Background
The World Health Organization (WHO) reports that mental health conditions are the leading causes of disability worldwide (WHO, 2019). It is estimated 970 million people globally, about 13% of the world's population, suffer from a mental health condition (Ritchie and Roser, Reference Ritchie and Roser2018). However, most people do not receive treatment or support. In Latin America and the Caribbean, the gap between those with mental health problems and those receiving mental health care (the ‘treatment gap’) is almost 75% (Kohn, Reference Kohn2017). This treatment gap is variable throughout the region, from 56.9% for schizophrenia to 73.9% for depression and 85.1% for alcohol use disorders (PAHO, 2021).
The mental health of populations can also be profoundly affected by health emergencies such as epidemics. During the severe acute respiratory syndrome (SARS) epidemic in Hong Kong between 2005 and 2006, the cumulative incidence of mental health problems in a cohort of patients reached almost 60%, with a high incidence of depression (44%) and post-traumatic stress disorder (PTSD) (47.8%) (Mak et al., Reference Mak, Chu, Pan, Yiu and Chan2009). Another study during the outbreak of Middle East respiratory syndrome in Korea in 2015 showed that almost half of affected people described anxiety during isolation (Jeong et al., Reference Jeong, Yim, Song, Ki, Min, Cho and Chae2016). Health personnel can also develop distress during and after epidemics as described in healthcare workers during an outbreak of SARS in Hong Kong (Chua et al., Reference Chua, Cheung, Cheung, McAlonan, Wong, Cheung, Chan, Wong, Tang, Choy, Wong, Chu and Tsang2004) and in 20% of health personnel (doctors and nurses) of a regional hospital in Singapore who reported PTSD 2 months after a SARS outbreak ended (Chan and Huak, Reference Chan and Huak2004).
In December 2019, a pneumonia outbreak caused by a new coronavirus was reported in Wuhan, China (WHO, 2019). By February 2020, this new disease, renamed COVID-19, was declared a pandemic, and by March the pandemic had caused significant clinical, political, social, and economic changes across the globe (Bonotti and Zech, Reference Bonotti, Zech, Bonotti and Zech2021), including mental health services disruption in 93% of the world's countries (WHO, 2020). In Latin America, the rapid spread of COVID-19 challenged even the most robust and resourceful health systems with experience responding to epidemics. In March 2020, the Peruvian government declared a state of national emergency due to the COVID-19 pandemic, establishing curfews and social distancing measures. By June 2020, the Ministry of Health (MINSA) reported 251 338 cases of COVID-19 in Peru (MINSA, 2020a, 2020b, 2020c, 2020d), and by early 2022 Peru registered the highest mortality rate related to COVID-19 in the world, with additional associated crises including hunger and orphanhood.
In the face of fear, concern, stress, and uncertainty in populations suffering from COVID-19, effective mental health interventions are an essential aspect of pandemic response (WHO, 2021). To respond to mental health needs during emergencies, the Inter-Agency Standing Committee (IASC) recommends implementing Psychological First Aid (PFA) as a first-line response to distress (IASC, 2007, 2020; Fox et al., Reference Fox, Burkle, Bass, Pia, Epstein and Markenson2012). The increase in mental health problems in emergencies also offers an opportunity to improve mental health service delivery (WHO, 2013). The United Nations has proposed national response plans for COVID-19 that include mental health care to ensure support for people already living with mental health conditions and lay the groundwork for building quality mental health services in the future (United Nations, 2020). The WHO also reports transitioning from face-to-face to remote service delivery during COVID-19 for infection prevention and control could have the potential long-term benefit of increasing access to mental health care by reducing costs and increasing the geographic distribution of care, benefits that have been demonstrated through remote provision of mental health services in other non-epidemic settings (Plata et al., Reference Plata, López, Baca and Gómez2014; López-Santín and Álvaro, Reference López-Santín and Álvaro Serón2018).
Digital technologies have increasingly captured the human imagination for mental health care delivery, recently being implemented in practice across global settings with dramatically increased uptake since the onset of COVID-19 (Stein et al., Reference Stein, Naslund and Bantjes2022). ‘Chatbots’, which are digital conversational agents that offer an intelligent and automated system for detecting and responding to immediate mental health needs, are currently being incorporated into digital mental health interventions (DMHI) to perform different functions such as screening, follow-up, and assistance, thus facilitating the access to mental health care, and have been found to be useful in the context of a broader treatment plan or program in settings with few human resources (Torous et al., Reference Torous, Bucci, Imogen, Kessing, Faurholt-Jepsen, Whelan, Carvalho, Keshavan, Linardon and Firth2021). Chatbots have been used effectively as a first contact screening or assessment tool to acquire clinical information (Crespo and Dominguez, Reference Crespo and Dominguez2020), as screening tools to identify people who are at risk of presenting anxiety, depression, attention-deficit/hyperactivity disorder, and other psychiatric symptoms, allowing an early intervention and reducing the likelihood of future complications (Rodríguez et al., Reference Rodríguez, Celis, Muñoz, García and Torres2018; Chieng and Medina, Reference Chieng and Medina2020; Dosovitsky et al., Reference Dosovitsky, Pineda, Jacobson, Chang, Escoredo and Bunge2020; Balaskas et al., Reference Balaskas, Schueller, Cox and Doherty2021; Boucher et al., Reference Boucher, Mcnaughton, Harake, Stafford and Parks2021). Chatbots have also been used to reach large populations and to collect information on the health of populations (Adamopoulou and Moussiades, Reference Adamopoulou, Moussiades, Maglogiannis, Iliadis and Pimenidis2020; Bonales et al., Reference Bonales, Pradilla and Citlali2021). Chatbots may also potentially serve as digital tools for administering psychotherapy that does not involve high degree of complexity such as cognitive behavioral therapy (Fitzpatrick et al., Reference Fitzpatrick, Darcy and Vierhile2017) and acceptance/commitment therapy (Montenegro et al., Reference Montenegro, Da Costa and Da Rosa2019). Chatbot technology was identified early in the Peruvian COVID-19 response as potentially helpful in extending support to vulnerable communities.
In Peru, the need for a mental health response to the coronavirus pandemic quickly became apparent. A telephone survey conducted in May 2020 showed that 70% of those surveyed felt anxious or distressed during COVID-19 community closures (IEP, 2020). The causes of distress were varied and included emotional suffering and isolation caused by COVID-19 prevention measures; the loss of a loved one; the inability to perform traditional mourning ceremonies; and the loss of work and financial resources to survive. Faced with the community's anguish, the MINSA implemented a toll-free number to provide emotional support to callers, however the response was insufficient due to high demand (MINSA, 2020a, 2020b, 2020c, 2020d).
Socios En Salud (SES) is a nonprofit organization focused on health system strengthening in Peru, rooted in social justice and a ‘preferential option for the poor’ (Farmer, Reference Farmer2013), which over the prior decade had served as a collaborating organization in support of MINSA mental health service delivery goals and priorities. For the past 25 years SES has directly supported poor communities and vulnerable populations with serious health problems. SES collaborates with the MINSA-led public sector, establishing relationships with local and national governments, and is supported by partner institutions – including leading global academic institutions – in the fight against disease, poverty, and social injustice. In October 2015, SES began focusing on mental health conditions as part of its overall programming to support poor communities, simultaneously with the passage of Law Regulation No. 29889 (modifying Article 11 of Law No. 26842) by the MINSA, which guarantees the rights of people with mental health conditions. Since that time SES has been working in coordination with the MINSA to develop community-based mental health interventions for populations affected by tuberculosis, HIV/AIDS, non-communicable diseases such as diabetes and hypertension, women in the perinatal period, caregivers of children under 3 years of age, transgender women, and people living with chronic mental disorders such as schizophrenia. The SES team uses a variety of community-based, low-intensity psychological interventions and other strategies for mental health care recommended by the MINSA and WHO, including PFA (WHO, 2012); Thinking Healthy (WHO, 2015); Problem Management Plus (WHO, 2016); and coping with grief (Alarcón et al., Reference Alarcón, Cabrera, García, Montejo, Plaza, Prieto, Rey, Robles and Vega2020). SES has developed its own internal care pathways through a program staffed by community health workers and psychologists, who support people living with both common and severe mental disorders. SES has also established protocols for referral to public institutions [health centers (HCs), community mental health centers (CMHCs), and women's emergency centers, among others] for specialized mental health care, particularly for those living with severe mental health conditions. Through these mechanisms, as well as over prior decades of collaboration in the care of people living with multi-drug-resistant tuberculosis, SES has worked with the public sector to increase the access and provision of mental health and psychosocial services available in poor communities in Peru.
To supplement MINSA's efforts to develop a robust mental health response to the coronavirus pandemic, SES leveraged its experience working in some of Lima's most underserved areas to implement a DMHI consisting of a screening tool for psychological distress, a chatbot, together with a telehealth system to provide PFA support sessions, grief therapy, and referral of cases. A newly developed digital screening tool, called ChatBot-Juntos (Chatbot-Together), was disseminated to screen the general population for psychological distress. A centralized team of psychologists then used key triage rules to identify individuals needing intervention, providing remote PFA via phone calls for individuals scoring positive for psychological distress as well as referrals for individuals needing additional care. The aim of this paper is to describe the development, implementation, and participant outcomes of this innovative system of virtual mental health screening and support in the population of Lima affected during the COVID-19 pandemic.
Methods
Study design
A retrospective cohort design was used. Data from participants were collected at two time points: during an initial screening for psychological distress using the ChatBot-Juntos screening, and 3 months after follow-up in a subset of participants who received remote PFA sessions.
Setting
The nine districts comprising the jurisdiction of DIRIS Lima Norte were the focus for intervention, with a population of around 3 million people (MINSA, 2018). Three of the nine districts have a high poverty rate, defined by insufficient resources to cover basic needs, or by a lower purchasing power that does not allow households to cover expenses. These districts include Santa Rosa (29.1% poverty rate), Puente Piedra (28.3% poverty rate), and Ancon (26.3% poverty rate). Across Lima, the average poverty rate is approximately 11% (MINSA, 2018). During the intervention period there were seven CMHCs operating in these nine districts, administered by the MINSA.
Participants
Any adult across Lima Norte or other geographic location responding to the ChatBot-Juntos screening process was included in the intervention. We initially did not consider the sample size calculation nor other inclusion/exclusion criteria in our intervention since our aim was to screen the largest number of adult people for psychological distress.
Screening (ChatBot-Juntos) and assessment process
Intervention activities were carried out between April and December 2020 (Fig. 1). Participants were screened for psychological distress using the Spanish version of the abbreviated Self-Report Questionnaire (SRQ), a 13-item version of a longer questionnaire that has shown good reliability and validity in studies conducted both in patients and in general population in many low- and middle-income countries (LMICs) (Vicente et al., Reference Vicente, Uribe, Saldivia, Escobar and Sanhueza1992; Husain et al., Reference Husain, Gater, Tomenson and Creed2006; Scholte et al., Reference Scholte, Verduin, van Lammeren, Rutayisire and Kamperman2011; Netsereab et al., Reference Netsereab, Kifle, Tesfagiorgis, Habteab, Weldeabzgi and Tesfamariam2018). The abbreviated SRQ was recommended by the MINSA's Directorate of Mental Health (in the Technical Guide for Mental Health Care in the COVID-19 context) as a screening tool appropriate for assessing distress in the context of the pandemic (MINSA, 2020a, 2020b, 2020c, 2020d).
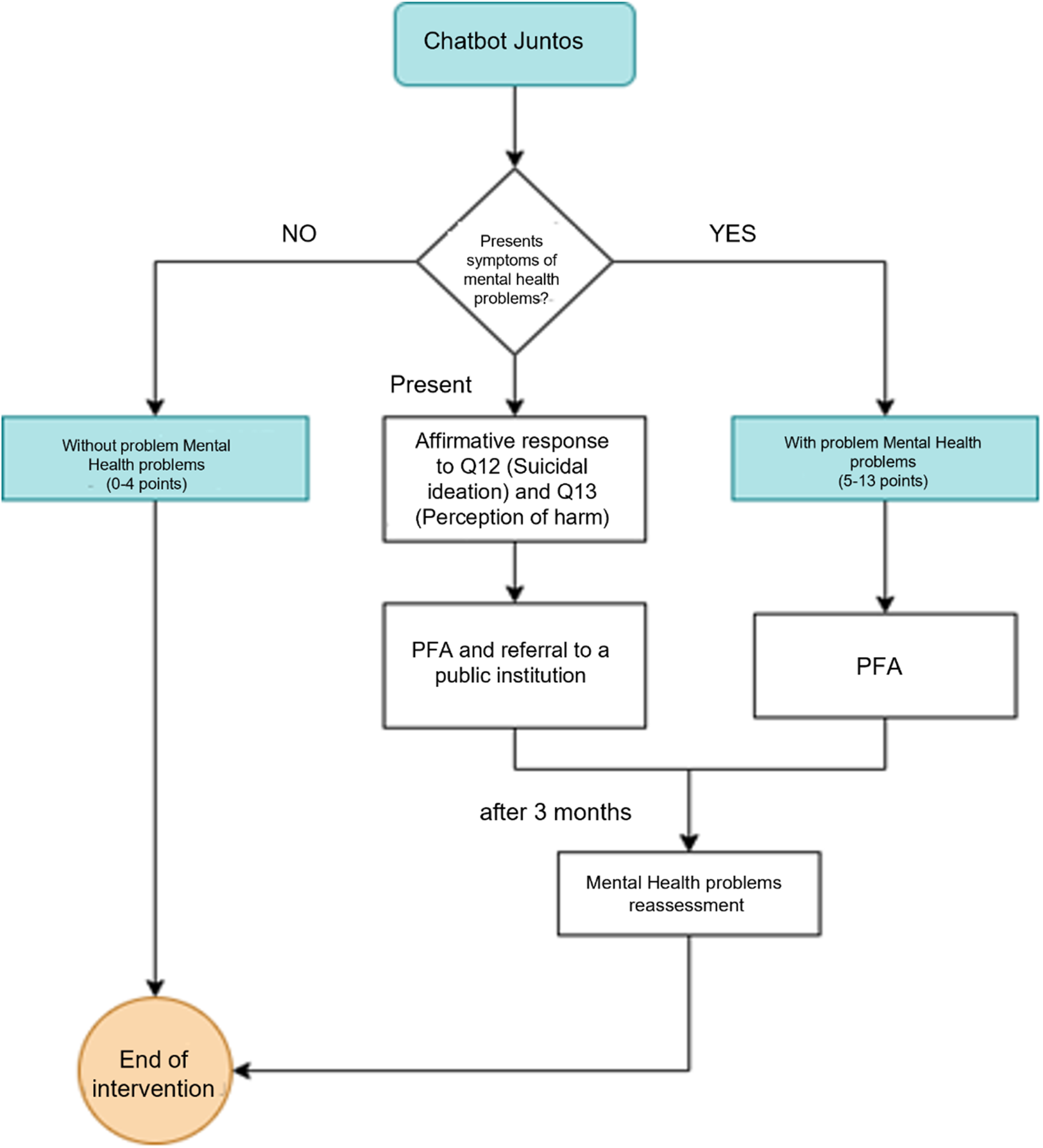
Figure 1. Virtual screening and support flowchart. Fuente: Material desarrollado por el equipo de Salud Mental de Socios En Salud (2022).
Screening was subsequently carried out through a ChatBot developed by SES. ChatBot-Juntos was developed in the ASP.Net programming language, using Microsoft SQL as the database engine. ChatBot-Juntos used an interface similar to text messages within a mobile application and a web page, and included multimedia elements such as maps, images, and sounds (see Fig. 2). ChatBot-Juntos was integrated into messaging systems on Facebook and through a WhatsApp link, for greater dissemination in the population, and to allow the user to maintain a fluid and interactive conversation within an established messaging system.
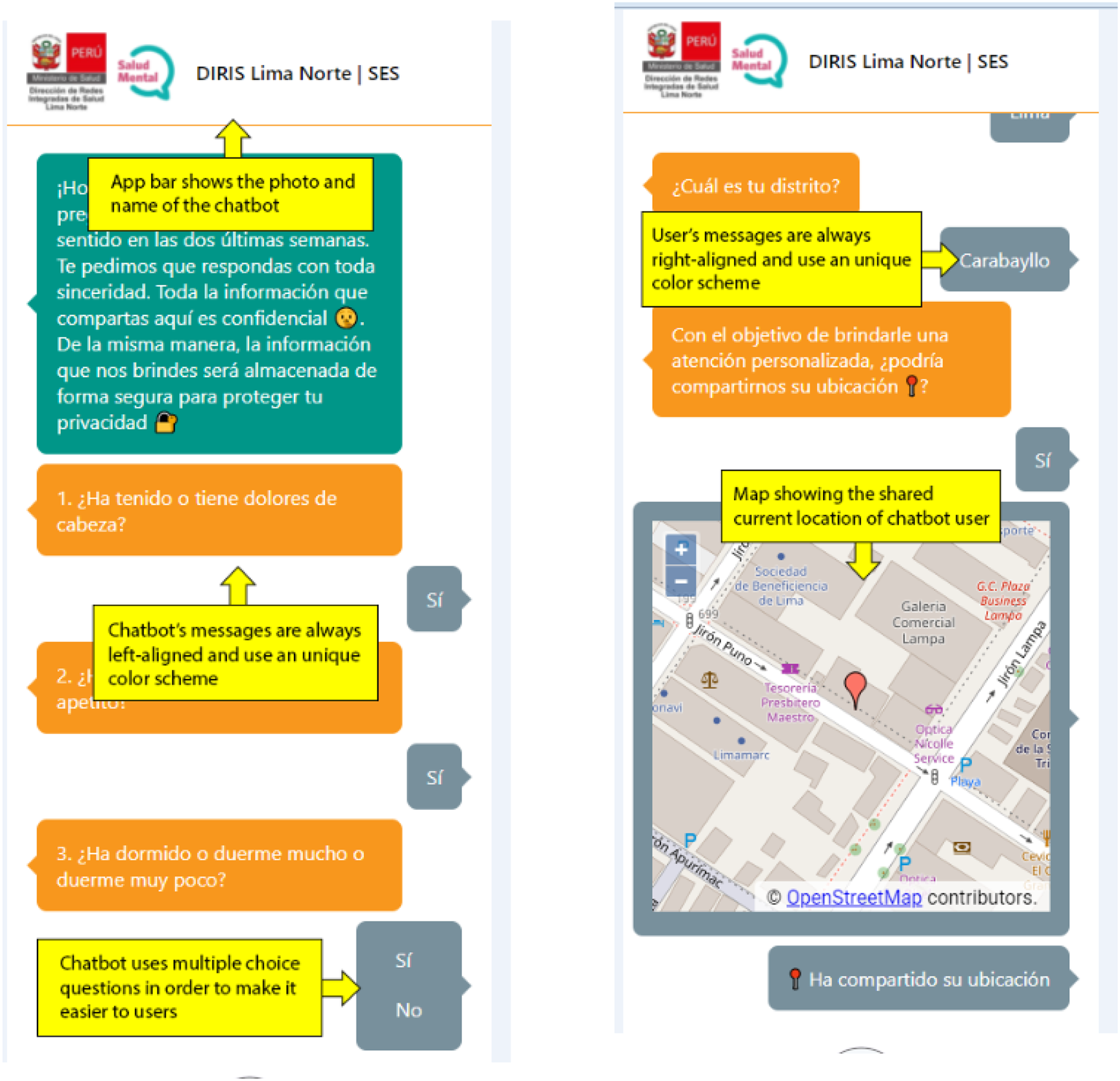
Figure 2. ChatBot-Juntos interface. Figura captado desde el Chat Bot ‘Juntos’ de Socios En Salud.
The ChatBot-Juntos screening process was accessed voluntarily by members of the general population who had found it on a hosting platform or through word of mouth. Upon opening the ChatBot-Juntos, participants were shown each item of the abbreviated SRQ sequentially. The SRQ uses a yes/no question format, and we considered a SRQ cutoff score of 5 or more as more sensitive to screen psychological distress in population-based studies as previously reported (Husain et al., Reference Husain, Gater, Tomenson and Creed2006). After each response was recorded, ChatBot-Juntos showed the participant the next question and waited for the answer before moving to the next. Sequential responses were uploaded and stored in an encrypted centralized database, using a secure data transfer protocol. Once the scale was completed, ChatBot-Juntos calculated the final abbreviated SRQ score for each participant. After completing the screening tool, ChatBot-Juntos asked all participants for their contact information in an open format that included the name, region, and residence district; how the participant had heard about ChatBot-Juntos; whether they were health workers; and cell phone number. These data were compiled in separate tables in the centralized database and linked to a unique patient ID. The de-identified data were then linked with SRQ scores in a separate encrypted file. For each participant scoring ⩾5 on ChatBot-Juntos an alert was sent to a group of psychologists hired by SES. The abbreviated SRQ also contains two questions related to suicidal ideation and thoughts of self-harm (questions 12 and 13). If a user answered yes to either of the questions, ChatBot-Juntos immediately asked the participant for contact information and sent an alert to the SES team of psychologists for urgent follow-up.
Each participant with a score ⩾5 on ChatBot-Juntos, and those with any score that included an affirmative response to question 12 and/or 13, was contacted by SES intervention psychologists. Up to three attempts were made to contact people on three different days if the intervention psychologists did not get a response on the first attempt. A standard script was created to initiate the phone conversation with ChatBot-Juntos participants. The responding psychologist introduced themselves as part of the SES team and reported their receipt of a ChatBot-Juntos score ⩾5 and/or a safety issue recorded via ChatBot-Juntos, which had precipitated the phone call, then asked for verbal consent to continue the call. If the participant indicated they believed the screen to be incorrect (e.g. denying psychological distress) or refused to continue, or if they were under 16 years of age, the psychologist recorded what happened and directed the user to seek attention at a health facility. For those who agreed to continue, the psychologist explained all calls were confidential, and connected by video or audio depending on the participants' preference.
Interventions
A total of 13 SES counseling-psychologists administered PFA for participants who agreed to participate in a brief mental health intervention. All the psychologists carried out remote activities from Lima, treated between 6–7 patients per day, and made up to three phone calls in three different days to contact people with mental disorders identified by the chatbot.
Psychological First Aid (PFA)
PFA is an initial disaster response intervention with the goal of promoting safety, restoring emotional balance, and stabilizing survivors of disasters and emergencies, and connecting people to help (WHO, 2019). The basic principle of PFA is to provide immediate support and help to a person who manifest distress due to a recent crisis, such as those that occur during the pandemic (Minihan et al., Reference Minihan, Gavin, Kelly and McNicholas2020). It can also be administered by trained non-specialists allowing to mobilize societal resources while health personnel can perform other activities (Fox et al., Reference Fox, Burkle, Bass, Pia, Epstein and Markenson2012; Minihan et al., Reference Minihan, Gavin, Kelly and McNicholas2020). In our study, the intervention consisted of a single session with a duration of approximately 45 min and were administered by study psychologists by telephone calls.
Grief counseling
During the intervention, if participants reported having lost a family member, directly or indirectly due to COVID-19, an additional introductory grief support session was held, alongside a recommendation the participant attend a specialized health facility to continue with grief therapy, if feasible and necessary.
Before disseminating of ChatBot-Juntos, psychologists working in SES and public HCs and CMHCs within Lima Norte, received 12 h of training on PFA and grief support by SES mental health team leaders and mental health experts based at SES’ US-based sister organization, Partners In Health (PIH), as part of a broader global cross-site response (Smith and Raviola, Reference Smith and Raviola2020).
Referral process
During the intervention, if the psychologist suspected or identified a mental health condition such as clinical depression or other severe mental health condition needing additional intervention, a safety concern such as suicidal ideation or plan, or domestic violence-consent was obtained for referral to specialized care in their community, such as a CMHC or other local mental health care facility. The referral process included the psychologist identifying the facility closest to the participant's home, contacting that facility, and following up with the participant to ensure that the referral was successful for in-person or virtual care. In places where there was no access to a CMHC, participants were referred to a nearby HC or hospital for acute needs. In addition, in the case of patients with suicide ideation or with self-harm who reject their referral to mental health institutions, the SES mental health team contacted their relatives to inform them of the patient's condition and the importance of the referral to a specialized institution for mental health care. They were also provided with additional information on the closest facility.
Intervention progress
As ChatBot-Juntos spread through social media platforms in Peru, the number of people accessing the screening tool continued to increase. By the end of the intervention period (June 2020) SES had extended the response hours of psychologists from 5 to 7 days per week to meet the need generated by ChatBot-Juntos, to deliver PFA and grief support to regions of Peru outside the initial target area of North Lima.
Intervention follow-up
Approximately 3 months after the initial contact, the SES psychologists contacted the intervention participants again by phone to re-administer the abbreviated SRQ. The administration of the questionnaire was by telephone for those consenting to participate. SRQ scores were established with participants in real-time during the follow-up call. For those scoring ⩾5 or with any score that included an affirmative answer to question 12 and/or 13, the psychologist repeated the intervention process once again from the beginning. SRQ results from follow-up participants were recorded on paper and later uploaded into an encrypted study database linking the score to the participant's initial ID.
Data collection
De-identified participant data were collected from the chatbot's centralized database and uploaded for analysis into the SES computer system (SEIS) by the intervention psychologists. Collected variables included sociodemographic variables (sex, age, health worker status, and location); the mechanism for learning about ChatBot-Juntos; initial SRQ score; the intervention strategy employed (PFA or PFA plus grief support); whether participants were referred to primary care or specialized mental health facilities within the health system; and SRQ score at 3 months post-intervention for those who agreed to participate in the follow-up call.
Data analysis
Initial screening SRQ scores collected via ChatBot-Juntos and 3-month follow-up SRQ scores collected via telephone were analyzed. Demographic data described included gender, age, location, how participants found ChatBot-Juntos, and health worker status. Numbers and percentages are reported for categorical variables, and medians and interquartile range (IQR) are reported for continuous variables. Differences between screening and follow-up SRQ scores (only for those who completed the post-intervention assessment) were compared using the Wilcoxon's signed-rank test with a 5% significance level. Data were analyzed using Stata v.15.
Results
Although intended for distribution within North Lima, ChatBot-Juntos reached a wide geographic distribution in Peru, including urban and rural areas, given its dissemination through social networks. ChatBot-Juntos participants were in 21 regions of Peru (Fig. 3). Four hundred fifty-three people (45%) found ChatBot-Juntos directly through social networks (Facebook and WhatsApp messages), 527 people (53%) reported that they initially found out about ChatBot-Juntos in the community (health brigades, family, friends, community spaces, and others), and 17 people (2%) did not specify (Table 1).

Figure 3. Reach of the chatbot in the 21 regions of the country. Fuente: Material desarrollado por el equipo de comunicaciones de Socios En Salud (2022).
Table 1. Where did you get the chatbot information (n = 997)
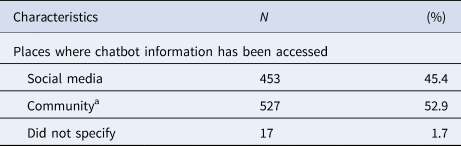
a Health brigades, family, friends, community spaces.
A total of 2027 people completed the ChatBot-Juntos screening process over the course of 6 months, of whom 1581 (78.0%) screened positive (score ⩾ 5) for psychological distress on the SRQ. Nine hundred ninety-seven (63%) agreed to receive psychological support during their initial contact with a psychologist. A complete participant flow diagram is shown in Fig. 4. Demographics of those individuals receiving support are described in Table 2. Nine hundred sixty of the 997 (96.3%) received PFA alone and 37 (3.7%) received PFA and grief support. In addition, 320 people (32.1%) were referred to additional mental health services due to the identification or suspicion of major depression, another chronic mental health condition, a safety problem such as suicidal ideation or plan, or violence in the home. Specific reasons for referral to specialized mental health services are outlined in Table 3. The health facilities they were referred to were CMHCs (n = 260, 81.3%), HCs (n = 40, 12.5%), and other specialized care centers in mental health (n = 20, 6.3%).
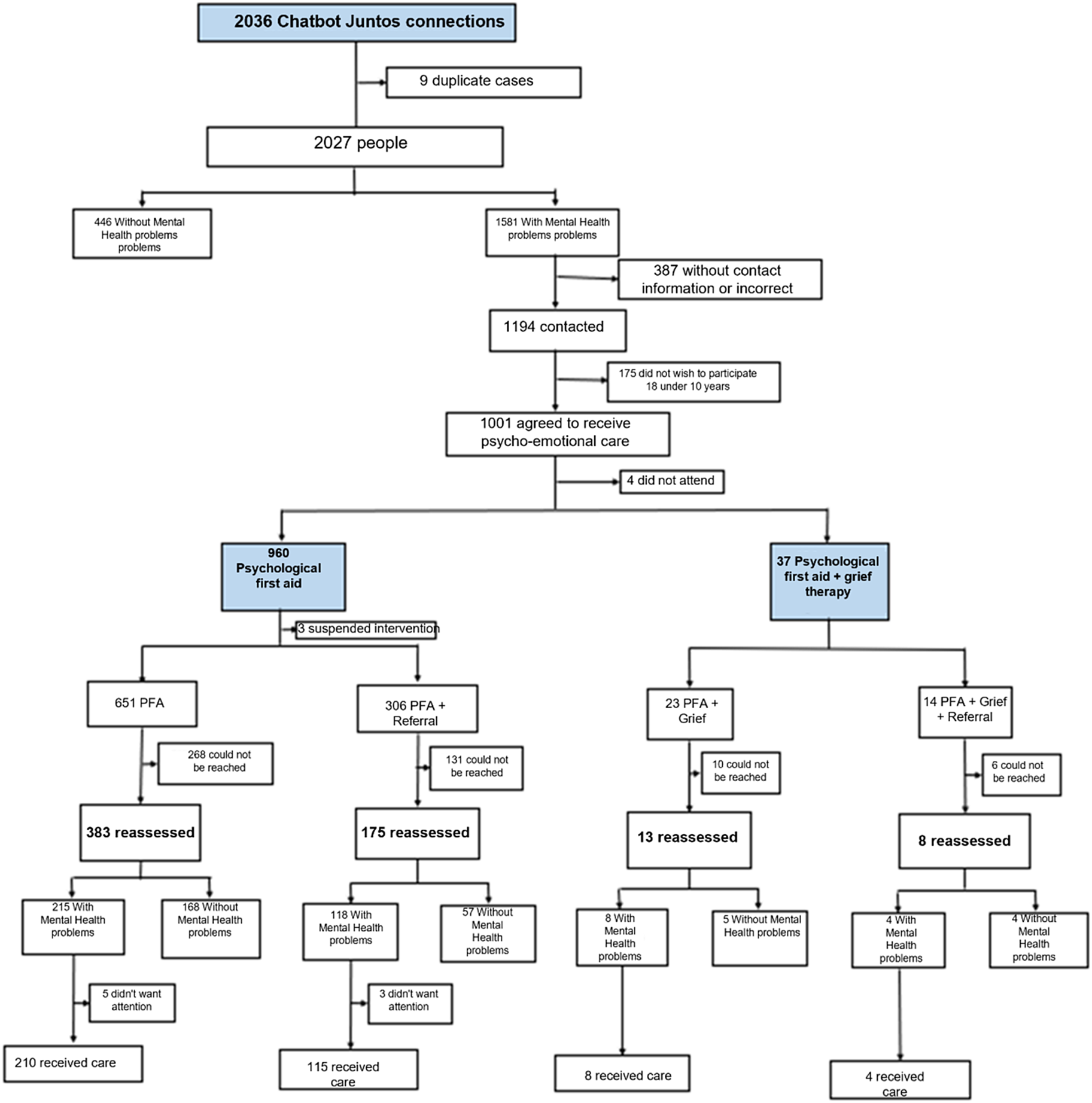
Figure 4. Care pathway for people who made a connection to ChatBot-Juntos (N = 2036 people). Fuente: Material desarrollado por el equipo de Salud Mental de Socios En Salud (2022).
Table 2. Characteristics of the participants who responded to the chatbot and received emotional support (n = 997)
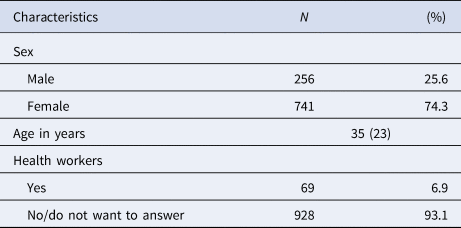
Table 3. Reasons for referral (n = 320)

The 997 initial chatbot participants were contacted 3 months after initial evaluation. Five hundred seventy-nine (58%) agreed to be re-evaluated. Four hundred eighteen (42%) were not re-evaluated, due to an inability to contact the participant (247), incorrect/non-functioning cell phone (106), or because they declined to participate in the re-evaluation (65). For those who were re-evaluated, significant improvements in SRQ score at 3 months post-intervention were seen in those participating in both PFA alone, with median SRQ score improving from 9 to 5 (p < 0.001), and in PFA and referral to mental health services, respectively, with median SRQ score improving from 11 to 6 (p < 0.001) (Table 4). The same trend was observed among participants who received both PFA and grief support (n = 13), with median SRQ score improving from 11 to 5, and in those who received PFA, grief support and additional referral to mental health services (n = 8), with median SRQ score improving from 12 v. 4, although the sample size was too small to achieve statistical significance. Although participants exhibited significant improvements in SRQ scores at 3-month follow-up, most of this group continued to report some degree of psychological distress, with 345 participants (59.6%) scoring ⩾5 on the SRQ at follow-up.
Table 4. Comparison of chatbot mental health scores before and after intervention
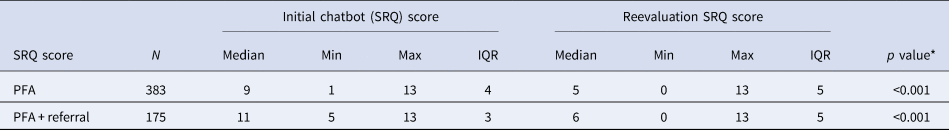
*Wilcoxon signed-rank test.
Discussion
In Peru and globally, COVID-19 and its social and economic consequences negatively affected the mental health of populations and created new barriers to accessing mental health care (MINSA, 2020a, 2020b, 2020c, 2020d). To support the Peruvian government's goal of reaching people in need during the pandemic, and to increase access to mental health services, SES developed a program to provide remote emotional support and referral to mental health care, making use of an innovative digital screening tool for psychological distress (ChatBot-Juntos) which leveraged chatbot technology and social media platforms to reach the general population.
The primary purpose of using ChatBot-Juntos was to offer support to an underserved urban population during the pandemic and more effectively link people in need of mental health care with available resources. Although our initial messaging around ChatBot-Juntos focused on the North Lima community, the reach of ChatBot-Juntos to 21 regions demonstrate the scope and rapid dissemination of this virtual tool through social networks and offers proof of concept that digital innovations can be used to detect mental health problems in the Peruvian population. It is interesting to note although internet users have increased in Peru during the pandemic (INEI, 2019, 2020), almost half of the population accessing ChatBot-Juntos initially found out about the tool in the community and not through social media platforms, suggesting that social media does not reach the entire population and access to technology may still be limited – an important consideration in the use of population-based approaches to mental health screening and referral using digital technology.
In the context of the social distancing measures put into place by the Peruvian government, the brief interventions employed by the team of psychologists also used digital technology for delivery. There are many benefits associated with this delivery mechanism, such as reaching a greater geographic region, reducing costs, and providing users with a safe, controlled, and confidential context (López-Santín and Álvaro, Reference López-Santín and Álvaro Serón2018). There is also growing evidence that remote mental health care and support could potentially contribute to decreasing the mental health care treatment gap; for example, Plata et al. (Reference Plata, López, Baca and Gómez2014) demonstrated remote treatment was feasible and beneficial for people who could not access a traditional psychological service.
A high proportion (78%) of people who accessed ChatBot-Juntos screened positive for psychological distress. Although this high proportion may indicate people who chose to access ChatBot-Juntos were more likely to be experiencing mental distress, it could also be an indication of the high levels of psychological distress in the population during the COVID-19 pandemic. Due to persistent anxiety and panic, fear of contracting COVID-19 and infecting others, fear of losing loved ones, fear of being left without a job or economic support (PAHO, 2019), and other persistent stressors, the incidence of mental health conditions during the pandemic may be increased, aligned with our finding that almost 35% of participants were deemed in need of referral to health facilities for more specialized mental health care. In these circumstances, early interventions such as PFA and referral may have prevented worsening of individuals' distress and mental health conditions, especially as there were significant improvements in SRQ scores for all surveyed individuals participating in the brief interventions offered by SES, as well as for those who were also referred to mental health care.
An unexpected finding in our study was the presence of lower SRQ scores was reported in health workers compared to the rest of the population [median score: 9 (range: 5–13) and median score: 10 (range: 1–13), not reported in the results]. These findings are contradictory to the hypothesis that health workers could have been at higher risk of distress during the pandemic and seems to be affected by the lack of representativity and disproportionality in the numbers of patients in both groups (69 health workers v. 928 non-health workers).
Most of those participating in the offered psychological interventions were women, similar to the proportion of women accessing the emotional support line provided by the MINSA throughout the coronavirus pandemic. It is known that psychological distress is more common in female than male, and this difference may be explained in part by the additional family and home burden that women carry, mainly in low-resource settings where gender inequity exists, and stressful conditions increased considerable during COVID pandemic (Hossain, Reference Hossain2021; Herrera-Añazco et al., Reference Herrera-Añazco, Urrunaga-Pastor, Benites-Zapata, Bendezu-Quispe, Toro-Huamanchumo and Hernandez2022). Additionally, women are more likely to report psychological distress and deterioration of well-being compared to men (Borrescio-Higa and Valenzuela, Reference Borrescio-Higa and Valenzuela2021). The higher proportion of women accessing remote support may reflect better access to virtual platforms during the day and in the context of the pandemic, or that women are the primary seekers of mental health support for themselves and their families. The lower proportion of men seeking services relative to women may also reflect the cultural context in Peru where men may deny or delay a need for physical or emotional help (Gómez, Reference Gómez2002).
PFA is considered a first-line intervention for mental health in emergencies (IASC, 2020) and can be delivered by people without formal professional training, although there is limited research evidence for its efficacy (Fox et al., Reference Fox, Burkle, Bass, Pia, Epstein and Markenson2012; Shultz and Forbes, Reference Shultz and Forbes2014). PFA was a centerpiece of the PIH response across all global sites (Smith and Raviola, Reference Smith and Raviola2020). The results of our follow-up SRQ assessments provide some real-world evidence that PFA may be effective in reducing distress, as SRQ scores were reduced significantly after 3 months for those participating in PFA. However, despite these improvements, almost 60% of individuals continued to score positive for psychological distress after 3 months, regardless of intervention. This number may be even higher given that follow-up scores were only obtained for 58% of participants. In the context of the prolonged COVID-19 pandemic, high distress levels indicate the critical need for continued emotional support, particularly for the most vulnerable populations including people living in poverty, older adults, people with comorbid health conditions, people living with disabilities, and other risk factors for prolonged psychological distress.
Our study has several limitations to be considered. First, the social networks used to share ChatBot-Juntos limited the intervention population only to those who had access to internet services, a smartphone, and basic computer skills, excluding sectors of the community that do not have these services and who might be even more vulnerable to emotional distress during the pandemic, therefore affecting the representativeness of the population. In addition, the lack of sample size calculation, and the lack of randomness in the sampling of participants (due to being a community intervention) could also have increased the selection bias of participants. Second, our use of the abbreviated SRQ scale with dichotomous scoring determining whether individuals received a psychological intervention may have missed some people with mental health conditions who may have benefitted from more individualized support or referral. The limited information about participating individuals obtained from ChatBot-Juntos did not allow for a more detailed analysis of sub-populations who did or did not benefit from remote mental health care and support such as PFA. An additional limitation is that follow-up SRQ scores were obtained only from 58% of participants, and the missing follow-up data may bias our results. It is also possible that the method of re-assessment (phone call v. screening chatbot) may have influenced the high percentage of participants not re-evaluated, most of which could not be contacted. Possible reasons include theft/loss of their phones or cancellation of phone services, although we cannot rule out the possibility that some patients did not want to answer the phone call for re-assessment. Also, the lack of a control group and randomization in our study limits our ability to demonstrate the efficacy of our intervention in reducing the burden of psychological distress since follow-up patients' scores may also decrease naturally over time. Therefore, future controlled trials are needed to determine the efficacy of our DMHI. Although the intervention protocol included referral to formal mental health services for those with a possible or probable mental health condition, those institutions often had difficulty in providing timely care for referred individuals, highlighting the need for ongoing mental health system development alongside digital innovations promoting access to mental health care. Finally, for implementing an effective mental health program in low- and middle-income settings is necessary to maintain high coverage of screening and intervention in the population, which mean to increase the number of psychologists and extend consultation hours. To reduce the burden for psychologists, community health workers and/or school psychologists should be trained and supervised in administering psychological support to improve the dissemination and cost-effectiveness of the intervention (Mistry et al., Reference Mistry, Harris-Roxas, Yadav, Shabnam, Rawal and Harris2021).
Conclusion
This study shows the feasibility of using digital technology to bring mental health services closer to affected populations in the context of the COVID-19 pandemic, allowing rapid screening and identification of people who need support, providing basic psychological support such as PFA to individuals, and effectively linking them to additional mental health care if necessary. More research is needed to determine whether virtual screening tools, such as chatbots alongside remote interventions providing basic psychological support and referral, can reduce the burden of illness attributable to mental health conditions in places of limited resources for mental health.
Acknowledgements
Gratitude is expressed to the population of the districts of Lima and provinces throughout the national territory amid the COVID-19 pandemic; and Mental Health Directorate from MINSA and Integrated Networks of North Lima for their support in carrying out this study.
Financial support
Public health response activities were funded by the United States Agency for International Development and Partners in Health, grant number 72052720FA00003.
Conflict of interest
None.
Ethical standards
The Ethics Committee of the Universidad Peruana Cayetano Heredia, with registration code 20004, approved an exemption for the review of a secondary database without access to confidential information. The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.













