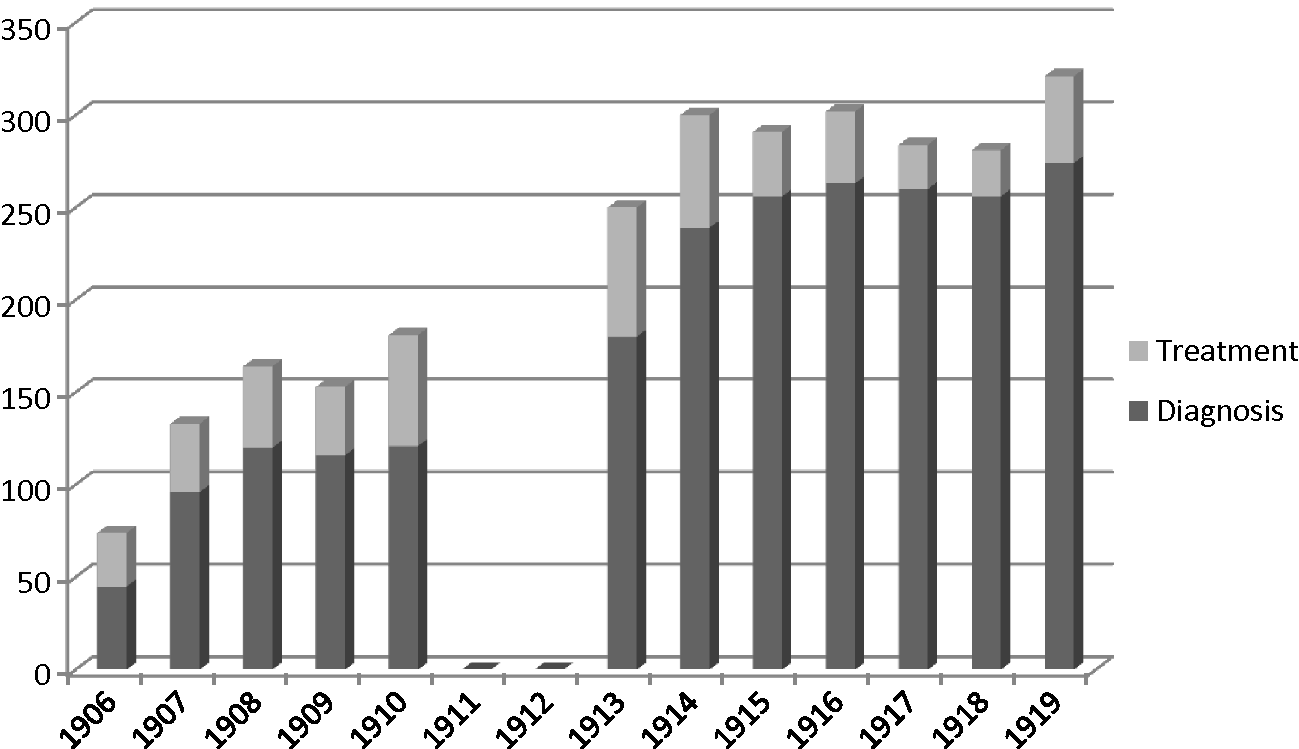
Figure 3.2 Use of the Electrical Department: NHW, 1906–1919.Footnote 24
In both years where a precise list of conditions diagnosed and treated by X-ray were provided, the former made up 72 per cent of the Electrical Department's resources. The sheer variety of conditions treated unsurprisingly bear witness to a new technology being used enthusiastically and experimentally (see Figures 3.3 and 3.4). Neither were the conditions treated gynaecological, as befitting the specialism's scepticism about radiotherapeutic means. In an article published in the Journal of Obstetrics and Gynaecology of August 1914, Cuthbert Lockyer was still trying to convince his fellow British gynaecologists of the need to keep up with medicine's evolution by betaking themselves ‘to the study of radiology’, so far undervalued in comparison with Europe's rapid adoption of techniques.Footnote 25 As Joel D. Howell has noted about the American hospital system's adoption of the X-ray, while machines were purchased by and for hospitals soon after Röntgen's discovery of the rays in 1895, usage of the equipment was primarily for diagnostic reasons and even then was utilised far more infrequently than medical literature would have one imagine.Footnote 26 Figure 3.2 reveals that, at the NHW, after about a 60:40 split in usage between diagnosis and treatment in the earliest years of the Electrical Department's existence, by 1918, fewer than 9 per cent of cases received X-ray treatment. Where the surgeons of the NHW could operate, they did.
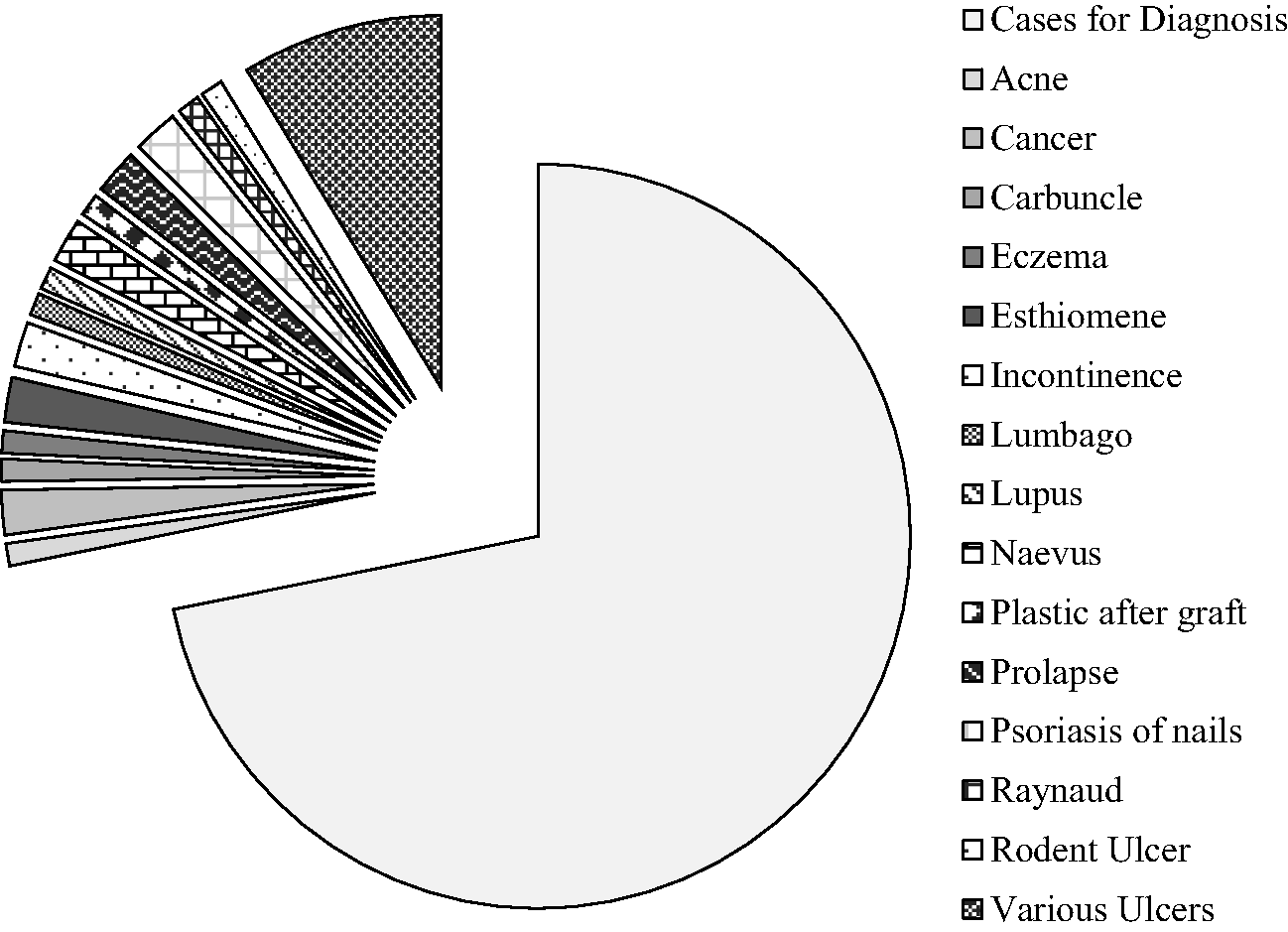
Figure 3.3 X-Ray Usage, With Breakdown of Conditions Requiring Treatment, 1906.Footnote 27
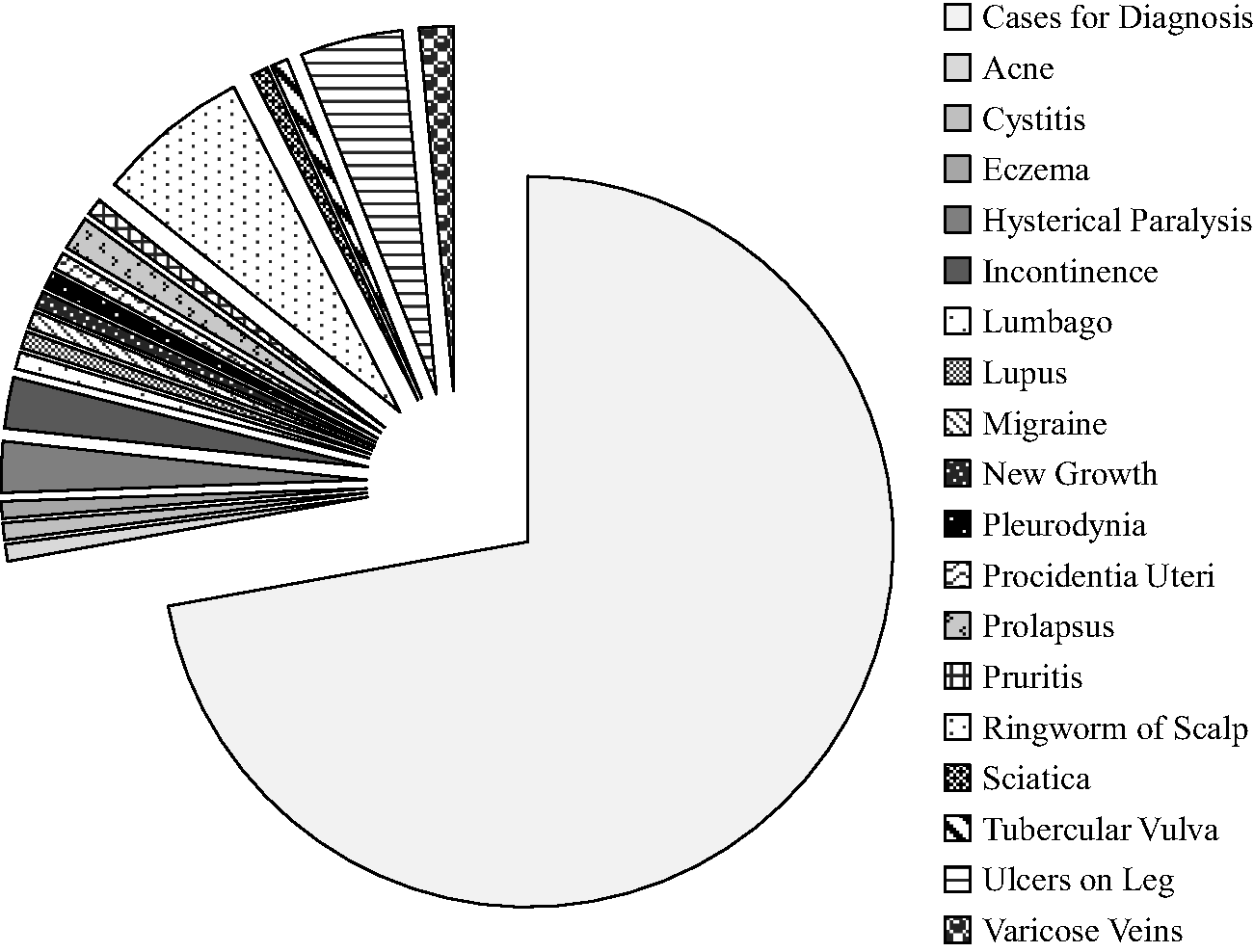
Figure 3.4 X-Ray Usage, With Breakdown of Conditions Requiring Treatment: 1907.Footnote 28
The number of operations carried out over the first 20 years of the twentieth century at the New shows almost a threefold increase from 328 in 1900 to 883 in 1919, with a peak of 914 in 1916. Similarly, the number of major procedures increases over fivefold between 1900, when there were 115, and 1919, when 600 were performed; again, the greatest amount of serious surgery took place in 1916, when operations peak at 604 (Figure 3.5). In 1900, as the graph reveals, minor procedures dominated, but, as the decade ended, the numbers began to reach parity, until major operations were more than three times as many in 1919 than less serious surgery. The surgeons’ confidence in their ability to operate in difficult and risky ways by 1919 provided a stark contrast to the controversy and indecision which dogged the NHW in the first 20 years of its existence, as detailed in chapter 1. Although the 1910s may have witnessed the start of the search for ways of treatment other than surgery, for women surgeons at the New it was a decade where increasing numbers of serious operative procedures were carried out. By 1919, indeed, major surgery was far more likely to take place at the NHW than minor.
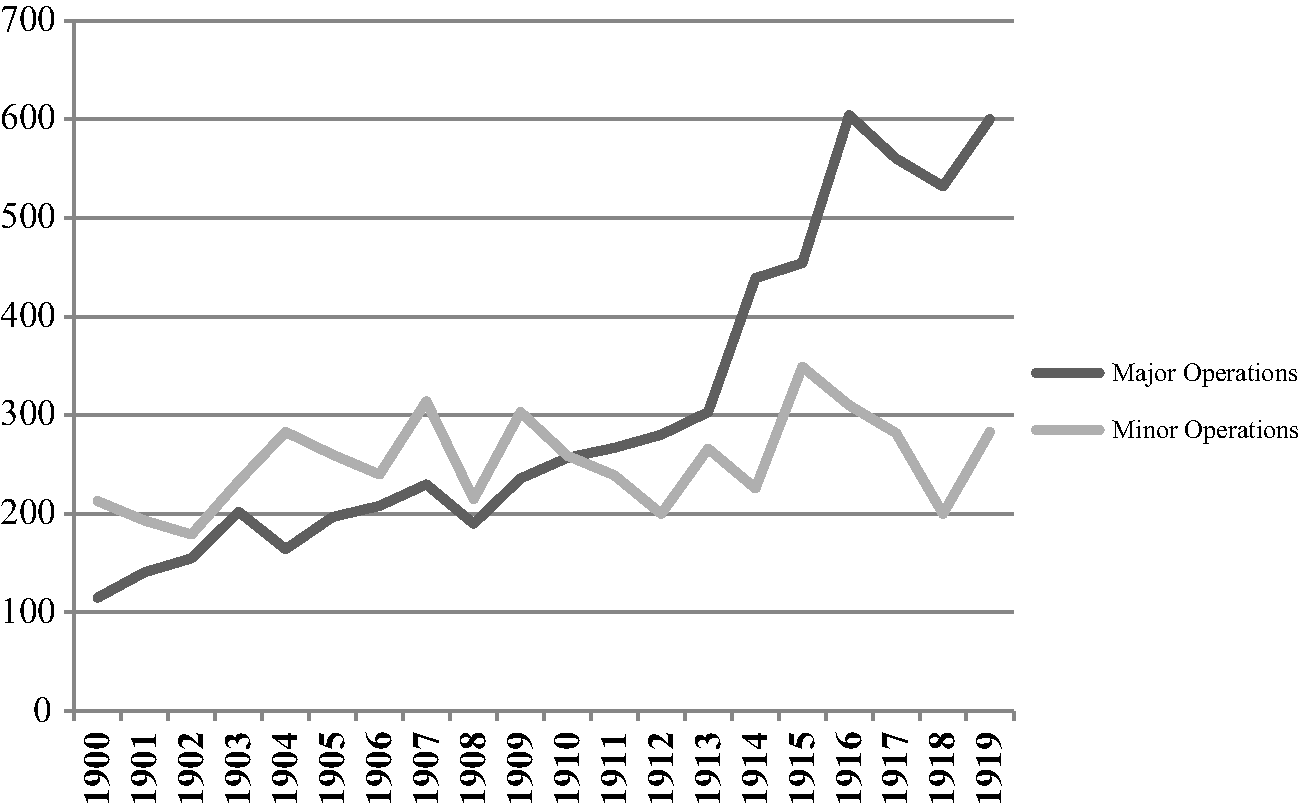
Figure 3.5 Major and Minor Procedures: NHW, 1900–1919.
A decline in alternative, new technologies such as radiotherapy and the corresponding increase in difficult, time-consuming, risky surgery meant that an in-patient at the hospital was more likely to be operated upon under general anaesthetic than treated medically. Through the death of Miss Rosa Morison, who bequeathed the New a large sum of money in her will, the hospital established what it called a House of Recovery or Continuation Hospital at New Barnet in 1912 (Illustration 3.1).Footnote 29 This was not, the New insisted repeatedly to its subscribers, a Convalescent Home, but, rather, an extra limb of the hospital, which freed up space in the main premises for those about to undergo procedures or receive treatment. Some of those who had already been operated upon could therefore spend the rest of their stay in the less urban, more congenial surroundings of North London. In practice, this meant that the NHW could admit more patients and add 20 more beds to its total, which helps to explain, in part, the rise both in the numbers of in-patients in the 1910s and the increase in the number of serious surgical procedures performed. There was simply more room to admit, operate upon and move patients on to the House of Recovery, whose discharge would ultimately be expedited by their removal here. While this new ‘wing’ of the NHW proved efficient in terms of providing extra room, there were problems with its location and purpose. There were complaints about the modes of transportation to Barnet; the bumpy ambulance rides for those recently recovering from surgical operations were far from ideal. Patients also tended to view their novel surroundings as akin to a convalescent home and resented the institutional tenor of the House, with its rules and regulations. There was even an escape mounted in June 1915 as well as revolts over food in October of the same year.Footnote 30 However, despite the initial teething troubles, the House of Recovery played a vital part in the expansion of surgical work at the NHW.
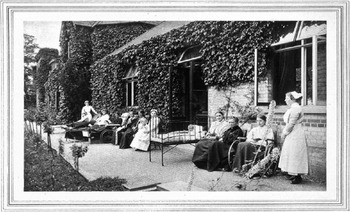
Illustration 3.1 Garden Terrace, Rosa Morison House, New Barnet (c.1916), CMAC SA/MWF/C.44, Wellcome Library, London.
The Annual Report for 1900 had drawn subscribers’ attention to the melancholy ‘constant occupation’ of the new Grace Chadburn (Cancer) Ward and the subsequent fact that many deaths at the NHW were inevitably from malignant disease. Mortality, the Managing Committee of the hospital warned its supporters, would be higher from now on because those suffering from various cancers often remained in the New until they died. That year, out of 23 deaths, 6 had been from malignant disease. Whether the alarm was due to public concern about cancer, or whether the hospital felt the need to defend itself in advance now it had indicated its decision to award malignant disease special ward status, this worrying prediction was not proven over the next two decades (Figure 3.6). The other new addition to the building, an Operating Theatre, however, certainly proved useful in dealing with the increasing numbers.
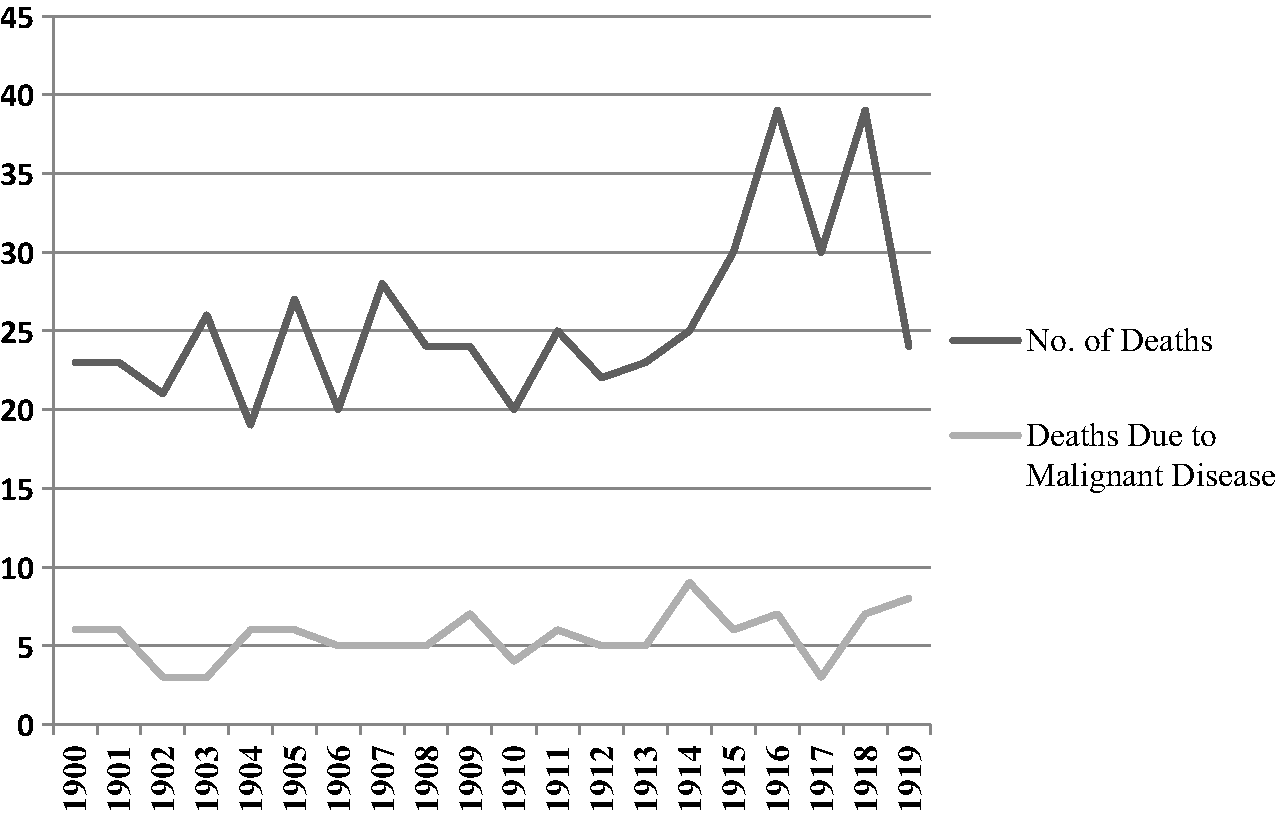
Figure 3.6 Deaths, including Malignant Disease: NHW, 1900–1919.Footnote 31
Figure 3.6 shows a peak in deaths from malignant disease at the hospital in 1914, when 36 per cent were due to cancer, yet 1903 and 1917 reveal lows of 11.5 and 10 per cent, respectively. Indeed, the same number of patients died of broncho-pneumonia in 1917 as of malignant disease. The NHW cancer patients were between 1 in 10 and just over 1 in 3 of all deaths over this 20-year period. Such statistics, because of the fluctuating numbers, do not suggest that either malignant disease was increasing or that death was inevitable for those patients who visited or who were sent on to the New by their general practitioners. Both concerns were mooted by the medical profession as preventing women from acknowledging their illness early enough. Even in the sixth edition of Tumours, Innocent and Malignant (1917), which had a preface acknowledging the ‘additions to our knowledge’, Bland-Sutton summed up the ongoing pessimism attached to the word ‘cancer’:
The disease is of very great importance on account of its insidious onset, and, in the earliest stages, painlessness; its progressive and irresistible destructiveness; the manner in which it infects lymph-glands; the extraordinary effects produced in different organs on account of the dissemination of the growth in the form of secondary nodules; the helplessness, misery, and pain it produces when fully advanced; and the inability of medical and surgical art to deal effectively with it, save in the earliest stages. Although this disease was recognised in the dawn of medicine, we not only remain ignorant of its cause, but, in many instances, the diagnosis of the malady is uncertain in the living. This is not due to supineness on the part of investigators, but to the absence of what is called ‘specific symptomatology’.Footnote 32
Against the mysterious, but omnipotent malignancy, Bland-Sutton pitted lay, but also, more troublingly, professional confusion and frailty. The early twentieth-century so-called ‘universal familiarity with “cancer”’Footnote 34 was riddled with misunderstanding, but that did not stop some from taking a risk and seeking treatment for distressing symptoms.
Mortality rates must be paired with the number of patients who sought treatment and were discovered to have a malignant disease in the first place. Although the profession worried about the many moribund patients who finally, but tardily gave in and who could not, therefore, be saved, there were others who, in similar fashion to May Beecham, sought advice as soon as their symptoms appeared. As Figure 3.7 shows, between 1900 and 1919, a patient entering the NHW with any form of cancer had an average chance of 7.7 per cent of not returning home again. The average number of deaths from all patients diagnosed as having malignant disease in the first decade of the twentieth century was 8.7 per cent; this was reduced to 6.7 per cent in the 1910s, with 1917, when only 2.6 per cent of cases died, standing out as the most effective year for patient survival. While this was not, for those leaving, a guarantee of long-term survival, or cure, that their death does not occur in the hospital itself would bode well for the New's reputation as an institution which successfully confronted and attacked one of the most feared contemporary diseases.
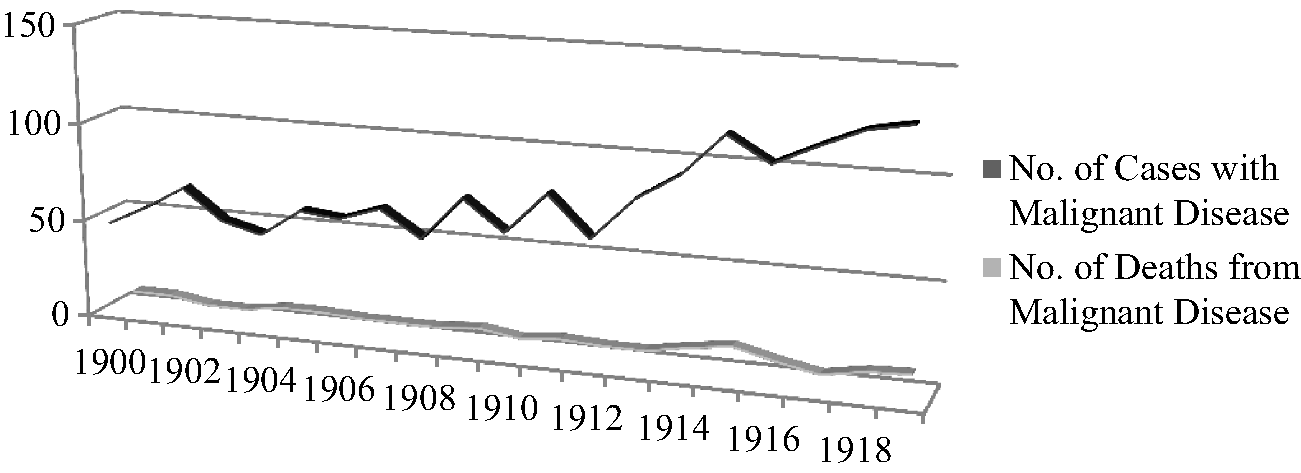
Figure 3.7 Cases and Deaths from Malignant Disease, 1900–1919.Footnote 33
The New treated a broad range of cancers in the first two decades of the twentieth century. Figure 3.8 shows the distribution of cases seen by organ, area or body part between 1900 and 1919. As was to be expected in an institution where the majority of patients were adult women, malignant disease of the female generative organs dominated. Indeed, 30 per cent of all cases were suffering from cervical cancer, 7 per cent from that of the uterine body, and 6 per cent from ovarian tumours. Breast cancer formed the second-highest number of malignant cases seen, with 22 per cent. However, in line with the hospital's general status, there were many patients diagnosed with other forms of malignancy. The numbers suffering from cancers of the alimentary system were particularly numerous. Rectal cancer cases formed 9 per cent of the total number between 1900 and 1919, becoming the third most prevalent cancerous form seen, while malignant disease of the stomach affected 4 per cent of patients. There were no colon cases at all before 1909, but these increased steadily until there were 7 in 1917. Patients diagnosed as having colon cancer formed 2 per cent of all cases, despite only being treated for the second decade of this period. This corresponded with the rise of surgical procedures relating to the colon, in which the New's surgeons were evidently keen to take a part.Footnote 36 As Figure 3.8 reveals, the NHW saw women suffering from cancers affecting most parts of the body between the face and the leg, but with a majority focused on the abdominal region.
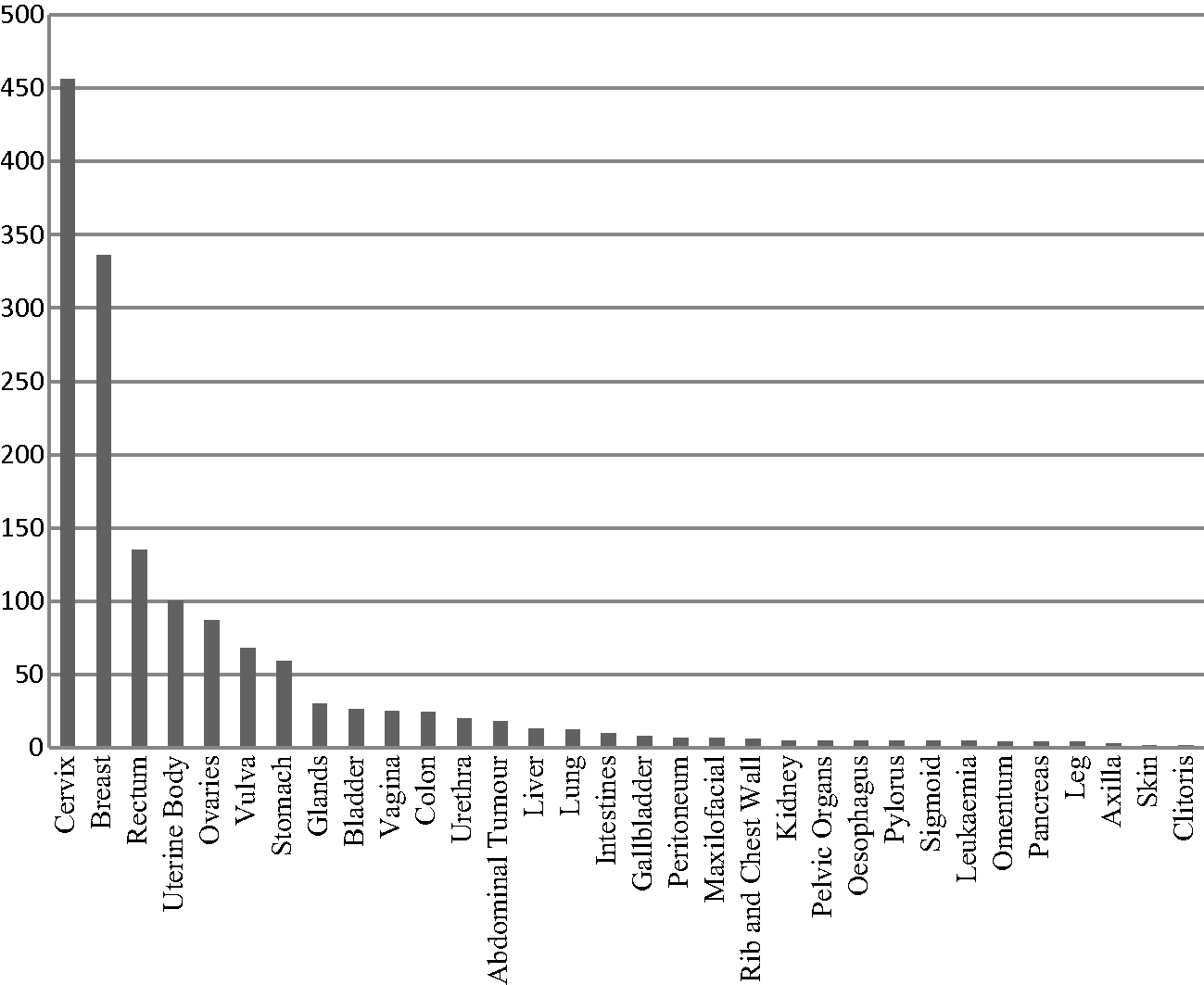
Figure 3.8 Types of Malignant Disease: NHW, 1900–1919.Footnote 35
After malignant disease of the cervix and the breast, the dominance of alimentary cancer in these statistics implied that, in some instances, women did indeed seek to consult their own sex first. According to Charles Ball, writing in 1908, rectal cancers formed 4 per cent of all large hospital cases; figures at the New suggest the hospital was witnessing more than twice this over a 20-year period.Footnote 37 Such statistics bear out Lindsay Granshaw's conjecture that fewer women attended the specialist metropolitan hospital for rectal diseases, St Mark's, because of the embarrassment attached to such conditions, instead possibly going to women's hospitals for advice.Footnote 38 According to an investigation published by the Cancer Research Laboratories of the Middlesex Hospital, based upon the hospital's own records, the nineteenth century had witnessed an increase in cancers of the alimentary tract, stomach, colon, rectum and anus in both sexes. But, cancer of this region was about seven times as common in males as in females seen at this institution between 1796 and 1904.Footnote 39 This may have been either because women suffered less from these particular types of cancerous disease or because they simply did not choose to consult professionals about their symptoms. The numbers attending the NHW who were eventually diagnosed with cancer of the rectum – 135 over 20 years – may not seem many when compared to the 446 with cancer of the cervix or 336 with malignant disease of the breast, but the fact they chose to come to the New at all suggests more confidence in women doctors than the previous chapter noted was in evidence at the RFH. The unpleasantness of the condition was described by rectal surgeon Harrison Cripps as moving from consciousness of the part, to a sensation of, if not actual, uneasiness, dull, heavy pain, before physical symptoms manifested themselves in blood-streaked faeces, possibly constipation, alternating with diarrhoea, staining of linen, and increasing emaciation. Secondary symptoms then appeared, affecting digestion, mobility due to swollen legs, and potential spread to the liver. Exhausted by pain and from anal bleeding, without treatment, the patient gradually died. The disease could end fatally in an average of two years if surgical interference was not sought.Footnote 40 It may have been this sheer physical discomfort, as well as the hard-to-disguise bowel problems and visible stains, overriding any shame or embarrassment caused by the location of the problem, which sent over 100 women to consult their own sex at the New.
Louisa Aldrich-Blake's pioneering at the NHW of what became known as the ‘Aldrich-Blake Method’ for excision of the rectum might also explain the large numbers of cases of malignant disease treated when compared with other forms of cancer. Aldrich-Blake had become Surgeon to In-Patients at the hospital in 1902, following Scharlieb's departure for the RFH, and would become Senior Surgeon in 1910.Footnote 41 In an issue of the BMJ of December 1903, Aldrich-Blake detailed ‘Abdomino-Perineal Excision of the Rectum By a New Method’, which she had first performed in February of that year at the NHW.Footnote 42 ‘Simple and efficient’, according to its originator, the Aldrich-Blake Method intended to avoid time-wasting by not performing a preliminary colotomy (intended to clear the bowels), unless essential, upon patients, because it would delay proceedings and subject the sufferer to a possible three procedures in total. Excising the disease as soon as possible was crucial to recovery. Previous operations for rectal cancer had been perineal, once the only route to remove malignant disease, but now falling out of fashion in the early twentieth century; sacral, recently pioneered by Swiss surgeon Paul Kraske, to remove growths which extended far up into the rectum; vaginal, utilised when the recto-vaginal septum was affected; and, another late nineteenth-century development, abdominal, which allowed the operator to see immediately the extent of the disease, facilitating a switch to colotomy, if the growth was too widespread, or closure, if the case was inoperable. The latter also permitted radical removal of the lymph glands or any ducts suspected of being infiltrated.Footnote 43 Aldrich-Blake's method was therefore a combination of two procedures, bringing together old and new surgical skills. She had devised the operation specifically for one patient, a 54-year-old widow, who had a freely movable, and, therefore, removable, rectal growth. After an abdominal incision, which allowed Aldrich-Blake to see the extent of the disease, the rectum and fatty tissue, containing several enlarged, and thus suspicious, glands, were held forward and now only attached by the superior and two middle haemorrhoidal vessels, which were tied and cut. Due to the shortness of ‘Mrs W's’ sigmoid, Aldrich-Blake straightened it and carried the lower part to the tip of the coccyx, where a healthy portion of rectum could stretch from the coccyx to the anus. Next, a silk stitch was passed through the peritoneum of the anterior wall of the rectum to guide the operator to the place of division when the bowel should be brought out into the peritoneum. The growth and its diseased attachments were then pushed into the lowest part of the pelvis. Mrs W's abdomen was closed and the patient moved from the Trendelenburg into the lithotrity position. An incision was made in the posterior wall, and, because of the previous movement of the diseased rectum, it was possible to draw it up carefully out of the wound, and then amputate it at the point where the silk suture, previously placed, indicated. Microscopic examination revealed adeno-carcinoma, but some of the higher glands removed were free from the disease. The patient made an uninterrupted recovery.
Aldrich-Blake's paper revealed her willingness to adopt, adapt and experiment with different methods of surgical procedure to devise her own operation. Her acknowledgment that she had since managed to save the sphincter of another patient intact, by further refining her technique, pointed to a confidence in tailoring still-novel surgery to the individual patient and their particular condition. As Sally Wilde has noted in an article on prostate operations for a later period, surgery varied from patient to patient, but also surgeon to surgeon; unlike the prescription of standardised drug treatment, surgeons modified, according to experience or level of skill.Footnote 44 Aldrich-Blake was sufficiently familiar with rectal surgery to ‘devise’ her own way of operating; one, indeed, which found its way into Ball's textbook on the rectum in a chapter on surgical ‘Cancer Treatment’ five years later.Footnote 45 As subsequent patients brought their own challenges, Aldrich-Blake, along with many other surgeons of the time, used her previous experience to adopt, adapt and modify to her satisfaction, as well as considering the patient's specific condition. The Senior Surgeon at St Mark's, Frederick Swinford Edwards, described this succinctly by noting that he was not ‘entirely wedded’ to any one method: ‘all cases should be judged on their own merits’.Footnote 46 Surgery still had enough of the art and craft about it at this point for surgeons to experiment and hone their skills.
Figures 3.9 and 3.10 show the numbers who sought medical advice for malignant disease of the rectum at the New and the precise way in which they were treated. Not every patient underwent a surgical procedure between 1900 and 1919, but the number of colotomies, coupled with the figures for excision, pointed to the majority receiving some form of relief, if not cure, via surgery. On the whole, colotomies, or the creation of an artificial outlet for faeces, were performed more frequently than excision (Figure 3.9). Given the number of cases of malignant disease, it is likely that colotomies were carried out either as preparation for the excision, a procedure which was not favoured by Aldrich-Blake unless it was strictly necessary, or as a palliative measure for cancers too advanced to be excised. In 1903, William Watson Cheyne, in his ‘Observations on the Treatment of Cancer of the Rectum’, claimed that there were really only three practical measures for dealing with the disease: to leave it alone and treat medically; to perform colotomy; or to remove the affected portion. The first two options were palliative for Watson Cheyne, ‘condemning the patient’ to die from the disease, while the third attempted to eradicate malignancy.Footnote 48 As far as the second option was concerned, Lockhart Mummery pointed out in 1908 that, while deaths from colotomies should be rare when experienced surgeons were operating, they did happen because they were often performed on those for whom it would provide a small amount of relief. For those ‘in extremis’, with an immovable growth, it could be momentarily life-saving.Footnote 49 Colotomies at the NHW over the period between 1900 and 1919 resulted in only four deaths out of a total of 93: one each in 1905, 1910, 1913 and 1915. This represented a 4.3 per cent mortality rate after the operation, with a corresponding 95.7 per cent relief for those patients requiring the procedure.
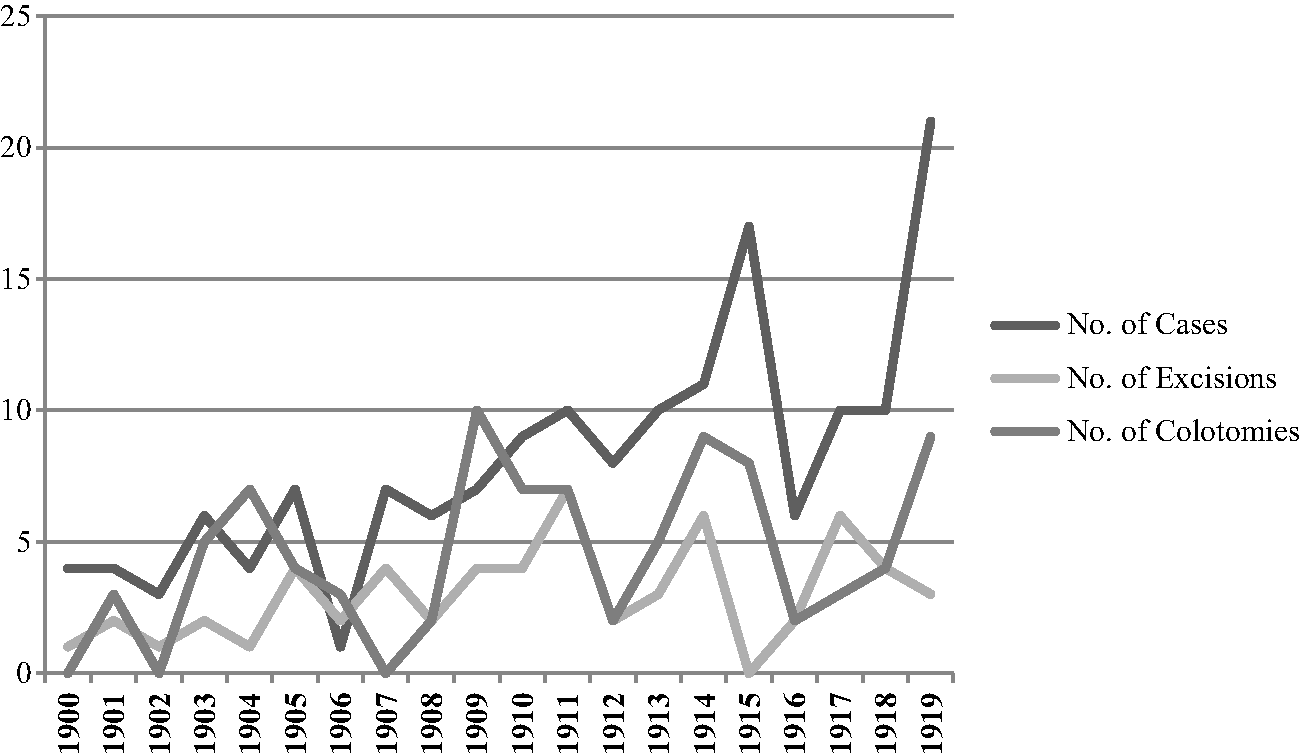
Figure 3.9 Cases of Rectal Cancer, With Surgical Procedures: NHW, 1900–1919.
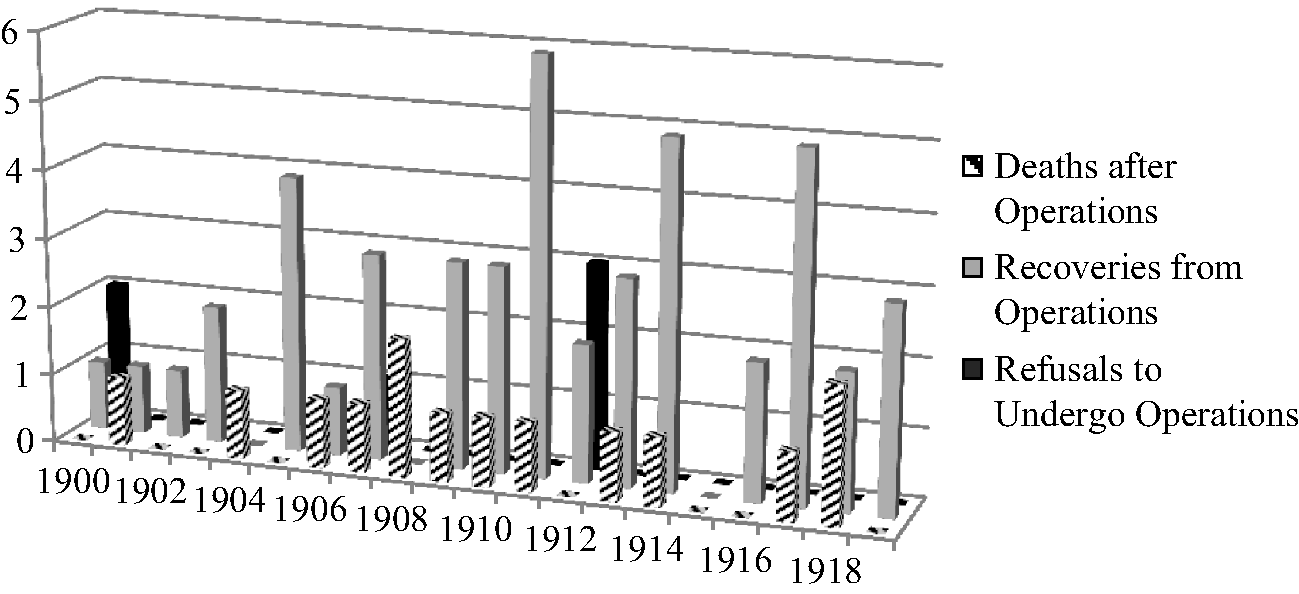
Figure 3.10 Deaths, Recoveries and Refusals in Excision for Rectal Cancer: NHW, 1900–1919.Footnote 47
Given Watson Cheyne's pessimism about the efficacy of the colotomy in providing anything other than a delaying of the inevitable, even if it did offer the patient a temporary measure to combat some of their pain and suffering, it is worth exploring the statistics for excisions performed at the NHW over the same period. Figure 3.10 shows the number operated upon for excision of the rectum out of the total number of patients seen. The final year, 1919, offers the anomalous 14.3 per cent, which depresses the average, but, across over the 20 years considered here, excision was the method of choice for, at the lowest, 25 per cent of patients, and the highest 70 per cent. On average, the procedure was carried out upon 36.8 per cent of sufferers from malignant disease of the rectum: 38.6 per cent in the first half of the period, which increased to 41.3 per cent in the 1910s. In 1903, Watson Cheyne had lamented that only around 20 per cent of patients who presented themselves for treatment were suitable for this radical surgical procedure. He noted, more hopefully, that this might be ‘somewhat increased’ in the near future with ongoing improvements in technique.Footnote 50 But a quarter of a century later, Sir William I. De C. Wheeler could still claim exasperatedly that around 70 per cent of patients were found to be suffering from inoperable cancer on admission.Footnote 51 If the situation had improved by around only 10 per cent over a 25-year period, the NHW was frequently operating upon more than twice and sometimes three times the number of cases other surgeons were considering. In 1911, for example, excisions were running at a rate of 70 per cent of patients seen; a complete reversal of the inoperable versus operable statistics cited by Wheeler nearly two decades later. Either the female patients at the New were presenting themselves earlier and were therefore more suitable to undergo excisions or the women surgeons at the hospital were taking risks and operating even when the outcome might not be certain or the disease too advanced for success.
The erratic nature of the mortality rates from excision of the rectum at the NHW pointed to this latter proposition. As Figure 3.11 reveals, deaths from this particular operation ranged from none to all. There was little consistency from year to year and vast differences could be seen with only 12 months between cases. So, for example, while 50 per cent of patients who were operated upon in 1901 died, 1900, 1902 and 1903 registered no deaths at all. Similarly, while in 1904, every case died, the year after none did. The statistics stabilised a little after 1909 for nearly a decade, when no more than a quarter of patients died from or following the procedure, but in 1918, the figure rose to 50 per cent again, although it dropped the next year to none. Over the 20 years covered here, the average death rate from excision of the rectum for malignant disease was 24.6 per cent. In 1903, Cheyne had optimistically claimed that while the mortality from cancer of the rectum ranged from 5 to 30 per cent, deaths from excision of a cancerous rectal growth should be no more than 5 to 10 per cent, due to recent improvements in procedure.Footnote 52 However, in 1911, J.W. Smith contemplated his mortality rate of 23½ per cent from a consecutive 34 cases, refusing to offer apologies for his statistics: ‘I have operated whenever it was in any way possible to remove the growth and the patient chose to run the very serious risk.’ If there was any opportunity to operate it should be advised
however bad it may appear. I have in this way done several cases pronounced inoperable by other surgeons, because in some of the worst and apparently hopeless cases the result has been excellent. I think surgeons who have had a wide experience of the operation would bear me out in this. Of course it means sacrificing statistics, for most of the fatalities have been after operations in such bad cases, but there is no greater hindrance to progress than a too careful eye on statistics.Footnote 53
Given the varying results of serious rectal surgery between 1900 and 1919, those operating at the NHW might have agreed. The chance, however slight, that recovery or at the very least relief from this debilitating condition could be achieved through surgical procedure must have been a good enough reason for those patients willing to undergo operations for cancer of the rectum over these two decades.
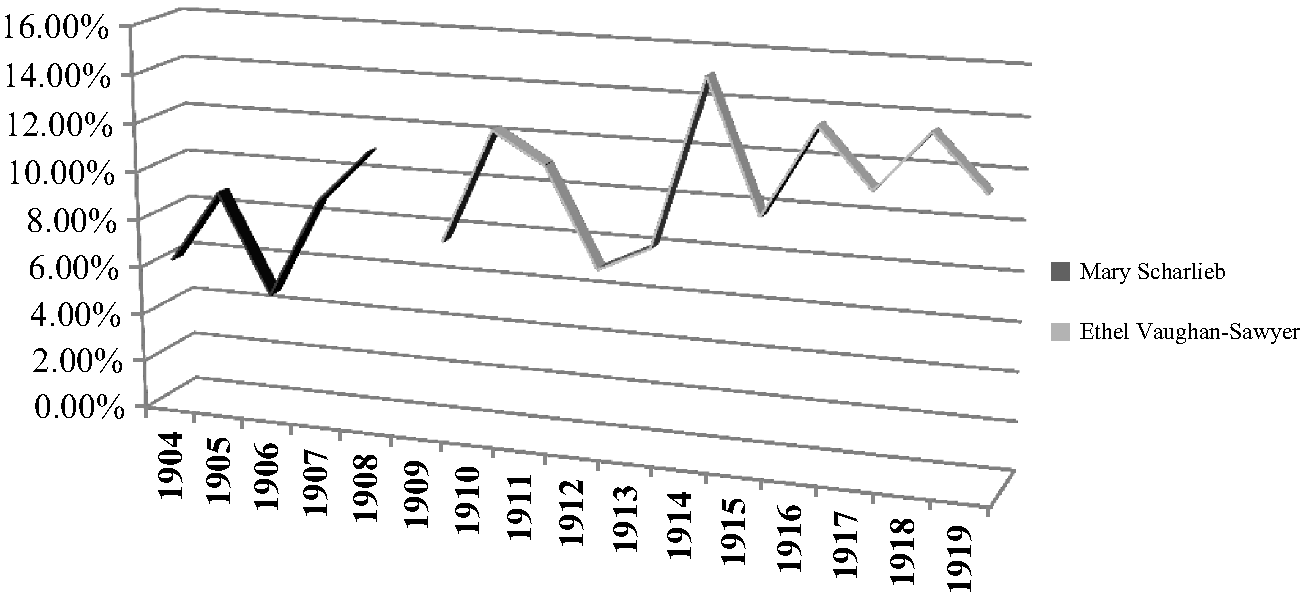
Figure 3.11 Percentage of Cancer Cases to Overall Numbers: RFH, 1904–1919.Footnote 67
Indeed, there were only six refusals to undergo excision of the rectum, and three of those occurred in one year: 1912. Additionally, there were two refusals in 1900 and one in 1907. Of the 161 patients diagnosed with rectal cancer, therefore, only 3.7 per cent would not consent to surgery. Ultimately, refusals formed just 10 per cent of those advised to undergo an operation for their condition. As Figure 3.10 shows, discharging oneself before surgery had taken place had very little to do with mortality rates. In 1912, when 50 per cent of the overall refusals occurred, not one patient died from a rectal excision. Similarly, while there was one death in 1907, there were three recoveries. In 1900, two patients refused the procedure, but the one who did take a chance recovered. The patient perception of the risk attached to the procedure had no concrete link with the number of deaths from that operation. By 1911, as Swinford Edwards made clear, for many surgeons operation was the only possible means of saving the patient: ‘All forms of treatment other than operative, whether by radium, X-rays, high frequency currents, trypsin and other digestive ferments, have I think it is generally admitted, proved unavailing, so we can confine our attention to the best means of effecting a cure by excision.’Footnote 54 Rather than focusing upon alternatives, surgery for rectal cancer, despite its riskiness and high mortality rate, gave the patient the greatest chance of survival. This was evidently how surgeons were recommending the odds to patients because, as Swinford Edwards went on to explain, the practicalities of life after extensive rectal surgery via the abdomino-perineal route, as recommended and performed by Aldrich-Blake, would surely put off many from consenting to the operation.Footnote 55 Surgery, however, was even recommended by those purveying one of the non-surgical treatments stated as unsuccessful by Swinford Edwards. The Radium Institute's reports from 1911 to 1914 became steadily bleaker when assessing prognosis following the radium treatment of rectal cancer. By 1914, indeed, for inoperable cases, while the growth might shrink enough to allow surgery to be carried out, for others ‘the amount of benefit is rarely so marked or so great as in cancer of the uterus.’Footnote 56 Such a statement, which revealed both the efficacy of the surgical procedure in this particular malignancy and radium's lack of success when directly compared with more exclusively women's diseases, could have given the female surgeon an advantage when trying to explain the options to a patient affected with cancer of the rectum. As specialist rectal hospital St Mark's discovered, after trying radium treatment out on their patients, surgery gave better hope as far as long-term prognosis was concerned.Footnote 57 At the NHW, either patient desperation, surgical confidence, which had communicated itself very effectively to patients, or a combination of the two meant that 90 per cent of those suffering from cancer of the rectum decided surgery was the correct way to relieve their illness, whatever the possible outcome.
Such reassurance that undergoing a radical surgical procedure was the most beneficial option to take was supported enthusiastically by an insistence on the importance of pathological diagnosis as a confirmation of clinical judgement and a strong belief in the follow-up system for cancer patients. Published articles by early twentieth-century female surgeons at the NHW, such as those by Mary Scharlieb, Louisa Garrett Anderson and the pathologist Kate Platt, made reference to the vital contribution pathology made to surgical scrupulousness, including the diagnosis, proof and treatment of malignant disease. Garrett Anderson and Platt's 1908 analysis of those patients who had suffered from uterine and cervical cancers emphasised the care with which microscopic sections had been examined and re-examined for their study of 264 cases between 1895 and 1907 in order to ensure that any condition described as malignant was in fact so.Footnote 58 Too often in the first two decades of the twentieth century surgeons were accused of unnecessarily removing so-called ‘growths’ without enough thought or consideration for the patient's actual circumstances. The fear surrounding cancer stoked this assumption in the public mind. Between 1904 and 1909, ‘a considerable amount of over-diagnosis’ was revealed through data gleaned from hospital statistics: 757 cases were wrongly diagnosed and treated as cancer. This could be contrasted with the 100 per cent cure rate promised through ancient and homely ‘quack’ methods such as caustics, herbs, ointments, plasters, pills, poultices and vegetable remedies, so derided by professionals and so attractive to the poor, as well as the light treatment, radio-active baths, waters and electric currents which, gaining popularity with some in the profession, stood on the boundaries of acceptability.Footnote 59 Surgeons, therefore, had much to prove to potential patients. As articles stemming from experience at the NHW illustrated, confidence in diagnosis through sound surgical judgement, supported by scientific confirmation, made surgery as accurate as it could be, and, importantly, tailored to the individual case rather than the disease itself.
As we saw in chapter 1, Scharlieb had extolled the importance of pathology in print since the 1890s. By 1910, in a debate about malignant and innocent ovarian growths, she laid out a regime which all surgeons should follow for as accurate a diagnosis as possible: a system which put the patient at the heart of the treatment. Scharlieb was shocked at the number of her own cases which had proved malignant and, comparing them with other female surgeons, including May Thorne and Ethel Vaughan-Sawyer, she discovered that her statistics were not unusual. The ‘startling proportion’ in which the growth was malignant, around one-sixth of cases for all three surgeons, led Scharlieb to label as justifiable the following three rules which should be followed with any malignancy. First, ‘that every case shall be carefully recorded; second, that in every case the specimen shall be examined by an expert pathologist; [and] third, that surgeons shall, in all instances, do their best to ascertain the subsequent history of their patients’.Footnote 60 Removal of the cancer through surgical procedure was only one part of the process, according to Scharlieb. Additionally, the more assiduously attention was paid to the exact details of each case, the more frequently specimens were examined by expert pathologists, even if they appeared innocent initially, the more easily surgeons would be able to prolong or save lives.Footnote 61 Louisa Aldrich-Blake went even further in her belief that follow-ups were essential to surgical success. Garrett Anderson and Platt made reference to a case whereby a woman was operated upon for ventral hernia, three years after a hysterectomy. When opening her up to repair the hernia, Aldrich-Blake removed her iliac glands. While the patient had not suffered any symptoms, Aldrich-Blake took precautions. A microscopic examination revealed cancer cells. While the pathological process confirmed Aldrich-Blake's suspicions, which were based upon experience and clinical assessment, it also justified the more radical procedure, performed in the interests of the patient. For Aldrich-Blake, the case further encouraged her to propose more radical surgical solutions to the usual follow-up process. It was only incidentally that deposits of malignancy had been discovered, but they had been found because of surgery for another complaint. Therefore, suggested Aldrich-Blake, why not ensure that the follow-up was a surgical one, via an exploratory laparotomy, every 18 months or two years after the initial operation? As Garrett Anderson and Platt put it, her reasoning was that ‘[t]he risk incurred from an exploratory operation is slight, and the advantage to be derived from it might be great’.Footnote 62 There was doubt at the outcome expressed in the second part of this proposal, but that may well have been enough for those patients anxious to ensure that their disease did not return.
The culture of surgery for malignant disease at the New in the first two decades of the twentieth century belies previous assessment that female surgeons were turning towards less invasive modes of treatment. If anything, the number of procedures increased, as did the seriousness and difficulty of the surgery performed. Additionally, women were not only operating on exclusively female conditions. The fact that rectal malignancy provided the third most prevalent form of cancer seen at the NHW shows that, in contrast to the previous chapter where women had not specifically chosen their own sex as general practitioners, regardless of the embarrassing or ‘female’ nature of their complaint, women with problems in this area did indeed seek the advice of their own sex. Moreover, they also showed willingness to undergo uncomfortable surgery, with only 10 per cent refusing operations over a 20-year period for cancer of the rectum. These are figures which compared very favourably to the despair experienced by other surgeons who tried and failed to encourage large numbers of resisting patients to undergo potentially life-saving surgery. The suspicions and superstitions which surrounded cancer undoubtedly led many simply to go home in pain, eventually to die. That so many did the opposite at the New illustrated that if the cause was serious enough, trust could be established between patient and surgeon because, as Sally Wilde has noted, of the possibility of cure.Footnote 63 This was achieved in spite of the ongoing public fear of surgery and, especially, the efficacy of procedures to remove malignancies. Although discussing benign growths, NHW surgeon Florence Nightingale Boyd commented that she thought ‘it unjustifiable that women should be allowed to suffer for years […] without being afforded the relief that surgery could give’.Footnote 64 This was certainly the policy at the New regarding malignancy. The promise of relief, however temporary, for many outweighed the substantial risks. Even the high mortality rates for the excision of the rectum, which, as the statistics showed, sometimes ran at 100 per cent, did not prevent the majority from undergoing the procedure. Women surgeons at the NHW were prepared to take those risks, but so, importantly, were their patients.
The Patient Response to Cancer Diagnosis and Treatment: RFH, 1903–1919
The RFH's wealth of case notes allow the historian to examine more closely those patients who were diagnosed with malignant disease at this institution, the ways in which they were treated, their reactions to their condition, and the trajectory of their illness over time, which crucially takes into consideration the question of cures or ongoing procedures for recurrence. Such detailed accounts also permit an insight into precisely how and where treatment was administered to patients, as well as the reasons behind a surgeon's decision to operate or not, or, indeed, a patient's choice whether to follow medical or surgical recommendations. The notes contain important debate between patient and surgeon, as well as, in the hospital's well-established system of staff consultation over tricky cases, between surgeons. Often, the weighing up of physical evidence meant there were delays in dispensing treatment or performing surgery, but this period of watching, learning and eventually deciding what to do for the best revealed that decisions were not made lightly and risk was assessed both by surgeon and patient. Unlike the NHW's team, the RFH surgeons, Mary Scharlieb and Ethel Vaughan-Sawyer, focused primarily on the diseases of women, situated as they were in the specialist gynaecological department of a general hospital. Therefore, the majority of their cases were abdominal and, most frequently, of the female generative organs. Their case notes can be used to explore the impact of the early twentieth-century concern about cancer on the prospective patient and to assess whether or not the profession's greatest fears about working-class women's reluctance to consult medical advice were borne out in actuality or whether the situation was more complicated than had been assumed. They also reveal many of the ways in which surgeons tried to keep track of their cancer patients, through a variety of methods dedicated to the follow-up of often hard to locate working-class women, for whom moving frequently because of changes in financial or personal circumstances was second nature.Footnote 65 This section will also examine what impact newer, less invasive treatment – such as X-ray applications and the use of radium – had upon female surgeons at the RFH and how it affected the ways in which they operated.
As noted in the first section of this chapter, in print Scharlieb expressed alarm at the number of malignant as opposed to benign cases she had encountered. Indeed, as Figure 3.11 shows, cancer formed no less than 5 per cent and often more than 10 per cent of the conditions treated by the two female surgeons. Across the period covered by this chapter, an average of 8.3 per cent of Scharlieb's patients suffered from malignant disease between 1903 and 1909, while Vaughan-Sawyer's average caseload was even higher: between 1904 and 1919, 10.9 per cent were diagnosed with or confirmed to have cancer. In 1915, cancer cases peaked at 15 per cent of all patients seen by Vaughan-Sawyer. While both Scharlieb and Vaughan-Sawyer were designated ‘Physicians’ for the Diseases of Women by hospital literature, the vast majority of their cases were surgical, from minor dilatation and curetting of the uterus to major, lengthy and risky procedures for carcinoma. Weisz has labelled gynaecology at this point ‘a rather wild and woolly specialist group’, a ‘protean’ and ‘enormous field of activity’.Footnote 66 As Cuthbert Lockyer explained in an article written in 1914, the ‘life history’ of the specialism proved fascinating. The gynaecologist had started off as a physician, before abdominal surgery had been thought possible, then ‘acquired the skill of a surgeon as soon as surgical intervention was required of him for proper fulfilment of his duties’. This ‘very adaptable person’Footnote 68 had become a surgeon, even if this was not in name. Vaughan-Sawyer was only listed as ‘Gynaecologist’ and not ‘Physician for the Diseases of Women’ in 1919, despite carrying out the role for the past decade and a half.Footnote 69 While the hospital may have been slow to recognise developing specialties, this particular ‘Physician’ had been a surgeon from the beginning of the twentieth century.
Malignant disease was, therefore, all too familiar to Scharlieb and Vaughan-Sawyer, who both encountered numerous cancer patients over the years covered by this chapter (see Figures 3.12 and 3.13). It is worth exploring in more detail the kinds of cancers seen by the two women between 1904 and 1919 in order to see which ‘Diseases of Women’ composed their caseload.Footnote 70 The two graphs show similarities, but also a number of key differences between the cases treated by the two women surgeons of the RFH's Gynaecological Department. Firstly, it is clear that cervical cancer was the most prevalent form; indeed, it is the only malignant disease seen every single year between 1904 and 1919. This, of course, tallies with the contemporary fears over the mortality rates from cancer of the cervix, as well as the assumption, as William Japp Sinclair put it in 1902, that the disease ‘occurs almost exclusively among the poor, the chronically overworked and underfed, among women, poor, prolific, harassed, worried, drained by lactation, reposeless’.Footnote 71 Even though, as explored in the previous chapter, not every patient at the RFH was poverty-stricken, this was the class of sick poor the hospital had wanted and aimed to treat since its foundation in 1838. The fact that cervical cancer dominated admissions indicated either that this was the disease which most affected the female population, or that the majority who sought hospital treatment were women suffering from this malignancy. Secondly, and contrary to early twentieth-century concerns about the increase in cancer, there was no apparent upward trend in the numbers admitted to the RFH. Indeed, the patients under Vaughan-Sawyer's care in 1919 were no more than 1911, and not as many as 1913. While she saw three patients in 1912, Scharlieb saw more than twice as many in 1905. Although we do need to bear in mind that both surgeons had access to only 12 or 13 beds in the hospital during this period, the statistics indicate that, because of the severity of their condition, cancer patients would be more likely than those suffering from comparatively minor gynaecological complaints to spend extended time on the wards, if they decided to undergo treatment. To cite only one example, Florence Parfrement, whose uterus was anteflexed, was sent home in September 1905 to be treated because her bed was needed for a more serious case.Footnote 72 Finally, both caseloads revealed a number of recurrences, reflecting contemporary pessimism about the efficacy of cancer treatment and suggesting the limitations of surgical procedure in some instances, something which will be returned to later in the chapter.
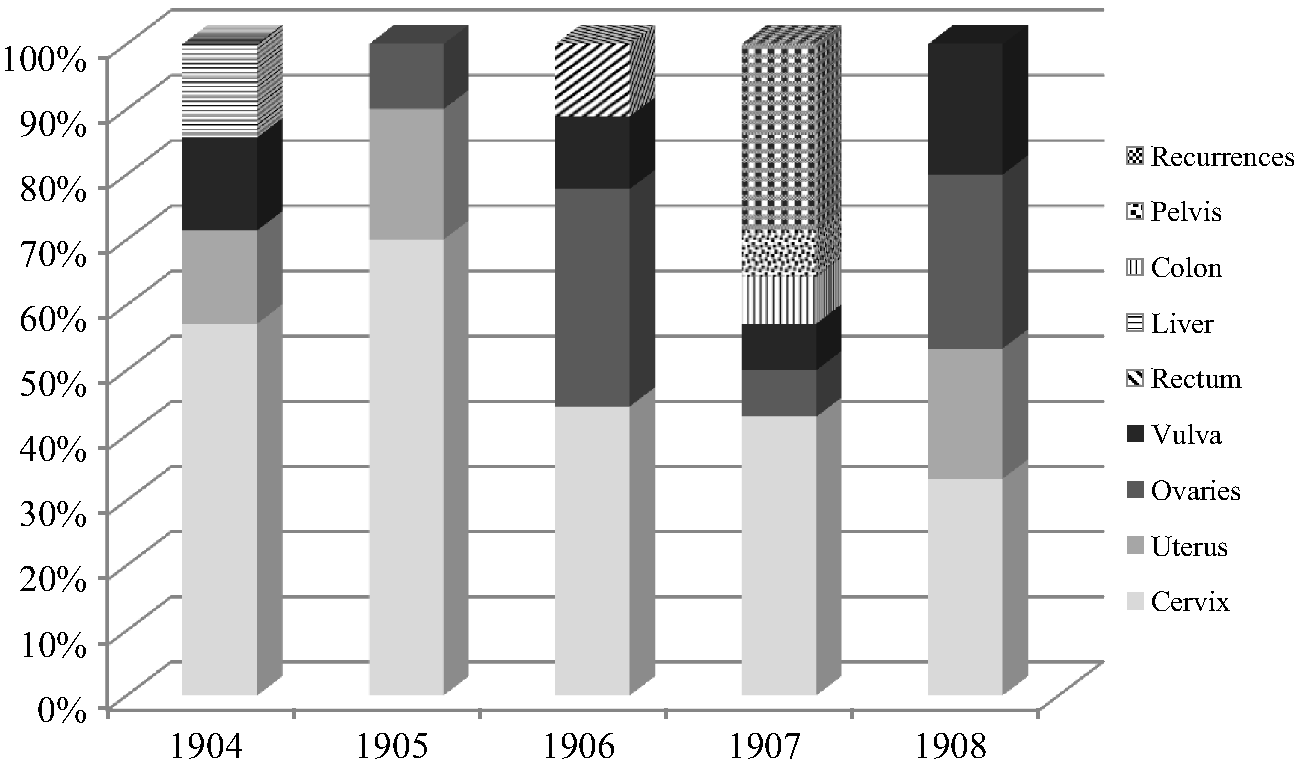
Figure 3.12 Scharlieb's Cancer Cases: RFH, 1904–1908.
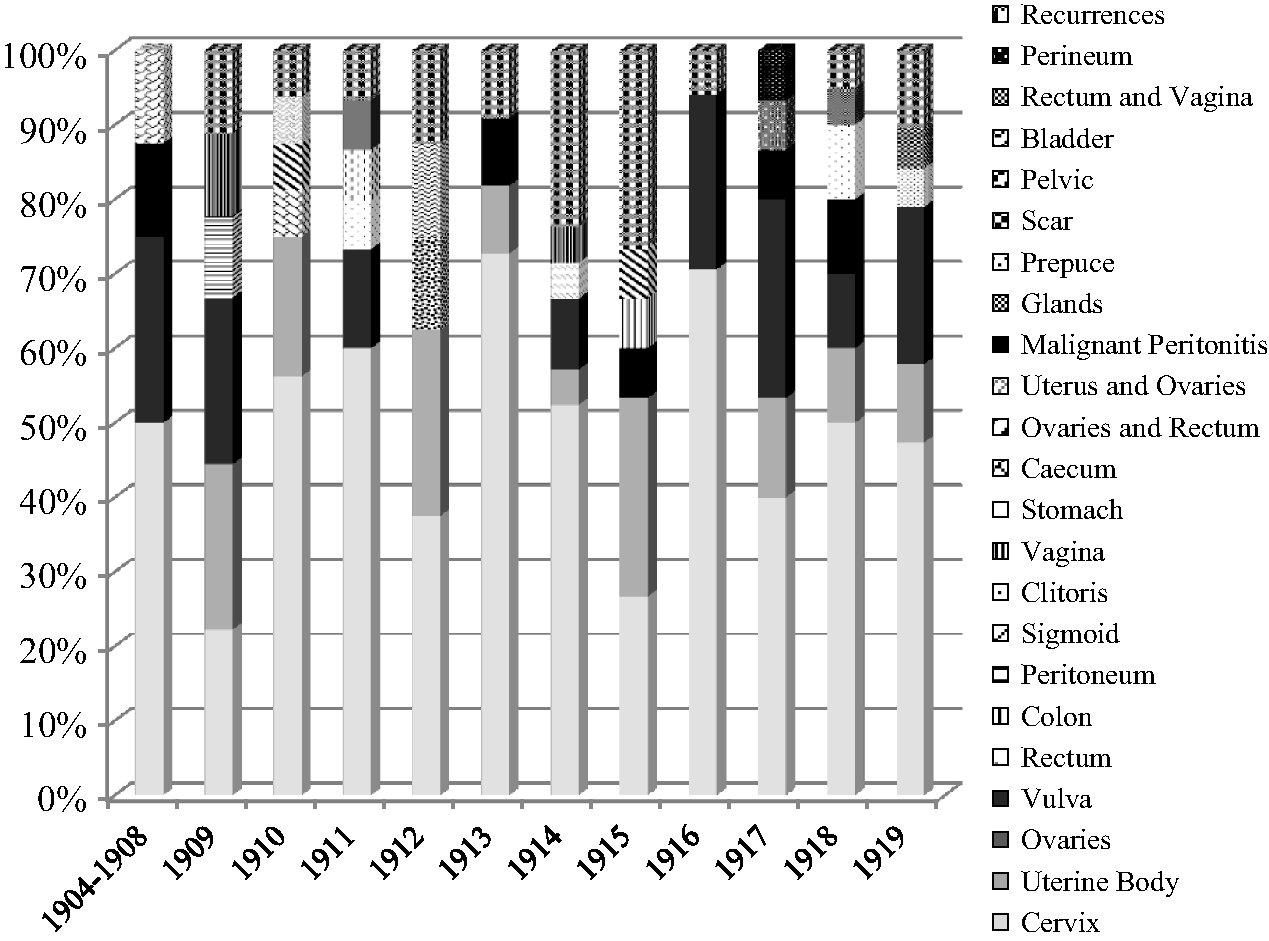
Figure 3.13 Vaughan-Sawyer's Cancer Cases: RFH, 1904–1919.
The differences between the two surgeons’ patients was also apparent from the variety of cancer cases which were treated by Vaughan-Sawyer when she took charge of the Gynaecological Department from 1909 onwards. Scharlieb saw eight different types of cancer, whereas Vaughan-Sawyer treated almost three times as many forms of malignant disease, with 22 affected areas seen over 15 years. This could be because patients were more willing to seek medical and surgical assistance in the 1910s or that public awareness of cancer was increasing. Similarly, if lay interest had been awoken by scaremongering about malignant disease, it could be that general practitioners were more likely to examine their patients and to send them on for specialist advice when cancer was suspected. According to Herbert Spencer, the ‘unfortunate state of things’ was a combination of patient ignorance regarding suspicious symptoms and the general practitioners’ delay in examining those with early signs of malignant disease.Footnote 73 Conversely, Vaughan-Sawyer's willingness to take on patients, as well as to operate upon them, even if the case was hopeless, indicated a growing confidence in attempting surgical approaches to cancer. Whereas frequently in the early part of the period covered here, patients were sent home to die without further treatment, the 1910s at the RFH witnessed an increasing desire to do something surgically for those suffering from malignancy. Even if that was a palliative procedure, it became apparent that, in Vaughan-Sawyer's case, as in those of the female surgeons at the NHW, surgery was the answer to the problem of relieving patients, either of their disease, if it was curable, or a short increase in their lives, if it was not.
To explore this latter point, it is necessary to examine the operability figures of the RFH surgeons. This requires assessing whether or not the patient underwent surgery for their condition against the overall number of patients seen. Operability was a particular bone of contention among gynaecological surgeons in the early twentieth century for a number of reasons. Primarily, the concern was that some were offering miraculous success rates due to their careful selection, which was not always acknowledged in print, of patients likely to survive the operation and beyond. Therefore, they either turned away those who could have been saved if they had seen a surgeon more willing to risk their reputation or less promising patients were simply excluded from the statistics. Japp Sinclair commented in 1902 that at the Christie Cancer Hospital in Manchester ‘operable cases were seldom seen’, they stood at 22 per cent over a decade in the Southern Hospital, and 18 per cent in the Glasgow Western Infirmary, but developments in Germany had indicated that over half of patients could be operated upon and potentially saved.Footnote 74 Two years later, Bland-Sutton suggested that his own hospital experience showed that only 5 per cent of 100 consecutive patients suffering from cancer of the cervix were ‘favourable subjects for the purposes of operation’.Footnote 75 He recommended his ‘too exclusive’, selection as a defence against the potential discrediting of hysterectomy for malignant disease by the sentimental, superstitious and erroneous. Others, including Middlesex Hospital surgeons Comyns Berkeley and Victor Bonney, believed the opposite, claiming in 1913 that: ‘[i]n estimating an operability rate it is absolutely necessary that it should include every case attending the in and out patient departments, that is, that the patients should not have undergone any previous select’.Footnote 76 As Berkeley had noted in 1909:
We are all agreed that if only early cases are chosen the percentage of cures will be much greater and that of operability much less. Still it is quite evident that most operators have not limited themselves in this way, with the result that many women have been cured whose chances from a clinical examination might have been thought to be hopeless.Footnote 77
For Berkeley, every woman, unless she was incapable of withstanding the operation, should be given a chance, even if the case appeared hopeless upon initial examination. Surgery could provide the best means for prolonging the lives even of those women whose condition was advanced. By taking the risk and increasing the operability rate, cures could be effected.
Surgery for malignant disease in the RFH's Gynaecological Department showed a similar increase to that of the NHW. From not a single operable case in 1904, Scharlieb operated on two-thirds of her patients by 1908, the last full year before her retirement from the RFH (see Figure 3.14). In contrast, Vaughan-Sawyer's cases showed more consistency from the start, as she operated upon 87.5 per cent of her patients between 1904 and 1908. The fewest number of operation cases could be found in 1912 and 1914, where only 50 per cent underwent surgical treatment; in the former year, however, the other 50 per cent were inoperable cases. Of the total number of cancer patients seen by Vaughan-Sawyer between 1904 and 1919, she operated upon an average of 67.4 per cent of them (see Figure 3.15). Although, in 1906 and 1908, two-thirds of Scharlieb's cancer cases underwent a surgical procedure, her average was less than Vaughan-Sawyer, at 41.2 per cent of the total between 1904 and 1908. For the period as a whole, the average ‘operability’ for both surgeons was 54.3 per cent of in-patients. Similarly, death rates after operation were very favourable. Scharlieb lost only three patients in the last two years at the RFH, while of Vaughan-Sawyer's malignant cases, only 16 did not recover from their surgery over the 15-year period covered by her extant patient notes. For the former, this was an initial success rate of 88.5 per cent; the latter 86.3 per cent. Of the refusals to undergo operative treatment, two of the three Vaughan-Sawyer patients who discharged themselves in 1910 and in 1914 were operable, while one, whose cancer was inoperable, refused all further treatment in 1915. Similarly, of Scharlieb's premature discharges, only one of the seven was offered an operation which might not be successful. The other cases were considered to have consulted surgical advice early enough or their condition was sufficiently localised to admit of removal. When these patients were included in the total number seen versus the number undergoing surgery, the operability rate increased to 60.4 per cent for Scharlieb and 69.2 per cent for Vaughan-Sawyer.
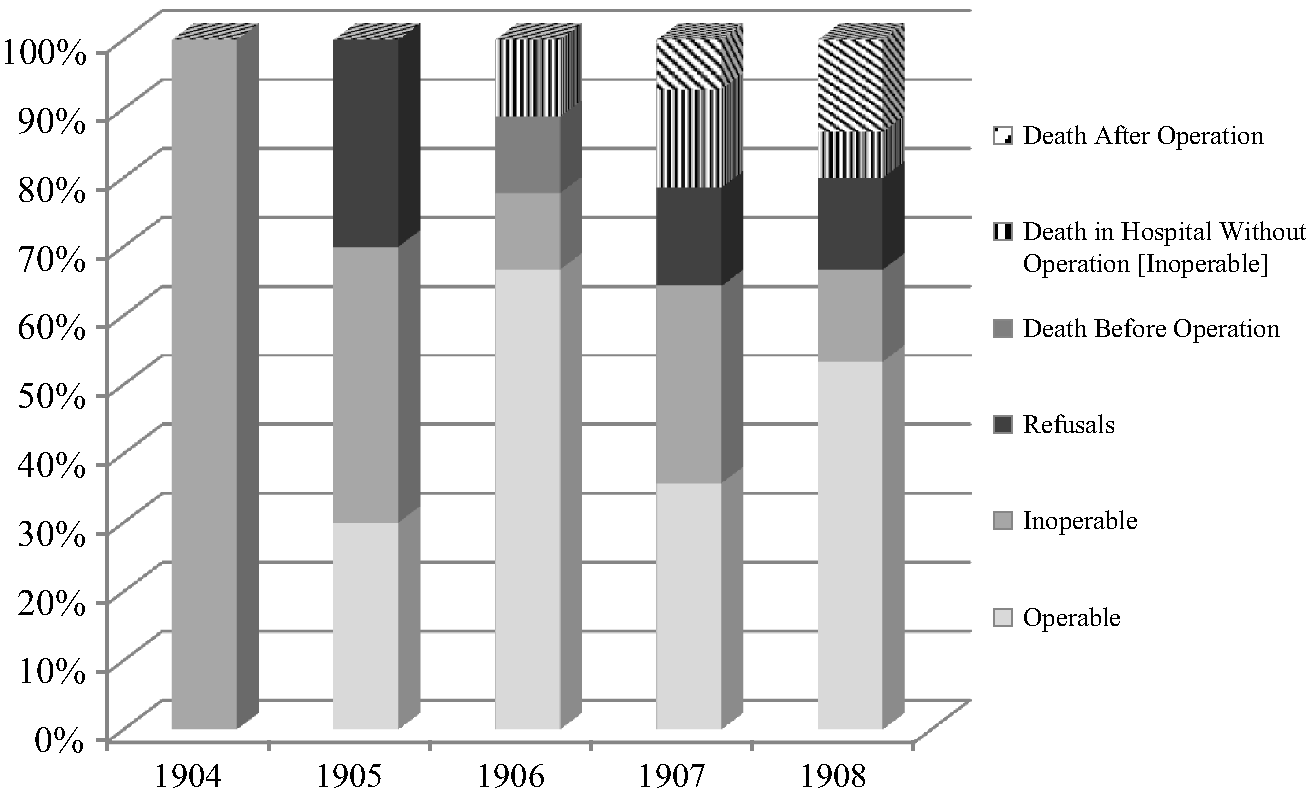
Figure 3.14 Scharlieb's Operability: RFH, 1904–1908.
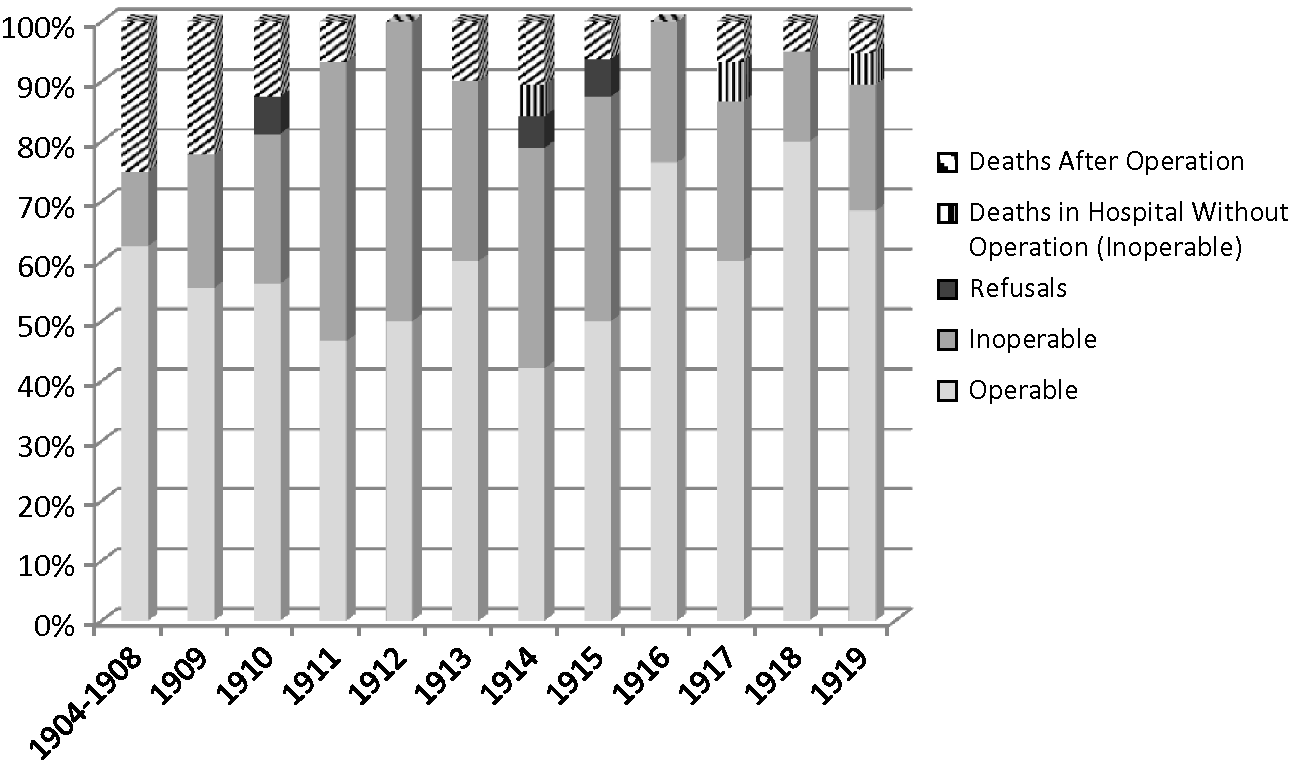
Figure 3.15 Vaughan-Sawyer's Operability: RFH, 1904–1919.
These statistics compared very favourably with the more depressing forecast of other gynaecologists, shown above. Regardless of the cancer's extent, the RFH's female surgeons were willing to attempt operations, rather than send patients home to die. Furthermore, even some of those deemed ‘inoperable’ were made more comfortable through palliative care given, at times, through surgical procedure. This approach included curetting and cauterisation of the growth under anaesthesia, acetone treatment, and, from 1909, although later intermittently offered due to wartime shortages, some of those for whom nothing could be done received X-ray exposures or insertions of radium to ease their pain.Footnote 78 In only one case was radium treatment given to an ‘operable’ patient. In March 1914, 48-year-old housewife, Gertrude E. Benwell, who was suffering from adeno-carcinoma of the cervix, had the tumour cauterised, treated with acetone, and then underwent a series of radium treatments. By the end of April, the growth had shrunk enough for her to be found to have an ‘operable’ condition. However, while being operated upon, it was discovered that she had a new growth near the orifice of her left ureter, even though her uterus was successfully removed. This nodule had to be left in situ.Footnote 79 Mrs Benwell did not return to Vaughan-Sawyer, however, so there was a possibility of a ‘cure’, at least in terms of a five-year survival. While radium treatment assisted the surgeon here, this was the only instance in the case notes of either Scharlieb or Vaughan-Sawyer where it was utilised as a means to facilitate surgery, rather than a final option when the patient was beyond any surgical assistance.
Scraping and cauterising, however, were used both for operable and inoperable patients, and became increasingly frequent in the 1910s. The removal of obvious parts of growth allowed it to be analysed pathologically, in order to support the surgeon's diagnosis. It also reduced the levels of pain experienced by the patient, as well as ensuring the extent of the cancerous area was more perceptible and, therefore, accessible to the operator. Acetone treatment in the 1910s was enthusiastically embraced by the Gynaecological Department to cleanse and treat the affected region after cauterisation. In December 1911, its use for inoperable cancer was described through Gellhorn's description of his method, which had originally been published in the Zentralblatt für Gynaekologie of the same year. After scraping as much of the disease away as possible under anaesthesia, induction was halted, and a speculum inserted into the vagina and further into the crater remaining after removal of the growth. Two or three tablespoons of acetone were then poured into the speculum. After ten minutes, the clotted blood was washed away and new acetone was introduced: this was left for twenty minutes. Then the patient was removed from an exaggerated lithotrity position and any remaining acetone was left to drain away through the speculum. A gauze plug was inserted and treatment continued at intervals. Gellhorn claimed that the patient's health and condition could be generally improved, as well as in many cases where it was possible to prolong life. It was painless, he noted, and could even be carried out by a general practitioner.Footnote 80 What patients felt about treatments such as acetone and radium applications, including their ability to relieve suffering, will be explored later in this chapter. Gellhorn's suggestion about handing back responsibilities to the patient's own doctor was also interesting, especially in the light of many gynaecologists’ dismay at the generalist's ignorance about cancer and its treatment. By returning the inoperable patient to their local practitioner, lessons might be learned. The doctor, who had perhaps not diagnosed the condition in the first place, or had not acted quickly enough in seeking specialist advice, would be compelled to witness their patient's decline. As they would be able only to care palliatively for them, the stark reality of what could be a slow and painful death might prompt greater alertness to signs and symptoms, as well as the necessity of thorough patient examination in the future.
By the 1910s, far from abandoning surgical procedures, Vaughan-Sawyer was embracing the more radical Wertheim's operation for cancer of the cervix, along with her contemporaries at other metropolitan female-run hospitals such as the NHW and the SLHW. Wertheim's method divided British and European gynaecologists, as both Moscucci and Löwy have explored. The latter has labelled the procedure ‘daring’ and ‘desperate’.Footnote 81 In 1911, Amand Routh, president of the Obstetric Section of the Royal Society of Medicine, expressed doubt about the wisdom of such ‘heroic operations’. Routh criticised the extremity of contemporary gynaecological surgery, looking forward to a time when treatment could be other than operative and condemning his colleagues recommending surgery because it was the ‘easiest way’ to deal with a patient.Footnote 82 He went on to criticise the use of Wertheim's procedure when the case was very advanced or very recent and feared that the mortality rates did not justify the risk taken both by surgeon and by patient. Briefly, as described by the man himself to a fascinated British audience at the 1905 BMA Annual Meeting held in Leicester, Wertheim had developed his approach seven years previously. While the uterus had been removed formerly through the vaginal route, Wertheim favoured the abdominal option, which allowed the performance of a hysterectomy and the additional removal of surrounding and potentially infected cellular tissue and lymphatic glands. He had adopted and adapted the procedures of others, but with the addition of a vaginal clamp, which would come to bear his name, in order to isolate the cancerous cervix.Footnote 83 His justification was that such a radical extirpation decreased the risk of recurrence, allowing 60 to 70 per cent of cases to be ‘cured’ five years after operation. Most importantly, it permitted those who ‘were otherwise irretrievably doomed’, having sought advice too late, to be relieved, however dangerous the procedure might be.Footnote 84 For detractors, the mortality rate was excessive; even if women survived the operation, death from shock was far too familiar to those who had tried and failed to save their patients. The procedure, at first taking over two hours and only reducing in length with practise, was physically demanding for the operator and required great skill in careful dissection around the bladder and ureters. While Wertheim felt he was offering renewed hope to those ‘shut out from life’, turned away by other surgeons as incurable, others saw fashionable, but ‘homicidal vivisections’, cruel experimentation upon dying women.Footnote 85
As both Moscucci and Löwy have charted fully the history of Wertheim's method of operating for cancer of the cervix, I will not do so further here. My interest lies in the adoption of this technique by women surgeons such as Vaughan-Sawyer precisely at the time when Moscucci and Löwy have noted the transition to less invasive procedures and when contemporaries such as Routh were recommending that gynaecologists consider becoming less surgical in their approach to their patients. At the BMA meeting in which Wertheim explained his procedure, Scharlieb commented that abdominal hysterectomy for cancer was not usual in Britain, but she made a point of noting that she had been very much in the minority when advocating this procedure in Oxford just one year earlier. The vaginal route was easier and quicker, but the abdominal was also safe and it prevented any possibility of the recurrence of the disease, as the whole was removed.Footnote 86 Of 17 cases of abdominal hysterectomy for cancer, she reported, four were free from recurrence after between two and four years; four had suffered a recurrence (one from cerebral disease), one had died on the day of operation, while the other eight had not been heard of since.Footnote 87 Scharlieb had achieved a 23.4 per cent freedom from recurrence as far as those from whom she had heard were concerned, but when the others were added, who had again been diagnosed with cancer, the survival rate beyond ten months was just over 47 per cent. This was clearly the sort of prolongation of life which detractors of the newer methods of abdominal extirpation claimed was torture and supporters viewed as relief. Indeed, as Garrett Anderson and Platt made clear in 1908, women surgeons at the NHW had been carrying out hysterectomies via the abdominal route since 1901, pioneering a method which became routine at this institution a year later. When they compared the results for vaginal hysterectomy with that of the abdominal method, the statistics were enlightening. Twenty-nine patients had the former operation, with only one survival seven years after operation; two had survived for two years, the rest had a recurrence and died soon after, or had not been found. Abdominal hysterectomies provided better results: 26 patients were living and healthy between 18 months and four years after their operation; a further 11 had remained free from cancer for a year and six within three and a half years, while 15 could not be contacted.Footnote 88 Vaginal hysterectomy had an extremely low success rate of 3.5 per cent, while 44.8 per cent of abdominal patients had survived for more than 18 months without recurrence. When recurrence figures were added, 74.1 per cent of the total number had been given an extra year of freedom from the disease. Although nearly 30 per cent of the ‘cure’ was temporary, the survival rate was far better than either the vaginal option or the depressing statistics of those who would not adopt the riskier methods nor operate on the more advanced cases. To return to the 1904 BMA meeting, where both Boyd of the NHW and Scharlieb of the RFH advocated abdominal hysterectomy for cancer, their optimism was countered by another delegate, Murdoch Cameron, Physician for the Diseases of Women at Glasgow's Western Infirmary, who simply noted that in his experience the great majority of cancer cases had advanced too far for operation.Footnote 89 Unlike many of their more pessimistic contemporaries, the RFH's women surgeons were willing to try out and adopt the latest methods, even when others would give up their patients as lost.
Ideally, of course, operability should be based upon the fundamental question: what can be gained through surgery for this patient? By focusing on the benefit, even if it was but a brief respite from malignancy, any procedure could be justified, both to the patient and to the surgeon themselves. British adopters of the Wertheim method recommended the procedure in precisely this way. In 1913, Berkeley and Bonney wrote an article which focused on the ‘life-prolonging effects’ of radical operations for cancer of the cervix.Footnote 90 They explained how they had adapted Wertheim's procedure in order to remove systematically all the glands in the parametric tissue, obturator fossa and the iliac vessels, regardless of whether or not they were enlarged. While this extension added not only to the risk from immediate shock but also the possibility of a more complicated convalescence, their experimentation with technique was both to improve results and allow them to operate on the most advanced cases, who would be considered inoperable by those who only removed the primary growth itself. Berkeley and Bonney's risk-taking, therefore, benefitted surgical advancement as well as the patient herself. By defending the patient's interests, the adopters and adapters of the Wertheim technique could claim that, whatever the cost, they were simply trying to save a greater number in the long run. Even the ‘inoperable’ could be given a more dignified, less painful death. Without the removal of tissues infected by malignancy, many women would suffer terribly, as the ‘great agony’ caused by the spread of the disease led to an end characterised by headache, nausea and vomiting. The cruelty, according to supporters of the radical solution to cancer of the cervix, was actually not to operate in this way. As Berkeley made clear, their procedure freed the patient from the ‘foul discharge’ of the disease, and, in the majority of cases, the end was more ‘peaceful’. ‘In some of our own cases’, he noted with pride, we ‘have had letters from relatives particularly mentioning the absence of pain and distress right up to the end’.Footnote 91 Malignant disease of the cervix was horrendous enough for the patient without prolonging her agony by refusing to carry out a more dangerous, difficult procedure for fear of denting one's statistics. For Berkeley, no one ‘worthy of the name of surgeon’Footnote 92 should be unwilling to help afflicted women.
Female surgeons were similarly inclined to assist their own sex through the performance of radical procedures such as Wertheim's for malignant disease. From early defences of abdominal methods by Boyd and Scharlieb in 1904, to the published statistics of Garrett Anderson and Platt and Vaughan-Sawyer's ‘meticulously careful’ and ‘particularly successful’ adoption of Wertheim's at the RFH, British women turned again and again to radical surgery to cure their patients.Footnote 93 The 1910s were supposed to have seen a turn away from invasive procedures for cancer, and yet 1918 was the first year where the NHW distinguished Wertheim's from abdominal hysterectomy, and 25 of them were performed.Footnote 94 There were 44 patients in the hospital that year for cancer of the cervix; 14 of them were ‘unrelieved’, so nearly every ‘operable’ patient underwent a Wertheim. The South London Hospital for Women, which only opened its permanent in-patient department in 1916, went from carrying out 2 Wertheim operations that year from the 5 cervical cancer cases it took in, to 6 in 1917 and 1918, from 13 and 14 patients respectively. By contrast, the SLHW surgeons only performed one vaginal hysterectomy each year between 1917 and 1918.Footnote 95 None of the patients undergoing the Wertheim procedure died at either hospital during these years. Although, as we have seen, Wertheim first introduced his method formally to Britain in 1905, British female surgeons at the NHW and the RFH had keenly embraced the abdominal route since the beginning of the century and they continued to take the riskier, more difficult option when Wertheim's procedure began to dominate their surgical treatment of cancer of the cervix.
At the RFH, Vaughan-Sawyer began carrying out Wertheim's operation at the end of 1910, after having performed abdominal hysterectomies for cancer of the cervix since at least 1904.Footnote 97 Forty-five-year-old Nellie Brown, a widowed housekeeper, was the first patient actively noted as undergoing a ‘Wertheim’.Footnote 98 Over the nine years covered by the extant patient records, Vaughan-Sawyer went from performing Wertheim's on 50 per cent of her operable cancer patients between 1911 and 1912, to 80 per cent in 1913 and 85.7 per cent in 1914. From this point, as Figure 3.16 reveals, Vaughan-Sawyer carried out the procedure on every patient in the years 1915, 1917 and 1919. Overall, between 1911 and 1919, an average of 79.8 per cent of Vaughan-Sawyer's patients with operable cancer of the cervix underwent a Wertheim or a modified form of the operation based on their individual condition. In the last five years of extant notes, this average rose to 90.6 per cent. During the 1910s, therefore, Vaughan-Sawyer, along with her colleagues at the NHW and the SLHW, was not simply performing these ‘heroic’ operations. They had actually become the procedure of choice for almost all patients with varying stages of cancer of the cervix. In similar fashion to Wertheim himself, as well as Bonney and Berkeley, Vaughan-Sawyer wanted her patients to be given a chance of survival. When considering what treatment to give 66-year-old factory worker Emma Knight in 1913, Vaughan-Sawyer strongly recommended Wertheim's because it would mean that her condition was much less likely to recur. Mrs Knight would be given a ‘chance’ through the more radical operation. In spite of bronchitis and emphysema, conditions which might prevent successful anaesthetisation or even recovery from induction, Vaughan-Sawyer decided to wait 25 days before operating, to allow her patient to regain her health. The pleasure in the success of the patient's recovery was evident in her notes, where remarks about Mrs Knight's ‘splendid pelvis’ post-operation and the rare confidence in the ‘cure’ added to the result of the case, showed how the risk taken was replaced by relief in the outcome.Footnote 99 As this was Emma Knight's only recorded RFH stay, then it was possible that she was indeed cured by the decision to operate in a more invasive – and, because of her age and condition, doubly risky – manner.
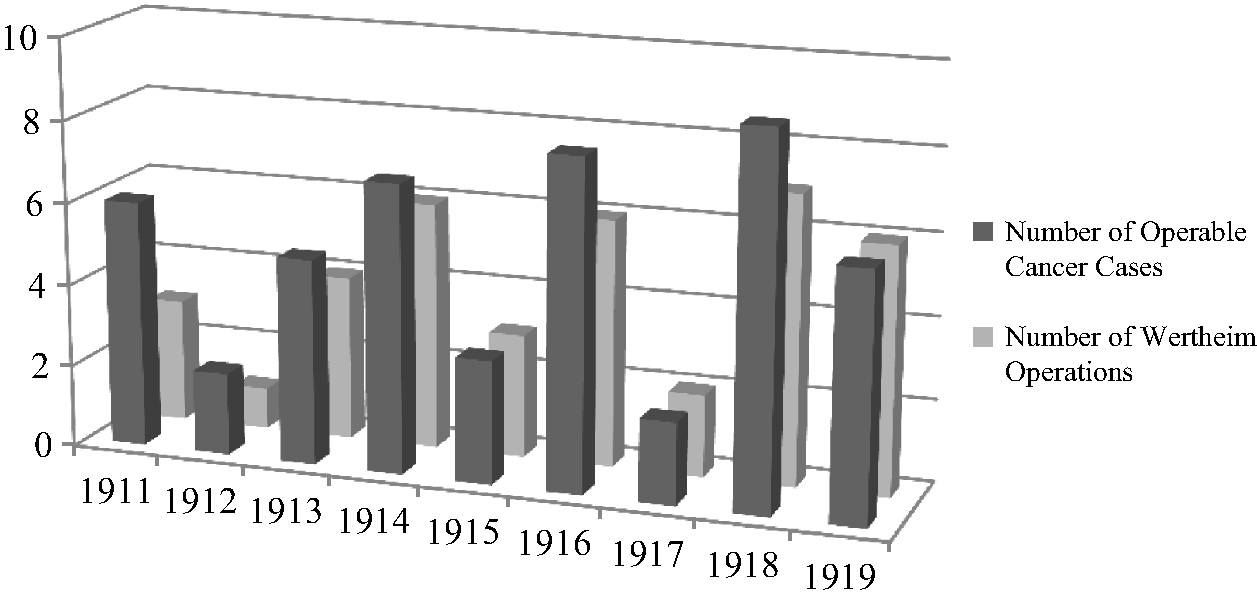
Figure 3.16 Number of Operable Cancer Cases and Wertheim Procedures by Vaughan-Sawyer: RFH, 1911–1919.Footnote 96
This is not to deny that Vaughan-Sawyer's propensity to gamble always paid off. While Emma Knight benefitted from the more extensive surgery, others did not. Elizabeth Tranter, a 59-year-old widow from Hoxton, also suffered from bronchitis and was a similar age and condition to Emma Knight.Footnote 100 Mrs Tranter's health required a longer rest and treatment period, and it was five weeks before she became a more suitable subject for operation. As a very stout, but healthy-looking woman, she was a less appropriate type for a Wertheim than the ‘wiry’ Emma Knight. A very fat abdomen, indeed, was enough to put off some surgeons from operating in this manner. In choosing cases, Berkeley reminded his colleagues, the very fat, or those who suffered from cardiac, pulmonary or renal diseases were ‘very bad subjects’ and ‘should be left alone’, although he did not agree with leaving those over 60 simply because of their age.Footnote 101 Other gynaecologists, such as Hastings Tweedy, felt that ‘[e]xtreme fatness’ was a ‘hindrance’, but should not be viewed as an ‘absolute contra-indication’ when considering Wertheim's.Footnote 102 Vaughan-Sawyer was evidently of the same mind when she made the decision to operate on Elizabeth Tranter. Although warned by her physician colleague Arthur Phear, with whom she consulted over Mrs Tranter's respiratory state, that her patient was not a good subject for operation because of her bronchitis, Vaughan-Sawyer wavered. Initially, she cancelled the procedure, fearing that, as well as the patient's poor physical condition, the growth had possibly extended too far and a recurrence would result. The likely side-effect of a permanent vesical fistula after operation was also feared, condemning the patient to a miserable future, even if the cancer was removed. However, a further delay meant that Vaughan-Sawyer had time to change her mind. A week later, Elizabeth Tranter's respiratory problems were better, and her flesh was firmer and so the procedure went ahead, successfully. There was a double triumph when Mrs Tranter was opened up. The disease had not spread as much as feared and, throughout, the patient remained in an excellent condition. However, four days after the procedure, Elizabeth Tranter died very suddenly from heart failure. This was another side-effect of Wertheim's, due to the length and seriousness of the operation, which exercised detractors because it caused the largest post-operative mortality.Footnote 103 Unlike Emma Knight's case, this was one where risks taken did not improve the final outcome.
Yet there was one more thing besides the improvements in Mrs Tranter's medical condition which compelled Vaughan-Sawyer to operate: Elizabeth Tranter had been ‘very anxious’ to have the procedure. In the light of contemporary medical and lay concerns about women's unwillingness to be operated upon, Mrs Tranter's situation revealed a very different picture of those who had been diagnosed with cancer. As we have already seen, there were refusals to undergo surgery in the period between 1904 and 1919, but the numbers were extremely small in comparison with those who were willing to trust their surgeon's capabilities and judgement. Indeed, as Figure 3.15 showed, only three of Vaughan-Sawyer's patients in the first two decades of the twentieth century refused an operation for cancer. This was just 1.7 per cent of the total number seen and diagnosed with malignant disease. If women were condemned as reluctant to consult in time, then it is hard to see, in this instance, how they could be castigated for not trying to help themselves, even if the outcome might be uncertain when difficult and dangerous surgery was the only answer. As noted in the previous chapter, and as feared by specialists, too often general practitioners were not examining their female patients when they came to them with suspicious symptoms indicating the possibility of malignancy. This broke the link in the referral chain between patient, doctor and gynaecologist, leading to many skipping the middle option and coming straight to the hospital when attempts to seek medical help had failed to produce any answers or effective treatment. Vaughan-Sawyer, in particular, was very keen to encourage her patients to keep her directly informed about their progress. This continuing care extended both to those diagnosed with cancer and those who had been warned about the possibility of malignant disease. Berkeley lamented how impossible it was to trace hospital patients in Britain in comparison to the Continent where authorities, such as the police, kept more accurate records.Footnote 104 The RFH female surgeons, however, encouraged letter-writing as well as attendance at the hospital's Out-Patients in order to follow their cases. Minnie Fuller's notes did not end with her surgical treatment for chorio-epithelioma, which developed after the miscarriage of a vesicular mole. She was to write to Vaughan-Sawyer fortnightly and to see her doctor very frequently. Unfortunately, Mrs Fuller's letters ceased after a couple of months, when a local reoccurrence, coupled with signs of a cerebral embolus, killed her.Footnote 105 Fifty-three-year-old Elizabeth Cuthbert was diagnosed with a malignant ovarian cyst and carcinoma of the rectum in 1910. While the tumour was removed, along with her ovary, the rectal cancer was discovered after the procedure, and was not operated upon at the RFH. After her death, local Norfolk practitioner, Dr Butterworth, wrote to Vaughan-Sawyer, in a letter dated 4 September 1910:
At first she improved considerably in her general condition. She had much less loss although in spite of douching it remained horribly offensive. The growth in the rectum made slower progress than did the ovarian one. Improved so far as to come down stairs and even walk into garden, but complained of feeling heaviness in hypogastrium. Pain relieved by aspirin for some weeks. By middle of July, condition had become much worse; could hardly get out of bed. Large mass of growth in left inguinal region, which felt almost as large as foetal head. At this time she had transient oedema of various limbs; right hand first part to become swollen; tongue remained clean, but had lost all appetite. Abdomen became very distended at about the time and there was some free fluid. Liver enlarged and no doubt full of secondary growths. Pain was most troublesome symptom and was only relieved by large doses of opium. Constipation began to be troublesome at end of July. At beginning of August she was very weak and growth in abdomen felt enormous; died Aug 17th.Footnote 106
This correspondence allowed a rare insight into the condition of a patient with malignant disease for whom only some surgical treatment could be carried out, due to the spread of the condition. Mrs Cuthbert's slow, painful death, after a brief period of respite, as well as the meticulous detailing of her decline by a general practitioner, revealed the desperation many medical professionals felt when faced with inoperable cancer. The prolonging of a patient's life through surgery was a hotly debated topic, but Dr Butterworth's letter, prompted by Vaughan-Sawyer's follow-up system, gave a chance to witness vicariously the last few months of a terminal case.
Additionally, instructing future possible sufferers to return at regular intervals was the most innovative form of patient monitoring in the early twentieth century. Vaughan-Sawyer warned a number of her cases that they had a very strong chance of developing cancer and encouraged vigilance. Ada Humphreys, for example, was tested for malignancy because of two years’ constant bloody discharge, combined with an evident family history of cancer. Mrs Humphreys had been attending Vaughan-Sawyer's Out-Patients since the beginning of 1909, and had been treated medically for prolapse and cervicitis, with pessaries and tonics. A year later, Vaughan-Sawyer feared malignancy and a wedge from her cervix was removed for pathological analysis, which returned with negative results. Yet the symptoms worsened, and Mrs Humphreys was admitted. Although her condition was not cancerous, Vaughan-Sawyer concluded that it was ‘favourable soil for the growth of malignant cells’ and acted accordingly by performing a panhysterectomy, as a preventative measure.Footnote 107 After seven children, two miscarriages, many years of pain and suffering and the possibility of developing cancer, Mrs Humphreys was happy for the operation to go ahead.
Alice Briggs was in a similar situation to Ada Humphreys, having suffered from intermenstrual loss for a few years. Additionally, as curettings looked suspicious under the microscope. Vaughan-Sawyer asked her to come up to the hospital frequently for ‘careful watching’.Footnote 108 Mrs Briggs returned to be observed, so that when her condition worsened again, Vaughan-Sawyer admitted her and performed a panhysterectomy. Similarly, Amy Cook was admitted initially for endometritis, after suffering from continual loss for the past nine months since the birth of a child in June 1910. While pathological examinations did not reveal cancerous cells, further sections were cut to make sure; the latter ‘inclining’ towards the future development of malignancy. Unsurprisingly, Vaughan-Sawyer wished the patient ‘to be watched’.Footnote 109 Mrs Cook diligently attended Out-Patients for observation and she deteriorated again in the late summer of 1911, she was admitted for panhysterectomy. While there were no malignancies found in the cases of Ada Humphreys, Alice Briggs and Amy Cook, the suspicious pathological findings allowed Vaughan-Sawyer to act preventively.Footnote 110 None of these patients were seen again. Neither were Annie Besnay, Elizabeth White nor Martha Webb, all of whom were warned to come to Out-Patients regularly or to seek medical advice the instant they experienced symptoms similar to those which brought them to the RFH in the first place. Although discussing a later period, John Pickstone has described interwar preventive measures as essentially catching the disease early and providing treatment in the hope of avoiding death.Footnote 111 At the RFH, however, Vaughan-Sawyer was attempting in the 1910s to prevent cancer before the disease had a chance to manifest itself in some of her patients. This could be seen as a drastic and unnecessary measure in women of active childbearing age, which resembled the ‘homicidal vivisections’ of Wertheim's procedure. Vaughan-Sawyer, however, was evidently as keen to prevent malignant disease by acting pre-emptively, as she was to ‘cure’ her patients through radical surgery.
This is not to deny, however, that some cases seen by Scharlieb and Vaughan-Sawyer ignored professional advice. The fact that there were any refusals in life-threatening situations to undergo surgical procedures which might allow the patient to live a little longer or to exist painlessly showed that not all could bring themselves to seek treatment surgically, whatever the cost. As we saw in the previous chapter, this could be due to fear of an anaesthetic, the operation itself, or lack of family support for such a step. Some also discharged themselves because there was no hope or the chances of success were slim. Scharlieb and Vaughan-Sawyer appear to have been honest with their patients about the possibility of a ‘cure’. Mary A. Newland, whose husband refused to allow surgery for cancer, was ‘not pressed’ after the decline of treatment, as Scharlieb felt it was doubtful whether the growth was really operable and the probability of a cure was not great.Footnote 112 While the surgeon would take the risk, the patient would not, and Scharlieb respected her wishes. In 1910, Mary A. Maynard was told clearly that her case was inoperable and that the growth had better be left, unless it troubled her, as it could not all be safely removed.Footnote 113 By contrast, Ruth Barden's initial refusal to allow a doctor to examine her vaginally and her two-month delay before she consulted female advice at the Bermondsey Medical Mission ensured that, when the latter swiftly dispatched her to the RFH for operative treatment, her cancer of the cervix had spread extensively and become quite inoperable. Mrs Barden discharged herself the day after admission when informed that nothing could be done for her.Footnote 114 Unlike those patients described in the previous paragraph, Mary Rose did not follow medical advice. After a severe attack of abdominal pain in August 1908, Mrs Rose went to Clapham Maternity Hospital, where she was encouraged to attend the RFH's Gynaecological Out-Patients. There, she was diagnosed with suspected fibroids, but was told to keep attending this clinic so an eye could be kept on her condition. She failed to do so. When Mrs Rose finally returned to Out-Patients in April 1909, her situation was severe enough for admission. She was discovered to have ovarian cancer, which had spread to her pelvis, described as ‘choked with growth’, and liver.Footnote 115 Others were apparently luckier. Thirty-year-old Emily King consulted Vaughan-Sawyer in the nick of time for what turned out to be an epithelioma of the vulva. It had been causing her pain since 1917, forced her to give up her job as a machinist, and was now in an advanced state. Vaughan-Sawyer recommended immediate operative interference because in a few months the growth would have spread to her urethra and femoral sheath and ‘all cure would be hopeless’.Footnote 116 Mrs King, unsurprisingly, consented to the procedure. However, during the surgery, Vaughan-Sawyer remarked upon the florid nature of the urethra and feared recurrence. She was, unfortunately, proved correct, when Emily King returned to have a new nodule removed from precisely this area in the summer of 1918. Given that she was then sent to the Radium Institute, and what that meant effectively, it could be presumed that Mrs King's late consultation rendered her case eventually inoperable. It was only when her condition became intolerable, not even allowing her to sit down comfortably, that Emily King sought advice. By then, it was too late and despite surgery, treatment became solely palliative.
In similar fashion to Emily King, those condemned as ‘inoperable’ in the second decade of the twentieth century were often recommended alternatives to surgery as a last resort or momentary respite before death. Rarely, as already noted, were therapeutic measures such as X-ray or radium treatment given for the ‘curable’ patient in the RFH's Gynaecological Department. Löwy has remarked that while surgery for malignant disease was still dangerous, therapeutic measures offered more attractive options, which were less risky and, even though dogged by some side-effects such as potential infection of the cancerous lesion by pathogenic bacteria, the advantages outweighed those of radical operations.Footnote 117 However, it is fruitful, in the final section of this chapter, to explore how women experienced such treatment, especially when being sent to places such as the Radium Institute in these experimental years meant that death was simply being postponed. As reported by the director, A.E. Hayward Pinch, many of the patients at the Institute had ‘exhausted all the known resources of medicine and surgery, their condition being almost helpless’.Footnote 118 It is telling that, in the first year of work recorded at the Institute, 88 patients abandoned their treatment; Pinch explained that this was due to the inconvenience or the expense of travelling to London.Footnote 119 While this decreased over the next two years, from 50 to 11,Footnote 120 it is worth examining why a supposedly less invasive, more ‘humane’ treatment put off some of those it was intended to help, to the extent that they stopped their attendance at hospital or at the Radium Institute. For some, indeed, early radiotherapies were little different to quack cures. In her history of this alternative approach to treatment, Murphy places radiotherapy before the Great War ‘on the fringes of quackery and orthodoxy’,Footnote 121 and, unlike surgery, suspicion of this approach was common both to patients and practitioners. Frederick Treves described the use of the X-ray in surgery as a sorry history of hopes dashed.Footnote 122 Two years later, indeed, E.F. Bashford, the General Superintendent of Research and Director of the Laboratory of the Imperial Cancer Research Fund, placed ‘Radio-activity’ alongside ‘Nonsense’ and ‘Faith-healing’ in the ‘Quack's Armamentary’.Footnote 123 Little had changed just before the war, when Cuthbert Lockyer's assertion that radiology should be the future for the gynaecologist was met with deafening silence.Footnote 124 Yet, if the medical profession itself was sceptical, how did the patient react to the proposition that they undergo a course of radiotherapy to prolong their lives?
The earliest patient to receive X-ray treatment in the Gynaecological Department was 65-year-old Mary A. Thompson, who became a surgical Consultation Case after being diagnosed with carcinoma of the vagina, which had spread to the wall of the rectum. An operation was not advised in this case, although it could have been ‘just’ anatomically possible. Vaughan-Sawyer was keen to operate, but, upon consultation with colleagues Scharlieb, Florence Willey and Thomas Legg, and in consideration of the patient's age and poor general condition, X-ray treatment was ‘tried’ instead in order to keep the growth down. X-ray applications improved Mrs Thompson's general condition markedly, the pain was a good deal less and the discharge also decreased. Her condition remained inoperable, however.Footnote 125 Annie Wheeler, whose womb had been removed for malignancy earlier in the year, came back in November 1912. Miss Wheeler had been suffering from pain in the right groin since August and a large mass of growth on the right side of her pelvis was discovered. She had been treated by a number of different procedures, most of which Bashford and others would have described as quackery, such as radiant heat baths, salt baths, vapour baths, liniments, and, most recently, massage. Despite her exceedingly good condition after the first operation and an entirely uneventful recovery, it was evident a few months later that the cancer had returned and spread to the bladder. After only a month, Miss Wheeler had what she labelled a nervous breakdown, which was followed by pain in her thigh and groin, lasting more or less ever since. When she was readmitted, her condition was considered quite inoperable and X-rays were utilised ‘in order to less the pain [sic], and if possible retard the growth’. Despite this proposition, the growth was spreading rapidly, and when she was discharged the pain was better than it was on admission, but actually increased by movement.Footnote 126 In these two early cases, X-rays reduced the pain experienced by both women, but they were unable to halt or shrink the tumours to render them operable. Instead, the treatment was simply palliative. Neither woman was seen at the RFH again.
Radium treatment was offered to inoperable patients from 1914, when all other options had failed. The popular press lauded radium as a miracle cure,Footnote 127 but none occurred in the gynaecological beds of the RFH. Hagar Walker, a patient since 1906, had undergone a modified Wertheim for carcinoma of the cervix at the end of 1913, but carcinomatous nodules had been discovered in February 1914 and the left sacro-uterine ligament and anterior rectal wall were also found to be infiltrated with growth. After X-ray treatment, which the patient found very painful and weakening, a radium application was tried with a vaginal emanation tube. The pain of this experience was considerable, but it afforded temporary relief and a good night's sleep. Mrs Walker was to come up again for further radium treatment if possible. Despite her frequent attendance at the RFH over the years, she was not seen again.Footnote 128 Melia Howlett, who had extensive carcinoma of the rectum, was treated with radium for a year and three-quarters. In contradistinction to usual procedures, whereby hospitals referred their patients to the Radium Institute, Dr Lynham of the Institute had sent Mrs Howlett to Vaughan-Sawyer. Initially, the patient's doctor had discovered a tumour and advised radium applications to prepare the growth for an operation. Mrs Howlett had consequently been undergoing radium treatment once a month for five days, and for six hours of each day. Then a radium tube was inserted into the rectum. There was very little improvement in her condition and haemorrhage continued. Furthermore, Mrs Howlett had felt much worse in herself, with pain down her right thigh and faintness; a vesico-vaginal fistula had developed and discharge now seeped through both rectum and vagina. Vaughan-Sawyer performed a colotomy upon Mrs Howlett, who began to feel ‘very well’ because of the surgery. While the growth was still very large and fungating, the switch from radium treatment to surgical procedure made Mrs Howlett far more comfortable than she had felt in a long while.Footnote 129 While surgery could not cure her, neither could radium, but the former relieved her situation, whereas the latter exacerbated her pain and suffering. Although this was only a single instance, it is important to note that there was not a one-way trajectory between the Radium Institute and the hospitals. Where one could no longer assist the patient, the other could take over. Radium was not the miracle cure for all, and, where it failed, surgery, as in the case of Melia Howlett, could relieve in ways it could not.
Some experienced pain relief from X-ray applications or radium treatment, but found that it did not work in the long run. Annie Ansell, who attended in 1915 for a Bartholini's cyst, was later discovered to have an epithelioma in her groin. X-ray treatment was tried, but it simply did not ‘arrest the course of the disease’; her pain was only relieved by the withdrawal of fluid from the growth. Vaughan-Sawyer recommended that X-rays were stopped and the patient sent to a home or an infirmary, evidently to die.Footnote 130 Others were simply too ill to keep going with the processes. Thirty-four-year-old Harriet Croydon, who had a recurrence of malignant disease in the pelvis, had undergone some electrical treatment after her Wertheim's operation in the summer of 1914 and had further X-ray applications in the RFH at the beginning of 1915. These reduced her pain considerably, but, after leaving the hospital and returning every week for repeat procedures, Mrs Croydon was unable to continue to attend the RFH because of the fatigue she experienced travelling from her home in North London.Footnote 131 The practicalities of suffering from incurable malignant disease often overtook any desire to continue the hassle of treatment which could only ever prove palliative. In similar fashion to Melia Howlett, it was also recommended by the Radium Institute that Kate Coles’ treatment for carcinoma of the fundus be carried out in hospital. Her notes described this procedure in detail: it was neither quick nor without unfortunate side-effects. A radium tube was inserted into the cavity of the uterus and left for 24 hours; this resulted in little pain, but a good deal of bleeding. On 24 June 1915, a second application was made, which caused Mrs Coles some burning pain and an ache in the lower part of the back and abdomen. Two days later, after the tube had been removed, there was more comfort.Footnote 132 Neither Harriet Croydon nor Kate Coles attended the hospital again. In May 1914, Elizabeth Fowles did not even have the option of radium applications for a recurrence after Wertheim's procedure a few months before. While such a course was advised, there was no radium obtainable. Neither the Radium Institute nor the Middlesex Hospital could assist the RFH in finding an emanation tube for this patient. Mrs Fowles left the hospital, with only heroin to help her pain and the promise that ‘if radium can be obtained she will be treated.’ Meanwhile, if she wished it, arrangements would be made to find her a place in a home for the dying. Mrs Fowles’ record ended here, and presumably the only option was the last.Footnote 133 It was noticeable that after 1915, the suggestion that radium be used in palliative care disappeared and did not return until the summer of 1918. Radiotherapy was not the mode of treatment most recommended by the RFH surgeons for gynaecological cancer patients unless the cases were terminal because surgery was always the first resort, and, even in cases eventually treated with radium, surgery was often attempted first and as much of the growth removed as possible. It is important to remember that the Great War actively prevented radium supplies from being obtained for dying patients.Footnote 134 The 1910s might have seen an interest in the properties of radiotherapy, but professional disinterest in what some labelled quack remedies, coupled with the expense and scarcity of radium meant that many, like Elizabeth Fowles, had to forgo this new treatment in favour of powerful painkillers to make the end of life bearable.
Conclusion
By exploring in detail the ways in which female surgeons treated malignant disease in the first two decades of the twentieth century, it is possible to draw the following conclusions. Firstly, and most fundamentally, that, in spite of previous claims to the contrary, these women specialists, in the vast majority of cases, resorted to surgery when dealing with cancer. While other treatments were considered, they were only suggested when the patient's condition was inoperable. Unlike some of their colleagues, women surgeons did not scoff at quackeries, but neither did they change the way they operated when newer possibilities emerged, thanks to the development of radiotherapy. This form of treatment was not embraced wholeheartedly by patients either, who suffered the side-effects of applications and even discontinued them. Secondly, women surgeons were not afraid to try long, hard and difficult surgical procedures in order to give their patients the best chance of survival, however limited that might be in reality. As Wertheim had noted the time of the operation could be reduced considerably with practise. This bypassed the problems which patients who were designated as unsuitable for surgery might encounter; which, in turn, allowed more to undergo surgery. By October 1919, Vaughan-Sawyer took just over an hour to perform a Wertheim, whereas seven years previously the same operation took twice this time.Footnote 135 Neither were female surgeons afraid to modify and rework existing methods. This satisfied both their own curiosity about the best means to tackle malignant disease and meant that they were able to tailor their surgery to each patient, in similar fashion to Aldrich-Blake's development of rectal procedures. Thirdly, a belief in the importance of the pathological confirmation of disease and a desire to keep track of patients who had suffered from cancer, as well as those who were likely candidates for malignancy, showed that surgery had to be supported for the women surgeons discussed here with scientific confirmation and careful observation. Finally, working-class female patients were attacked as the worst culprits when it came to taking care of their health. When diagnosed, however, the majority were more than willing to take risks if an invasive, potentially life-threatening operation could give them a little longer. For many patients, early twentieth-century surgery was an ‘option worth trying’, as Wilde has discussed.Footnote 136 Some, such as Mary Keyworth, who was told by Vaughan-Sawyer in 1910 that her carcinoma of the cervix was operable if she wanted to ‘take the risk’, decided ‘after careful consideration’ that they did not want surgery.Footnote 137 This did not mean, as this chapter has revealed, that women surgeons themselves were not prepared to do everything they could to relieve their patients surgically. For them, the chance was always worth taking even if there was only a slight possibility that a life could be saved.