Little research has been conducted on the predictors of the long-term course of posttraumatic stress disorder (PTSD) (Steinert et al., Reference Steinert, Hofmann, Leichsenring and Kruse2015). The literature suggests that even though a substantial proportion of cases recover within a few months, at least one-third of cases persist for many years (Kessler et al., Reference Kessler, Sonnega, Bromet, Hughes and Nelson1995; Breslau et al., Reference Breslau, Kessler and Chilcoat1998; Pietrzak et al., Reference Pietrzak, Goldstein, Southwick and Grant2011; Chapman et al., Reference Chapman, Mills and Slade2012), and that chronic PTSD can lead to both secondary disorders (Perkonigg et al., Reference Perkonigg, Pfister and Stein2005) and suicidality (Tarrier & Gregg, Reference Tarrier and Gregg2004). To date, retrospective studies have focused on three predictors of PTSD recovery: trauma type characteristics, PTSD symptom severity, and history of comorbid mental disorders (Breslau et al., Reference Breslau, Kessler and Chilcoat1998; Pietrzak et al., Reference Pietrzak, Goldstein, Southwick and Grant2011; Chapman et al., Reference Chapman, Mills and Slade2012), while prospective naturalistic studies have identified socio-demographic factors and childhood adversities (CAs) as important predictors (Steinert et al., Reference Steinert, Hofmann, Leichsenring and Kruse2015).
Previous studies of PTSD recovery were based on relatively small samples, making it impossible to investigate fine-grained associations. We address this limitation by presenting data on patterns and predictors of PTSD recovery in a sample of 1,575 respondents with a history of PTSD in the World Mental Health (WMH) surveys (Kessler & Üstün, Reference Kessler and Üstün2008).
Methods
Analyses are based on the same 22 WMH surveys that assessed PTSD due to randomly selected traumas and are described in other chapters. The predictors considered were: respondent age at trauma exposure, sex, trauma type and history (see Chapter 9), childhood adversities (CAs; see Chapter 10), and prior psychopathology (see Chapter 12). Number of months with PTSD was defined as the minimum of the number of months (or years) the respondent reported having re-experiencing (DSM-IV criterion B), avoidance/numbing (criterion C), and hyperarousal (criterion D) symptoms. If symptoms within all three clusters persisted at the time of interview, the respondent was classified as not having experienced recovery. PTSD recovery was assessed using a discrete-time survival model framework (Willett & Singer, Reference Willett and Singer1993), with person-month the unit of analysis and a logistic link function in SAS version 9.3 (SAS Institute Inc., 2010). The outcome was coded 0 for each person-month until the retrospectively reported month of recovery. Respondents were censored after the month of recovery. The actuarial method (Halli & Rao, Reference Halli and Rao1992) was used to generate descriptive information about the distribution of speed of recovery.
All models included dummy variables for person-month and survey location so that coefficients for other predictors could be interpreted as pooled within-survey coefficients. This approach implicitly assumed that within-survey slopes were constant across surveys. We made this decision because we wanted to focus on central tendencies in the data rather than on analysis of between-survey differences. These associations would have been difficult to interpret because of the small number of countries represented in the series.
Model 1 examined associations of recovery with sex, age at trauma exposure, and number of years between age at exposure and age at interview. These variables were also controlled for in all subsequent models. Model 2 then added dummy variables for the random trauma type. Model 3 added information about history of prior (to the random trauma) trauma exposure. Model 4 added information about history of CAs, and Model 5 added information about prior DSM-IV/CIDI mental disorders. Significant predictors were carried forward across models. Logistic regression coefficients and standard errors were exponentiated and are reported as odds ratios (ORs) with 95% confidence intervals (CIs). In model 2, the logistic regression coefficients were scaled to have a sum of 0 across the 28 trauma types, resulting in the ORs for these trauma types having a product of 1.0. Therefore, the ORs that are significantly different from 1.0 can be interpreted as meaning that PTSD due to the associated trauma types has either a significantly more rapid (ORs >1.0) or more slow (ORs <1.0) odds of recovery than PTSD due to the average trauma. (Our definition of “average” was derived by giving each trauma type equal weight and ignoring the relative prevalence of the different trauma types.) Statistical significance was consistently evaluated using 0.05-level two-sided tests. The design-based Taylor series linearization method (Wolter, Reference Wolter1985) implemented in the SAS software system (SAS Institute Inc., 2008) was used to adjust for the weighting and clustering of observations. Design-based Wald χ2 tests were used to evaluate statistical significance of predictor sets.
In order to examine overall final model performance, we generated individual-level predicted probabilities of recovery and examined observed recovery curves separately within the first two quartiles and the latter half of the distribution of predicted probability of recovery. The method of replicated 10-fold cross-validation with 20 replicates (i.e., 200 separate estimates of model coefficients) was used to correct for the overestimation of prediction accuracy when, as in this analysis, model coefficients are both estimated and evaluated in the same sample (Smith et al., Reference Smith, Seaman, Wood, Royston and White2014).
Results
Observed Speed-of-Recovery Distributions by Age-of-Onset
A total of 1,404 respondents out of 1,575 eventually recovered. The slope of the recovery curve was steepest in the first 6 months, with 20% of cases recovering within 3 months and 27% within 6 months (see Figure 16.1). Fifty percent of cases recovered within 24 months and 77% within 10 years (120 months; the longest follow-up period for which a sufficient number of cases were observed for stable estimation of conditional probability of remission). The lowest projected recovery rate was among cases with onsets at ages 60+ (48%), and the highest among cases with onsets at ages 25–44 (89%).

Figure 16.1 Speed of recovery from random trauma PTSD, in the total sample and age of trauma exposure subgroups
Predictors of Recovery
Socio-demographics and Length of Recall
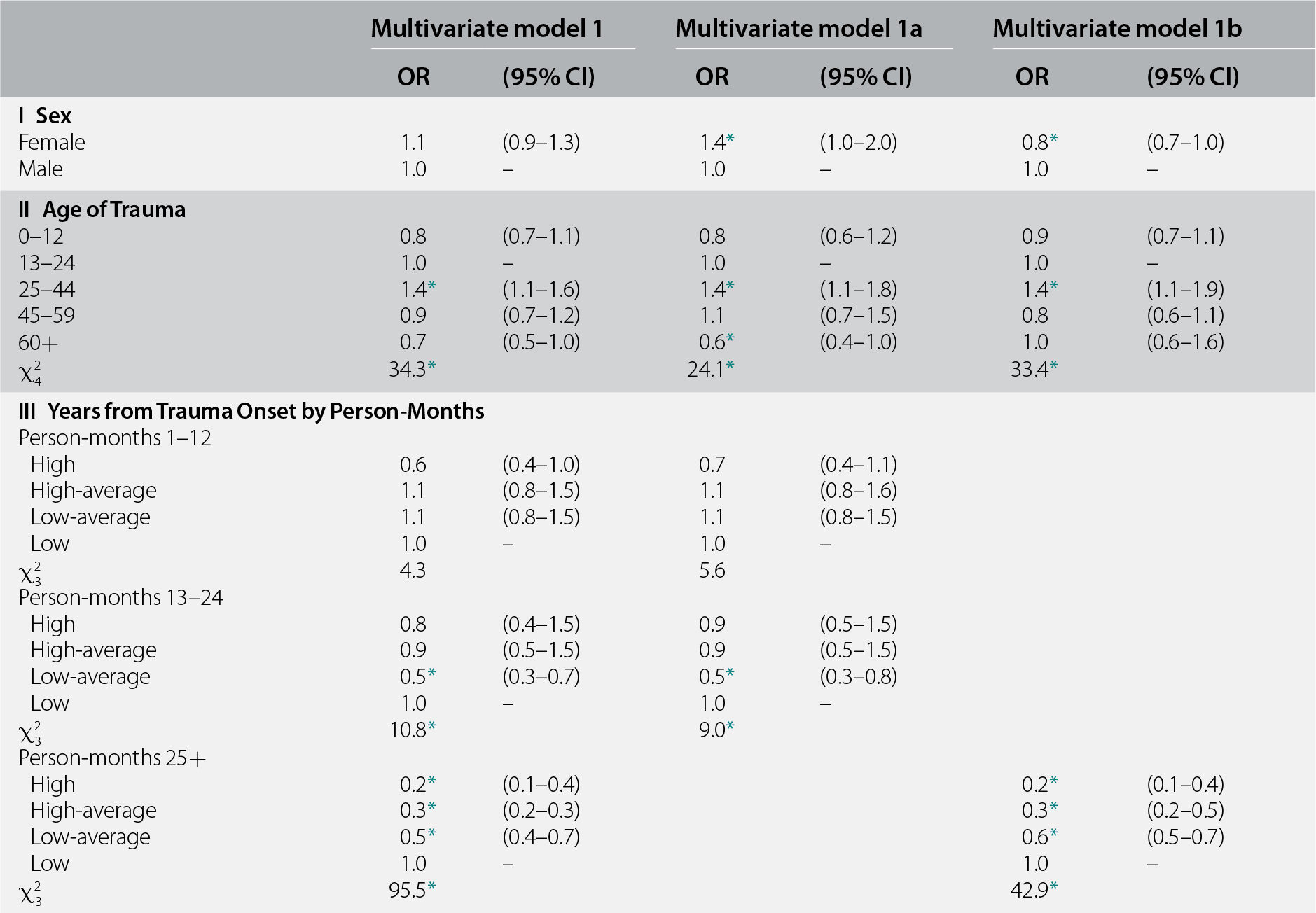
Sex was not associated with recovery overall (χ21 = 1.0, p = 0.31), and age at trauma exposure was significant along the lines seen in Figure 16.1 (χ24 = 34.3, p < 0.001) (see Table 16.1, model 1). Length of recall between respondent age at trauma exposure and age at interview was also significant; this association is most plausibly interpreted as evidence of time-related recall bias. Length of recall was divided into quartiles (low = 0–7, low-average = 8–16, high-average = 17–30, and high = 31+ years) and its association with recovery was found to differ by time to recovery, where the latter was collapsed to capture meaningful interactions. Length of recall did not predict recovery in the first 12 months after onset (χ23 = 4.3, p = 0.23), by which time, as seen in Figure 16.1, roughly one-fourth of cases had recovered. Length of recall was significant in months 13–24 (χ23 = 10.8, p = 0.013), by which time roughly half of cases had recovered due to a single significantly reduced OR associated with low-average length of recall (OR = 0.5), but odds of recovery were equivalent for cases with both lower and higher length of recall. It was only in months 25+ that a consistently strong monotonic inverse association emerged between length of recall and odds of recovery (ORs in the range 0.5–0.2 for low-average to high length of recall; χ23 = 95.5, p < 0.001).
Table 16.1 Associations of sex, age at trauma exposure, and length of recall with recovery from DSM-IV/CIDI PTSD in the WMH surveys (n = 1,575)a
| Multivariate model 1 | Multivariate model 1a | Multivariate model 1b | ||||
|---|---|---|---|---|---|---|
| OR | (95% CI) | OR | (95% CI) | OR | (95% CI) | |
| I Sex | ||||||
| Female | 1.1 | (0.9–1.3) | 1.4* | (1.0–2.0) | 0.8* | (0.7–1.0) |
| Male | 1.0 | – | 1.0 | – | 1.0 | – |
| II Age of Trauma | ||||||
| 0–12 | 0.8 | (0.7–1.1) | 0.8 | (0.6–1.2) | 0.9 | (0.7–1.1) |
| 13–24 | 1.0 | – | 1.0 | – | 1.0 | – |
| 25–44 | 1.4* | (1.1–1.6) | 1.4* | (1.1–1.8) | 1.4* | (1.1–1.9) |
| 45–59 | 0.9 | (0.7–1.2) | 1.1 | (0.7–1.5) | 0.8 | (0.6–1.1) |
| 60+ | 0.7 | (0.5–1.0) | 0.6* | (0.4–1.0) | 1.0 | (0.6–1.6) |
| χ24 | 34.3* | 24.1* | 33.4* | |||
| III Years from Trauma Onset by Person-Months | ||||||
| Person-months 1–12 | ||||||
| High | 0.6 | (0.4–1.0) | 0.7 | (0.4–1.1) | ||
| High-average | 1.1 | (0.8–1.5) | 1.1 | (0.8–1.6) | ||
| Low-average | 1.1 | (0.8–1.5) | 1.1 | (0.8–1.5) | ||
| Low | 1.0 | – | 1.0 | – | ||
| χ23 | 4.3 | 5.6 | ||||
| Person-months 13–24 | ||||||
| High | 0.8 | (0.4–1.5) | 0.9 | (0.5–1.5) | ||
| High-average | 0.9 | (0.5–1.5) | 0.9 | (0.5–1.5) | ||
| Low-average | 0.5* | (0.3–0.7) | 0.5* | (0.3–0.8) | ||
| Low | 1.0 | – | 1.0 | – | ||
| χ23 | 10.8* | 9.0* | ||||
| Person-months 25+ | ||||||
| High | 0.2* | (0.1–0.4) | 0.2* | (0.1–0.4) | ||
| High-average | 0.3* | (0.2–0.3) | 0.3* | (0.2–0.5) | ||
| Low-average | 0.5* | (0.4–0.7) | 0.6* | (0.5–0.7) | ||
| Low | 1.0 | – | 1.0 | – | ||
| χ23 | 95.5* | 42.9* | ||||
* Significant at the 0.05 level, two-sided test.
a Coefficients in the first pair of columns are based on a multivariate discrete-time person-month survival model controlling for number of follow-up person-months and survey location among the 1,575 respondents with PTSD associated with random traumas (a total of n = 111,355 person-months). The coefficients in the next columns are based on separate subgroups in multivariate discrete-time person-month survival models for early recovery (months 1–24) and later recovery (months 25–120) among the same 1,575 respondents.
Based on these results, all subsequent analyses were carried out separately for months 1–24 and 25+, with a recognition that results in the latter subsample might be biased due to recall error. Women had a significantly elevated odds of early recovery (OR = 1.4) and a significantly decreased odds of later recovery (OR = 0.8) compared to men (see Table 16.1, models 1a and 1b). Both models found a significantly elevated odds of recovery among respondents whose traumas occurred in middle age (OR = 1.4), whereas odds of early recovery were significantly decreased among respondents whose traumas occurred at ages 60+ (OR = 0.6).
Trauma Type
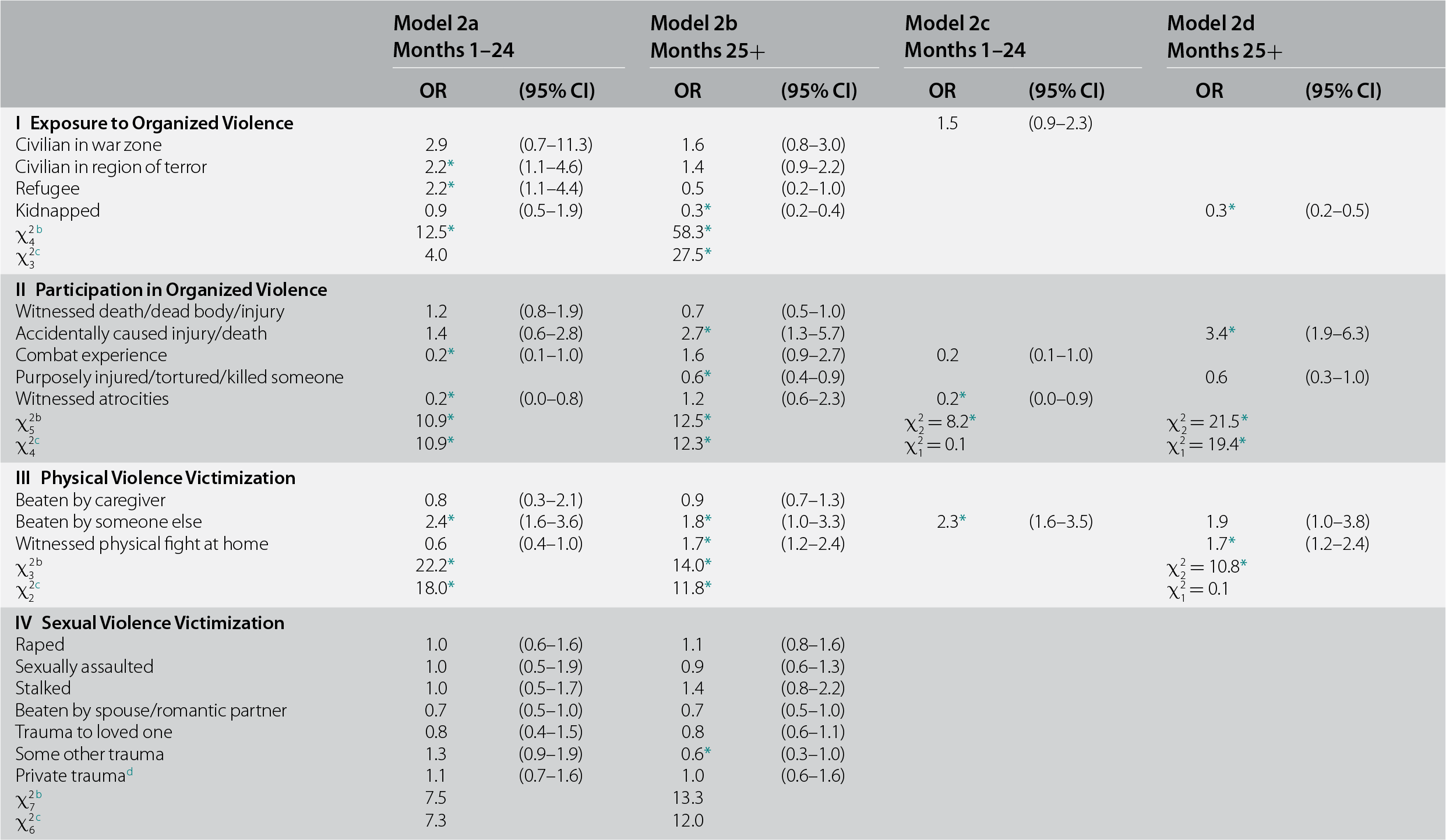
Distribution of random trauma types ranged from a high of 19.8% for unexpected death of a loved one to 0.2% for natural disasters. This wide variation was a joint function of differences in population prevalence (Benjet et al., Reference Benjet, Bromet and Karam2016) and PTSD risk (Liu et al., Reference Liu, Petukhova and Sampson2017). Controlling for the predictors in models 1a and 1b, random trauma type significantly predicted both early (χ226 = 87.8, p < 0.001) and later (χ226 = 201.3, p < 0.001) recovery (see Table 16.2, models 2a and 2b). As none of the respondents whose random trauma was purposefully injuring/torturing/killing someone recovered within 24 months of onset, we removed those respondents from the early-recovery sample. Other traumas in five of the six trauma groups were significant in both the early-recovery and later-recovery models, sexual violence victimization being the exception in both cases. Two of five within-group OR differences were nonsignificant in the early-recovery model, leading us to collapse traumas in these groups in that model. We retained individually significant traumas otherwise. Neither collapsed group (exposure to organized violence, and accidents/injuries) had early-recovery odds significantly different from the omitted category (OR = 1.0–1.5). Being beaten up by someone other than a caregiver or romantic partner was the only trauma that had significantly elevated odds of recovery in the early-recovery (OR = 2.3) model, and two other traumas had significantly reduced odds (witnessed atrocities and mugged/threatened with a weapon; OR = 0.2–0.5). The reduced later-recovery model, in comparison, had four traumas with elevated odds of recovery (accidentally caused serious injury/death, witnessed physical fights at home in childhood, other life-threatening accident, and human-made disaster; OR = 1.7–5.0) and two additional traumas with significantly reduced odds (kidnapped and automobile accident; OR = 0.3–0.6).
Table 16.2 Associations between randomly selected trauma type with recovery from DSM-IV/CIDI PTSD in the WMH surveys (n = 1,575)a
| Model 2a Months 1–24 | Model 2b Months 25+ | Model 2c Months 1–24 | Model 2d Months 25+ | |||||
|---|---|---|---|---|---|---|---|---|
| OR | (95% CI) | OR | (95% CI) | OR | (95% CI) | OR | (95% CI) | |
| I Exposure to Organized Violence | 1.5 | (0.9–2.3) | ||||||
| Civilian in war zone | 2.9 | (0.7–11.3) | 1.6 | (0.8–3.0) | ||||
| Civilian in region of terror | 2.2* | (1.1–4.6) | 1.4 | (0.9–2.2) | ||||
| Refugee | 2.2* | (1.1–4.4) | 0.5 | (0.2–1.0) | ||||
| Kidnapped | 0.9 | (0.5–1.9) | 0.3* | (0.2–0.4) | 0.3* | (0.2–0.5) | ||
| χ24b | 12.5* | 58.3* | ||||||
| χ23c | 4.0 | 27.5* | ||||||
| II Participation in Organized Violence | ||||||||
| Witnessed death/dead body/injury | 1.2 | (0.8–1.9) | 0.7 | (0.5–1.0) | ||||
| Accidentally caused injury/death | 1.4 | (0.6–2.8) | 2.7* | (1.3–5.7) | 3.4* | (1.9–6.3) | ||
| Combat experience | 0.2* | (0.1–1.0) | 1.6 | (0.9–2.7) | 0.2 | (0.1–1.0) | ||
| Purposely injured/tortured/killed someone | 0.6* | (0.4–0.9) | 0.6 | (0.3–1.0) | ||||
| Witnessed atrocities | 0.2* | (0.0–0.8) | 1.2 | (0.6–2.3) | 0.2* | (0.0–0.9) | ||
| χ25b | 10.9* | 12.5* | χ22 = 8.2* | χ22 = 21.5* | ||||
| χ24c | 10.9* | 12.3* | χ21 = 0.1 | χ21 = 19.4* | ||||
| III Physical Violence Victimization | ||||||||
| Beaten by caregiver | 0.8 | (0.3–2.1) | 0.9 | (0.7–1.3) | ||||
| Beaten by someone else | 2.4* | (1.6–3.6) | 1.8* | (1.0–3.3) | 2.3* | (1.6–3.5) | 1.9 | (1.0–3.8) |
| Witnessed physical fight at home | 0.6 | (0.4–1.0) | 1.7* | (1.2–2.4) | 1.7* | (1.2–2.4) | ||
| χ23b | 22.2* | 14.0* | χ22 = 10.8* | |||||
| χ22c | 18.0* | 11.8* | χ21 = 0.1 | |||||
| IV Sexual Violence Victimization | ||||||||
| Raped | 1.0 | (0.6–1.6) | 1.1 | (0.8–1.6) | ||||
| Sexually assaulted | 1.0 | (0.5–1.9) | 0.9 | (0.6–1.3) | ||||
| Stalked | 1.0 | (0.5–1.7) | 1.4 | (0.8–2.2) | ||||
| Beaten by spouse/romantic partner | 0.7 | (0.5–1.0) | 0.7 | (0.5–1.0) | ||||
| Trauma to loved one | 0.8 | (0.4–1.5) | 0.8 | (0.6–1.1) | ||||
| Some other trauma | 1.3 | (0.9–1.9) | 0.6* | (0.3–1.0) | ||||
| Private traumad | 1.1 | (0.7–1.6) | 1.0 | (0.6–1.6) | ||||
| χ27b | 7.5 | 13.3 | ||||||
| χ26c | 7.3 | 12.0 | ||||||
| V Accidents/Injuries | 1.0 | (0.7–1.3) | ||||||
| Natural disaster | 2.6* | (1.3–5.3) | ||||||
| Toxic chemical exposure | 0.7 | (0.2–2.3) | 0.6* | (0.5–0.9) | 0.6 | (0.4–1.0) | ||
| Automobile accident | 1.6* | (1.0–2.6) | 0.5* | (0.4–0.7) | 0.6* | (0.4–0.9) | ||
| Life-threatening illness | 0.9 | (0.5–1.6) | 0.7 | (0.4–1.1) | ||||
| Child with serious illness | 1.4 | (1.0–2.0) | 0.7* | (0.5–1.0) | 0.8 | (0.5–1.2) | ||
| Other life-threatening accident | 0.6 | (0.2–1.9) | 1.8* | (1.4–2.3) | 1.9* | (1.3–2.7) | ||
| χ26b | 14.5* | 76.1* | χ21 = 60.0* | |||||
| χ25c | 9.4 | 76.1* | χ23 = 59.9* | |||||
| VI Other | ||||||||
| Mugged/threatened with a weapon | 0.5* | (0.3–0.9) | 0.7* | (0.6–1.0) | 0.5* | (0.3–0.9) | 0.8 | (0.6–1.1) |
| Human-made disaster | 0.9 | (0.2–3.0) | 5.1* | (3.1–8.4) | 5.0* | (3.1–8.1) | ||
| UD of a loved one | 1.3 | (1.0–1.7) | ||||||
| χ23b | 9.6* | 49.5* | 51.7* | |||||
| χ22c | 9.5* | 48.8* | 48.7* | |||||
| χ227e | 87.8* | 201.3* | χ25 = 37.3* | χ211 = 265.0* | ||||
* Significant at the 0.05 level, two-sided test.
a Coefficients are based on multivariate discrete-time person-month survival models for early recovery (months 1–24) and later recovery (months 25–120) among the 1,575 respondents with PTSD associated with random traumas (a total of n = 111,355 person-months) controlling for number of follow-up person-months, survey location, and all significant variables in Table 18.1 multivariate models 1a and 1b.
b The joint significance of the set of ORs for traumas in the group.
c The significance of differences among the ORs within the group.
d A private trauma is a trauma that some individuals reported in response to a question at the very end of the trauma section that asked if they ever had some other very upsetting experience they did not tell us about already because they were too embarrassed or upset to talk about it. Respondents were told, before they answered, that if they reported such a trauma we would not ask them anything about what it was, only about their age when the trauma happened.
e The joint significance of all traumas in the model.
Prior Traumas
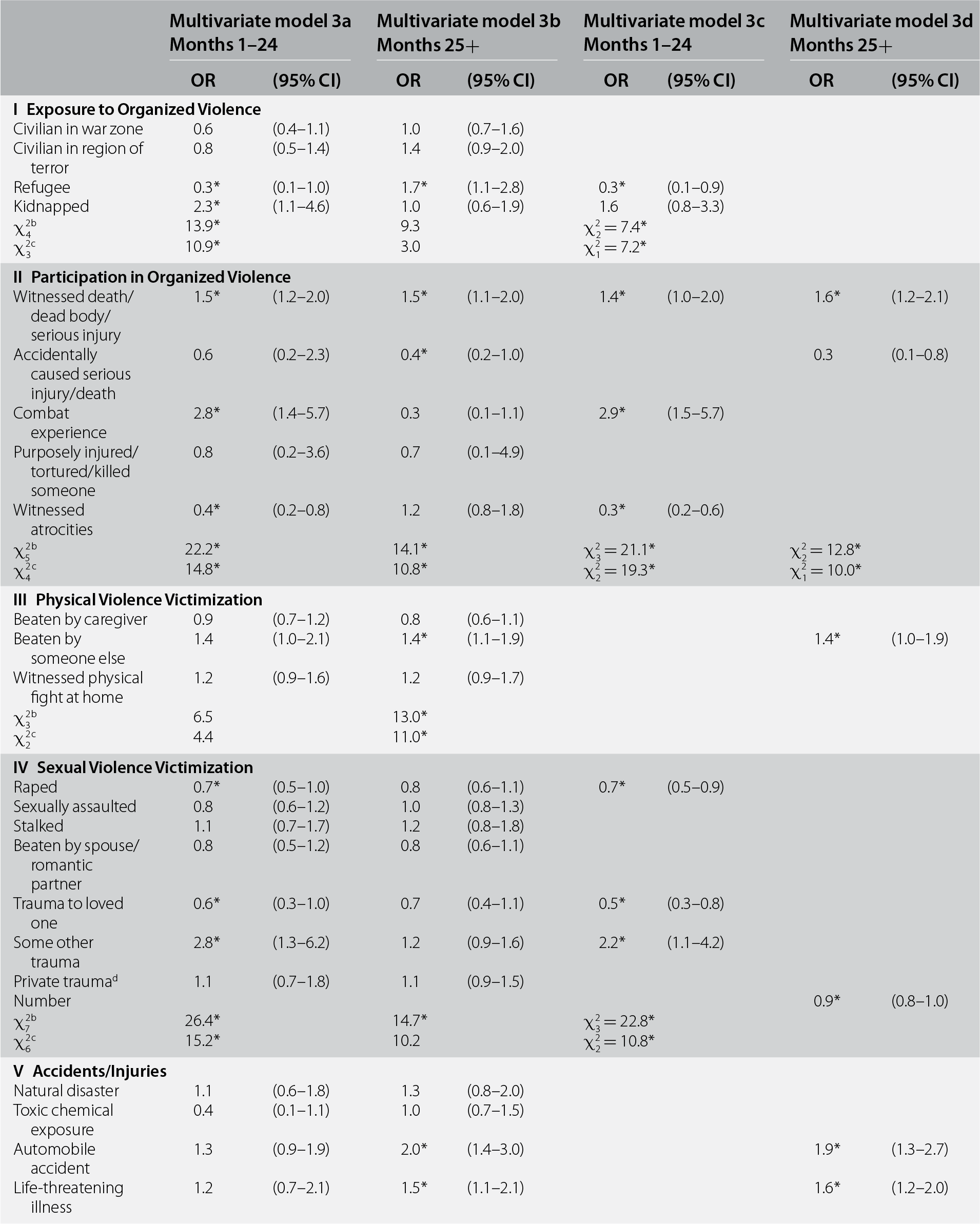
Controlling for the predictors in models 2c and 2d, prior (to age at random trauma exposure) lifetime trauma exposure significantly predicted both early (χ228 = 114.1, p < 0.001) and later (χ228 = 348.2, p < 0.001) recovery (see Table 16.3, models 3a and 3b). Three of the six prior trauma sets were significant in the early-recovery model, in each case with ORs differing significantly within the group, whereas five trauma sets were significant in the later-recovery model (the exception being exposure to organized violence). In one of the latter groups (sexual assault victimization), within-group ORs did not differ significantly from each other, and we consequently entered a count variable of all prior lifetime traumas in that group in the reduced model.
Table 16.3 Associations of history of prior trauma with recovery from DSM-IV/CIDI PTSD in the WMH surveys (n = 1,575)a
| Multivariate model 3a Months 1–24 | Multivariate model 3b Months 25+ | Multivariate model 3c Months 1–24 | Multivariate model 3d Months 25+ | |||||
|---|---|---|---|---|---|---|---|---|
| OR | (95% CI) | OR | (95% CI) | OR | (95% CI) | OR | (95% CI) | |
| I Exposure to Organized Violence | ||||||||
| Civilian in war zone | 0.6 | (0.4–1.1) | 1.0 | (0.7–1.6) | ||||
| Civilian in region of terror | 0.8 | (0.5–1.4) | 1.4 | (0.9–2.0) | ||||
| Refugee | 0.3* | (0.1–1.0) | 1.7* | (1.1–2.8) | 0.3* | (0.1–0.9) | ||
| Kidnapped | 2.3* | (1.1–4.6) | 1.0 | (0.6–1.9) | 1.6 | (0.8–3.3) | ||
| χ24b | 13.9* | 9.3 | χ22 = 7.4* | |||||
| χ23c | 10.9* | 3.0 | χ21 = 7.2* | |||||
| II Participation in Organized Violence | ||||||||
| Witnessed death/dead body/serious injury | 1.5* | (1.2–2.0) | 1.5* | (1.1–2.0) | 1.4* | (1.0–2.0) | 1.6* | (1.2–2.1) |
| Accidentally caused serious injury/death | 0.6 | (0.2–2.3) | 0.4* | (0.2–1.0) | 0.3 | (0.1–0.8) | ||
| Combat experience | 2.8* | (1.4–5.7) | 0.3 | (0.1–1.1) | 2.9* | (1.5–5.7) | ||
| Purposely injured/tortured/killed someone | 0.8 | (0.2–3.6) | 0.7 | (0.1–4.9) | ||||
| Witnessed atrocities | 0.4* | (0.2–0.8) | 1.2 | (0.8–1.8) | 0.3* | (0.2–0.6) | ||
| χ25b | 22.2* | 14.1* | χ23 = 21.1* | χ22 = 12.8* | ||||
| χ24c | 14.8* | 10.8* | χ22 = 19.3* | χ21 = 10.0* | ||||
| III Physical Violence Victimization | ||||||||
| Beaten by caregiver | 0.9 | (0.7–1.2) | 0.8 | (0.6–1.1) | ||||
| Beaten by someone else | 1.4 | (1.0–2.1) | 1.4* | (1.1–1.9) | 1.4* | (1.0–1.9) | ||
| Witnessed physical fight at home | 1.2 | (0.9–1.6) | 1.2 | (0.9–1.7) | ||||
| χ23b | 6.5 | 13.0* | ||||||
| χ22c | 4.4 | 11.0* | ||||||
| IV Sexual Violence Victimization | ||||||||
| Raped | 0.7* | (0.5–1.0) | 0.8 | (0.6–1.1) | 0.7* | (0.5–0.9) | ||
| Sexually assaulted | 0.8 | (0.6–1.2) | 1.0 | (0.8–1.3) | ||||
| Stalked | 1.1 | (0.7–1.7) | 1.2 | (0.8–1.8) | ||||
| Beaten by spouse/romantic partner | 0.8 | (0.5–1.2) | 0.8 | (0.6–1.1) | ||||
| Trauma to loved one | 0.6* | (0.3–1.0) | 0.7 | (0.4–1.1) | 0.5* | (0.3–0.8) | ||
| Some other trauma | 2.8* | (1.3–6.2) | 1.2 | (0.9–1.6) | 2.2* | (1.1–4.2) | ||
| Private traumad | 1.1 | (0.7–1.8) | 1.1 | (0.9–1.5) | ||||
| Number | 0.9* | (0.8–1.0) | ||||||
| χ27b | 26.4* | 14.7* | χ23 = 22.8* | |||||
| χ26c | 15.2* | 10.2 | χ22 = 10.8* | |||||
| V Accidents/Injuries | ||||||||
| Natural disaster | 1.1 | (0.6–1.8) | 1.3 | (0.8–2.0) | ||||
| Toxic chemical exposure | 0.4 | (0.1–1.1) | 1.0 | (0.7–1.5) | ||||
| Automobile accident | 1.3 | (0.9–1.9) | 2.0* | (1.4–3.0) | 1.9* | (1.3–2.7) | ||
| Life-threatening illness | 1.2 | (0.7–2.1) | 1.5* | (1.1–2.1) | 1.6* | (1.2–2.0) | ||
| Child with serious illness | 0.7 | (0.4–1.2) | 1.3 | (0.7–2.6) | ||||
| Other life-threatening accident | 1.1 | (0.6–2.0) | 0.9 | (0.5–1.5) | ||||
| χ26b | 9.9 | 66.2* | χ22 = 46.4* | |||||
| χ25c | 9.9 | 12.4* | χ21 = 0.4 | |||||
| IV Other | ||||||||
| Mugged/threatened with a weapon | 0.9 | (0.6–1.4) | 0.8 | (0.6–1.0) | ||||
| Human-made disaster | 0.6 | (0.3–1.0) | 1.0 | (0.7–1.4) | ||||
| UD of a loved one | 1.1 | (0.8–1.5) | 1.7* | (1.3–2.2) | 1.6* | (1.2–2.0) | ||
| χ23b | 4.2 | 25.1* | ||||||
| χ22c | 3.8 | 22.2* | ||||||
| χ228e | 114.1* | 348.2* | ||||||
* Significant at the 0.05 level, two-sided test.
a Coefficients are based on multivariate discrete-time person-month survival models for early recovery (months 1–24) and later recovery (months 25–120) among the 1,575 respondents with PTSD associated with random traumas (a total of n = 111,355 person-months) controlling for number of follow-up person-months, survey location, and all significant variables in Table 16.2, multivariate models 2c and 2d.
b The joint significance of the set of ORs for traumas in the group.
c The significance of the differences among the ORs within the group.
d A private trauma is a trauma that some individuals reported in response to a question asked at the very end of the trauma section that asked if they ever had some other very upsetting experience they did not tell us about already (and this includes in response to a prior open-ended question about “any other” trauma) because they were too embarrassed or upset to talk about it. Respondents were told, before they answered, that if they reported such a trauma we would not ask them anything about what it was, only about their age when the trauma happened.
e The joint significance of all traumas in the model.
In the reduced early-recovery model, three traumas had significantly elevated odds (witnessed death/dead body/serious injury, combat experience, and the residual “other” trauma category; OR = 1.4–2.9) and four others had significantly reduced odds (refugee, witnessed atrocities, raped, and trauma to loved one; OR = 0.3–0.7). In the reduced later-recovery model (model 3d), five traumas had significantly elevated odds (witnessed death/dead body/serious injury, beaten up by someone other than a caregiver or romantic partner, automobile accident, life-threatening illness, and unexpected death of loved one; OR = 1.4–1.9) and two other significantly reduced odds (accidentally caused serious injury/death and number of sexual violence victimizations; OR = 0.3–0.9).
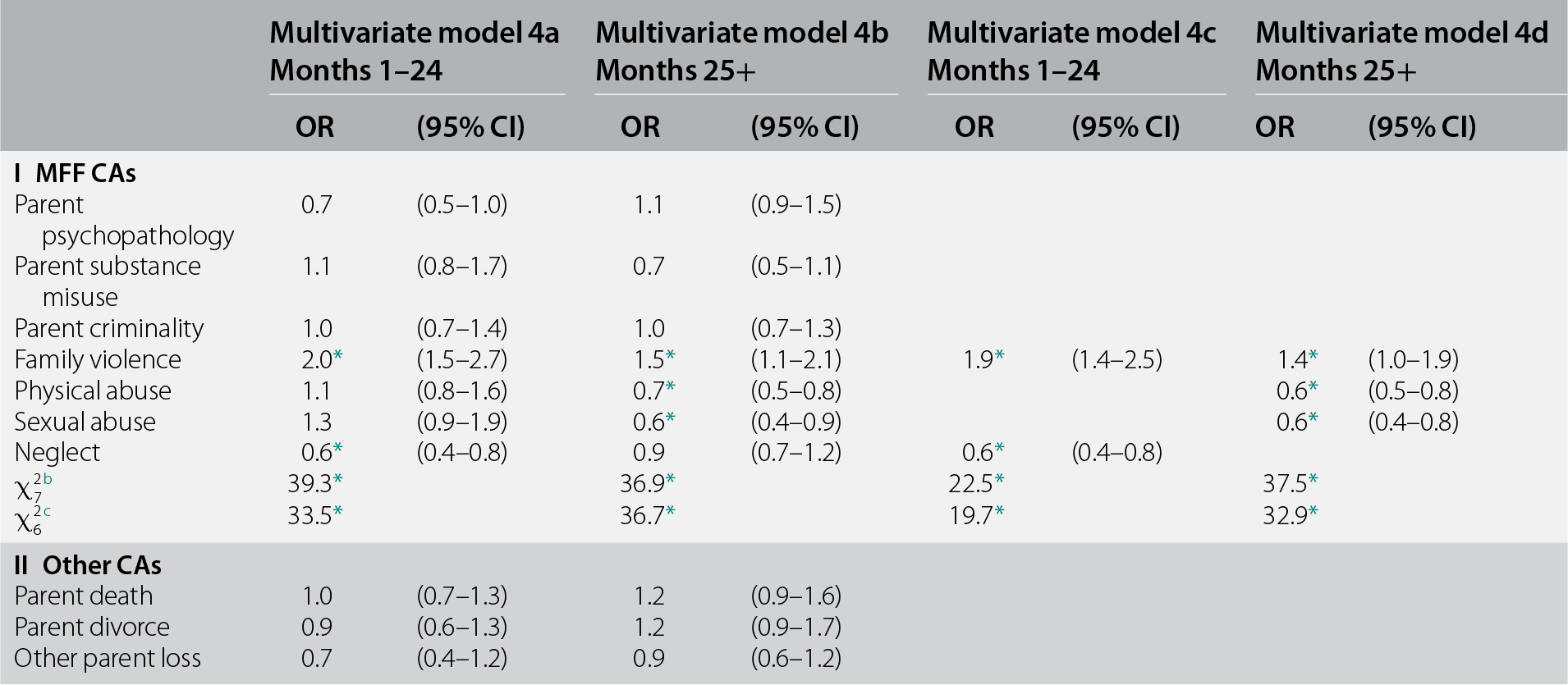
Childhood Adversities
Controlling for the predictors in models 3c and 3d, CAs significantly predicted both early (χ212 = 44.9, p < 0.001) and later (χ212 = 50.8, p < 0.001) recovery (see Table 16.4, models 4a and 4b) In both cases, this was due to maladaptive family functioning (MFF) CAs (χ27 = 36.9–39.3, p < 0.001) rather than other CAs (χ25 = 5.2–5.6, p = 0.35–0.40). One MFF CA, witnessing family violence, was associated with significantly elevated odds of recovery in both early-recovery and later-recovery models (OR = 1.4–1.9) and three others with significantly reduced odds in either the early-recovery (neglect; OR = 0.6) or later-recovery (physical and sexual abuse; OR = 0.6) models.
Table 16.4 Associations between CAs and recovery from DSM-IV/CIDI PTSD in the WMH surveys (n = 1,575)a
| Multivariate model 4a Months 1–24 | Multivariate model 4b Months 25+ | Multivariate model 4c Months 1–24 | Multivariate model 4d Months 25+ | |||||
|---|---|---|---|---|---|---|---|---|
| OR | (95% CI) | OR | (95% CI) | OR | (95% CI) | OR | (95% CI) | |
| I MFF CAs | ||||||||
| Parent psychopathology | 0.7 | (0.5–1.0) | 1.1 | (0.9–1.5) | ||||
| Parent substance misuse | 1.1 | (0.8–1.7) | 0.7 | (0.5–1.1) | ||||
| Parent criminality | 1.0 | (0.7–1.4) | 1.0 | (0.7–1.3) | ||||
| Family violence | 2.0* | (1.5–2.7) | 1.5* | (1.1–2.1) | 1.9* | (1.4–2.5) | 1.4* | (1.0–1.9) |
| Physical abuse | 1.1 | (0.8–1.6) | 0.7* | (0.5–0.8) | 0.6* | (0.5–0.8) | ||
| Sexual abuse | 1.3 | (0.9–1.9) | 0.6* | (0.4–0.9) | 0.6* | (0.4–0.8) | ||
| Neglect | 0.6* | (0.4–0.8) | 0.9 | (0.7–1.2) | 0.6* | (0.4–0.8) | ||
| χ27b | 39.3* | 36.9* | 22.5* | 37.5* | ||||
| χ26c | 33.5* | 36.7* | 19.7* | 32.9* | ||||
| II Other CAs | ||||||||
| Parent death | 1.0 | (0.7–1.3) | 1.2 | (0.9–1.6) | ||||
| Parent divorce | 0.9 | (0.6–1.3) | 1.2 | (0.9–1.7) | ||||
| Other parent loss | 0.7 | (0.4–1.2) | 0.9 | (0.6–1.2) | ||||
| Serious physical illness | 1.3 | (0.8–2.0) | 0.9 | (0.6–1.3) | ||||
| Economic adversity | 0.9 | (0.5–1.4) | 1.0 | (0.8–1.4) | ||||
| χ25b | 5.2 | 5.6 | ||||||
| χ24c | 4.0 | 5.2 | ||||||
| χ212d | 44.9* | 50.8* | ||||||
* Significant at the 0.05 level, two-sided test.
a Coefficients are based on multivariate discrete-time person-month survival models for early recovery (months 1–24) and later recovery (months 25–120) among the 1,575 respondents with PTSD associated with random traumas (a total of n = 111,355 person-months) controlling for number of follow-up person-months, survey, and all significant variables in Table 16.3, multivariate models 3c and 3d.
b The joint significance of the full set of ORs for CAs in the group.
c The significance of the differences among the ORs within the group.
d The joint significance of all CAs in the model.
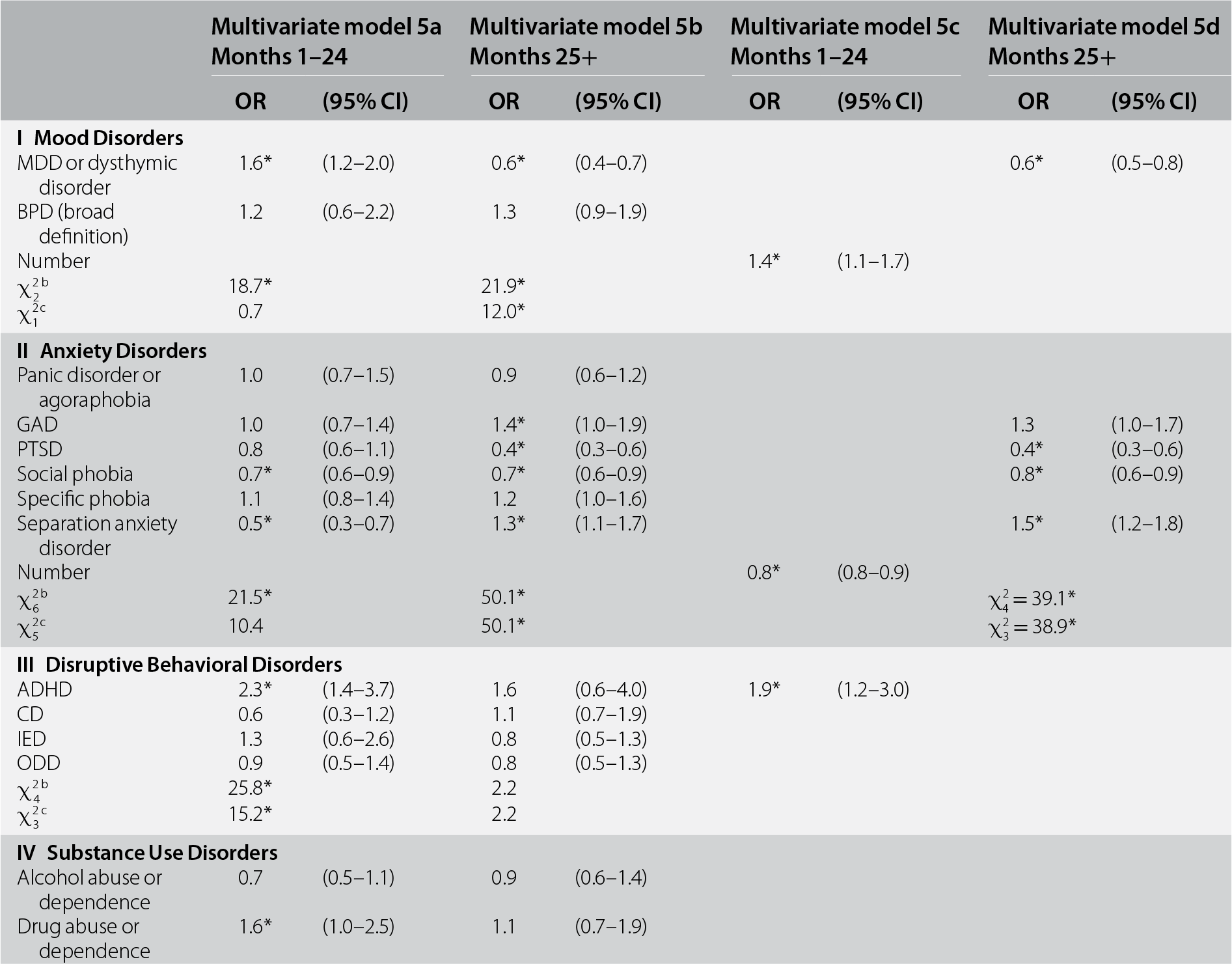
Mental Disorders
Controlling for earlier predictors, prior (to age at random trauma exposure) lifetime DSM-IV/CIDI disorders significantly predicted both early (χ214 = 66.3, p < 0.001) and later (χ214 = 78.4, p < 0.001) recovery. Mood and anxiety disorders were significant as sets in both models, although ORs did not vary within either group in the early-recovery model, but did in the later-recovery model (see Table 16.5, models 5a and 5b). Disruptive behavior disorders were also significant as a set (with significant within-group differences in ORs) in the early-recovery model, but not the later-recovery model. Substance use disorders were not significant as a set in either model. In the reduced early-recovery model (model 5c), number of mood disorders and ADHD were associated with significantly elevated odds of recovery (OR = 1.4–1.9) and number of anxiety disorders with significantly reduced odds (OR = 0.8). In the reduced later-recovery model (model 5d), prior separation anxiety disorder was associated with significantly elevated odds of recovery (OR = 1.5), whereas major depression-dysthymia, PTSD, and social phobia had significantly reduced odds (OR = 0.4–0.8).
Table 16.5 Associations between mental disorders prior to randomly selected trauma and recovery from DSM-IV/CIDI PTSD in the WMH surveys (n = 1,575)a
| Multivariate model 5a Months 1–24 | Multivariate model 5b Months 25+ | Multivariate model 5c Months 1–24 | Multivariate model 5d Months 25+ | |||||
|---|---|---|---|---|---|---|---|---|
| OR | (95% CI) | OR | (95% CI) | OR | (95% CI) | OR | (95% CI) | |
| I Mood Disorders | ||||||||
| MDD or dysthymic disorder | 1.6* | (1.2–2.0) | 0.6* | (0.4–0.7) | 0.6* | (0.5–0.8) | ||
| BPD (broad definition) | 1.2 | (0.6–2.2) | 1.3 | (0.9–1.9) | ||||
| Number | 1.4* | (1.1–1.7) | ||||||
| χ22b | 18.7* | 21.9* | ||||||
| χ21c | 0.7 | 12.0* | ||||||
| II Anxiety Disorders | ||||||||
| Panic disorder or agoraphobia | 1.0 | (0.7–1.5) | 0.9 | (0.6–1.2) | ||||
| GAD | 1.0 | (0.7–1.4) | 1.4* | (1.0–1.9) | 1.3 | (1.0–1.7) | ||
| PTSD | 0.8 | (0.6–1.1) | 0.4* | (0.3–0.6) | 0.4* | (0.3–0.6) | ||
| Social phobia | 0.7* | (0.6–0.9) | 0.7* | (0.6–0.9) | 0.8* | (0.6–0.9) | ||
| Specific phobia | 1.1 | (0.8–1.4) | 1.2 | (1.0–1.6) | ||||
| Separation anxiety disorder | 0.5* | (0.3–0.7) | 1.3* | (1.1–1.7) | 1.5* | (1.2–1.8) | ||
| Number | 0.8* | (0.8–0.9) | ||||||
| χ26b | 21.5* | 50.1* | χ24 = 39.1* | |||||
| χ25c | 10.4 | 50.1* | χ23 = 38.9* | |||||
| III Disruptive Behavioral Disorders | ||||||||
| ADHD | 2.3* | (1.4–3.7) | 1.6 | (0.6–4.0) | 1.9* | (1.2–3.0) | ||
| CD | 0.6 | (0.3–1.2) | 1.1 | (0.7–1.9) | ||||
| IED | 1.3 | (0.6–2.6) | 0.8 | (0.5–1.3) | ||||
| ODD | 0.9 | (0.5–1.4) | 0.8 | (0.5–1.3) | ||||
| χ24b | 25.8* | 2.2 | ||||||
| χ23c | 15.2* | 2.2 | ||||||
| IV Substance Use Disorders | ||||||||
| Alcohol abuse or dependence | 0.7 | (0.5–1.1) | 0.9 | (0.6–1.4) | ||||
| Drug abuse or dependence | 1.6* | (1.0–2.5) | 1.1 | (0.7–1.9) | ||||
| χ22b | 4.6 | 0.3 | ||||||
| χ21c | 4.0* | 0.2 | ||||||
| χ214d | 66.3* | 78.4* | χ23 = 26.9* | χ25 = 52.9* | ||||
* Significant at the 0.05 level, two-sided test.
a Coefficients are based on multivariate discrete-time person-month survival models for early recovery (months 1–24) and later recovery (months 25–120) among the 1,575 respondents with PTSD associated with random traumas (a total of n = 111,355 person-months) controlling for number of follow-up person-months, survey location, and all significant variables in earlier models.
b The joint significance of the set of ORs for mental disorders in the group.
c The significance of the difference among the ORs within the group.
d The joint significance of all the mental disorders in the model.
Overall Model Performance
Each respondent was assigned 20 predicted probabilities of recovery in each person-month, based on the coefficients in 20 replicates of 10-fold cross-validated versions of models with the predictors in models 5c and 5d (i.e., the final models), but with coefficients allowed to vary across these replicates. The observations in these two sets of 20 replicates were then divided into three groups consisting of the cases in the top 25%, next 25%, and lowest 50% of predicted probabilities of recovery. Speed-of-recovery curves based on observed time to recovery in these subgroups were then generated to simulate the likely performance of the models in an independent dataset (see Figure 16.2).

Figure 16.2 Speed of recovery from random trauma PTSD within subgroups defined by cross-validated final model predicted probability of recovery separately for early-recovery (a, 1–24 months) and later-recovery (b, 25–120 months) models
The model distinguished well the two groups predicted to have highest probabilities of recovery (i.e., top 25% and next 25%) from the 50% with lowest predicted probability of recovery and less well between the top two groups. It took 3–4 months for 25% of respondents in the top two groups to recover compared to 12 months in the group predicted to have lowest probability of recovery (see Figure 16.2a). It took 12 months for 50% of respondents in the top group to recover, and 66% recovered by 24 months, compared to 55% in the middle group and 42% in the group with lowest predicted probability of recovery. Seventy-five percent of respondents with highest predicted probability of later recovery did, in fact, recover within 10 years of onset (25% within 3 years, 50% within 5 years), compared to 68% of those with intermediate predicted probabilities (25–50% within 5 years) and 39% of those with lowest predicted probabilities (25% within 5 years) (see Figure 16.2b).
Discussion
Despite substantial variation in the definition of “recovery” in prior studies of PTSD course (Steinert et al., Reference Steinert, Hofmann, Leichsenring and Kruse2015), our findings that 50% of WMH respondents with PTSD recovered within 2 years and roughly 25% had not recovered within 10 years are broadly consistent with previous epidemiological estimates of PTSD recovery after random traumas (Breslau et al., Reference Breslau, Kessler and Chilcoat1998). However, it should be noted that slightly lower and slower rates of recovery have been reported in epidemiological studies of PTSD based on “worst” traumas (Kessler et al., Reference Kessler, Sonnega, Bromet, Hughes and Nelson1995; Chapman et al., Reference Chapman, Mills and Slade2012).
Our failure to find a sex difference in PTSD recovery is consistent with the results of a meta-analysis of predictors of PTSD recovery (Morina et al., Reference Morina, Wicherts, Lobbrecht and Priebe2014). Our finding of opposite-sign sex differences in early recovery (women higher recovery than men) and later recovery (women lower recovery than men) is new as no previous studies have examined interactions between predictors and timing of recovery. Nor are we aware of any previous research that addresses the significant association we found between length of recall and retrospective reports about PTSD recovery. As noted earlier, this association is most plausibly interpreted as resulting from a recall bias related to length of the recall period. But this association was largely confined to later recovery, so our results regarding the predictors of early recovery may well have been less influenced by recall bias.
Very low relative odds of early recovery (OR = 0.0–0.3) were found for two trauma types (purposefully injuring/torturing/killing someone and witnessing atrocities) and of later recovery for another (being kidnapped). Very high odds of early recovery (OR = 3.0+) were found for no trauma types and of later recovery for two trauma types (accidentally causing injury/death, and human-made disaster). Other significant between-trauma differences in recovery were few in number and comparatively modest in magnitude. No trauma type was a significant predictor in both early-recovery and later-recovery models. These results are broadly consistent with prior research showing that between-trauma differences in recovery rates are for the most part nonsignificant (Morina et al., Reference Morina, Wicherts, Lobbrecht and Priebe2014). While the literature suggests there is an exception to this general pattern – that there is a significantly higher recovery rate from natural disasters than from other traumas – the WMH data did not replicate this finding.
We are unaware of previous epidemiological research on the associations of PTSD recovery with prior traumas or CAs, even though both factors have consistently been found to predict increased risk of onset of PTSD (Liu et al., Reference Liu, Petukhova and Sampson2017; McLaughlin et al., Reference McLaughlin, Koenen and Bromet2017). In the WMH data, history of being a refugee and of witnessing atrocities (early recovery) and accidentally causing serious injury/death (later recovery) were the only prior traumas associated with very low odds of recovery. No prior trauma type was associated with very high odds of recovery, and no CAs were associated either with very low or with very high odds of recovery. No prior trauma type other than witnessing death/dead body/serious injury, and no CA other than exposure to childhood family violence was a significant predictor in both the early-recovery and later-recovery models. However, the consistently significant ORs for these variables were not large (OR = 1.4–1.9).
Our finding that history of DSM-IV anxiety disorders (i.e., number of disorders, social phobia, and PTSD) was associated with decreased likelihood of PTSD recovery is broadly consistent with the results of both cohort (Pietrzak et al., Reference Pietrzak, Feder and Singh2014) and clinical (Zlotnick et al., Reference Zlotnick, Rodriguez and Weisberg2004) studies that found comorbid prior anxiety disorders to be associated with a more chronic course of PTSD. It is noteworthy, though, that separation anxiety disorder was associated with decreased likelihood of early PTSD recovery, but increased likelihood of later recovery. Such divergent results may help explain why a summary measure of any pretrauma anxiety disorder was not significantly associated with PTSD recovery in the one prior general population epidemiological study that examined these associations using retrospective reports (Chapman et al., Reference Chapman, Mills and Slade2012). We are unaware of prior studies that examined the association of temporally primary ADHD with PTSD recovery.
Our finding that observed recovery curves differed substantially between the subgroups defined as having higher and lower predicted probabilities of recovery raises the possibility that a model such as the ones presented here could be developed at the time of trauma exposure to classify survivors into those with higher and lower probabilities of recovery. However, it is unclear how much value such a model would have for targeting interventions. After all, much more robust models that predict PTSD onset already exist (Kessler et al., Reference Kessler, Rose and Koenen2014), and various post-trauma factors, such as initial treatment response, which are not available at the time of trauma exposure, have been found to predict recovery (Brackbill et al., Reference Brackbill, Hadler and DiGrande2009; North et al., Reference North, Pfefferbaum, Kawasaki, Lee and Spitznagel2011; Pietrzak et al., Reference Pietrzak, Feder and Singh2014). The receipt of an evidence-based treatment for PTSD, which we did not evaluate here, is also an important determinant of PTSD recovery (Courtois et al., Reference Courtois, Sonis and Brown2017). Nonetheless, our results are noteworthy, given that the pretrauma predictors considered here as well as the random trauma type are associated with striking differences in the shape of speed-of-recovery curves.
A number of limitations of the analysis are noteworthy. First, the data were based on retrospective reports that are subject to recall bias. Second, PTSD was assessed with a fully structured diagnostic interview with a low sensitivity rather than with a semi-structured clinical interview, while recovery was defined using a relatively coarse dichotomous measure. Third, the predictors were limited to those available in the survey, namely, socio-demographics, CAs, prior (to the index trauma) traumas, and prior psychopathology. Fourth, we did not take into consideration treatment or other factors that occurred after the trauma. Within the context of these limitations, we analyzed a unique cross-national epidemiological sample. We focused on representative PTSD cases associated with randomly selected traumas. We replicated the findings in previous studies that a substantial minority of PTSD cases recover within a short period of time, that the majority of cases recover within 2 years, and that another substantial minority of cases do not recover even after many years. We found weak evidence for associations of socio-demographics, trauma types, and trauma history with recovery. We found that prior anxiety disorders predict recovery, but again with fairly modest magnitudes of association. Although our composite risk model discriminated well between the recovery trajectories within the 50% of patients predicted to have the highest and lowest probabilities of recovery, this recovery model was much weaker than models using the same kinds of pretrauma variables to predict PTSD onset, highlighting the importance of including information on post-trauma symptoms and experiences to develop robust models of PTSD recovery.