No CrossRef data available.
Article contents
Sleep spindle and slow wave activity in Bipolar Disorder: preliminary observations from a high–density EEG study
Published online by Cambridge University Press: 19 July 2023
Abstract
Recent research on Schizophrenia (SCZ) suggests that reduced sleep spindle and slow wave density could be particularly informative of underlying thalamocortical and cortical synchronization mechanisms and dysfunctions. Although sleep disturbances are also highly prevalent across all stages of Bipolar Disorder (BD), the objective evaluation of sleep macrostructure and microstructural oscillatory activity remains understudied in this population.
We aimed to investigate sleep EEG activity in BD, with a focus on sleep architecture, sleep spindles and slow waves.
We recorded high-density EEG (64–channel BrainAmp, Brain Products GmbH, Germany) during sleep in 18 euthymic patients with BD and 18 age/gender-matched healthy control (HC) subjects. After sleep scoring and EEG artifact rejection, several parameters of sleep spindles (12-16 Hz), including density and amplitude, and slow waves (0.1-4 Hz) were identified for the first cycle of sleep using automated algorithms and compared between groups using non-parametric statistics.
BD subjects showed significantly higher Wake After Sleep Onset and lower Sleep Efficiency (Table 1). Total (12 - 16 Hz), slow (12 - 14 Hz) and fast (14 - 16 Hz) sleep spindle parameters of density (Image 1) and amplitude did not differ significantly between groups. On the other hand, slow wave density was reduced in a large frontal cluster of electrodes in the BD group (Image 2).Table 1
| BD (n = 18) | HC (n = 18) | Difference(p value) | |
|---|---|---|---|
| WASO (min ± sd) | 140,61 ± 74,23 | 84,34 ± 59,84 | 0,017 |
| Sleep efficiency (% ± sd) | 72,47 ± 14,33 | 82,43 ± 11,58 | 0,028 |
Image:
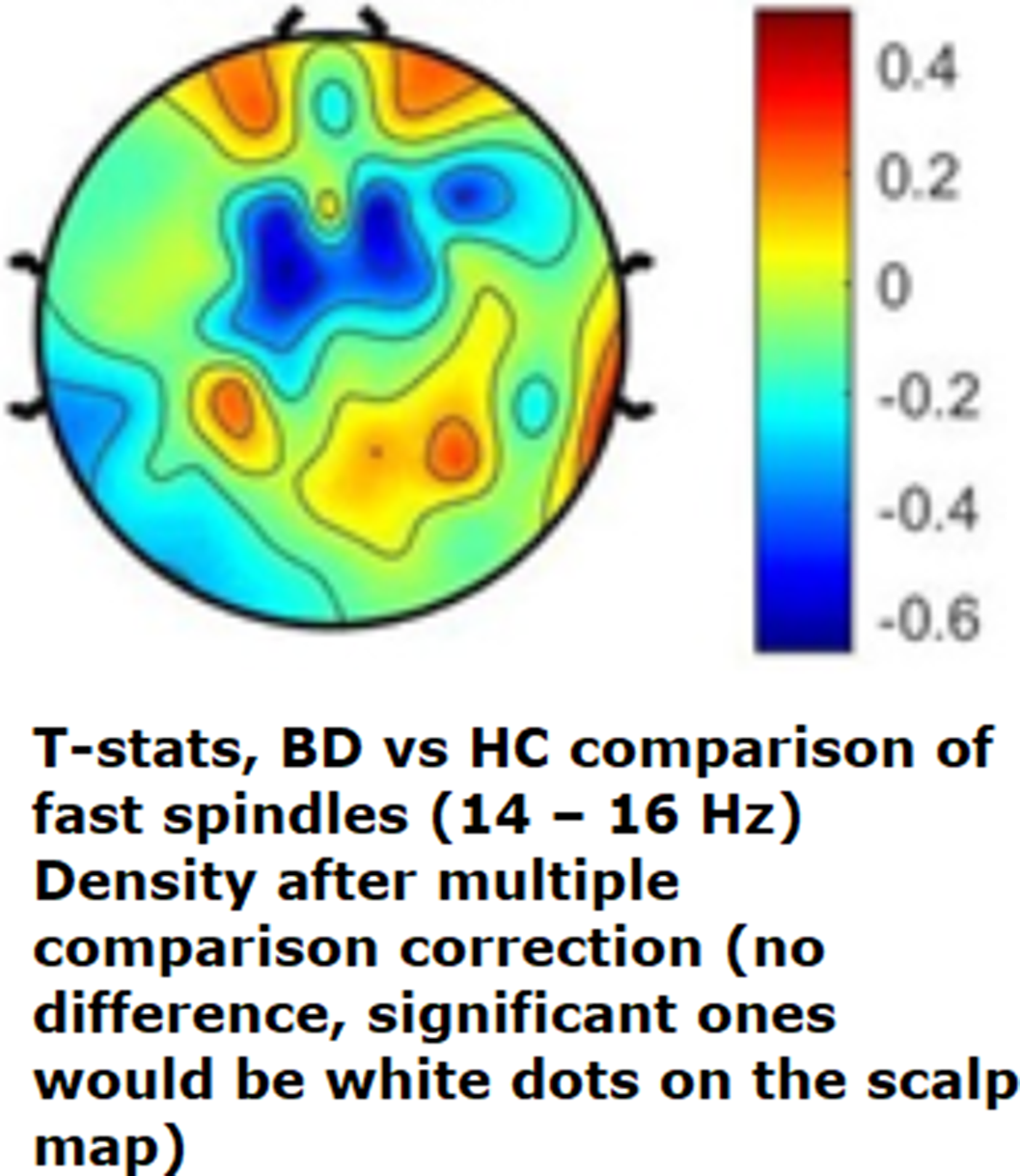
Image 2:
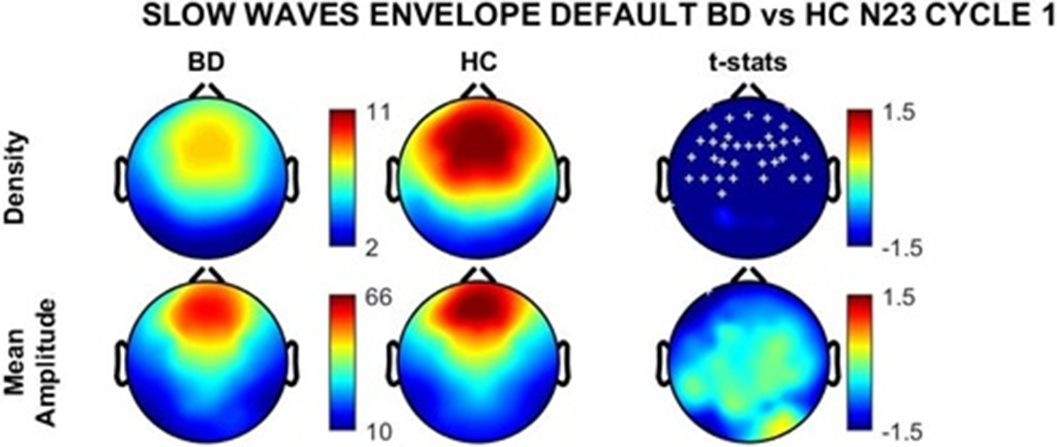
The absence of sleep spindle deficits in the BD group suggests that the systems involved in generating and maintaining these thalamocortical oscillations are presevered during periods of clinical stability in Bipolar Disorder. Conversely, reduced sleep slow wave density points to an altered cortical synchronization, which might represent a common neurophysiological feature shared with Schizophrenia. Further research is needed to confirm these preliminary observations in all–night recordings and with a direct comparison of larger cohorts of patients with both diagnoses.
None Declared
- Type
- Abstract
- Information
- European Psychiatry , Volume 66 , Special Issue S1: Abstracts of the 31st European Congress of Psychiatry , March 2023 , pp. S506 - S507
- Creative Commons
- This is an Open Access article, distributed under the terms of the Creative Commons Attribution licence (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted re-use, distribution, and reproduction in any medium, provided the original work is properly cited.
- Copyright
- © The Author(s), 2023. Published by Cambridge University Press on behalf of the European Psychiatric Association





Comments
No Comments have been published for this article.