Refine listing
Actions for selected content:
135494 results in Open Access
Changing drinking patterns among Italians: 7 out of 10 students experience Binge Drinking
-
- Journal:
- European Psychiatry / Volume 67 / Issue S1 / April 2024
- Published online by Cambridge University Press:
- 27 August 2024, p. S132
-
- Article
-
- You have access
- Open access
- Export citation
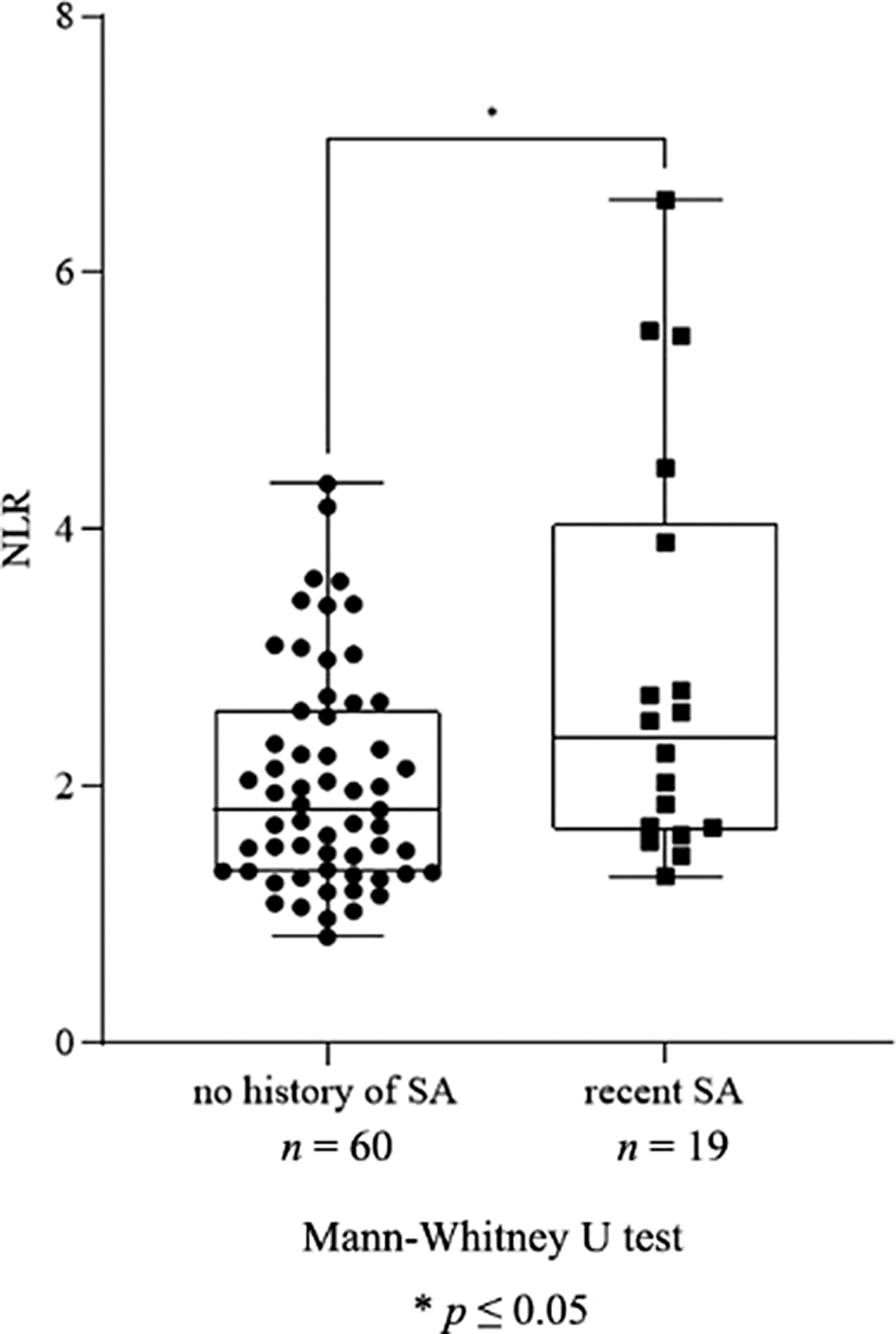
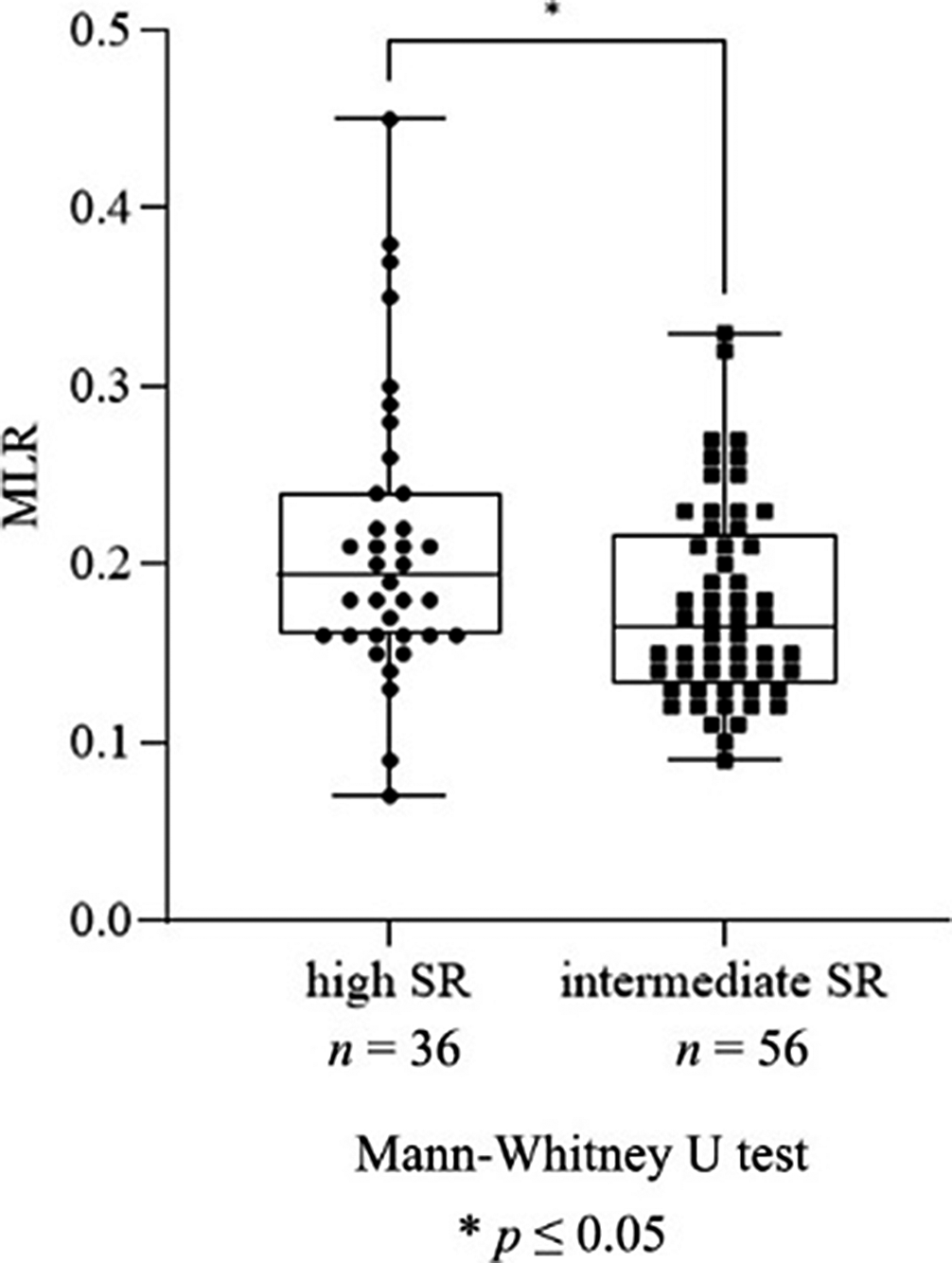
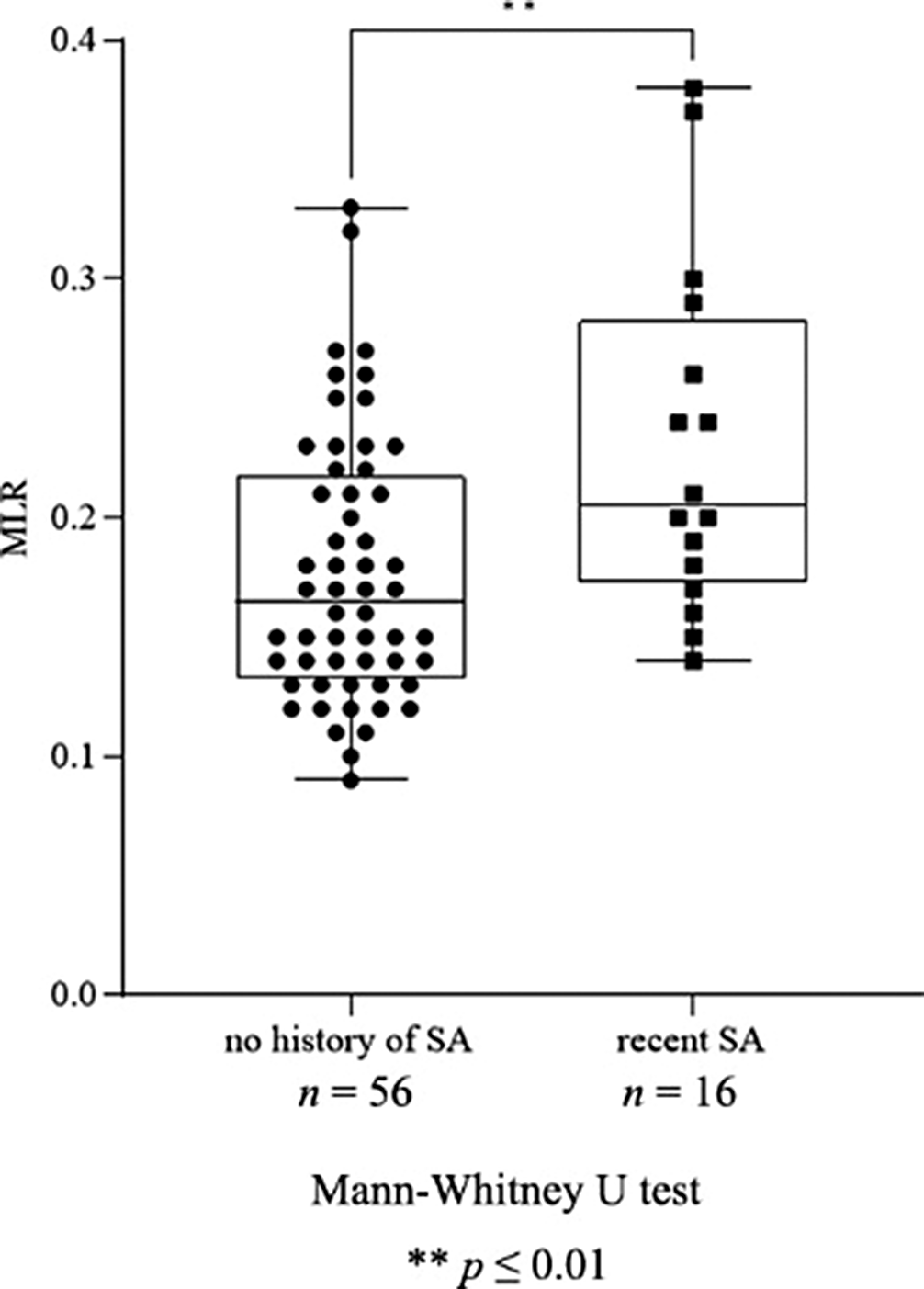
Investigation of peripheral inflammatory biomarkers in association with suicide risk in major depression
-
- Journal:
- European Psychiatry / Volume 67 / Issue S1 / April 2024
- Published online by Cambridge University Press:
- 27 August 2024, pp. S792-S793
-
- Article
-
- You have access
- Open access
- Export citation
Sleep disorders comorbid with ADHD: an overview of the clinical presentation and management
-
- Journal:
- European Psychiatry / Volume 67 / Issue S1 / April 2024
- Published online by Cambridge University Press:
- 27 August 2024, p. S37
-
- Article
-
- You have access
- Open access
- Export citation
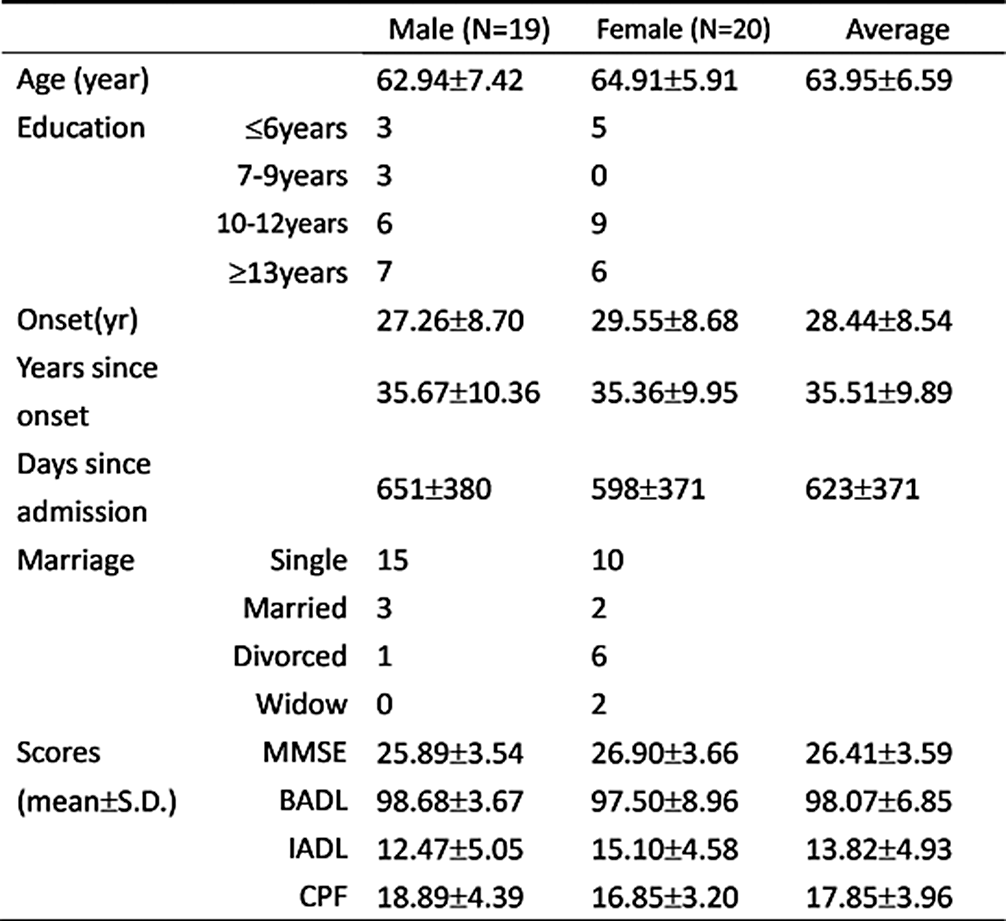
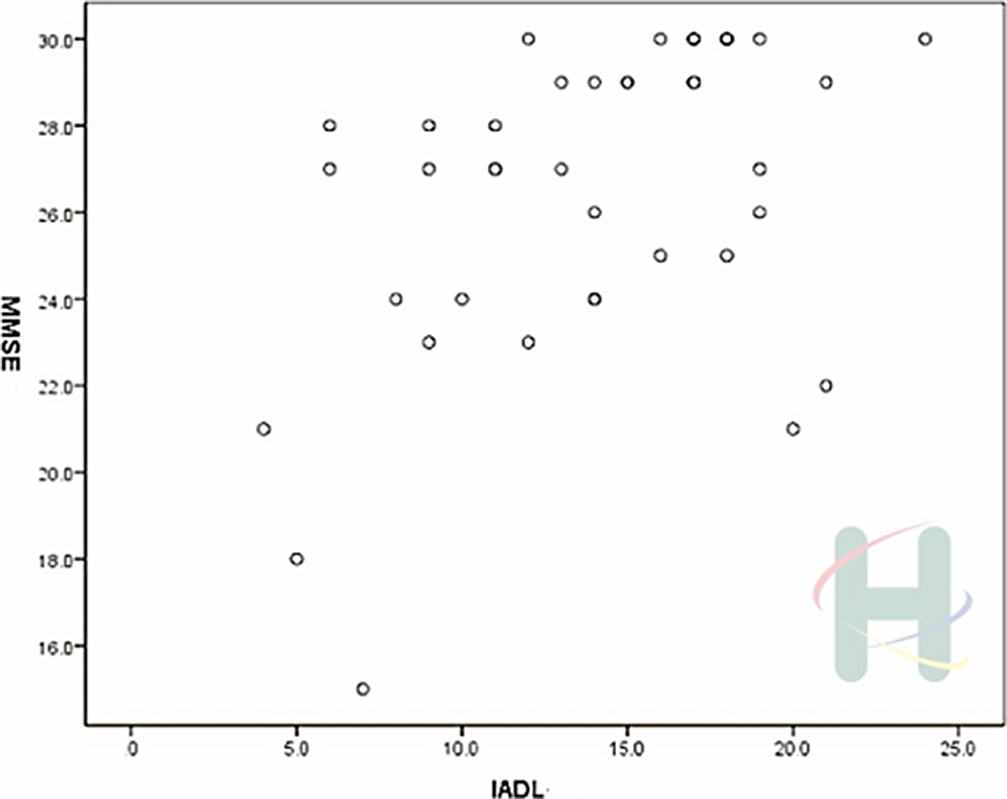
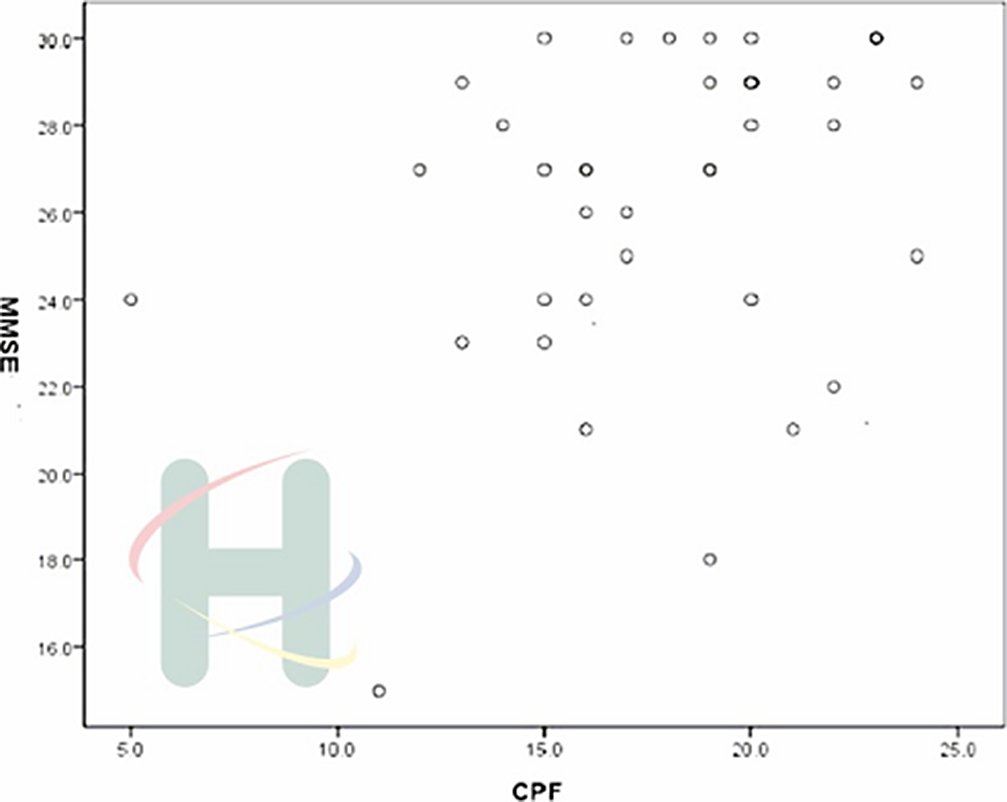
Relationships between cognitive function and activities of daily living in psychiatric nursing home patients with schizophrenia
-
- Journal:
- European Psychiatry / Volume 67 / Issue S1 / April 2024
- Published online by Cambridge University Press:
- 27 August 2024, p. S758
-
- Article
-
- You have access
- Open access
- Export citation
Subjective discomfort and lack of volitional drive with neuroleptic pharmacotherapy - a phenomenological case study
-
- Journal:
- European Psychiatry / Volume 67 / Issue S1 / April 2024
- Published online by Cambridge University Press:
- 27 August 2024, pp. S828-S829
-
- Article
-
- You have access
- Open access
- Export citation
Mental disorders in internally displaced persons: clinical features, therapy, prevention
-
- Journal:
- European Psychiatry / Volume 67 / Issue S1 / April 2024
- Published online by Cambridge University Press:
- 27 August 2024, pp. S166-S167
-
- Article
-
- You have access
- Open access
- Export citation
The Relationship Between Internal Stigmatisation, Recovery and Treatment Adherence in Individuals with Schizophrenia
-
- Journal:
- European Psychiatry / Volume 67 / Issue S1 / April 2024
- Published online by Cambridge University Press:
- 27 August 2024, p. S732
-
- Article
-
- You have access
- Open access
- Export citation
Impact of child maltreatment on bulimic behaviors among the tunisian general population
-
- Journal:
- European Psychiatry / Volume 67 / Issue S1 / April 2024
- Published online by Cambridge University Press:
- 27 August 2024, p. S561
-
- Article
-
- You have access
- Open access
- Export citation
Temperamental and Neurocognitive predictors in Korean basketball league draft selection
-
- Journal:
- European Psychiatry / Volume 67 / Issue S1 / April 2024
- Published online by Cambridge University Press:
- 27 August 2024, pp. S380-S381
-
- Article
-
- You have access
- Open access
- Export citation
Dual diagnosis of bipolar disorder and substance use disorder – type of substance used and its impact on treatment adherence and maintenance of abstinence
-
- Journal:
- European Psychiatry / Volume 67 / Issue S1 / April 2024
- Published online by Cambridge University Press:
- 27 August 2024, p. S365
-
- Article
-
- You have access
- Open access
- Export citation
The impact of eating habits on mood disorders (A prospetive study to show the importance of food on preventing mental heath disorders )
-
- Journal:
- European Psychiatry / Volume 67 / Issue S1 / April 2024
- Published online by Cambridge University Press:
- 27 August 2024, pp. S672-S673
-
- Article
-
- You have access
- Open access
- Export citation
Logistic regression model for the prediction of asthenia development in schizophrenia based on inflammatory blood markers
-
- Journal:
- European Psychiatry / Volume 67 / Issue S1 / April 2024
- Published online by Cambridge University Press:
- 27 August 2024, pp. S280-S281
-
- Article
-
- You have access
- Open access
- Export citation
Climate change and mental health. Polish perspective
-
- Journal:
- European Psychiatry / Volume 67 / Issue S1 / April 2024
- Published online by Cambridge University Press:
- 27 August 2024, p. S77
-
- Article
-
- You have access
- Open access
- Export citation
Cultural Diversity and Mental Health Care: A Case Study
-
- Journal:
- European Psychiatry / Volume 67 / Issue S1 / April 2024
- Published online by Cambridge University Press:
- 27 August 2024, p. S522
-
- Article
-
- You have access
- Open access
- Export citation
Domestic violence in Tunisia: which forms of physical violence?
-
- Journal:
- European Psychiatry / Volume 67 / Issue S1 / April 2024
- Published online by Cambridge University Press:
- 27 August 2024, pp. S806-S807
-
- Article
-
- You have access
- Open access
- Export citation
Demographic Factors, Cumulative Stressors, and Psychological Well-being
-
- Journal:
- European Psychiatry / Volume 67 / Issue S1 / April 2024
- Published online by Cambridge University Press:
- 27 August 2024, p. S603
-
- Article
-
- You have access
- Open access
- Export citation
Depression among patients with ankylosing spondylitis in southern Tunisia: Prevalence and associated factors
-
- Journal:
- European Psychiatry / Volume 67 / Issue S1 / April 2024
- Published online by Cambridge University Press:
- 27 August 2024, p. S528
-
- Article
-
- You have access
- Open access
- Export citation
Schizophrenia and Risk of Dementia: A Literature Review.
-
- Journal:
- European Psychiatry / Volume 67 / Issue S1 / April 2024
- Published online by Cambridge University Press:
- 27 August 2024, pp. S760-S761
-
- Article
-
- You have access
- Open access
- Export citation
Psychiatric disorders in patients with rheumatoid arthritis
-
- Journal:
- European Psychiatry / Volume 67 / Issue S1 / April 2024
- Published online by Cambridge University Press:
- 27 August 2024, p. S217
-
- Article
-
- You have access
- Open access
- Export citation
Postpartum Depression: Plaguing the Joy of New Mothers
-
- Journal:
- European Psychiatry / Volume 67 / Issue S1 / April 2024
- Published online by Cambridge University Press:
- 27 August 2024, p. S808
-
- Article
-
- You have access
- Open access
- Export citation