Book contents
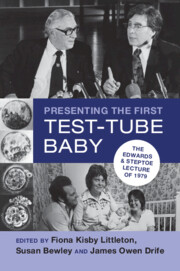
- Presenting the First Test-Tube Baby
- Presenting the First Test-Tube Baby
- Copyright page
- Contents
- Illustrations
- Tables
- Acknowledgements
- Foreword
- Abbreviations
- 1 Introduction
- 2 From Oldham and Cambridge to the Rest of the World
- 3 The Lecture, 1979
- 4 The Professional Reminiscence, 2019
- 5 The Local Reminiscence
- 6 The Legacy
- Index
- References
6 - The Legacy
2019 and Beyond
Published online by Cambridge University Press: 23 February 2023
- Presenting the First Test-Tube Baby
- Presenting the First Test-Tube Baby
- Copyright page
- Contents
- Illustrations
- Tables
- Acknowledgements
- Foreword
- Abbreviations
- 1 Introduction
- 2 From Oldham and Cambridge to the Rest of the World
- 3 The Lecture, 1979
- 4 The Professional Reminiscence, 2019
- 5 The Local Reminiscence
- 6 The Legacy
- Index
- References
Summary
Peter Braude and Martin Johnson were young researchers, a doctor and a scientist, working with Robert Edwards at Cambridge. They both witnessed (from the inside) how the IVF programme and first birth changed the worlds of science and O&G over the next forty years. Johnson wrote Edward’s citation for the Nobel Prize. They are uniquely placed to act as a bridge from 1979 into speculating about the future and whether the course of science can even be predicted.
Keywords
- Type
- Chapter
- Information
- Presenting the First Test-Tube BabyThe Edwards and Steptoe Lecture of 1979, pp. 201 - 215Publisher: Cambridge University PressPrint publication year: 2023