Introduction
Long considered to be specific for autism spectrum disorders (ASDs), impairing restrictions in reciprocal interpersonal interaction and communication have been reported in groups diagnosed with schizophrenia (Owen et al. Reference Owen, O'Donovan, Thapar and Craddock2011), bipolar disorder (Ståhlberg et al. Reference Ståhlberg, Söderström, Råstam and Gillberg2004), obsessive-compulsive disorder (OCD) (Bejerot et al. Reference Bejerot, Nylander and Lindström2001), antisocial behaviour disorder (Siponmaa et al. Reference Siponmaa, Kristiansson, Jonsson, Nydén and Gillberg2001), personality disorders (PDs) (Anckarsäter et al. Reference Anckarsäter, Ståhlberg, Larson, Håkansson, Jutblad, Niklasson, Nydén, Wentz, Westergren, Cloninger, Gillberg and Råstam2006) and anorexia nervosa (AN) (Wentz Nilsson et al. Reference Wentz Nilsson, Gillberg, Gillberg and Råstam1999). The available literature does not permit conclusions on whether to regard such sociocommunicative problems as an ‘endophenotype’, carrying susceptibility for a wider range of mental disorders, as a ‘co-morbidity’ with ASD, or as a by-product of the pathological processes defined by the mental disorder. Recent studies have demonstrated common genetic effects behind conditions previously considered independent, such as ASDs and attention deficit hyperactivity disorder (ADHD), tics, motor dyscoordination and learning disorder (Lichtenstein et al. Reference Lichtenstein, Carlström, Råstam, Gillberg and Anckarsäter2010; Lundström et al. Reference Lundström, Chang, Kerekes, Gumpert, Råstam, Gillberg, Lichtensten and Anckarsäter2011). The understanding of the clinical phenotype of patients having neurocognitive sociocommunicative restrictions, including convergence with diagnostic criteria for ASDs and PDs and to concepts of personality traits and cognitive functioning, is therefore a challenge for psychiatric research across adult diagnostic categories (further information on AN and this clinical problem constellation is provided in the Supplementary online material).
A ‘social cognitive phenotype’ was recently proposed to characterize a subgroup of subjects with AN (Zucker et al. Reference Zucker, Losh, Bulik, LaBar, Piven and Pelphrey2007). Two major studies have so far described a subgroup of AN subjects with clear ASDs (Råstam et al. Reference Råstam, Gillberg and Wentz2003; Wentz et al. Reference Wentz, Lacey, Waller, Råstam, Turk and Gillberg2005). Studies applying psychological tests have yielded conflicting findings. ‘Theory of mind’ tests in women recovered from AN found significant abnormalities (Russell et al. Reference Russell, Schmidt, Doherty, Young and Tchanturia2009) or only slight impairments after recovery (Oldershaw et al. Reference Oldershaw, Hambrook, Tchanturia, Treasure and Schmidt2010). Another study found poor emotional recognition in AN (Kucharska-Pietura et al. Reference Kucharska-Pietura, Nikolaou, Masiak and Treasure2004), most marked for negative face emotions, and for positive and negative voice emotions. Indications of a link between eating disorders and ASDs may also be found in the autism literature. Eating problems, such as feeding difficulties or over-eating, phobic aversion of foods with specific features and selective eating, are clinically important associated features in many cases of ASD (Råstam, Reference Råstam2008).
Personality (and its disorders) has traditionally been construed as partly the result of variation in cognitive and interpersonal skills (Cloninger et al. Reference Cloninger, Svrakic and Przybeck1993). In AN, a personality profile including restrictions in the ability to identify and describe emotional states, referred to as alexithymia, has been identified (Taylor et al. Reference Taylor, Bagby and Parker1993), and this is probably most typical of the AN subgroup with empathy problems or ASDs (Råstam et al. Reference Råstam, Gillberg, Gillberg and Johansson1997). Normal-intelligence adults with ASD often meet Diagnostic and Statistical Manual of Mental Disorders (DSM) criteria for anxious PDs [i.e. avoidant, dependent, and obsessive-compulsive PD (OCPD)] and describe a personality structure with low reward dependence, high harm avoidance, and an immature character profile in Cloninger's temperament and character model (Anckarsäter et al. Reference Anckarsäter, Ståhlberg, Larson, Håkansson, Jutblad, Niklasson, Nydén, Wentz, Westergren, Cloninger, Gillberg and Råstam2006; Hofvander et al. Reference Hofvander, Delorme, Chaste, Nydén, Wentz, Ståhlberg, Stopin, Anckarsäter, Gillberg, Råstam and Leboyer2009).
We recently published data on psychiatric health and predictors of long-term outcome 18 years after AN onset in adolescence. The study was initiated in the mid-1980s, and the AN group and their matched comparison cases have now been examined on four occasions (for details, see Wentz et al. Reference Wentz, Gillberg, Anckarsäter, Gillberg and Råstam2009). Poor overall outcome [Morgan–Russell assessment schedule, the Global Assessment of Functioning (GAF) scale] was predicted by pre-morbid OCPD, age at AN onset, and autistic traits in childhood. At 18 years after AN onset, neurocognitive tests showed problems in all domains studied (attention, executive function and mentalizing), independent of current body mass index (BMI), current eating disorder, or the length of the eating disorder, and there was a considerable AN subgroup (21%) with slow processing in mentalizing tasks and working memory tasks (Gillberg et al. Reference Gillberg, Billstedt, Wentz, Anckarsäter, Råstam and Gillberg2009).
The aims of the present report on this longitudinal population-based controlled follow-up study of AN were to: (1) replicate previous findings of over-representation of ASDs and PDs in AN, (2) provide details on specific ASD symptoms, personality profiles, neurocognition and outcome in the AN+ASD subgroup, and (3) assess whether sociocommunicative problems are also over-represented among AN subjects without an ASD diagnosis.
Method
Earlier assessments
A total of 51 subjects (three men and 48 women) with adolescent-onset AN according to the DSM-III-R (and subsequently to the DSM-IV) criteria (AN group) were originally recruited in a screening of all schools in Gothenburg using individual physical examinations, analysis of growth charts and an eating disorders questionnaire (Råstam et al. Reference Råstam, Gillberg and Garton1989; Råstam, Reference Råstam1992).
Half the AN group consisted of all adolescents with AN from a total population cohort (except for one) born in 1970 and living in the city of Gothenburg, Sweden, in 1985. This group (22 girls and two boys) was pooled with another group of individuals with AN (26 girls and one boy), recruited at the same time from the same schools, consisting of individuals not born in 1970, but in adjacent years. The two groups were similar in virtually all aspects other than treatment received, and were pooled to constitute the AN group. The comparison group (COMP group) had been selected by the same school nurses and consisted of 51 healthy individuals without any suspicion of eating problems, matched for age, gender and school. All 51 AN subjects and 51 COMP subjects were exam-ined in depth together with their mothers at the mean age of 16 years in the original study, AN Study I, including a structured interview with the mothers on perinatal factors and subsequent development in infancy and childhood by milestones and possible medical and/or other adjustment problems, performed in 1985 or the following years (Råstam, Reference Råstam1992). The developmental history was completed by scrutinizing pregnancy, obstetrical, child health and school medical records, which are excellent in Sweden. This work, including diagnoses of DSM-III-R PDs – especially childhood schizoid traits according to the terminology of Wolff (Reference Wolff2004) – and ASDs assigned on the basis of de-identified case notes on pre-morbid history, is described in detail by Råstam (Reference Råstam1992). The whole study group was subsequently followed up after 6 years (at mean age 21 years, AN Study II; Gillberg et al. Reference Gillberg, Råstam and Gillberg1995), 10 years (at mean age 24 years, AN Study III; Wentz Nilsson et al. Reference Wentz Nilsson, Gillberg, Gillberg and Råstam1999), and, in the present study, 18 years after the onset of AN (at mean age 32 years, AN Study IV; Wentz et al. Reference Wentz, Gillberg, Anckarsäter, Gillberg and Råstam2009), each study comprising clinical assessments by a new clinician blinded to previous assessments and to AN/COMP status, which was possible as >90% of AN subjects were normal-weight at follow-up.
Present study – AN Study IV
All 51 individuals in the AN group and their 51 COMP subjects were followed up in AN Study IV of which 45 AN subjects agreed to a personal interview and five were interviewed over the phone. For one AN subject, the mother did not want us to see her daughter, who had persisting AN, but agreed to a collateral interview with the semi-structured instruments used with the other subjects. Two more women had AN at the time of the present study, but the rest of the AN group were normal-weight, and the majority had been weight-restored already at AN Study II. Three women were diagnosed with a persisting eating disorder with normal-weight (for details, see Wentz et al. Reference Wentz, Gillberg, Anckarsäter, Gillberg and Råstam2009). All 51 COMP subjects participated in AN Study IV. Forty-eight were interviewed in person and three over the phone.
Diagnostic procedures
The psychiatric diagnostics was based on the Structured Clinical Interview for DSM-IV Axis I (SCID-I) (First et al. Reference First1997a ) and the Cluster C module of the SCID-II (targeting the ‘anxious’ PDs, First et al. Reference First1997b ) clinical interviews for DSM axis I and II diagnoses (the prevalences of cluster A and B disorders, i.e. ‘aloof’ and ‘dramatic’ PDs, had been very low in the previous phases). Sociocommunicative problems were assessed by the Asperger Syndrome Diagnostic Interview (ASDI), which contains 20 specific interview questions or expert ratings exploring each of the six Gillberg and Gillberg research criteria for Asperger's disorder/high-functioning autism (Gillberg et al. Reference Gillberg, Gillberg, Råstam and Wentz2001). Three ratings are possible: ‘does not apply’ (coded as 0), ‘probably applies to some extent’ (coded as 0.5), and ‘applies definitively’ (coded as 1), giving sum scores for each criterion and for the whole interview (with a maximum score of 20). The ASDI includes a number of observational items, especially for verbal and non-verbal communication, which are systematically observed and rated. Further findings of perceptual and psychomotor aberrations were systematically documented. Based on all the available information provided during the interview, the 12 DSM-IV symptom criteria for autistic disorder (A1–A3 a–d) and categorical diagnoses according to the DSM-IV were assessed in a last step. While the DSM-IV algorithms for autistic disorder and Asperger's disorder are relatively clear-cut and require specific constellations of symptoms (⩾6 items for autistic disorder and ⩾3 items for Asperger's disorder, both with specific distributions across the three domains), the pervasive developmental disorders not otherwise specified (PDD NOS) diagnosis may be assigned based on impairment in the development in reciprocal social interaction with either communication problems or stereotyped behaviours, meaning that there should be at least two A1 symptoms or one A1 and one other symptom item and that the overall impairment is considered sufficient for a mental disorder (APA, 1994). As the interviewer was blinded to previous diagnostic assessments, the rating of the ASD criteria only focused on the present time-frame and the information provided by the subjects themselves during the course of the interview. All subjects were carefully instructed not to provide any information on eating habits, which thus were not assessed along with other ritualistic behaviours.
The Morgan–Russell outcome interview (Ratnasuriya et al. Reference Ratnasuriya, Eisler, Szmukler and Russell1991) provided an averaged composite score summarizing outcome data on body weight, diet restriction, menstruation, attitude to sex and menstruation, social relationships, relationship with family and mental state.
Self-rating instruments
The self-ratings included the Autism Spectrum Quotient (AQ) (Baron-Cohen et al. Reference Baron-Cohen, Wheelwright, Skinner, Martin and Clubley2001), the Temperament and Character Inventory (TCI) (Cloninger et al. Reference Cloninger, Svrakic and Przybeck1993), and questions assessing criteria for ADHD, and tics according to the DSM-IV algorithms. The AQ is a self-report instrument designed to measure the degree, on a continuum, to which an individual has traits associated with the ASDs. It comprises 50 questions, divided into five areas: social skills, attention switching, attention to detail, communication, and imagination. The TCI assesses the following personality dimensions: harm avoidance (HA), novelty seeking (NS), reward dependence (RD), persistence (P), self-directedness (SD), cooperativeness (C), and self-transcendence (ST). Raw scores for each dimension and its subscales were transformed into T-scores by comparison with gender- and age-matched norm groups (Brändström et al. Reference Brändström, Schlette, Przybeck, Lundberg, Forsgren, Sigvardsson, Nylander, Nilsson, Cloninger and Adolfsson1998).
Neurocognitive tests
The neuropsychological assessments performed in AN Study IV included tests of attention and working memory using the Wechsler Adult Intelligence test III (Wechsler, Reference Wechsler1997), computerized measures of attention processes with the Test of Variables of Attention (TOVA; Greenberg & Waldman, Reference Greenberg and Waldman1993), the Tower of London (Shallice, Reference Shallice1982) test of executive functions, especially planning and organization, and the mental and non-mental cartoons test by Happé (Gallagher et al. Reference Gallagher, Happé, Brunswick, Fletcher, Frith and Frith2000), as described in Gillberg et al. (Reference Gillberg, Billstedt, Wentz, Anckarsäter, Råstam and Gillberg2009).
Statistical analyses
Mann–Whitney U tests were used to test for differences between two groups and the Kruskal–Wallis test for differences between three groups in continuous variables. Fisher's exact χ2 test was used to compare differences between the AN subgroups in frequencies of coexisting axis I and II disorders. Correlations were calculated by the Spearman rank method. The non-parametric tests were used due to the skewed non-normal distributions of the samples. For analyses of diagnostic agreement across assessments, Cohen's κ were calculated. All p values are two-tailed, and significance was considered at the 5% level for the hypothesis-based group comparison.
Ethics
The study was approved by the regional ethical review board at the University of Gothenburg (register no. Ö 529-02). The subjects participated voluntarily after giving their informed consent.
Results
ASDs in AN subjects as compared with COMP subjects in the present study – AN Study IV
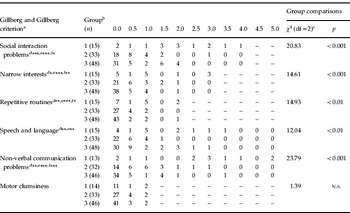
AN subjects more often met DSM ASD criteria and had higher ASDI scores as compared with COMP subjects (Table 1), a difference that was statistically significant for social interaction problems, stereotype interests, routines and rituals, and non-verbal communication. The total number of DSM-IV autistic disorder criteria (A1–A3 a–d) ranged from 0 to 7 out of 12. Fourteen AN subjects met criteria for an ASD (autistic disorder in one subject, Asperger's disorder in four, and PDD NOS in nine) as compared with one COMP subject (PDD NOS). Seven AN subjects and one COMP subject met four or more DSM-IV ASD criteria. Seventeen AN subjects and five COMP subjects clinically fulfilled the social interaction criterion, three AN subjects v. zero COMP subjects the communication criterion, and 14 AN subjects v. two COMP subjects the lack of flexibility criterion. All three DSM-IV domains differed significantly between AN subjects and COMP subjects (exact distributions are given in Table 1).
Table 1. Distribution and comparison of DSM-IV criteria in the two AN groups and the COMP group

DSM-IV, Diagnostic and Statistical Manual of Mental Disorders; AN, anorexia nervosa; COMP, comparison; df, degrees of freedom; ASD, autism spectrum disorder.
a For each subcriterion, 0.5 was assigned when ‘applies to some extent’ and 1.0 when ‘applies fully’.
b 1=AN+ASD, 2=AN-ASD, 3=COMP.
c Kruskal–Wallis test.
d AN+ASD v. AN-ASD.
e AN+ASD v. COMP.
f AN v. COMP.
* p<0.05, ** p<0.01, *** p<0.001 (Mann–Whitney U test).
Three additional subjects had been assigned an ASD diagnosis at one of the previous waves of the study, but were now considered as no longer meeting criteria for an ASD. In total, 17 AN subjects and one COMP subject had been assigned an ASD diagnosis in at least one of the four studies (I–IV), and six subjects had ASDs at all four studies. In one subject, the ASD was not diagnosed until after life events had had an impact on brain functioning. Empathy problems had been noted earlier, but after suffering a severe traumatic brain injury at about 20 years of age, she has repeatedly displayed social interaction problems considered to correspond to a PDD NOS. In addition, the COMP subject who was assigned a diagnosis of PDD NOS in the two most recent follow-up studies had suffered a severe cannabis-related psychotic episode before reporting symptoms considered as an ASD. These two subjects were omitted from further analyses in this report, as their social interaction problems had clear adult-age exogenous causes (even if these by all means may have acted on an underlying susceptibility), leaving a subgroup of 16 out of 50 AN subjects (32%) assigned an ASD diagnosis in at least one study within the project (referred to as the AN+ASD group in the following sections, while the AN subjects who had never been assigned an ASD diagnosis will be referred to as the AN-ASD group).
Seven AN subjects with ASD diagnoses assigned in the later studies within the project had been diagnosed with Tourette's disorder, OCD and/or OCPD at one or several previous studies. One of two subjects with Asperger's disorder at AN Study I and II was not found to have an ASD in any of the two following studies, while the other had Asperger's disorder at AN Study III but only autistic-like traits in AN Study IV. Both these subjects had created social situations ‘congruent with’ their personalities.
ASD diagnoses in the last study that were blind to previous assessments agreed with ASD diagnoses in AN Study III about 8 years earlier with a Cohen's κ=0.75 and with AN Study II about 12 years earlier with a κ=0.70, while the agreement with the pre-morbid diagnoses recorded at AN Study I were considerably lower, κ=0.23. The agreement between ASD diagnoses in AN Study II and AN Study III, which were made with 6 years in between, was at κ=0.80.
Subthreshold autistic-like traits, considered to be part of the normal variation rather than a pathological condition, were equally common in the AN (9/51) and the COMP group (10/51).
According to the SCID-II interviews, five AN subjects and zero COMP subject met criteria for avoidant PD. Five AN subjects and two COMP subjects met criteria for OCPD. No subject met criteria for a dependent PD. AN subjects met significantly more SCID-II criteria for avoidant PD and OCPD than COMP subjects (p=0.004 and 0.004, respectively).
ASD symptoms, personality profiles, neurocognition and prognosis in the AN+ASD group
According to the DSM-IV, the AN+ASD group had their most pronounced problems in social interaction and lack of flexibility (non-verbal communication deficits form a part of the social interaction criterion). These subjects also met Gillberg and Gillberg criteria for non-verbal communication problems, narrow interests and routines and rituals (Table 2). In contrast, verbal communication problems were only present in a few subjects and did not characterize the AN+ASD group as a whole.
Table 2. Distribution and comparison of Gillberg and Gillberg criteria in the two AN groups and the COMP group
AN, Anorexia nervosa; COMP, comparison; df, degrees of freedom; n.s, non-significant; ASD, autism spectrum disorder.
a For each subcriterion, 0.5 was assigned when ‘applies to some extent’ and 1.0 when ‘applies fully’.
b 1=AN+ASD, 2=AN-ASD, 3=COMP.
c Kruskal–Wallis test.
d AN+ASD v. AN-ASD.
e AN+ASD v. COMP.
f AN v. COMP.
* p<0.05, ** p<0.01, *** p<0.001 (Mann–Whitney U test).
The self-rating instruments AQ and TCI were compared across AN subjects with or without ASDs and COMP subjects (Tables 3 and 4). There were significant group differences between the AN and the COMP groups for all AQ scores (the only exception being imagination, with a borderline p value just above the 0.05 significance level) and for several personality dimensions according to the TCI, especially novelty seeking and self-directedness. However, novelty seeking was unexpectedly high in the COMP group.
Table 3. Distribution and comparison of personality traits according to the Autism Spectrum Quotient in the two AN groups and the COMP group
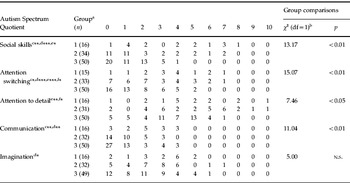
AN, Anorexia nervosa; COMP, comparison; df, degrees of freedom; n.s, non-significant; ASD, autism spectrum disorder.
a 1=AN+ASD, 2=AN-ASD, 3=COMP.
b Kruskal–Wallis test.
c AN+ASD v. AN-ASD.
d AN+ASD v. COMP.
e AN v. COMP.
f AN-ASD v. COMP.
* p<0.05, ** p<0.01, *** p<0.001 (Mann–Whitney U test).
Table 4. Personality traits according to the TCI in the two AN groups and the COMP group
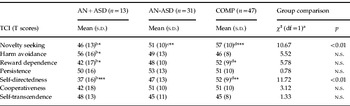
TCI, Temperament and Character Inventory; AN, anorexia nervosa; COMP, comparison; ASD, autism spectrum disorder; s.d., standard deviation; df, degrees of freedom; n.s, non-significant.
a Kruskal–Wallis test.
b AN+ASD v. COMP.
c AN-ASD v. COMP.
d AN v. COMP.
* p<0.05, ** p<0.01, *** p<0.001 (Mann–Whitney U test).
Similar analyses were subsequently performed for results on the neurocognitive tests. Again, AN+ASD subjects differed from COMP subjects, most significantly on arithmetic, total Tower of London, TOVA commission score, and Happé's mental cartoons, with the AN-ASD group generally scoring between the AN+ASD and the COMP groups (Table 5). The TOVA omission results of the three groups had suspicious similarities but after thorough controls we concluded that these results were correct and the identical medians and range scores were probably due to restricted norm groups in this age span.
Table 5. Group differences on neuropsychological variables between the three groups
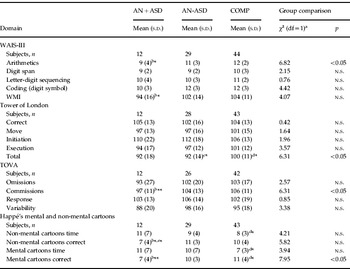
AN, Anorexia nervosa; ASD, autism spectrum disorder; COMP, comparison; s.d., standard deviation; df, degrees of freedom; WAIS-III, Wechsler Adult Intelligence test III; n.s, non-significant; WMI, working memory index; TOVA, Test of Variables of Attention.
a Kruskal–Wallis test.
b AN+ASD v. COMP.
c AN-ASD v. COMP.
d AN v. COMP.
e AN+ASD v. AN-ASD.
* p<0.05, ** p<0.01 (Mann–Whitney U test).
The AN+ASD group did not differ from the AN-ASD group in age at onset, minimum BMI or co-existing mental disorders (even if avoidant and OCPD tended to be somewhat over-represented (20% v. 6% and 12%, respectively). Morgan–Russell scores were significantly lower in the AN+ASD group (mean 9 v. 10, p<0.01, Mann–Whitney U test).
Sociocommunicative problems in the non-ASD AN group (AN-ASD)
The AN subjects who had never been assigned an ASD diagnosis nevertheless had higher ASDI scores than the COMP subjects for the fifth Gillberg and Gillberg criterion non-verbal communication problems (Table 2). These subjects also scored in between the AN+ASD group and the COMP subjects in personality scales (besides novelty seeking, in which they were lower than the AN+ASD and the COMP groups), and differed significantly from the COMP group on the total AQ score and on the subscores for attention switching and attention to detail (Table 3), and in Tower of London total score (Table 5). In all neurocognitive scales that differed significantly between the AN+ASD and COMP groups, the AN-ASD group scored in between the two other groups (even if these differences did not reach statistical significance).
Discussion
This report has used a longitudinal, community-based, controlled study of adolescent-onset AN to describe the sociocommunicative deficit subgroup in AN with regard to clinical symptoms, personality, neurocognition and prognosis. Longitudinally, ASD and related problems were assessed at four consecutive time points over a period of 18 years, each time by new clinical raters, blinded to previous assessments. All four waves of the project identified an important minority among AN subjects with social communication deficits corresponding to DSM-IV definitions of ASD and/or the Gillberg and Gillberg research criteria for Asperger's disorder, in total about a third who at least once was diagnosed with an ASD, and about one in nine having severe ASDs recognized as such by four independent clinicians and present prior to AN onset. The inter-rater consistency of these assessments was remarkable in view of the long time between assessments, showing that sociocommunicative problems may be diagnosed reliably in adults without access to collateral or other types of information on childhood development. In spite of the overall consistency, it was clear, however, that subclass diagnoses within the autism spectrum (i.e. ‘classic’ autism, Asperger's disorder or PDD NOS) have much less consistency, and that the differentiation from OCPD and other OCD-related clinical presentations and from autistic-like traits is, to some extent, arbitrary (Chasson et al. Reference Chasson, Timpano, Greenberg, Shaw, Singer and Wilhelm2011). The notion that the sociocommunicative problems were indeed autism-related may to some extent be supported by previous findings of alexithymia, that is an autism-related restriction in developing meta-psychological concepts, in this group (Råstam et al. Reference Råstam, Gillberg, Gillberg and Johansson1997; Silani et al. Reference Silani, Bird, Brindley, Singer, Frith and Frith2008) and of broader sociocommunicative problems in first-degree relatives of subjects in this group (Wentz Nilsson et al. Reference Wentz Nilsson, Gillberg and Råstam1998). In the absence of a clear understanding of the pathophysiology or cognitive deficits behind mental disorders, it is, however, not possible to conclude whether the clinical, personality and neurocognitive features reported here are ‘truly’ autistic or rather features derived from the underlying psychology of the AN (if such a distinction can be made). OCPD has been the only PD consistently over-represented in the AN group across all four phases of the present project. The overlap between ASDs and OCPD has recently been the subject of a large number of studies (e.g. Rydén & Bejerot, Reference Rydén and Bejerot2008; Hollander et al. Reference Hollander, Kim, Braun, Semeon and Zohar2009).
The present study is rare in presenting repeated assessments of ASDs in a comparatively large group consisting both of subjects initially identified with a mental disorder and controls, and supports the usefulness of ASD diagnoses to identify subjects with significant sociocommunicative problems. It also shows that such problems may both remit over time with successful social adaptation and develop after brain injuries. Once the ASDs were accounted for, subthreshold autistic-like traits were not more common among the ‘ASD-negative’ AN cases than among controls. Such traits can be regarded as personality traits (Briskman et al. Reference Briskman, Happé and Frith2001; Constantino & Todd, Reference Constantino and Todd2003), and our prevalence rates resemble those of PDs reported in healthy subjects (Torgersen et al. Reference Torgersen, Kringlen and Cramer2001). It is, however, noteworthy that also the ASD-negative AN subgroup described themselves as more autistic-like than controls in the AQ (two subscores and the total score).
All individual DSM and Gillberg and Gillberg ASD criteria were more common in AN subjects, apart from verbal peculiarities and motor clumsiness. That the latter difference did not reach statistical significance may be due to the small range of variation in the ASDI scale. The lack of difference in verbal peculiarities might be related to the relatively high number of female study participants, considering that ASDs in women are less often characterized by the ‘Asperger-typical’ pedantic, stiff and formalistic verbal communication.
The ‘social cognitive phenotype’ in clinical groups with AN or other mental disorders has not yet been sufficiently studied in order to establish specific diagnostic instruments. As proxies, scales that assess Asperger's disorder criteria (such as the ASDI) or cognitive styles associated with the ASDs (such as the AQ) come closest. Several such instruments have been used for the present long-term follow-up study and the convergence of ratings by different raters and the consistency of significant differences between the AN+ASD group and the other groups support that they may all be used to study the sociocommunicative phenotype in mental health research, and that even if a longitudinal, expert, all-data diagnosis according to the ‘LEAD principle’ (Üstün & Tien, Reference Üstün and Tien1995) remains the ‘gold standard’ to aim for in clinical research, the AQ and TCI provide results that may be interpreted in terms of the proposed phenotype or specific subgroup of sociocommunicative deficits in large-scale epidemiological studies.
The subgroup of six individuals who had a childhood history of ASDs or OCPD with marked autistic traits, and with a stable diagnosis of ASDs at every evaluation, had few peer relations as children and tended to be dependent on only one friend that they used as a role model, according to retrospective interviews with their mothers at the diagnostic study (Råstam, Reference Råstam1992). They were ambitious and ‘perfect’ little girls, while at the same time they were described as being stubborn with inexplicable outbursts. They would do bizarre things and seemed not to understand other people's perspective.
The TCI has previously been very useful in the study of personality variants associated with neurodevelopmental disorders such as the ASDs and ADHD (Anckarsäter et al. Reference Anckarsäter, Ståhlberg, Larson, Håkansson, Jutblad, Niklasson, Nydén, Wentz, Westergren, Cloninger, Gillberg and Råstam2006). A similar picture emerged here, where the AN+ASD subjects described themselves as the least mature in self-directedness, significantly lower than the controls in reward dependence and novelty seeking and higher in harm avoidance. It is, however, noteworthy that the AN subgroup without ASD did not differ from controls in TCI personality dimensions (besides a lower novelty seeking), but had lower Tower of London results, and significantly more non-verbal communication problems than controls, indicating that socio-communicative problems among subjects with AN are not restricted to the subgroup meeting diagnostic criteria for an ASD.
A wide range of neurocognitive tests has been established for the assessment of executive functions, including computer-based continuous performance tests. In comparison, it has proved more difficult to establish tests that measure social interaction and communication abilities. The AN group performed lower than controls on the cartoons test by Happé and co-workers (Gallagher et al. Reference Gallagher, Happé, Brunswick, Fletcher, Frith and Frith2000), which is currently one of the best tests in this field.
There are several limitations to this study. The first and most important is the small sample size. The advantages provided by its representativeness and the longitudinal diagnostics are partly outweighed by the limited number of subjects, which precludes generalized conclusions, especially as regards the ‘negative’ comparisons that did not yield significant differences between the AN groups with or without ASD and the controls. Even if population representativeness is often taken to indicate quality in research, it has to be remembered that it does not mean representativeness for clinical groups. For example, regardless of whether it is most ‘true’, the degree of co-existing problems is often higher in population-based studies than in clinical groups. The instruments used for our study have comparatively small sets of published validation data and were developed and validated mostly on boys. The neurodevelopmental collateral interviews and file-reviews performed in the first phase of the study used standardized check-lists accepted at the time but would now have been performed by the Autism Diagnostic Interview (LeCouteur et al. Reference LeCouteur, Rutter, Lord, Rios, Robertson, Holdgrafer and McLennan1989) or the Diagnostic Interview for Social and Communication (Wing et al. Reference Wing, Leekam, Libby, Gould and Larcombe2002). For the present phase of the study, however, it would not have been feasible to include either of these instruments (as the clinical information was collected from the adult subjects themselves). Another limitation is that the adult Autism Diagnostic Observation Schedule (Lord et al. Reference Lord, Risi, Lambrecht, Cook, Leventhahal and DiLavore2000) was not used for structured observations instead of the observational items in the ASDI (Gillberg et al. Reference Gillberg, Gillberg, Råstam and Wentz2001). Several key areas of autistic symptoms were, however, systematically observed (verbal and non-verbal communication, neuromotor functioning, perceptual problems) and the use of independent clinicians (tested for convergence) and self-rate instruments in addition to clinical examinations may to some extent make up for the lack of instruments with tested inter-rater reliability. Better standardized tests of social interaction and non-verbal communication, preferentially in unstructured situations, are urgently needed in psychiatric research and diagnostics, including better adaptations for different developmental phases and adults and validated across genders.
Note
Supplementary material accompanies this paper on the Journal's website (http://journals.cambridge.org/psm).
Acknowledgements
This work was supported by the Swedish Research Council (K2006-21X-20048-01-2), government grants under the ALF agreement, Knut and Alice Wallenberg's Foundation, the SöderströmKönigska Nursing Home Foundation, the Swedish Medical Society, and the Göteborg Freemasons.
Declaration of Interest
None.









