A 50-year-old man suffered from acute lacunar infarction of the right thalamus, midbrain and pons 3 months earlier and was left with blurred speech and unstable gait. Neurological examination revealed mild dysarthria, left-sided central facial paralysis, left-sided hypoglossal paralysis and gait ataxia. There was no palatal myoclonus or nystagmus. The remaining neurological examinations were unremarkable. Serologic and metabolic work-up were unrevealing. Brain MRI showed chronic infarction of right thalamus, midbrain and pons, and bilateral olivary hyperintensity on T2 and fluid-attenuated inversion recovery, indicating bilateral hypertrophic olivary degeneration (HOD) (Figures 1A-1B). Diffusion tensor imaging showed decreased volume of right central tegmental tract (Figure 1C).
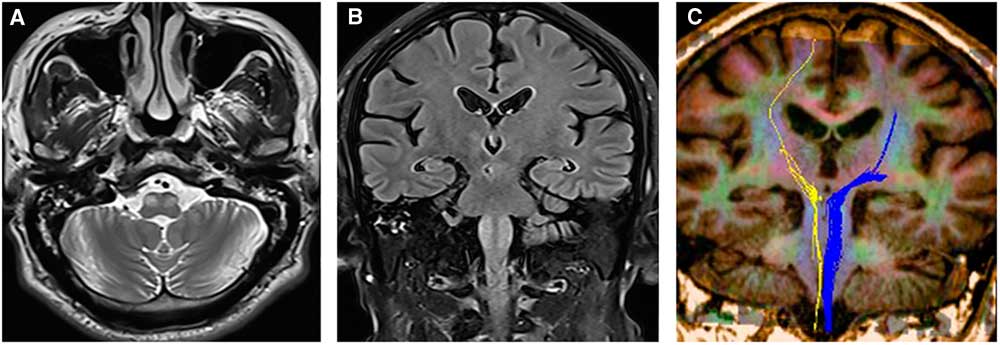
Figure 1 MRI and diffusion tensor imaging. Symmetric hyperintense signal abnormality and enlarged inferior olives on T2-weighted image (A) and fluid-attenuated inversion recovery image (B). Decreased volume of right central tegmental tract was shown on diffusion tensor imaging (C).
Hypertrophic olivary degeneration is secondary trans-synaptic degeneration of the inferior olivary nucleus (ION) owing to primary lesions in the dento-rubro-olivary pathway, also named as Guillain-Mollaret Triangle (GMT). Guillain-Mollaret Triangle comprises connections among the inferior olive nucleus, the red nucleus and the contralateral dentate nucleus, which was first described by Guillain and Mollaret in 1931.Reference Guillain and Mollaret 1 The common causes of HOD include infarction, hemorrhage, arteriovenous malformation, tumor, trauma, prior surgery, inflammation and demyelination.Reference Sabat, Mannering and Agarwal 2 , Reference Konno, Broderick, Tacik, Caviness and Wszolek 3 In addition, other disorders including abscesses, Wilson’s disease, metronidazole intoxication and neuro-Behcet disease may also cause HOD.Reference Konno, Broderick, Tacik, Caviness and Wszolek 3 , Reference Martins, Schilling, Neto and Becker 4 Pathological changes of HOD are characterized by enlargement and vacuolation of neurons, astrocytic hyperplasia and demyelination, which are considered secondary to loss of afferent input to the ION.Reference Konno, Broderick, Tacik, Caviness and Wszolek 3 Bilateral HOD is more common than unilateral HOD.Reference Carr, Hunt, Kaufmann, Kotsenas, Krecke and Wood 5 Palatal tremor, Holmes tremor, nystagmus and cerebellar ataxia are classically associated features of HOD, but they are often not present.Reference Sabat, Mannering and Agarwal 2 , Reference Cosentino, Velez and Nunez 6 About 61%-77% of the patients are asymptomatic and could be found incidentally on MRI scans.Reference Konno, Broderick, Tacik, Caviness and Wszolek 3 , Reference Carr, Hunt, Kaufmann, Kotsenas, Krecke and Wood 5 Differential diagnoses of HOD include brain stem infarction, inflammatory diseases and neoplastic diseases.
Disclosures
QL, CZ, RZ, XL, YL and QX have nothing to disclose.
Statement of Authorship
QL: design of the work, drafting the work and revising the manuscript. CZ: design of the work, acquisition and analysis of data. RZ: analysis and interpretation of the data and drafting the work. XL: acquisition and interpretation of data. YL: acquisition and interpretation of data, and revising the manuscript. QX: design of the work and revising the manuscript.
Consent
Informed consent was obtained from the patient for publication of this case report and any accompanying images. The study protocol has been approved by the ethics committee of Zhejiang hospital on human research.





