Refine listing
Actions for selected content:
135398 results in Open Access
Alcohol and tobacco dependence among medical practitioners
-
- Journal:
- European Psychiatry / Volume 67 / Issue S1 / April 2024
- Published online by Cambridge University Press:
- 27 August 2024, p. S403
-
- Article
-
- You have access
- Open access
- Export citation
Prevalence of psychiatric disorders in patients with craniofacial malformations - a statistical analysis
-
- Journal:
- European Psychiatry / Volume 67 / Issue S1 / April 2024
- Published online by Cambridge University Press:
- 27 August 2024, pp. S483-S484
-
- Article
-
- You have access
- Open access
- Export citation
Sociodemographic and Clinical Profile of Perpetrators of conjugal Homicides
-
- Journal:
- European Psychiatry / Volume 67 / Issue S1 / April 2024
- Published online by Cambridge University Press:
- 27 August 2024, p. S163
-
- Article
-
- You have access
- Open access
- Export citation
Phycian assisted suicide: A Swiss perspective - a liberal view
-
- Journal:
- European Psychiatry / Volume 67 / Issue S1 / April 2024
- Published online by Cambridge University Press:
- 27 August 2024, pp. S32-S33
-
- Article
-
- You have access
- Open access
- Export citation
Attachment representations in high intellectual potential (HIP) children compared to non-HIP children during development
-
- Journal:
- European Psychiatry / Volume 67 / Issue S1 / April 2024
- Published online by Cambridge University Press:
- 27 August 2024, pp. S442-S443
-
- Article
-
- You have access
- Open access
- Export citation
Forearm bisection task suggests an alteration in Body Schema in patients with Motor Conversion Disorders (Functional Movement Disorders)
-
- Journal:
- European Psychiatry / Volume 67 / Issue S1 / April 2024
- Published online by Cambridge University Press:
- 27 August 2024, p. S368
-
- Article
-
- You have access
- Open access
- Export citation
From schizotypy to psychosis: is it a natural continuum?
-
- Journal:
- European Psychiatry / Volume 67 / Issue S1 / April 2024
- Published online by Cambridge University Press:
- 27 August 2024, pp. S658-S659
-
- Article
-
- You have access
- Open access
- Export citation
Reasons for Individuals not Enrolling for Yoga trial in Addiction
-
- Journal:
- European Psychiatry / Volume 67 / Issue S1 / April 2024
- Published online by Cambridge University Press:
- 27 August 2024, pp. S353-S354
-
- Article
-
- You have access
- Open access
- Export citation
Pharmaco-EEG of antipsychotics’ response: a systematic review
-
- Journal:
- European Psychiatry / Volume 67 / Issue S1 / April 2024
- Published online by Cambridge University Press:
- 27 August 2024, pp. S669-S670
-
- Article
-
- You have access
- Open access
- Export citation
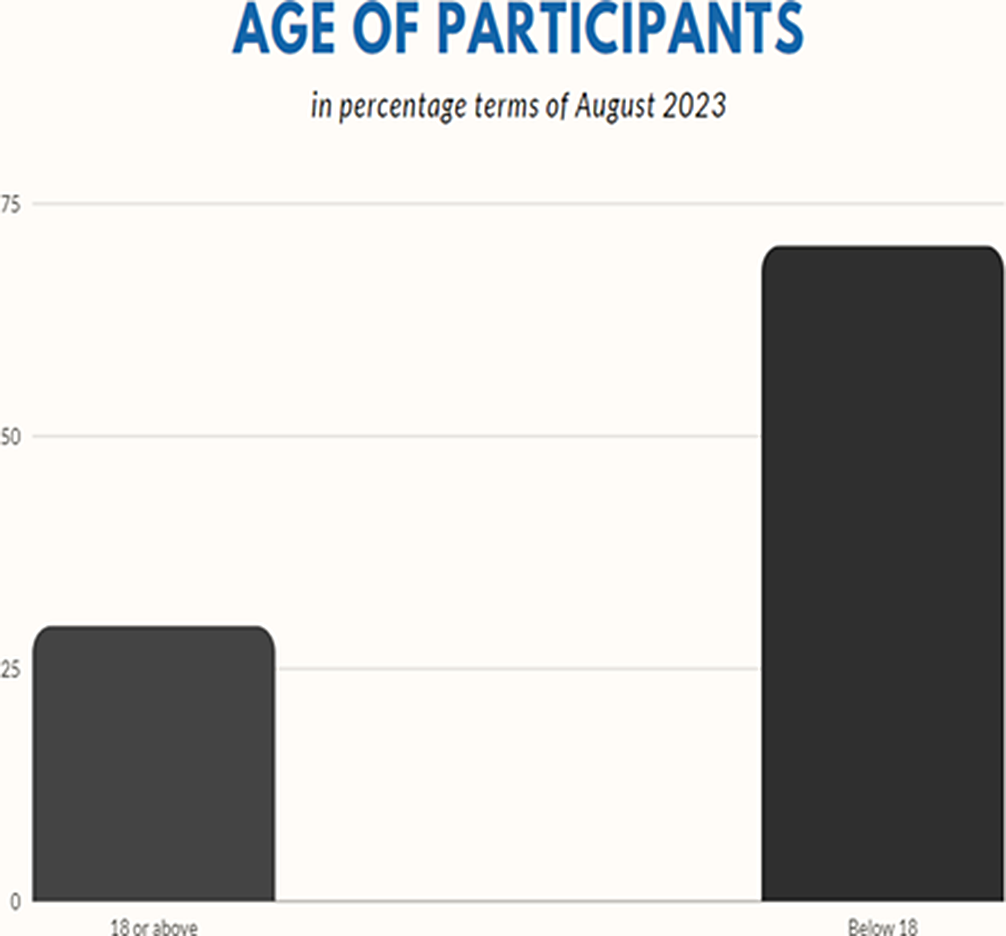
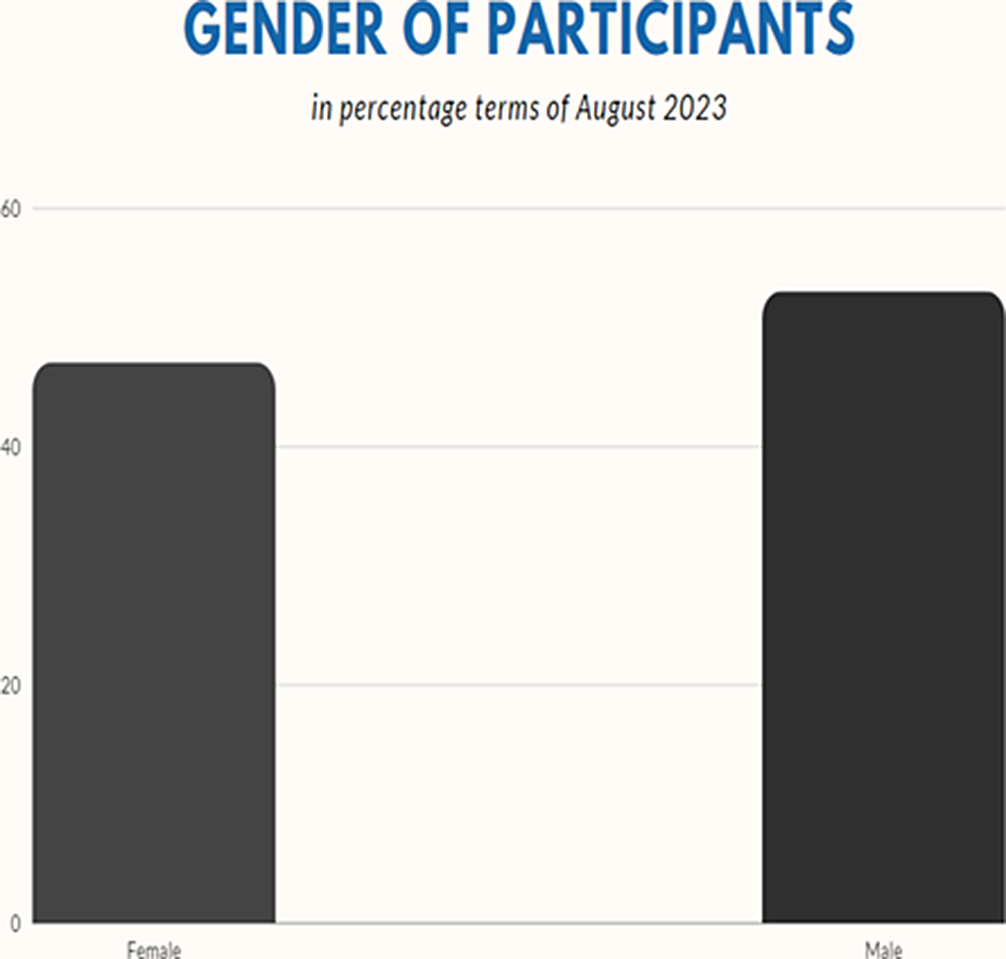
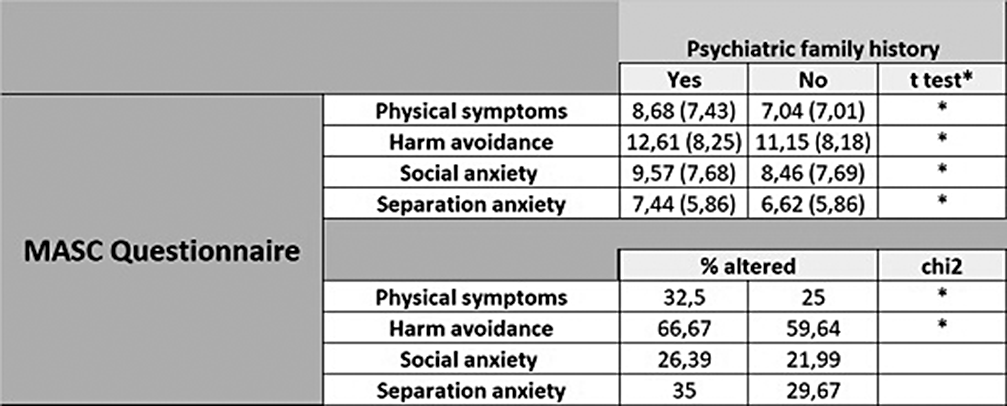
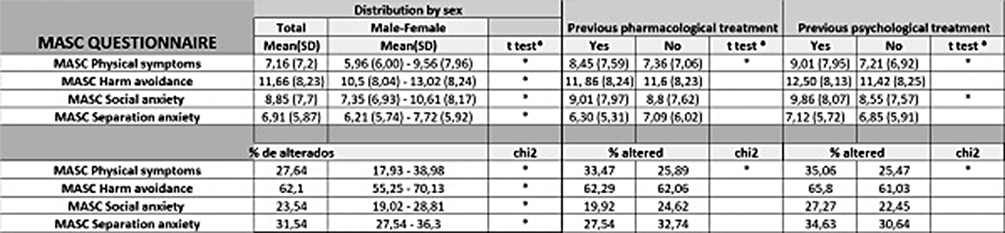
Association and predictor role of MASC scores in pharmacological or psychological treatment indication in a sample of children and adolescent in Spain
-
- Journal:
- European Psychiatry / Volume 67 / Issue S1 / April 2024
- Published online by Cambridge University Press:
- 27 August 2024, pp. S461-S462
-
- Article
-
- You have access
- Open access
- Export citation
Esketamine new tool for resistant depressive disorder. About a case
-
- Journal:
- European Psychiatry / Volume 67 / Issue S1 / April 2024
- Published online by Cambridge University Press:
- 27 August 2024, p. S533
-
- Article
-
- You have access
- Open access
- Export citation
Long-term prognosis of chronic depression in adolescence
-
- Journal:
- European Psychiatry / Volume 67 / Issue S1 / April 2024
- Published online by Cambridge University Press:
- 27 August 2024, pp. S359-S360
-
- Article
-
- You have access
- Open access
- Export citation
The current status of recommendations for non-invasive neuromodulation therapy in severe mental disorders
-
- Journal:
- European Psychiatry / Volume 67 / Issue S1 / April 2024
- Published online by Cambridge University Press:
- 27 August 2024, p. S705
-
- Article
-
- You have access
- Open access
- Export citation
Epidemiological, clinical, and forensic approach to a series of defendants examined in criminal psychiatric expertise
-
- Journal:
- European Psychiatry / Volume 67 / Issue S1 / April 2024
- Published online by Cambridge University Press:
- 27 August 2024, p. S581
-
- Article
-
- You have access
- Open access
- Export citation
Evaluation of Neurocognitive Functions of Children and Adolescents Diagnosed with Pediatric Bipolar Disorder and Disruptive Mood Dysregulation and at High Risk for Bipolar Disorder
-
- Journal:
- European Psychiatry / Volume 67 / Issue S1 / April 2024
- Published online by Cambridge University Press:
- 27 August 2024, pp. S78-S79
-
- Article
-
- You have access
- Open access
- Export citation
New treatment perspectives for negative symptoms
-
- Journal:
- European Psychiatry / Volume 67 / Issue S1 / April 2024
- Published online by Cambridge University Press:
- 27 August 2024, p. S17
-
- Article
-
- You have access
- Open access
- Export citation
Transcranial Magnetic Stimulation and Dual Pathology: An Integrative Protocol
-
- Journal:
- European Psychiatry / Volume 67 / Issue S1 / April 2024
- Published online by Cambridge University Press:
- 27 August 2024, p. S145
-
- Article
-
- You have access
- Open access
- Export citation
Factors associated with anxious distress in major depressive episodes: a cross-sectional study
-
- Journal:
- European Psychiatry / Volume 67 / Issue S1 / April 2024
- Published online by Cambridge University Press:
- 27 August 2024, p. S302
-
- Article
-
- You have access
- Open access
- Export citation
Predictors of change in emotional regulation from 6 to 30 months of age in infants born after a threatened preterm labour.
-
- Journal:
- European Psychiatry / Volume 67 / Issue S1 / April 2024
- Published online by Cambridge University Press:
- 27 August 2024, p. S360
-
- Article
-
- You have access
- Open access
- Export citation
An Umbrella Review of Effectiveness of Intravenous Ketamine in Treatment-Resistant Depression
-
- Journal:
- European Psychiatry / Volume 67 / Issue S1 / April 2024
- Published online by Cambridge University Press:
- 27 August 2024, pp. S86-S87
-
- Article
-
- You have access
- Open access
- Export citation