Introduction
Vaccination is one of the most effective methods of preventing and controlling infectious diseases (Nichol et al., Reference Nichol, Lind, Margolis, Murdoch, McFadden and Hauge1995). However, despite the consensus in the scientific and public health communities about its effectiveness, millions of people die annually from vaccine-preventable diseases (Ehreth, Reference Ehreth2003). Influenza is a common vaccine-preventable disease, but the World Health Organization (WHO) estimates that between 290,000 and 650,000 people die globally from influenza-related respiratory deaths every year (WHO, 2020). Influenza cases and deaths are well-documented in middle- and high-income countries unlike in low-income countries where they largely go unreported due to multiple factors, including limited surveillance (Paget et al., Reference Paget, Spreeuwenberg, Charu, Taylor, Iuliano and Bresee2019). The WHO estimate is believed to be a conservative estimate of the global burden of the disease (Iuliano et al., Reference Iuliano, Roguski, Chang, Muscatello, Palekar and Tempia2018; Paget et al., Reference Paget, Spreeuwenberg, Charu, Taylor, Iuliano and Bresee2019). The disease impacts the economies and health care systems of both developing and developed countries. In Canada, an estimated 1.5 million workdays are lost annually due to influenza, resulting in health care costs and lost productivity of approximately CAD$1 billion (Canadian Healthcare Influenza Immunization Network, 2019), while in the United States, the economic burden of influenza on the health care system is estimated at US$11.2 billion annually (Putri, Muscatello, Stockwell, & Newall, Reference Putri, Muscatello, Stockwell and Newall2018). Increasing influenza vaccination (flu shot) coverage can reduce both influenza-related mortality and the economic burden of the disease by lowering the risks for pneumonia, hospitalization, and death (Casado et al., Reference Casado, Domínguez, Toledo, Chamorro, Astray and Egurrola2018; Gross, Reference Gross1995).
Although the influenza virus is self-limiting and most people recover from infection without medical intervention (Grohskopf et al., Reference Grohskopf, Alyanak, Broder, Walter, Fry and Jernigan2019), it can result in severe complications or even death in adults ages 65 years and older, and in people with chronic or underlying medical conditions (Nielsen et al., Reference Nielsen, Vestergaard, Richter, Schmid, Bustos and Asikainen2019; Wong et al., Reference Wong, Cheng, Foppa, Jain, Fry and Finelli2014). Studies have shown that both healthy older adults and older adults with chronic or underlying medical conditions benefit significantly from influenza vaccination (Nichol, Nordin, Nelson, Mullooly, & Hak, Reference Nichol, Nordin, Nelson, Mullooly and Hak2007; Nichol, Wuorenma, & Sternberg, Reference Nichol, Wuorenma and Sternberg1998). In Canada, the vaccination coverage for older adults ages 65 years and older is 70 per cent, compared with 34 per cent for individuals ages 18 to 64 years (Government of Canada, 2020). While vaccination coverage among older adults is generally high, it is still below the national Canadian target of 80 per cent (Buchan & Kwong, Reference Buchan and Kwong2016), thus there is a need to increase influenza vaccination coverage, especially among older adults.
Vaccination decision-making is influenced by several factors, including trust or mistrust in modern medicine, prior experience of vaccination, perceived risk of disease, and perceived effectiveness of vaccine and disease severity (Hoogink et al., Reference Hoogink, Verelst, Kessels, van Hoek, Timen and Willem2020; Telford & Rogers, Reference Telford and Rogers2003). A recent study of 5,014 Canadians ages 65 years and older showed that the most common reasons for abstaining from influenza vaccination were thinking that it was unnecessary and ineffective, concerns over side-effects, and dislike of injections (Andrew, Gilca, Waite, & Pereira, Reference Andrew, Gilca, Waite and Pereira2019). These factors are not limited to influenza vaccination; they are also likely to affect coronavirus disease (COVID-19) vaccine uptake (Deroo, Pudalov, & Fu, Reference Deroo, Pudalov and Fu2020). Factors that influence vaccination decision-making can equally influence health–care-seeking behaviours (Telford & Rogers, Reference Telford and Rogers2003), and one of the factors that influence health–care-seeking behaviour and influence vaccination rates is life satisfaction (Goel, Rosella, Fu, & Alberga, Reference Goel, Rosella, Fu and Alberga2018; Kim, Park, Sun, Smith, & Peterson, Reference Kim, Park, Sun, Smith and Peterson2014). Life satisfaction is defined as an individual’s satisfaction with aspects of their life, including housing, relationships, body image, autonomy, environment, perceived health, and many others (Nedjat et al., Reference Nedjat, Sahaf, Khankeh, Fadayevatan, Majdzadeh and Karimlou2018). These factors contribute to how individuals perceive their life satisfaction and quality of life. For example, social environment, older adults’ social environment plays a crucial role in their vaccine uptake. Older adults who live in co-housing communities have noted that it gave them a sense of community and belonging, which contributes to their quality of life and life satisfaction (Puplampu et al., Reference Puplampu, Matthews, Puplampu, Gross, Pathak and Peters2019). Similarly, in a cross-sectional study, Chiatti et al. (Reference Chiatti, Barbadoro, Lamura, Pennacchietti, Di Stanislao and D’Errico2011) showed that social support (the availability of assistance from partners, neighbours, and home helpers) significantly increased the odds of influenza vaccination among older Italians. The above highlight the importance of older adults’ environment in increasing both life satisfaction and vaccination coverage.
This study aims to investigate the relationship between life satisfaction status and recent history of influenza vaccination among older adults within the two years preceding the 2015–2016 Canadian Community Health Survey (CCHS). Previous research has shown that higher life satisfaction is associated with better overall health (Siahpush, Spittal, & Singh, Reference Siahpush, Spittal and Singh2008), increased well-being and health among older adults (Yamada, Kawamata, Kobayashi, Kielhofner, & Taylor, Reference Yamada, Kawamata, Kobayashi, Kielhofner and Taylor2010), increased self-care and utilization of health knowledge (Nedjat et al., Reference Nedjat, Sahaf, Khankeh, Fadayevatan, Majdzadeh and Karimlou2018), higher usage of preventive health care services (Kim, Kubzansky, & Smith, Reference Kim, Kubzansky and Smith2015), and engagement in health-promoting behaviours (Grant, Wardle, & Steptoe, Reference Grant, Wardle and Steptoe2009). Life satisfaction is determined by several factors (Celik, Celik, Hikmet, & Khan, Reference Celik, Celik, Hikmet and Khan2017; Ngoo, Tey, & Tan, Reference Ngoo, Tey and Tan2014; Prenda & Lachman, Reference Prenda and Lachman2001), which have also been shown to influence the rates of seasonal influenza vaccination (Crouse Quinn, Jamison, Freimuth, An, & Hancock, Reference Crouse Quinn, Jamison, Freimuth, An and Hancock2017; Okoli et al., Reference Okoli, Lam, Racovitan, Reddy, Righolt and Neilson2020; Portero de la Cruz & Cebrino, Reference Portero de la Cruz and Cebrino2020).
While evidence exists to support the association between life satisfaction and positive health behaviours and outcomes, little is known about the extent to which life satisfaction impacts influenza vaccination and vaccination recency among older adults. Given that Canada’s older adult population is growing rapidly, older adults are living longer, and they are expected to make up 23 per cent of Canada’s population by 2030 (Government of Canada, 2019a), knowledge of the determinants of influenza vaccination behaviour can inform public health interventions that are aimed at increasing vaccination coverage, particularly among older adults. We hypothesized that older adults with higher life satisfaction status would be more likely to have a recent history of influenza vaccination.
Methods
Study Design and Data Collection
The study is a secondary data analysis of an original survey data extracted from the 2015–2016 Canadian Community Health Survey (CCHS). The CCHS is a national cross-sectional survey that is conducted annually; it is aimed at providing information related to health status, health care utilization, and health determinants at the regional and provincial levels for surveillance and public health research (Statistics Canada, 2020). The 2015–2016 survey is representative of approximately 98 per cent of the Canadian population and includes Canadians 12 years of age and older living in the 10 provinces and 3 territories. Those excluded from the survey comprise persons living on reserves and other Aboriginal settlements, full-time members of the Canadian Forces, institutionalized population, children under the age of 12 years, and those living in foster care (Statistics Canada, 2019, 2020). A total of 109,659 individuals were interviewed over the phone in the 2015–2016 survey, representing a response rate of 59.5 per cent. The number of respondents and survey designed are meant to provide reliable population-level estimates of measured variables (Statistics Canada, 2020). A more detailed description of both the sampling and interviewing methods is available from Statistics Canada (2020).
Study Participants
The analytic sample included individuals ages 65 years and older who have complete data for whether they had a flu shot within the two years preceding the survey. Adults ages 65 years and older were the population of interest for this study because they are considered a high-risk group for complications or death from influenza (WHO, 2018; Wong et al., Reference Wong, Cheng, Foppa, Jain, Fry and Finelli2014). For both explanatory and outcome variables, invalid responses (Don’t Know, Refusal, Not Stated) were excluded from the analytic sample. Invalid responses were also excluded from the potential confounders of age, perceived health status, sex, income, and educational attainment. Of those who had complete data on recent vaccination status (the two years preceding the survey), 26,989 were ages 65 years and older, and 91.3 per cent of them provided valid responses to both explanatory and outcome variables (n = 24,647), while 8.6 per cent provided invalid responses (n = 2,342). An additional 2,223 of them provided invalid responses for the confounding variables, resulting in a final analytic sample of 22,424 individuals. The sample represented 83 per cent of eligible adults ages 65 years and older (Figure 1).
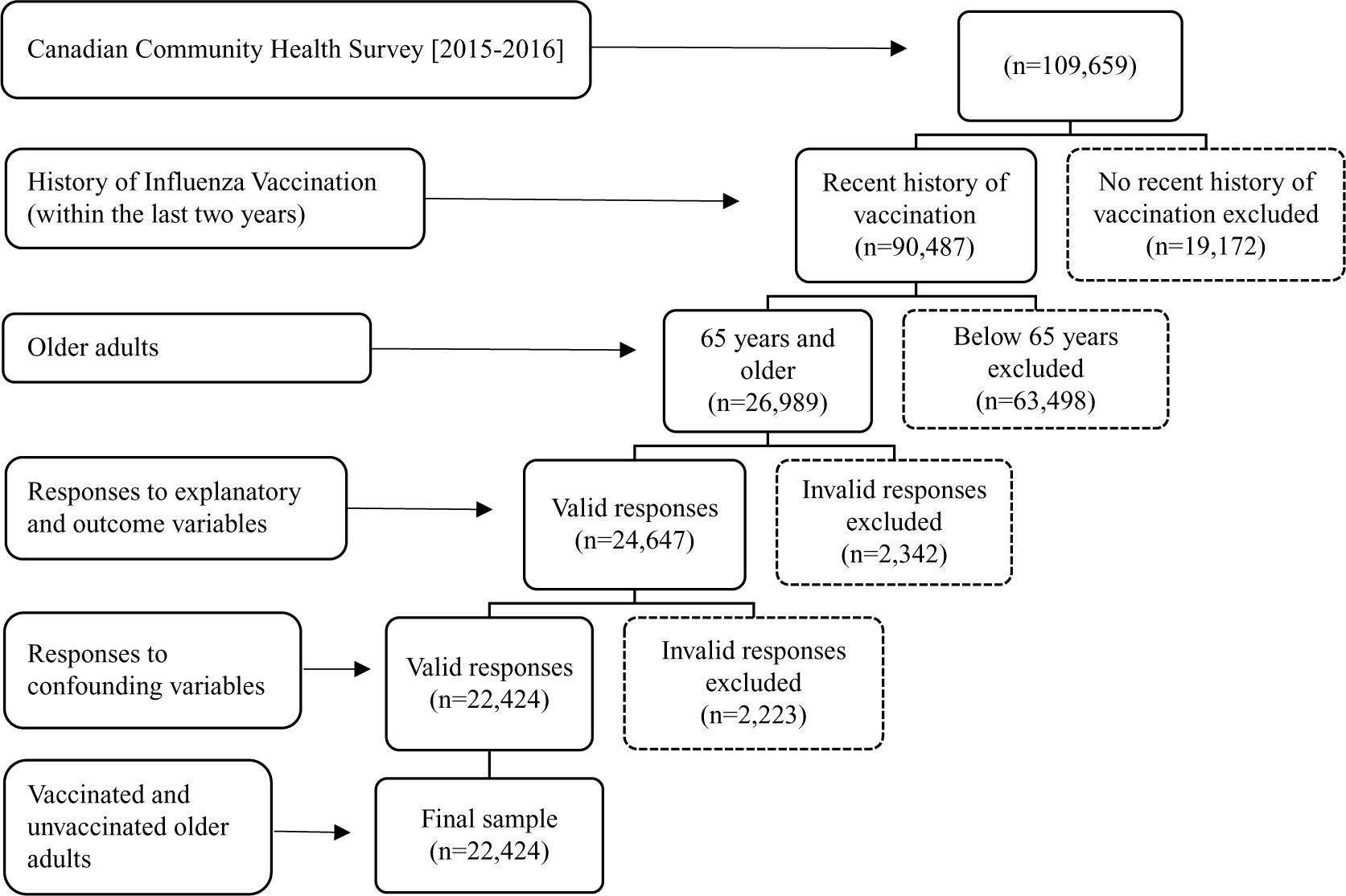
Figure 1. Selection of final sample from the 2015–2016 Canadian Community Health Survey (CCHS) for studying the relationship between life satisfaction status and influenza vaccination among older adults.
Measures
The outcome variable (influenza vaccination status) was categorized into two categories (“Yes” and “No”). The variable was derived from individuals who responded to questions about their recent influenza vaccination history. All respondents were asked the questions: Have you had the flu shot in the current or last year?, When did you have your last seasonal flu shot? Those who responded that they have received a flu shot in the current year, last year, and one year to less than two years ago were placed in the “Yes” category of the outcome variable. Individuals who responded that they have not received a flu shot within the last two years were placed in the “No” category of the outcome variable regardless of the reasons for not getting the flu shot.
The explanatory variable (life satisfaction status) consisted of five categories (“very satisfied”, “satisfied”, “neither satisfied nor dissatisfied”, “dissatisfied”, and “very dissatisfied”). The variable was derived by Statistics Canada, and proxy respondents were used in cases where people were not able to respond due to language barriers, physical, or cognitive limitations. The proxy responses accounted for 2.5 per cent (n = 2,695) of all survey responses. The explanatory variable was based on the self-reported level of life satisfaction for those who were able to respond to the survey and the level of life satisfaction as reported by the proxies. All responses were rated on a scale of 0 to 10, with 0 being “very dissatisfied” and 10 being “very satisfied”. The respondents were asked: How do you feel about your life as a whole right now? Those who rated themselves between 0 and 1 were placed in the “very dissatisfied” category, 2 to 4 were placed in the “dissatisfied” category, 5 in the “neither satisfied nor dissatisfied” category, 6 to 8 were placed in the “satisfied” category, and 9 to 10 in the “very satisfied” category.
Potential confounders of the relationship included self-reported health status (excellent, very good, good, fair, and poor), personal income (no income or income loss, <$20,000, $20,000-39,000, $40,000-59,000, $60,000-79,000, and $80,000+ in CAD), educational attainment (less than secondary, secondary, post-secondary), sex (men vs. women), and age group (65 to 69 years, 70 to 74 years, 75 to 79 years, 80 years and over).
Analysis
Data analysis was done using SAS Studio version 3.8 on SAS University Edition (SAS Institute, 2020). All statistics were weighted using sampling weights provided by Statistics Canada, to account for uneven selection probabilities and produce population-representative estimates. Study-specific ethics approval was covered by the University of British Columbia’s Policy Number LR9: Research Involving Human Participants, specifically Clause 1.3.1 governing the use of public release data for research (University of British Columbia, 2019). Following descriptive statistics examining the relationship between the explanatory and outcome variables and study sample characteristics, a logistic regression model was constructed to investigate the relationship between the outcome and explanatory variables (Starkweather & Moske, Reference Starkweather and Moske2011), adjusting for the effects of self-reported health status, income, educational attainment, sex, and age group. A sensitivity analysis was also performed by restricting the study sample to non-proxy respondents to understand the effect of proxy responses on the relationship between the outcome and explanatory variables.
Results
Descriptive Statistics
The study sample (n = 24,424) consisted of 54.9 per cent women and 45.1 per cent men. Within this sample, more respondents were ages 65 to 74 years (64.7%) than were ages 75 years and over. Thirty-five per cent of respondents reported an annual income in the CAD$20,000-39,000 bracket, and 16.8 per cent reported an income of CAD$60,000 and above. Additionally, a little over half (52.5%) of respondents reported post-secondary education as their highest level of educational attainment (Table 1). The prevalence of seasonal influenza vaccination in the study sample was 68.5 per cent. Most respondents reported that they were either satisfied (46.7%) or very satisfied (43.0%) with life.
Table 1. Characteristics of the sample of respondents ages 65 years and over for the relationship between life satisfaction and influenza vaccination within the last two years preceding the 2015–2016 CCHS

Logistic Regression Models
In the unadjusted model, no influenza vaccination within the last two years in the study sample was higher among those who reported being dissatisfied with life (OR 1.14; 95% CI: 0.82, 1.59) and very dissatisfied (OR 1.08; 95% CI: 0.67, 1.74) compared to those who reported being very satisfied (reference category). In the adjusted model, influenza vaccination within the last two years increased across all life satisfaction categories relative to the reference category (Table 2). Particularly, no influenza vaccination was highest for older adults who were dissatisfied with life (OR 1.70; 95% CI: 1.16, 2.51). For the confounding variables, women were more likely to be vaccinated (OR 0.81; 95% CI: 0.74, 0.90) compared to men, and the likelihood of vaccination increased with age (see Table 2). Compared to the reference category, older adults who reported being in poor health were more likely to have been vaccinated within the last two years (OR 0.34; 95% CI: 0.25, 0.46). Self-reported health status and age had the strongest confounding effect on the relationship between life satisfaction and influenza vaccination in the last two years. Self-reported health status alone increased the main effect by 16.1 per cent, and the two variables combined increased the main effect by 14.3 per cent. Finally, when proxy responses were removed, the likelihood of vaccination within the last two years remained unchanged across all categories.
Table 2. Regression models for the relationship between life satisfaction and influenza vaccination within the two years preceding the 2015–2016 CCHS for older adults ages 65 years and over

1 Adjusted for sex, age, self-reported health status, education, and income.
2 Not vaccinated within the two years preceding the survey.
Note: Values in bold represent associations that are of significance.
Discussion
The study investigated the relationship between life satisfaction and influenza vaccination among adults ages 65 years and older using the 2015–2016 Canadian Community Health Survey data. The results showed that older adults who reported being very satisfied with life had a more recent history of influenza vaccination compared to older adults who reported being dissatisfied or very dissatisfied. As the life satisfaction status of older adults improved from dissatisfied to very satisfied, the recency of influenza vaccination within the two years preceding the survey also increased. These findings suggest an association between life satisfaction status and influenza vaccination behaviour among older adults when adjusted for potential confounding variables such as sex, income, age, educational attainment, and self-reported health status.
The above findings are consistent with previous research, which has shown that high life satisfaction is associated with higher use of preventive health services (Kim et al., Reference Kim, Kubzansky and Smith2015), and that people with high life satisfaction generally engage in more healthy and health-improving behaviours, hence, they make fewer doctor visits compared to people with low life satisfaction (Kim et al., Reference Kim, Park, Sun, Smith and Peterson2014). The rationale is that the more satisfied older adults are with their lives, the more proactive they will be in maintaining or improving their overall health by adopting positive health behaviours and making use of available and recommended health care services (Strine, Chapman, Balluz, Moriarty, & Mokdad, Reference Strine, Chapman, Balluz, Moriarty and Mokdad2007). However, it is worth noting that the social determinants of health also influence people’s ability to access health care services. For example, people from marginalized communities, those who live in resource-limited settings, and those in lower-income brackets, all face significant challenges that affect both their health–care-seeking behaviours and ability to access health care services (Taylor & Haintz, Reference Taylor and Haintz2018). The above studies have helped explain differences in vaccination recency among older adults who reported being dissatisfied or very dissatisfied with life in our study sample compared with those who reported being satisfied or very satisfied and are more likely to be vaccinated.
The vaccination prevalence of 68.5 per cent in this study is relatively lower than the prevalence of 69.5 per cent for 2016–2017, and 70.7 per cent for 2017–2018 among older adults in Canada (Government of Canada, 2019b). Additionally, we found that influenza vaccination differed by gender, age, and perceived health status as women, much older adults, and those with the poorest self-reported health status were more likely to be vaccinated (see Table 2). The findings are similar to previous studies, which have shown that women and older adults in Canada are more likely to get vaccinated compared to men and younger adults (Chen, Yi, Wu, & Li, Reference Chen, Yi, Wu and Li2007), frail or vulnerable adults are more likely to be vaccinated than those who are very fit or well (Andrew et al., Reference Andrew, Gilca, Waite and Pereira2019), and people with chronic conditions or recently hospitalized are more likely to be vaccinated against influenza (Chen et al., Reference Chen, Yi, Wu and Li2007; Jiménez-García et al., Reference Jiménez-García, Hernández-Barrera, Andres, Jimenez-Trujillo, Esteban-Hernández and Carrasco-Garrido2010). Influenza vaccination is highly recommended for older adults due to the weakening of immune defenses because of old age (Wong et al., Reference Wong, Cheng, Foppa, Jain, Fry and Finelli2014), and older adults see their doctors more frequently (Endrich, Blank, & Szucs, Reference Endrich, Blank and Szucs2009; Jiménez-García et al., Reference Jiménez-García, Hernández-Barrera, Andres, Jimenez-Trujillo, Esteban-Hernández and Carrasco-Garrido2010). Compared to men, women are also more likely to visit a medical practitioner or receive home medical visits (Quashie, Reference Quashie2018; Redondo-Sendino, Guallar-Castillón, Banegas, & Rodríguez-Artalejo, Reference Redondo-Sendino, Guallar-Castillón, Banegas and Rodríguez-Artalejo2006), thus, they are more likely to receive an influenza vaccine from their health care providers. Edwards and Hackell (Reference Edwards and Hackell2016) showed that physicians are the most important influencers of vaccine decision-making. The influence of health care professionals such as physicians on vaccine decision-making can be useful in tackling vaccine-hesitancy and encouraging public acceptance of COVID-19 vaccines (Deroo et al., Reference Deroo, Pudalov and Fu2020; Paterson et al., Reference Paterson, Meurice, Stanberry, Glismann, Rosenthal and Larson2016). The above evidence also supports our finding that the likelihood of influenza vaccination increases with age.
A major strength of this study is that it uses a large sample of respondents to investigate the relationship between life satisfaction in older adults and the recency of influenza vaccination. However, the study is not without limitations. First, there was relatively limited variability in the life satisfaction variable as 89.7 per cent of the study population reported being either satisfied or very satisfied with life, hence, our study participants could be healthier than the general population of older adults in Canada. Brule, McDonald, and McDiarmid (Reference Brule, McDonald and McDiarmid2019) showed that Canadians ages 12 years and older who report that their health is excellent or very good are more likely to be satisfied or very satisfied with life. Additionally, over 50 per cent of older adults in our study have at least a post-secondary education. As high educational attainment has been associated with high life satisfaction and the use of preventive health services (Meeks & Murrell, Reference Meeks and Murrell2001; Mullahy, Reference Mullahy1999), the study participants could consist of more vaccinated individuals. Evidence suggests that as of 2006, over 50 per cent of older adults in Canada have at least a post-secondary level education, with the trend expected to increase (Statistics Canada, 2007), suggesting that our study sample is reflective of the average educational attainment of Canada’s older adults.
Second, the categorization of respondents into groups can result in a misclassification bias and influence the reported associations. For example, placing someone who self-reports a life satisfaction score of 4 in the “dissatisfied” category rather than the “neither satisfied nor dissatisfied” category can affect the distribution of respondents and influence the association (Dosemeci, Wacholder, & Lubin, Reference Dosemeci, Wacholder and Lubin1990). Furthermore, the life satisfaction variable is a self-reporting variable, and proxy interviewees were used in cases where individuals were not able to respond. Self-reported data may be subject to some biases, including desirability bias (providing socially acceptable responses), response bias (differences between those who respond to the survey and those who don’t), and recall bias (unable to accurately recall information) (Chan & Bacila, Reference Chan and Bacila2019). The use of proxies can also impact the observed association because people tend to rate their health and quality of life differently than proxies (Magaziner, Bassett, Hebel, & Gruber-Baldini, Reference Magaziner, Bassett, Hebel and Gruber-Baldini1996). However, when restricted to non-proxy respondents, no differences were observed in the recency of vaccination by life satisfaction status in our study population, suggesting that the impact of proxy respondents on the observed association was very minimal. It is worth noting that the lack of differences may also be because proxy responses represented a very small proportion of total survey responses. Lastly, although the cross-sectional study design and secondary data analysis limit generalization of the findings, the study contributes to knowledge on the relationship between life satisfaction and influenza vaccination among older adults.
While Canada’s influenza vaccination policies and recommendations have generally prioritized encouraging and increasing vaccination coverage in high-risk individuals, and people working or living with high-risk individuals, some policy measures at the provincial level are aimed at ensuring universal coverage (Government of Canada, 2021). For example, provinces including Nova Scotia and Ontario have implemented Universal Influenza Immunization Programs (UIIP) that provide publicly funded influenza vaccination for individuals ages six months and older who live in these provinces (Government of Ontario, 2021). Although these programs are reported to have increased vaccination coverage in both high- and low-risk groups in these two provinces (Isenor, O’Reilly, & Bowles, Reference Isenor, O’Reilly and Bowles2018) and reduced influenza-related mortality and health care use (Kwong et al., Reference Kwong, Stukel, Lim, McGeer, Upshur and Johansen2008), other provinces have yet to implement UIIPs. For both provinces that have implemented UIIPs and those that have yet to implement them, including programming aspects that are aimed at improving the social environment and life satisfaction of older adults into their UIIPs can help increase vaccination coverage among older adults in the long term.
Conclusion
This study has helped shed light on the relationship between life satisfaction and influenza vaccination among older adults in Canada, finding that older adults who are satisfied with life are more likely to have a recent history of influenza vaccination. The findings can help inform public health measures that are geared towards increasing influenza vaccination among older adults in Canada by improving factors that impact their life satisfaction. As these factors are complex, a combination of both universal and targeted policy measures and interventions are needed to meet Canada’s national vaccination coverage targets, particularly for older adults. While our findings have pointed to how life satisfaction can impact influenza vaccination in older adults, additional research is needed to examine other factors that also impact influenza vaccination coverage in older adults.
Acknowledgements
The authors would like to thank Professor Mieke Koehoorn at the School of Population and Public Health, University of British Columbia, for her feedback on the original drafts of the manuscript, and Disann Katende for his suggestions and feedback on subsequent drafts.
Conflict of Interest
BM and CEO report no conflict of interest. MKA reports grants from Sanofi, GSK, Pfizer, Public Health Agency of Canada, Canadian Immunity Task Force, and the Canadian Frailty Network, and payments for past advisory activities from Sanofi, Seqirus and Pfizer outside the current study.








