Dear Editor
Over the past decade, there has been an increase in studies of individuals at clinical high risk (CHR) of developing psychosis characterized by subthreshold psychotic symptoms and functional decline before the emergence of a diagnosable psychotic disorder. Typically, this research focuses on an improved understanding of the prodromal period, the predictors of developing psychosis as well as potential interventions (Addington & Heinssen, Reference Addington and Heinssen2012). Conducting prospective research with young people at CHR of psychosis poses many challenges, including the recruitment of an adequate sample size to increase the power of the study (Heinssen et al. Reference Heinssen, Cuthbert, Breiling, Colpe and Dolan-Sewell2003). Based on the low incidence rates (<1 case per 10 000 persons per year in the general population) research centres that are involved in this research recruited 18–30 individuals per year (Addington et al. Reference Addington, Cadenhead, Cannon, Cornblatt, McGlashan, Perkins, Seidman, Tsuang, Walker, Woods and Heinssen2007). However, it should be noted that first these participants are help-seeking, and are not recruited through targeted screening and secondly since these individuals are help-seeking, sampling strategies will be different across CHR research centres. Although much of the research focuses on understanding the development of psychosis, of those who do not go on to develop psychosis, many remain disabled with poor functional outcome and potentially chronic subthreshold symptoms (Addington et al. Reference Addington, Cornblatt, Cadenhead, Cannon, McGlashan, Perkins, Seidman, Tsuang, Walker, Woods and Heinssen2011).
Collaborative multi-site research, an alternative to the typical single-site, single principal investigator approach to early psychosis research, does address the issue of having adequately powered samples. However, from a public health perspective it fails to address the issue of population-based identification and treatment of those at CHR of developing psychosis.
This paper describes the attempts at recruiting and engaging youth at CHR of psychosis through the joint efforts of an integrated research and clinical service in the Canadian health system. The research programme was conducted at the University of Calgary site of the North American Prodrome Longitudinal Study (NAPLS) and the PRIME clinic is for those at CHR for psychosis.
Initial phone screening is done through NAPLS by an experienced clinician who screens and invites appropriate referrals for consultation. All sources of referrals are encouraged to call to discuss any young person whom they may have had concerns with respect to impending psychosis. Potentially suitable participants are offered an initial screening appointment through NAPLS within 1 week of referral. This screening is conducted by experienced clinical raters, under the supervision of J.A., who are trained in the Structured Clinical Interview for DSM Disorders (SCID) and the Structured Interview of Prodromal Syndromes (SIPS) which is one of the most widely used assessments to determine the prodromal status (McGlashan et al. Reference McGlashan, Walsh and Woods2010). Once it is established that individuals meet relevant criteria, they are invited to participate in the NAPLS project and to attend the PRIME clinic.
Finding those at CHR
Recruiting symptomatic, help-seeking youth who are at risk for psychosis requires active outreach to potential health care-oriented referrals (McGlashan et al. Reference McGlashan, Addington, Cannon, Heinimaa, McGorry, O'Brien, Penn, Perkins, Salokangas, Walsh, Woods and Yung2007). In addition, an education and referral campaign must reach the individual and address any existing barriers to their seeking help, which requires multiple recruiting strategies. Between 2009 and 2011, we used marketing strategies (mass mailing, print advertisements), outreach to referring sites, and the development of collaborative relationships to maintain a steady flow of referrals.
Mail-Out
Our first recruitment strategy was to mail educational material (brochures highlighting CHR symptoms and clinic contact information) to all possible referring sources. This mass mailing included 2155 general practitioners, paediatricians and psychiatrists located in Calgary and the adjacent rural areas. A database was developed for all community agencies, child and youth services, mental health urgent care services and counsellors in the Calgary area that would likely be in contact with our target population. In total, 171 clinics, agencies and schools received the package.
Presentations
Following the mass mail-out, every community, mental health or counselling agency in the Calgary area was personally contacted and many questions were answered. They were given an opportunity to attend a presentation that focused on the early warning signs of psychosis and the referral process to the clinic or to inquire about the research projects. These presentations were typically 1–3 h in length with the depth of content determined by the needs of the audience. Word of mouth from key stakeholders that work with youth was instrumental in facilitating these presentations. For example, reaching all secondary school counsellors was complicated by the large number of schools and administrative policies for various school boards. Informal snowballing within the network of family school liaison social workers resulted in large groups of junior and senior high counsellors from the public and separate school boards being brought together for eight presentations. The slide presentation given to these counsellors was also posted on the school board internal website, which also enhanced awareness of at risk symptoms. Between 2009 and 2011, 55 presentations were given. Comprehensive educational packages were distributed at each presentation. Included in this package was a CHR symptom assessment chart, several case studies, referral information, PRIME and NAPLS brochures and flyers of various NAPLS treatment studies. Follow-up calls were made every 6 months to each agency or clinic that was most likely to refer in order to assess the need for further information or presentations.
Advertising
An informational campaign to increase public awareness of at risk symptoms was launched in late 2010. A poster with the slogan ‘Is Something Not Quite Right?’ with key symptoms and NAPLS contact information was displayed on Calgary Transit trains and buses for 6 months. A similar advertisement ran for 1 month in a free Calgary newspaper with a wide circulation. Posters were placed in busy locations throughout the city that had a large amount of pedestrian traffic.
Collaboration with Referral Sources
Establishing and maintaining a strong collaborative relationship with key referring sources was essential for long-term successful recruitment. Development of a mutually beneficial relationship was a time-consuming process that did not become fully solidified until well after NAPLS was launched. To encourage the building of a positive relationship, we offered various forms of assistance to the referring sources. In addition to presentations and educational packages, we provided support in the screening process. For example, if a school guidance counsellor was uncertain about the mental health status of a student, we provided telephone screens of the individual in question. By speaking directly to the young person, we could address any concerns about mental health, research and confidentiality of information. Moreover, with the written consent of a NAPLS participant or their legal guardian if they were a minor, we provided the referral source with a written summary of the NAPLS clinical results. This service became particularly important if the youth was going to continue to see the referring source for future care. We also maintained a close relationship with the psychiatrists and case managers in our early psychosis programme so that the flow between the early psychosis service and the CHR clinic and projects was seamless.
Outcome
Over a 3-year-period (2009–2011), 378 referrals were received, the outcome of which is presented in Fig. 1. All 378 referrals were initially screened by telephone to determine if they were likely to meet our criteria prior to inviting them for an initial interview. Based on this phone screen, 74 referrals were clearly not at CHR, 45% (n = 34) of whom appeared to already be psychotic (e.g. clearly had psychotic symptoms, were already receiving antipsychotics) and so were referred elsewhere. Of the 378 referrals, 78% (295) appeared to be suitable for an initial consultation and were subsequently invited to attend for an interview. Of those invited for an interview 107 met the prodromal criteria and agreed to participate in NAPLS and/or the PRIME clinic. This is 28% of the total referrals and 36% of those attending an initial assessment.
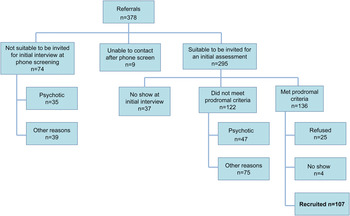
Fig. 1. Outcome of referrals.
Figure 2 describes the number of referrals made by different sources plus the number that actually met the prodromal criteria from each source. Our early psychosis treatment service was responsible for 34% of all referrals. The second largest referral source was family, friends and self, followed by acute care mental health services (e.g. emergency room, in- and out-patient units). Community agencies included central mental health referring agencies, community resource programmes for family, children and youth and mental health clinics.
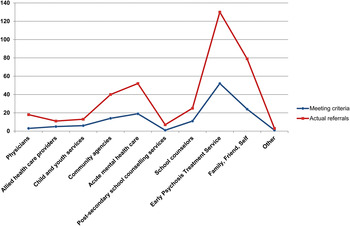
Fig. 2. Referral sources.
Figure 3 demonstrates the change in referrals over the 3 years. Compared with the previous 2 years, there is a 50% increase of referrals in 2011, 46% increase in those being invited for an assessment but only a 15% increase in those meeting criteria and a 32% increase in those consenting to participate.
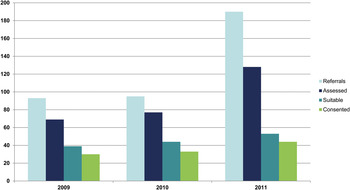
Fig. 3. Number of referrals.
Discussion
This paper has described a recruitment strategy for individuals who are at CHR for the development of psychosis. Services offered to these people include a research programme for early psychosis and a publicly funded clinic. Of all our referrals, 36% are suitable and about 28% engage. However, of those we actually assess, the numbers are 46 and 36%, respectively. In addition, 16% of those are identified as having a psychotic illness. For this group, identification and referral represent a significant benefit (Nelson & Yung, Reference Nelson and Yung2007).
The annual increases in the number of referrals suggest that this recruitment effort is effective in generating more referrals, and more referrals that in a phone screen seem appropriate to invite for a consultation. However, we did not observe the same increase in those that met the criteria (15%) and those that were willing to participate (32%). Constraints on financial resources have an impact on the depth and breadth of recruitment. An additional focus on paid advertising could have potentially increased our numbers but may also have increased the number of inappropriate/unsuitable referrals. We may also need to address the referral sources that provided the largest number of referrals but a relatively lower number of actual participants, for example, family friends and self-referrals or acute mental health services. One option is that we increase our feedback to referral sources to help them understand the participants that we are seeking better. A second limitation is that our focus was specifically on individuals identified as ‘help seekers’. We did not use any widespread screening procedures such as screening in schools (Laurens et al. Reference Laurens, Hodgins, Maughan, Murray, Rutter and Taylor2007). One advantage of our efforts is that participants are not limited to participating in a research project. Participants could attend the PRIME clinic, whereas participation in the NAPLS project offered them additional follow-up and the opportunity for clinical trials. In terms of generalization, due to possibly, different sampling strategies CHR samples are not necessarily comparable across centres. Secondly, it is not clear if there are aspects of recruitment into services for those at CHR that may be uniquely Canadian. Canada offers health services which are free at the point of care delivery but access to services is a challenge. Participation in a free research clinic may be less of an advantage than in countries where people pay for health care.
There are several implications. First, the increase in referral of help seeking individuals suggests that there appears to be a greater understanding of the notion of early intervention and CHR (de Girolamo et al. Reference de Girolamo, Dagani, Purcell, Cocchi and McGorry2012). A similar approach in Toronto over a 4-year period showed that only 21% of all referrals met the criteria and only 14% agreed to participate in a research or clinical service (Addington et al. Reference Addington, Epstein, Reynolds, Furimsky, Rudy, Mancini, McMillan, Kirsopp and Zipurksy2008). Yet, despite this, based on typical percentages of those at CHR who do convert to a psychotic illness (Yung et al. Reference Yung, Yuen, Berger, Francey, Hung, Nelson, Phillips and McGorry2007; Cannon et al. Reference Cannon, Cadenhead, Cornblatt, Woods, Addington, Walker, Seidman, Perkins, Tsuang, McGlashan and Heinssen2008), the majority of the newly identified first episode of psychosis patients in Calgary do not present through our CHR programmes. It may be that at the present time work with those at CHR represents an important and useful research approach but the recruitment challenges reinforce the argument that this is not yet ready to be a public health approach to prevention.
Future research should continue to explore clinical and biological predictors and mechanisms of conversion to psychosis as well as the developmental trajectories of these CHR individuals. Recent studies have suggested that there may be a decline in such samples of those who go on to develop full blown psychosis (Yung et al. Reference Yung, Yuen, Berger, Francey, Hung, Nelson, Phillips and McGorry2007; Fusar-Poli et al. Reference Fusar-Poli, Bonoldi, Yung, Borgwardt, Kempton, Valmaggia, Barale, Caverzasi and McGuire2012). Thus, greater attention in CHR studies to recruitment and ascertainment strategies, and subsequent changes in ascertainment may shed some light on these declining rates. Finally, little attention has been given to help-seeking particularly among youth and this may be an important area to address in the future.
Conflict of Interest
This work was supported by NIMH grant U01MH08984 to Dr Jean Addington and the Alberta Centennial Mental Health Research Chairs Program. Authors have no conflict of interest related to the present paper.







