No CrossRef data available.
Article contents
Effectiveness of a Staphylococcus aureus mupirocin decolonization protocol in a neonatal intensive care unit
Published online by Cambridge University Press: 29 September 2023
Abstract
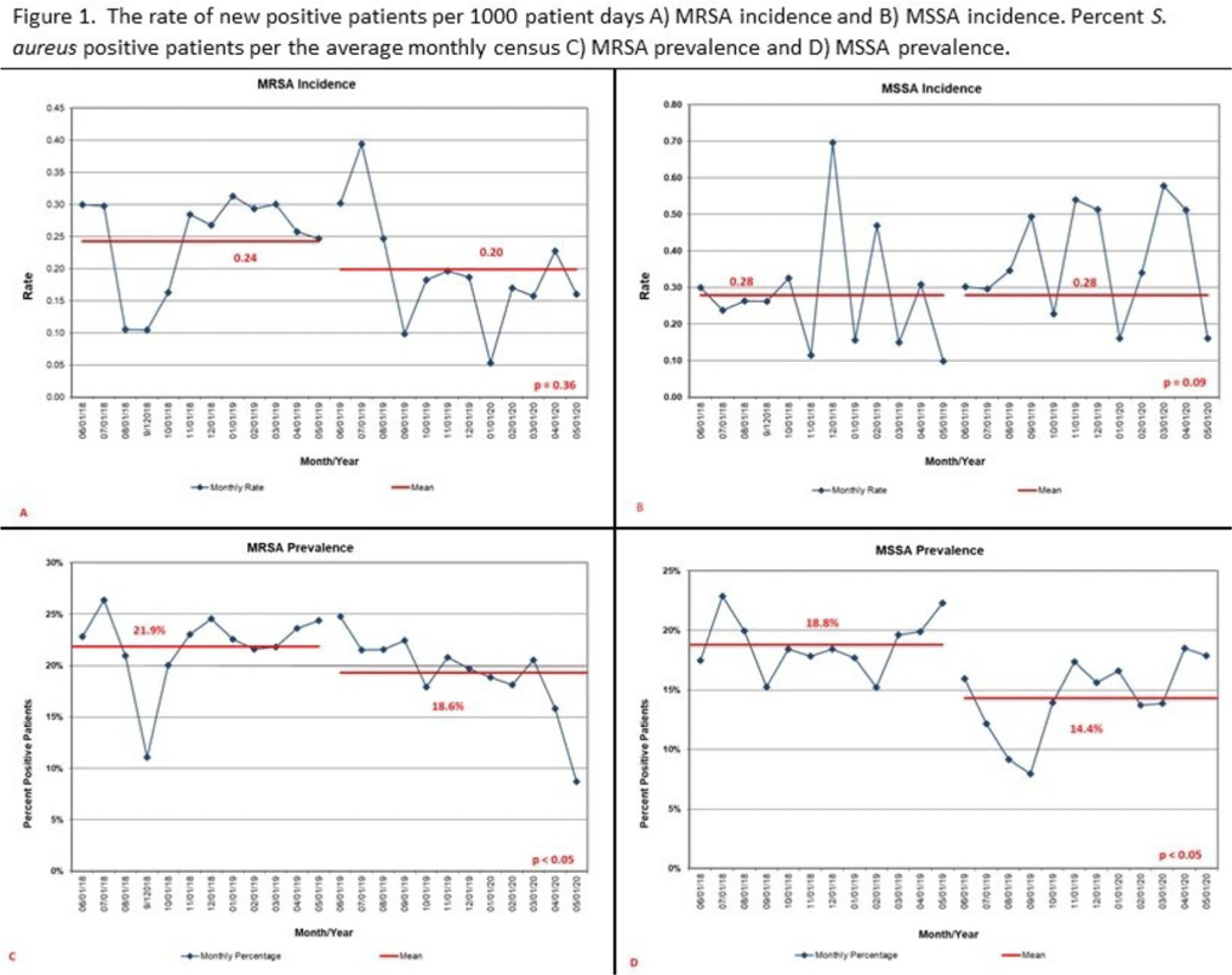
Background: Staphylococcus aureus infections are a significant cause of morbidity in neonatal intensive care units (NICUs), and they are typically preceded by nasal colonization. Mupirocin decolonization protocols as an infection prevention tool can halt S. aureus outbreaks and prevent infections. We examined the effect of a mupirocin treatment protocol on S. aureus incidence, prevalence, decolonization, and infections in a level IV NICU. Methods: We conducted a retrospective before-and-after observational study from June 1, 2018, to May 31, 2020. Beginning June 1, 2019, patients identified with either methicillin-sensitive or -resistant S. aureus (MSSA or MRSA) received mupirocin ointment to bilateral nares 3 times daily for 5 days. Patients with central lines or surgical incisions were treated every 30 days. All NICU patients were screened weekly unless positive for MRSA. We defined MSSA decolonization as 3 consecutive negative screens following mupirocin treatment. We calculated monthly S. aureus incidence as any new positive per 1,000 patient days and monthly prevalence as a percentage of the average daily number of patients with S. aureus per the average monthly census. Total number of infections were compared. Statistical significance was determined using a 2 sample proportions test and P < .05. Decolonization was calculated as percentage of occurrences among treated patients. Results: Overall, 190 patients received mupirocin; 142 patients received 1 course and 48 received 2 or more courses. There was no difference in incidence of MSSA (P = .09), but prevalence decreased from 18.8% to 14.4% (P < .05) (Fig. 1). Of 66 patients with MSSA, 35% were decolonized. An additional mupirocin treatment for 16 of these patients had a 50% decolonization rate. For MRSA, incidence decreased from 0.24 to 0.20 (P = .36) and prevalence decreased from 21.9% to 18.6% (P < .05) (Fig. 1). There was no statistical difference in the number of total S. aureus infections (P = .91) or when stratified by MSSA (P = .72) or MRSA (P = .82). In the postmupirocin population, there were 5 MRSA and 7 MSSA infections. Of the MSSA-infected patients, 6 remained colonized at the time of infection. Conclusions: Implementing a single mupirocin treatment course for S. aureus decolonization in NICU was only effective in one-third of patients and had no effect on infection occurrence. Changes in incidence and prevalence could be confounded by other infection prevention practices. Further study is needed to determine whether continued screening and additional mupirocin treatment could improve effectiveness of S. aureus decolonization programs.
Disclosure: None
- Type
- Decolonization Strategies
- Information
- Antimicrobial Stewardship & Healthcare Epidemiology , Volume 3 , Issue S2: SHEA Spring 2023 Abstracts , June 2023 , pp. s8
- Creative Commons
- This is an Open Access article, distributed under the terms of the Creative Commons Attribution licence (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted re-use, distribution, and reproduction in any medium, provided the original work is properly cited.
- Copyright
- © The Author(s), 2023. Published by Cambridge University Press on behalf of The Society for Healthcare Epidemiology of America




