Food security is an ideal state when people at all times have access to sufficient, safe and nutritious food to remain healthy and active( Reference Tarasuk 1 , 2 ). Food insecurity occurs when access to food is limited, inadequate or insecure to meet the dietary requirements for a productive and healthy life of individuals, families or households( Reference Tarasuk 1 ). Food insecurity, with its associated health consequences, remains pervasive in Canada( Reference Anema, Vogenthaler and Frongillo 3 – Reference Tarasuk, Dachner and Hamelin 7 ). In 2012–2013, 13–14 % of North American households were food insecure( Reference Coleman-Jensen, Gregory and Singh 8 , Reference Tarasuk, Mitchell and Dachner 9 ), with acute or chronic financial insecurity or poverty as the main determinant of household food insecurity( Reference Gorton, Bullen and Mhurchu 10 – 12 ).
People experiencing poverty and homelessness are at heightened risk of experiencing hunger and food insecurity( Reference Lee and Greif 13 ). A national survey of individuals experiencing homelessness in the USA found that approximately 40 % of participants reported fasting for an entire day in the past month or were unable to afford food in the past month, while 12 % engaged in subsistence eating (eating out of trash cans or via hand-outs) in the last week( Reference Lee and Greif 13 ). In the same study, approximately three-fifths of the respondents also reported food inadequacy in terms of quantity or preference (61 %) and infrequent meals (57 %)( Reference Lee and Greif 13 ). In Toronto, Canada, Holland et al. reported that 72 % of individuals experiencing homelessness were food insecure; specifically, 30 % of the sample reported marginal levels of food security, 10 % low food security and 32 % very low food security( Reference Holland, Kennedy and Hwang 14 ). A series of studies of youths experiencing homelessness in Toronto similarly demonstrated that this sub-population experiences nutritional deficiencies( Reference Li, Dachner and Tarasuk 15 , Reference Tarasuk, Dachner and Li 16 ), severe food insecurity (among 85 % of females and 73 % of males)( Reference Tarasuk, Dachner and Poland 17 ) and chronic food deprivation (among 43 % of females and 28 % of males)( Reference Tarasuk, Dachner and Poland 17 ).
Previous research has revealed that specific individual-level factors are associated with food security among individuals experiencing homelessness, including living at or below the poverty line, mental and physical health issues, increased rates of hospitalization and emergency department visits, and chronic homelessness( Reference Lee and Greif 13 , Reference Baggett, Singer and Rao 18 , Reference Weiser, Frongillo and Ragland 19 ). Population-level factors are also associated with food security among individuals experiencing homelessness. Emergency shelter policies have been shown to constrain food choice by restricting the storage of perishable items and providing limited cooking facilities and food storage space. Such policies often lead to purchasing of non-perishable and less healthful food products( Reference Richards and Smith 20 , Reference Wicks, Trevena and Quine 21 ).
Although prior research has shown that up to 71 % of individuals with severe mental illness experience food insecurity( Reference Goetz 22 – Reference Muldoon, Duff and Fielden 24 ), to date, the prevalence of and factors associated with food insecurity have not been specifically examined in a sample of individuals experiencing homelessness and mental illness. We seek to add to this small but growing literature.
Interventions to improve food security among homeless people have focused primarily on charity food programmes such as food banks and soup kitchens( Reference Kirkpatrick and Tarasuk 25 , Reference Roncarolo, Adam and Bisset 26 ) and community-based initiatives such as community kitchens and gardens( Reference Armstrong 27 , Reference Engler-Stringer and Berenbaum 28 ). However, studies on these topics have been plagued by low participant rates( Reference Tarasuk, Dachner and Hamelin 7 , Reference Kirkpatrick and Tarasuk 25 , Reference Loopstra and Tarasuk 29 , Reference Vozoris and Tarasuk 30 ) and the evidence of their positive impacts on reducing food insecurity is inconclusive( Reference Kirkpatrick and Tarasuk 25 , Reference Engler-Stringer and Berenbaum 28 , Reference Loopstra and Tarasuk 29 ). Housing First (HF), which combines permanent housing in conjunction with access to mental health supports, has emerged as a promising intervention for individuals experiencing homelessness and mental illness, and has been shown to be effective in improving residential stability, quality of life and health-service use( Reference Aubry, Tsemberis and Adair 31 – Reference Tsemberis, Gulcur and Nakae 35 ); however, the impact of HF on food security is unknown. We hypothesized that access to stable housing and mental health supports would improve food security among homeless adults experiencing mental illness. Thus the present study aimed to: (i) assess the levels and predictors of baseline food insecurity among individuals experiencing homelessness and mental illness participating in the At Home/Chez Soi study; and (ii) determine the effect of an HF intervention on food security over 18 months of follow-up.
Methods
At Home/Chez Soi study design
The At Home/Chez Soi study was a multi-site randomized controlled trial that examined the effectiveness of an HF intervention among adults experiencing both homelessness and mental illness across five sites in Canada( Reference Aubry, Tsemberis and Adair 31 , Reference Stergiopoulos, Hwang and Gozdzik 33 , Reference Goering, Streiner and Adair 36 ). HF offers individuals experiencing homelessness and mental illness permanent housing in conjunction with access to mental health support services, without the prerequisites for abstinence or treatment acceptance imposed by more traditional ‘treatment first’ interventions aimed at this population( Reference Tsemberis, Gulcur and Nakae 35 ). Details of the research protocol have been previously published( Reference Goering, Streiner and Adair 36 ). Briefly, eligibility for the At Home/Chez Soi study included: (i) legal adult age (≥18 years; ≥19 years in Vancouver); (ii) absolute homelessness or being precariously housed; and (iii) severe mental illness with or without a concurrent substance use problem. Participants were excluded if they were not legally residing in Canada or were already receiving assertive community treatment (ACT) or intensive case management (ICM)( Reference Goering, Streiner and Adair 36 ). The study was approved by the research ethics boards of all participating institutions.
Prior to randomization, participants were classified as high or moderate need based on their need level for mental health services. High need (HN) participants were identified as having: (i) a Multnomah Community Ability Scale (MCAS)( Reference Barker, Barron and McFarland 37 ) score of ≤62; (ii) a Mini International Neuropsychiatric Interview 6.0 (MINI 6.0)( Reference Sheehan, Lecrubier and Sheehan 38 ) diagnosis of current psychotic or bipolar disorder (or an observation of psychotic behaviour); and (iii) one of the following criteria: ≥2 hospitalizations for mental illness in any one of the past 5 years, co-morbid substance use or recent arrest/incarceration. Moderate need (MN) participants were identified as all others who met eligibility criteria but were not identified as HN. People with HN for mental health services are best served by a multidisciplinary ACT team, which provides comprehensive 24 h/d mental health and crisis services. ICM provides a lower intensity of mental health services for people who do not require ACT: case managers work one-on-one with the client to assess his or her needs and secure necessary services from community-based providers. As a result, participants in the HN group were randomized to HF and ACT or a standard-care treatment as usual (TAU) group, while those in the MN group were randomized to HF and ICM or TAU. In Moncton, both MN and HN participants were randomized to HF and ACT or TAU. The protocol also included the addition of site-specific intervention arms that have been adapted to the local context (see Fig. 1 for flow diagram).

Fig. 1 Participant flow diagram (ACT, assertive community treatment)
Participants randomized to the HF intervention were provided with housing in areas of the city they preferred. To help facilitate participant community integration, housing was scattered in units throughout the city (‘scattered-site’) and a maximum of 20 % of the total units in any one building or residence were dedicated to study participants( Reference Goering, Streiner and Adair 36 ). In addition to housing, intervention participants also received mental health services offered via either ICM or ACT, which were provided off-site and not tied to their tenancy. TAU participants were provided with a list of existing resources in their city, which they could access at their choosing. Sites varied in the number and extent of services available; however, some access to food banks and emergency shelters and drop-in centres that offered meals was available at all sites and available to participants in both randomization groups. All participants were followed for 2 years post-randomization.
Participants
The sample consisted of 2148 individuals experiencing homelessness and mental illness who were enrolled in the At Home/Chez Soi study from October 2009 to July 2011. All participants provided written informed consent and received an honorarium, ranging from $CAN 10 to $CAN 80, depending on the site and interview duration, for their participation in the study.
Data collection
Participants completed interviews at study entry and subsequently every 3 months during the 24-month period following enrolment. All study interviews were conducted by trained interviewers who input the data directly into a secure online database. In addition to food security, the survey assessed sociodemographic characteristics, health-service use, housing situation, community functioning, physical and mental health status and substance use, which have been described in detail in a former publication( Reference Goering, Streiner and Adair 36 ).
Variables
Food security status, the main outcome, was assessed every 6 months, using a modified version of the US Food Security Survey Module (US FSSM)( Reference Bickel, Nord and Price 39 ) for single adults, with the period of interest spanning the 30d prior to the interview. This instrument, previously tested in a sample of individuals who were homeless, has shown moderate agreement with the original version of the US FSSM and was preferred over the original US FSSM instrument as being more relevant to homeless people( Reference Holland, Kennedy and Hwang 14 ). It is important to note that while frequently used as a measure of food security, the US FSSM measures food security as resulting directly from constraints of financial resources. As a result, it does not encompass the multifaceted dimensions of food security( Reference Bickel, Nord and Price 39 ), which are captured by the FAO’s definition and include ‘physical, social and economic access to sufficient, safe and nutritious food which meets their dietary needs and food preferences for an active and healthy life’( 2 , 40 ). The resulting total scores for the US FSSM scale range from 0 to 10 and are classified into four food security status groups: (i) high (score of 0); (ii) marginal (score of 1 or 2); (iii) low (score of 3–5); (iv) and very low (score of 6–10). These updated categories were outlined by the US Department of Agriculture in 2006, based on recommendations from the Committee on National Statistics (Table 1)( 41 ). Prior to these recommendations, a score of 0 was defined as ‘food secure’, while a score of 1 or 2 was ‘food insecure without hunger’, 3–5 was ‘food insecure with hunger (moderate)’ and 6–10 was ‘food insecure with hunger (severe)’. Since 2006, the updated labels interpret all categories in terms of level of food security (very low to high). According to the US FSSM guide, the combination of the first two categories (high and marginal food security) can continue to be considered ‘food secure’ while the latter two categories (low and very food security) can be considered ‘food insecure’( 41 ).
Table 1 Old and new categories of food security from the US Food Security Survey Module (US FSSM)( 41 )

Other variables used in our analyses included the MCAS( Reference Barker, Barron and McFarland 37 ) to assess community functioning and the Colorado Symptom Index (CSI)( Reference Boothroyd and Chen 42 ) to assess psychiatric symptom severity. For the CSI, we created a dichotomous variable (<30 v. ≥30), as prior research indicates that scores higher than 30 can be used to predict a psychiatric diagnosis( Reference Boothroyd and Chen 42 ). Two variables assessed drug or alcohol problems among participants: the number of days in the past 30d in which alcohol or drug problems were experienced and the percentage of income spent on alcohol or non-prescription drugs. Four self-reported physical health conditions were included based on their hypothesized association with food intake: ulcers, bowel problems, high blood pressure and diabetes. Information about service use was included, specifically whether the participant had seen a health or social services provider at his or her office in the past month and any emergency room visits in the past 6 months. Demographic characteristics including age, sex, study site and duration of homelessness (dichotomized as <3 years v. ≥3 years) were also included.
Statistical analysis
Descriptive statistics were first generated and stratified by level of need for mental health services. We then used logistic regression models to determine associations between high or marginal levels of food security status and several sociodemographic covariates for participants at study enrolment. We included variables that were selected a priori to be potentially associated with food security: age, sex, duration of homelessness, MCAS, CSI, days experienced drug/alcohol problems, percentage of income spent on alcohol/drugs, physical health problems and service use.
To determine the impact of the HF intervention on food security, negative binomial regression models were used due to overdispersed count data for the number of times participants achieved ‘food security’ (either high or marginal food security on the US FSSM)( 41 ) between 6 and 24 months after randomization. For assessment of change in food security, we excluded baseline data, as the enrolment observation points would not reflect the impact of the intervention. To retain our large sample size, we took a conservative approach and assigned values of ‘food insecurity’ (either low or very low food security on the US FSSM) to participants with missing US FSSM data. We used descriptive statistics to test if any baseline variables differed between participants with complete US FSSM data and those with missing data; variables that differed significantly between the groups were included as covariates in the negative binomial regression models.
Models tested the main effects of treatment group and study site as well as an interaction between treatment group and study site. The model estimates the rate ratios and 95 % confidence intervals for counts of the number of times participants achieved high or marginal food security on the US FSSM between 6 and 24 months. All statistical analyses were performed using the statistical software package SAS version 9.4. A two-tailed test was used and a P value <0·05 was considered statistically significant( Reference Streiner and Norman 43 ).
Results
Baseline characteristics of study participants are shown in Table 2. We obtained information about baseline food security status for 2097 participants, 914 and 1183 from the HN and MN groups, respectively. Interestingly, fewer HN participants had marginal or high food security (n 347, 38 %) compared with MN participants (n 517, 44 %).
Table 2 Characteristics of At Home/Chez Soi study participants at enrolment for all five sites by study arm. Participants were individuals (n 2148) experiencing homelessness and mental illness enrolled at five Canadian sites (Moncton, Montreal, Toronto, Winnipeg and Vancouver), October 2009 to July 2011

MN, moderate need; HN, high need; HF, Housing First; TAU, treatment as usual; MCAS, Multnomah Community Ability Scale; CSI, Colorado Symptom Index.
Data are presented as n and % unless indicated otherwise.
There were no significant differences in baseline food security levels or any other baseline characteristics between the HF and TAU arms for the HN group.
In the MN group, a statistically significant association was observed between intervention arm and site (P<0·01). Moreover, a greater proportion of MN participants in the TAU arm saw a health or social services provider in the past month compared with those in the HF arm (88·4 v. 83·2 %; P=0·01). Finally, TAU participants spent more money on alcohol in the past 30d compared with HF participants ($CAN 92·71 (sd 215·05) v. $CAN 76·10 (sd 179·28); P=0·05).
Multiple logistic regression results of predictors of baseline food security
The results of the multiple logistic regression analyses are presented in Table 3. In the MN group, adjusted analyses revealed that the odds of reporting high or marginal food security status at baseline increased by 22 % for each 10-year increment of age over 18 years (adjusted OR (AOR)=1·22; 95 % CI 1·04, 1·42; P=0·02). Males compared with females were 32 % less likely to report high or marginal food security status at baseline (AOR=0·68; 95 % CI 0·48, 0·97; P=0·03). Individuals experiencing higher (CSI score≥30) v. lower levels of mental health symptoms were 51 % less likely to report high or marginal food security at baseline (AOR=0·49; 95 % CI 0·33, 0·74; P<0·01).
Table 3 Unadjusted and adjusted odds ratios for variables associated with high or marginal food security status at baselineFootnote * among At Home/Chez Soi study participants for all five sites by need level. Participants were individuals (n 2148) experiencing homelessness and mental illness enrolled at five Canadian sites (Moncton, Montreal, Toronto, Winnipeg and Vancouver), October 2009 to July 2011

MN, moderate need; HN, high need; UOR, unadjusted odds ratio; AOR, adjusted odds ratio; MCAS, Multnomah Community Ability Scale; CSI, Colorado Symptom Index.
* The analysis was also adjusted for site (data not shown).
† OR in 10·0 units.
‡ OR in 5·0 units.
In the HN group, individuals reporting higher levels of psychiatric symptom severity were 56 % less likely to report high or marginal food security status at baseline (AOR=0·44; 95 % CI 0·27, 0·71; P<0·01). Moreover, among HN participants, for each 10 % increase in the amount of income spent on drugs, participants were 16 % less likely to report high or marginal food security status at baseline (AOR=0·84; 95 % CI 0·77, 0·92; P<0·01).
Impact of Housing First on food security over the follow-up period
A non-negligible number of participants did not complete the modified US FSSM during the 6-, 12-, 18- or 24-month follow-up visits, for whom we conservatively assigned values of ‘food insecure’ (low or very low food security). In total, of the 950 HN participants, 202 were missing one report of the US FSSM, 109 were missing two data points and 159 were missing three or four US FSSM observations; for the MN group the numbers were 206, 103 and 157, respectively, out of a total of 1198 MN participants. We found a statistically significant difference in age between those with and without missing US FSSM data, for both the MN (40·3 v. 43·3 years) and the HN (38·6 v. 40·2 years) group, respectively. No significant differences between those with and without missing US FSSM data were noted for gender, lifetime duration of homelessness, presence of health conditions such as ulcers or diabetes or high blood pressure, social service utilization and proportion of money spent on alcohol or drugs. In order to adjust for age differences between those with and without missing data, we included participant age as a covariate in the statistical models.
Over half of our sample was able to achieve high or marginal food security during the 18-month follow-up period and across our four trial arms between 35 and 38 % never achieved high or marginal food security during follow-up (Fig. 2). The different arms ranged from 16 to 22 % in the proportion of participants who achieved marginal to high food security three or more times over 18 months of follow-up.
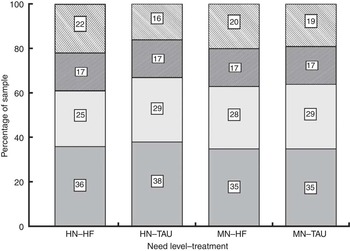
Fig. 2 Percentage of the sample of At Home/Chez Soi study participants who achieved high or marginal food security a given number of times over the 18-month follow-up period (![]() , zero times;
, zero times; ![]() , one time;
, one time; ![]() , two times;
, two times; ![]() , three or more times), by need level (HN, high need; MN, moderate need) and randomization group (HF, Home First; TAU, treatment as usual). Participants were individuals (n 2148) experiencing homelessness and mental illness enrolled at five Canadian sites (Moncton, Montreal, Toronto, Winnipeg and Vancouver), October 2009 to July 2011
, three or more times), by need level (HN, high need; MN, moderate need) and randomization group (HF, Home First; TAU, treatment as usual). Participants were individuals (n 2148) experiencing homelessness and mental illness enrolled at five Canadian sites (Moncton, Montreal, Toronto, Winnipeg and Vancouver), October 2009 to July 2011
Among the MN group, the negative binomial regression analyses showed no significant differences between the HF and TAU study arms with respect to the number of times high or marginal food security status was achieved over the 18-month follow-up period (Fig. 2). Moreover, the interaction between treatment arm and study site was not significant for the MN group.
Unlike the MN groups, there were statistically significant differences between treatment arms among HN participants. Overall, 61 % of the HF arm compared with 54 % of the TAU arm achieved marginal to high food security (z =−2·18, P=0·02).
When examined by site, the HN treatment arms of Toronto and Moncton sites had higher rates of achieving high or marginal food security compared with the TAU groups over the 18-month study period (Fig. 3). The rate of achieving high or marginal food security for the HF arm compared with the TAU arm increased by a factor of 1·42 (95 % CI 1·04, 1·95; P=0·03) for Moncton and 1·48 (95 % CI 1·11, 1·97; P<0·01) for Toronto.

Fig. 3 Mean (with 95 % CI represented by vertical bars) number of times At Home/Chez Soi study participants achieved high or marginal food security over the 18-month follow-up period, by study site and randomization group (![]() , HN–HF;
, HN–HF; ![]() , HN–TAU;
, HN–TAU; ![]() , MN–HF;
, MN–HF; ![]() , MN–TAU). The table below shows rate ratios (95 % CI) for the Home First (HF) group compared with the treatment as usual (TAU) group, at each site, by need level (HN, high need; MN, moderate need). Participants were individuals (n 2148) experiencing homelessness and mental illness enrolled at five Canadian sites (Moncton, Montreal, Toronto, Winnipeg and Vancouver), October 2009 to July 2011
, MN–TAU). The table below shows rate ratios (95 % CI) for the Home First (HF) group compared with the treatment as usual (TAU) group, at each site, by need level (HN, high need; MN, moderate need). Participants were individuals (n 2148) experiencing homelessness and mental illness enrolled at five Canadian sites (Moncton, Montreal, Toronto, Winnipeg and Vancouver), October 2009 to July 2011
Discussion
The present study is the first large-scale cross-site study to examine the prevalence of and factors associated with food security in a sample of individuals experiencing homelessness and mental illness. The prevalence of overall food security (high or marginal food security on US FSSM) observed in our study at baseline was higher than previously reported among homeless youth (8 %), lower than values reported by an earlier study of homeless adults in Toronto (58 %)( Reference Holland, Kennedy and Hwang 14 ) and less than half the reported prevalence of high or marginal food security in the general population of Canada in 2012 (90 %)( Reference Tarasuk, Mitchell and Dachner 9 ). The results of the multiple logistic regression analyses suggest that in the absence of an intervention the level of food security at baseline was associated with a few individual-level factors: being male and young. These findings are in line with prior studies demonstrating that food security is associated with demographic variables such as gender and young age( Reference Lee and Greif 13 , Reference Hamelin and Hamel 44 ). Consistent with our findings, prior research has also identified increased food insecurity among individuals experiencing homelessness who face additional obstacles, such as alcohol or substance use problems. Studies have suggested that individuals with dependence or addiction problems may have impaired decision making about how they spend their money( Reference Lee and Greif 13 ); however, others have failed to confirm this association( Reference Baggett, Singer and Rao 18 ). In contrast with previous research( Reference Lee and Greif 13 , Reference Baggett, Singer and Rao 18 ), we did not observe an association between food security and lifetime duration of homelessness of 3 years or longer. However, it is possible that this cut-off may have been too short for older adults who may have been on the street for many years. These discrepant findings may further be due to differences in the composition of populations studied (compared with other studies, the participants in the current study were all experiencing both homeless and mental illness)( Reference Lee and Greif 13 ), use of different measures of food security and use of different predictors in analyses( Reference Lee and Greif 13 , Reference Baggett, Singer and Rao 18 ). Neither physical health variables, community functioning nor health-service use variables were associated with food security in our sample. Further longitudinal studies such as ours are needed to clarify the association between these factors and food security among individuals experiencing homelessness. Taken together, our findings contribute to a growing body of literature indicating the difficulties of achieving food security among individuals experiencing homelessness.
To our knowledge, ours is the first study to examine the impact of a supported housing intervention on food security in a sample of participants experiencing homelessness and mental illness. We hypothesized that access to housing would improve food security among HF participants by providing them with access to kitchen facilities where they can prepare and store food. Taking advantage of the longitudinal nature of our data, we documented that over half of our sample was able to achieve marginal to high food security at least one time over the 18-month period. Moreover, about one-fifth of participants in both treatment arms achieved moderate to high food security throughout the follow-up period. Interestingly, only within the HN group did those in the HF arm show greater improvements in food security over the 18 months of follow-up compared with those in the TAU arm.
Our findings show that the rate of achieving high or marginal food security was higher in the HF group compared with the TAU group in only two of the five study sites that had an HN group (Moncton and Toronto). This is not surprising given that each site had unique contexts and populations. For example, in Winnipeg, the majority of participants were of Aboriginal background and in Toronto the sample comprised a large proportion of ethno-racial and non-Canadian-born participants. There are several additional reasons for variation in intervention effects across sites. Although all study sites achieved high levels of fidelity to the HF programme model( Reference Nelson, Stefancic and Rae 45 ), variation may have existed in the implementation of the HF intervention and it is likely that the ability of support teams to refer clients to services related to food security was not uniform. Site differences may also have arisen from heterogeneity in the composition of the homeless population and food landscapes in each community, including availability of affordable or accessible healthy food options. Moreover, participants in the TAU arms were not precluded from obtaining housing throughout the study period and some were successfully housed via existing programmes and services; however, HF participants in both need level groups were able to achieve greater housing stability compared with their TAU counterparts( Reference Stergiopoulos, Hwang and Gozdzik 33 , Reference Aubry, Goering and Veldhuizen 46 ).
It is also unclear to what extent our results are driven by other factors related to food security that were not assessed in our study such as household size, proximity to relevant resources and expenditures( Reference Weiser, Frongillo and Ragland 19 , Reference Furness, Simon and Wold 47 ). HF was unable to and did not seek to fully alleviate poverty, which may be an additional explanation for our findings. Social protection programmes, which include social assistance, social insurance and labour market protection, may be better equipped to address the multidimensional factors surrounding poverty and deprivation and may have a more tangible effect on food security in this population( 48 ). Moreover, it is also plausible that the HF intervention may not directly influence food security. In our sample, regardless of the treatment arm, over half of the participants achieved a high food security level at least once during the four follow-up visits. It is also important to note, however, that the US FSSM only captures food security arising from economic constraints( 2 , 40 , 41 ), and we are therefore unable to comment on whether the HF intervention was able to improve the physical and social domains of our participants’ food security. Further research is required to examine how these and other factors impact and improve food security.
Although our study has notable strengths (e.g. large sample size, longitudinal follow-up, diverse study sites, use of a validated food security measure), it also had the following limitations. Recall bias may have influenced the accuracy of participants’ self-reported data. Because participants received an honorarium for their participation, we cannot dismiss that this incentive may have also biased their answers. Given that all participants had to be experiencing severe mental illness with or without a concurrent substance use problem in order to be eligible for the study, our findings may not be generalizable to the entire homeless population. Blinding of interviewers and participants to their randomization was not possible due to the nature of the intervention and may have also resulted in biased estimates of treatment effects( Reference Karanicolas, Farrokhyar and Bhandari 49 ).
In summary, food security was low among individuals experiencing homelessness and mental illness in the At Home/Chez Soi study and was associated with demographic variables and mental health and substance use problems. Although few participants achieved food security throughout the follow-up period, our findings suggest that an HF intervention does result in higher rates of food security compared with usual care over an 18-month study period, especially among HN individuals. Differences in the treatment effect across study sites indicate that variation between cities in terms of study population characteristics and food landscapes may play a factor. Food security continues to be a significant issue in Canada that requires coordinated and effective policies and programmes to ensure that homeless individuals with severe mental illness have adequate access to food assistances programmes and income for food.
Acknowledgements
Acknowledgements: The authors would like to thank the following for their contribution to this project and the research: Dr Jayne Barker (2008–2011), Cameron Keller (2011–2012) and Catharine Hume (2012–present), Mental Health Commission of Canada At Home/Chez Soi National Project Leads; Dr Paula Goering, the National Research Lead; the National Research Team, the five site research teams, the Site Coordinators, and the numerous service and housing providers; as well as the persons with lived experience. Financial support: This research was supported by the Mental Health Commission of Canada, via funds from Health Canada. The views expressed herein solely represent the authors. Conflict of interest: None. Authorship: P.O. and S.W.H. designed the study. All authors contributed to the formulation of the research questions, study design and interpretation of the empirical results. P.O., S.W.H., A.S., A.G. and L.I.P.L. planned the statistical analysis. L.I.P.L. performed all statistical analyses. P.O., A.S. and A.G. wrote the original draft and all authors provided comments and corrections on manuscript versions. All authors read and approved the final manuscript draft. Ethics of human subject participation: This study was conducted according to the guidelines laid down in the Declaration of Helsinki and all procedures involving human subjects were approved by the institutional research ethics boards (REB) at each study site (University of Moncton REB in Moncton; Douglas Mental Health University Institute REB in Montreal; St. Michael’s Hospital REB in Toronto; University of Winnipeg REB in Winnipeg; Simon Fraser University REB in Vancouver). All participants received information on the study and provided their written informed consent. Trial registration: The study was registered with the International Standard Randomized Control Trial Number (ISRCTN) 42520374 on 18 August 2009.











