Introduction
Approximately 9% of the global population is aged 65 or over in 2019, predicted to increase to 16% by 2050 (Qiu et al., Reference Qiu, Li, Wang, Zheng, Wang, Wang and Chen2022). As the population ageing, age-associated diseases and disabilities worldwide become an important public health issue, which imposes heavy economic burden on society and families (Pérez Palmer et al., Reference Pérez Palmer, Trejo Ortega and Joshi2022; Su et al., Reference Su, Shang, Xu, Li, Chen, Zhang, Zhang and Hua2014). Cognitive impairment has tended to worsen to a great extent in recent years. The estimated prevalence of cognitive impairment is 10%–15% among population over 65 years and reaches 25% in those aged 80–84 (Anderson, Reference Anderson2019; Pérez Palmer et al., Reference Pérez Palmer, Trejo Ortega and Joshi2022). Population aged 80 years and over comprises the fastest-growing segment of Chinese population. The prevalence of cognitive impairment ranges between 6% and 16% among Chinese people aged 60 years and over (Jia et al., Reference Jia, Du, Chu, Zhang, Li, Lyu, Li, Li, Zhu, Jiao, Song, Shi, Zhang, Gong, Wei, Tang, Fang, Guo, Wang, Zhou, Chu, Zuo, Yu, Yuan, Wang, Li, Shi, Yang, Zhou, Liao, Lv, Li, Kan, Zhao, Wang, Yang, Li, Liu, Wang, Qin and Jia2020) and reaches around 48% in people aged more than 80 years old (An and Liu, Reference An and Liu2016). Primary health care plays a vital role in cognitive impairment (Mullins et al., Reference Mullins, Bynum, Judd and Clarke2021). Nevertheless, current primary health care faces serious challenge in preventing and managing cognitive impairment in the elderly population (Belmin et al., Reference Belmin, Min, Roth, Reuben and Wenger2012; Lu et al., Reference Lu, Liu, Wells and Yu2022).
Due to lack of family companionship, cognitive function of nursing home residents is more worthy of attention. Notably, the prevalence of CI in the older nursing home residents is higher than the community elderly (Wu et al., Reference Wu, Ke and Su1998; Miranda et al., Reference Miranda, Smets, Van Den Noortgate, Deliens and Van den Block2021; Yuan et al., Reference Yuan, Lapane, Tjia, Baek, Liu and Ulbricht2021; Qiu et al., Reference Qiu, Li, Wang, Zheng, Wang, Wang and Chen2022). Previous studies report age, married status, male, diabetes, low income, low education, unfavourable cardiovascular health and carrying apolipoprotein E (APOE) e4 allele were risk factors of cognitive impairment (Peloso et al., Reference Peloso, Beiser, Satizabal, Xanthakis, Vasan, Pase, Destefano and Seshadri2020; Frison et al., Reference Frison, Proust-Lima, Mangin, Habert, Bombois, Ousset, Pasquier, Hanon, Paquet, Gabelle, Ceccaldi, Annweiler, Krolak-Salmon, Béjot, Belin, Wallon, Sauvee, Beaufils, Bourdel-Marchasson, Jalenques, Chupin, Chêne and Dufouil2021; Najar et al., Reference Najar, Aakre, Vassilaki, Wetterberg, Rydén, Zettergren, Skoog, Jack, Knopman, Petersen, Kern and Mielke2021). Cognitive impairment is always accompanied by declines in health-related quality of life (HRQOL), disability, death and cardiopulmonary dysfunction. About 18% of CI patients experience respiratory dysfunction (Martinez et al., Reference Martinez, Richardson, Han and Cigolle2014), and 43% of cognitive decline patients have heart failure (HF) (Cannon et al., Reference Cannon, Moffitt, Perez-Moreno, Walters, Broomfield, McMurray and Quinn2017). Accumulating evidence from different countries not only indicates abnormal cardiopulmonary function increased the risk of cognitive impairment (Emery et al., Reference Emery, Finkel and Pedersen2012; Cermakova et al., Reference Cermakova, Eriksdotter, Lund, Winblad, Religa and Religa2015; Jefferson et al., Reference Jefferson, Beiser, Himali, Seshadri, O’Donnell, Manning, Wolf, Au and Benjamin2015; Zhang et al., Reference Zhang, Gao, Han, Xiang and Liu2020; Duong et al., Reference Duong, Usman, Ma, Xie, Huang, Zaman, Dragoman, Jiatong Chen, Farooqi and Raina2022) but also reveals the complex interactions between cognitive impairment and HRQOL (Ezzati et al., Reference Ezzati, Zammit, Katz, Derby, Zimmerman and Lipton2019; Liu et al., Reference Liu, Tsai, Chiu, Tang, Lee, Shyu and Wang2019; Phyo et al., Reference Phyo, Gonzalez-Chica, Stocks, Storey, Woods, Murray, Orchard, Shah, Gasevic, Freak-Poli and Ryan2021). Currently, the mechanisms of abnormal cardiac function and cognitive impairment mainly involve cerebral hypoperfusion, hypoxia, systemic inflammation, endothelial injury and neurohormonal activation (Cermakova et al., Reference Cermakova, Eriksdotter, Lund, Winblad, Religa and Religa2015; Diener et al., Reference Diener, Hart, Koudstaal, Lane and Lip2019) and of abnormal pulmonary function and cognitive impairment mainly involved hypoxia, systemic inflammation and cerebral vascular dysfunction (Wang et al., Reference Wang, Mao, Wang, Li, Liu and Wu2020). Related studies mainly focus on community populations under the age of 80. The cognitive function of order nursing home residents received less attention. However, the association between abnormal cardiopulmonary function, HRQOL and cognitive impairment remains to be clarified in the nursing home residents aged over 80 years old.
In this study, we aimed to assess the association between cognitive impairment and HRQOL and cardiopulmonary function, so as to explore the notable indicators of cognitive impairment, therapy providing evidence for the prevention and control of cardiovascular-related cognitive dysfunction and reduction of the disease burden of cognitive impairment.
Methods
Study participants
Strategy of participants’ selection using a multi-stage stratified cluster sampling method in this study is shown in Supplementary material 1. Briefly, a randomized district in the urban and suburban areas of Shanghai from 2016 to 2017 was selected, respectively, and then randomly selected four nursing homes from each district, and a total of 677 participants who met the criterion were recruited in the study.
Participants enrolled in the study met the following conditions: (1) participants were at least 80 years old; (2) locally residents lived in nursing homes in Shanghai; (3) had normal hearing, vision and speech.
Exclusion criteria included (1) absence of cognitive function or in a vegetative state; (2) diagnoses of schizophrenia or serious mental retardation; (3) suffered a traumatic brain injury; and (4) inability to cooperate with the following inspections or assessment.
Each participant received physical and chemical inspection, face-to-face interview and cognitive assessment.
For effective assessment in cardiopulmonary function and HRQOL, the additional exclusion criteria were formulated: (1) unable to follow the precautions for cardiopulmonary function tests as directed by the researchers; (2) patients who could not complete the questions about daily activities in HRQOL test. Finally, a total of 197 participants who met the criteria were included in the analysis.
Cognitive assessment
Chinese version of the Mini-Mental State Examination (MMSE) was used to evaluate cognitive function because of the high proportion of low-educated subjects in this study (Wu et al., Reference Wu, Zhang, Yuan, Guo and Gao2021). The MMSE is a 30-point questionnaire assessing five areas of cognitive function including orientation, registration, language and praxis, attention and calculation, and recall, and education attainments were adjusted when calculating the raw total score. Cognitive impairment was classified if MMSE ≤ 17 for illiterates; MMSE ≤ 20 for elementary school graduates; MMSE ≤ 24 for junior school graduates or above (Li et al., Reference Li, Jia and Yang2016). Cronbach’s alpha value of the MMSE scale was tested to examine the reliability of the MMSE questionnaire, and the result was 0.899, indicating that it can be utilized to assess cognitive impairment of subjects in this study.
Assessment of HRQOL
Chinese version of the Short Form-36 scales (SF-36) was used to measure HRQOL of participants, which not only has a better split-half reliability (r = 0.91, P < 0.001) (Zhou et al., 2018) but also is a valid and reliable tool for assessing HRQOL among Chinese population (Wang et al., Reference Wang, Wu, Zhao, Yan, Ma, Wu, Liu, Gu, Zhao and He2008). SF-36 includes eight scales, evaluating the following areas: physical functioning (PF), role limitations due to physical health (RP), body pain (BP), general health (GH), vitality (VT), social functioning (SF), role limitations due to emotional problems (RE) and mental health (MH). Cronbach’s alpha value of Chinese version SF-36 scale was 0.821 in this study, suggesting good internal consistency of the scale.
Assessment of heart function
Heart function was measured by trained technicians via the Vscan V1.2 (GE Healthcare, Milwaukee, WI, USA). The sensitivity and specificity of palm ultrasound to detect left ventricular dilatation range from 71% to 94% and 97% to 100%, respectively (Liebo et al., Reference Liebo, Israel, Lillie, Smith, Rubenson and Topol2011). According to the American Society of Echocardiography (ASE) (Lang et al., Reference Lang, Bierig, Devereux, Flachskampf, Foster, Pellikka, Picard, Roman, Seward, Shanewise, Solomon, Spencer, Sutton and Stewart2005), heart rate, systolic blood pressure (SBP), diastolic blood pressure (DBP), pulse pressure (PP), end-diastolic dimension of left ventricle (LVD), end-systolic dimension of left ventricle (LVS), the thickness of the basal interventricular septum (IVS), left ventricular posterior wall (LVPW), LVEF and calculated left ventricle fractional shortening (LVFS) were determined. The measured values were divided into normal and abnormal groups according to the standard (Supplementary material 2) (Yancy et al., Reference Yancy, Jessup, Bozkurt, Butler, Casey, Colvin, Drazner, Filippatos, Fonarow, Givertz, Hollenberg, Lindenfeld, Masoudi, McBride, Peterson, Stevenson and Westlake2017).
Assessment of respiratory function
Respiratory function was measured using CHESTHI-101 (COSMED S.r.l. Japan). Vital capacity (VC) is the amount of air that people can try to exhale after maximal inspiration. Maximal ventilatory volume (MVV) was collected to measure elasticity of thoracic lung tissue, airway resistance and respiratory muscle strength. However, forced expiratory volume in 1 s, which is a commonly used indicator to determine asthma and chronic obstructive pulmonary disease, was not collected because it is difficult for ultra-aged people to exhale in a second.
Other baseline measurements
Sociodemographic information and health-related data were collected for all participants by using an interviewer-administered questionnaire, including age, gender, education, marital status, smoking status, body mass index (BMI, weight, in kilograms/height2, in metres), physical activity, disease histories and medication histories. Education attainment was divided into 3 groups: illiteracy, elementary school (<6 years of education) and junior school or above (≥6 years of education). Marital status included unmarried, married, widowed and divorced, and we further defined it as a dichotomous variable (with and without partners). Physical activity was defined as standing, walking and outdoor time of participants (≤1 h/>1 h). Information of disease history including previous hypertension, diabetes, dyslipidemia, coronary heart disease, stroke and tumour were collected by self-reported physican's diagnosis or medical records. Medication histories were recorded as antihypertensive, antidiabetic, anticoagulation and lipid-lowering drugs usage.
Quality control
Experienced professionals were invited to review and give amendments to the survey questionnaires, and their professional guidance was required. Standardized protocols and statistical methods were used, and all investigators (doctors and research technicians) underwent joint training sessions before implementation of the study.
The quality control of echocardiographic data collection followed the ‘Echocardiography laboratory standards and accreditation guidelines for adults’ recommended by ASE (Restrepo et al., Reference Restrepo, Gutiérrez Fajardo, Lowenstein, Paz-Ardaya, Vieira, Spina, Córdova-Alvéstegui, Beltrán, Pizzano and Revilla-Alcocer2011), and the quality control of pulmonary function examination data collection followed the ‘Pulmonary Function Examination Guidelines’ recommended by the Chinese Medical Association.
Statistical analysis
EpiData3.1 (Odense, Denmark) was used for double data input. SPSS20.0 (SPSS Inc., Chicago, IL, USA) was used for data management and analysis. Continuous variables were presented as means [95% confidence intervals (95%CI)]. Cronbach’s alpha value was calculated to assess internal reliability of MMSE and SF-36 scales. Crude differences in the proportions according to cognitive state were analysed by chi-square test. Two independent samples t test and the Mann-Whitney test were performed for the comparison of two independent samples. Multivariate logistic regression analysis was performed to evaluate the association between cardiopulmonary function, health-related quality of life and cognitive impairment adjusted for potential confounders. Adjusted odds ratio (AOR) and their 95%CI were reported. Variance inflation factor (VIF) was used to detect multicollinearity of variables in the model, and VIF > 10 was diagnosed as multicollinearity (Athavale et al., Reference Athavale, Kumar, Clark, Mondal and Sur2021). Two-sided P-value <0.05 was considered statistically significant.
Results
Population analysis
The baseline information of 677 participants is shown in Supplementary material 3. The prevalence of cognitive impairment was 30.7% among 677 nursing home-based older population aged 80 years and over. The average age was 84.99 years (95%CI, 84.61–85.38 years). Compared to subjects with normal cognition, patients with cognitive impairment were more likely to be older, women, non-partnered, less physical activity, no history of smoking, lower BMI, no history of hypertension, dyslipidemia and coronary heart disease history (All P < 0.05).
One hundred and ninety-seven subjects who have effective assessment in cardiopulmonary function and HRQOL were included in the present investigation, the average age was 86.1 years (95%CI, 85.6–86.7 years), and 75% were women, average BMI was 23.91 kg/m2 (95%CI, 23.35–24.47 kg/m2). About 32.5% of the subjects were diagnosed as cognitive impairment. Demographic characteristics stratified by cognitive status are presented in Table 1. Compared to subjects with normal cognition, patients with cognitive impairment were more likely to be older, women, non-partnered, less physical activity, lower BMI, hypertensive history and no history of antihypertensive drugs (All P < 0.05).
Table 1. Demographic and health characteristics of the older nursing home residents in Shanghai, China (N = 197)

Continuous parameters were presented as means (95% confidence intervals). Categorical variables were presented as number of participants (column percentage). BMI = body mass index; BP = body pain; DBP = diastolic blood pressure; GH = general health; IVS = the thickness of the basal interventricular septum; LVD = end-diastolic dimension of left ventricle; LVEF = left ventricular ejection fractions; LVFS = left ventricle fractional shortening; LVPW = left ventricular posterior wall; LVS = end-systolic dimension of left ventricle; MH = mental health; MMSE = Mini-Mental State Examination; MVV = maximal ventilatory volume; PF = physical functioning; RE = role limitations due to emotional problems; RP = role limitations due to physical health; SBP = systolic blood pressure; SF = social functioning; SF-36 = short form-36 scales; VC = vital capacity; VT = vitality.
Abnormal LVEF, VC and MVV detected in patients with cognitive impairment were 42.2%, 79.7% and 98.4%, respectively. When comparing to subjects with normal cognitive function, subjects with cognitive impairment showed significantly crude decline in LVEF, LVFS, VC, MVV, PF and VT (All P < 0.05) (Table 1).
Sub-Domain analysis of cognitive function
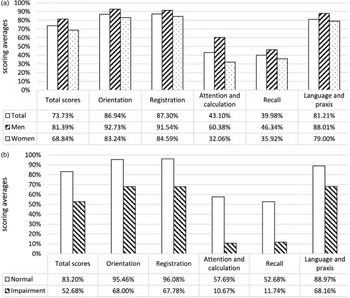
The transformed MMSE scores of domains stratified by gender and the classification of cognitive function were displayed (Figure 1 ). In the older Chinese nursing home residents, MMSE scores were clearly the lowest in attention and calculation (43.1%) and recall (40.0%). Men had higher scores in all MMSE dimensions than women. Besides, participants classified as cognitive impairment performed worse than those with normal cognition in all domains, and cognitive scores of the two groups differed most in attention and calculation (57.7% vs. 10.7%) and recall (52.7% vs. 11.7%).

Figure 1. Transformed MMSE scores of five domains stratified by gender and cognitive function.
The logistic regression model adjusted age and gender. The logistic regression model adjusted age and gender, marital status, physical activity and BMI. HRQOL: health-related quality of life; LVEF: left ventricular ejection fraction; LVFS: left ventricle fractional shortening; VC: vital capacity; MVV: maximal ventilator volume; PF: physical functioning; VT: vitality; BMI: body mass index; AOR, adjusted odds ratio. MMSE: Mini-Mental State Examination.
Cardiopulmonary dysfunction, HRQOL and cognitive impairment
The variables of P < 0.05 in the Table 1 were integrated into the multivariable logistic regression model. Multicollinearity analysis did not detect severe collinearity among these variables in the model (Supplementary material 4). Abnormal LVEF (AOR, 1.983; 95%CI, 1.034–3.805) and VC (AOR, 2.079; 95%CI, 1.069–4.041) were significantly associated with cognitive impairment after adjusting confounders including age and gender, while history of antihypertensive drugs (AOR, 0.397; 95%CI, 0.208–0.759) and higher PF (AOR, 0.982; 95%CI, 0.970–0.994) was associated with the decrease in cognitive impairment risk and this association still existed after adjusting age and gender, marital status, physical activity, and BMI (Table 2).
Table 2. Estimating the risk of cognitive impairment associated with factors of interest among the older nursing home residents in Shanghai, China (N = 197)

Model 1 adjusted age and gender. Model 2 adjusted age, gender, marital status, physical activity and BMI. AOR = adjusted odds ratio; BMI = body mass index; CI = confidence intervals; LVEF = left ventricular ejection fraction; LVFS = left ventricle fractional shortening; MVV = maximal ventilatory volume; PF = physical functioning; VC = vital capacity; VT = vitality.
Analysis of five domains of cognitive function
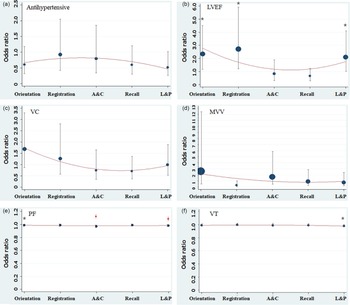
After adjusting age and gender, marital status, physical activity and BMI, decreasing in LVEF was related to the abnormal orientation (AOR, 2.337; 95%CI, 1.204–4.538), registration (AOR, 2.707; 95%CI, 1.237–5.924) and language and praxis (AOR, 2.085; 95%CI, 1.055–4.119). Besides, PF (AOR, 0.982; 95%CI, 0.970–0.995) and VT (AOR, 0.978; 95%CI, 0.961–0.995) were protective factors of language and praxis. Moreover, PF was associated with better attention and calculation (AOR, 0.970; 95%CI, 0.953–0.987) (Figure 2).

Figure 2. The association of cardiopulmonary function, HRQOL and five domains of cognitive function.
The logistic regression model adjusted age and gender, marital status, physical activity and BMI. HRQOL: health-related quality of life; LVEF: left ventricular ejection fraction; LVFS: left ventricle fractional shortening; VC: vital capacity; MVV: maximal ventilator volume; PF: physical functioning; VT: vitality; BMI: body mass index. A&C: attention and calculation; L&P: language and praxis. *P < 0.05, ![]() P < 0.01. Size of the point represents the weight.
P < 0.01. Size of the point represents the weight.
Discussion
As one of the major public health concerns, cognitive impairment is not only highly prevalent, but has a negative impact on HRQOL, thus imposing a substantial socioeconomic burden (Sanford, Reference Sanford2017). Besides those confirmed risk factors including age, gender, marital status, personal income, physical activity, BMI and history of stroke, impaired cardiopulmonary function had already been identified as medical co-morbidity with cognitive impairment (Jia et al., Reference Jia, Du, Chu, Zhang, Li, Lyu, Li, Li, Zhu, Jiao, Song, Shi, Zhang, Gong, Wei, Tang, Fang, Guo, Wang, Zhou, Chu, Zuo, Yu, Yuan, Wang, Li, Shi, Yang, Zhou, Liao, Lv, Li, Kan, Zhao, Wang, Yang, Li, Liu, Wang, Qin and Jia2020; Duong et al., Reference Duong, Usman, Ma, Xie, Huang, Zaman, Dragoman, Jiatong Chen, Farooqi and Raina2022; Huang et al., Reference Huang, Chen, Leng, Kuo, Wang, Cui, Tan, Wang, Dong and Yu2022). Thus, ascertain relationships between HRQOL score, cardiopulmonary function and cognitive performance are fundamental for providing evidence for the prevention and control of cognitive decline-associated disease burden.
In this study, we found that 30.7% of the older nursing home residents aged over 80 years in Shanghai were classified as cognitive impairment, which was higher than the community elderly aged over 80 years (Lv et al., Reference Lv, Li, Ma, Chen, Zeng, Yu, Hofman and Wang2019; Jia et al., Reference Jia, Du, Chu, Zhang, Li, Lyu, Li, Li, Zhu, Jiao, Song, Shi, Zhang, Gong, Wei, Tang, Fang, Guo, Wang, Zhou, Chu, Zuo, Yu, Yuan, Wang, Li, Shi, Yang, Zhou, Liao, Lv, Li, Kan, Zhao, Wang, Yang, Li, Liu, Wang, Qin and Jia2020), suggesting it was necessary to pay close attention to the cognitive function of the elderly over 80 years old. Antihypertensive drug was found to be a protective factor of cognitive function in this study, which was consistent with some previous researches (Levi Marpillat et al., Reference Levi Marpillat, Macquin-Mavier, Tropeano, Bachoud-Levi and Maison2013; Peters et al., Reference Peters, Collerton, Granic, Davies, Kirkwood and Jagger2015; Ou et al., Reference Ou, Tan, Shen, Xu, Hou, Dong, Tan and Yu2020), which might be due to the fact that antihypertensive drug ameliorates or mitigates white matter lesions caused by high blood pressure (Iadecola and Gottesman, Reference Iadecola and Gottesman2019).
About 42.2% of subjects with cognitive impairment had abnormal LVEF value, suggesting these residents were at a high risk of HF; 79.7% of them had abnormal VC value and might have restricted ventilation disorders; furthermore, 98.4% of cognitive impairment subjects had abnormal MVV value, indicating reduced ventilation reserve capacity. Thus, the co-prevalence of cognitive dysfunction and cardiopulmonary diseases was worthy of attention. Association between LVEF and cognitive function still remains unclear nowadays. A nonlinear U-shaped correlation between LVEF and measures of accelerated cognitive ageing was reported in one of the Framingham Heart Studies (Jefferson et al., Reference Jefferson, Himali, Au, Seshadri, Decarli, O’Donnell, Wolf, Manning, Beiser and Benjamin2011). Abnormal LVEF was found to be related with cognitive impairment in our study, which was agreement with previous studies (Bossola et al., Reference Bossola, Laudisio, Antocicco, Tazza, Colloca, Tosato and Zuccalà2014; Xing et al., Reference Xing, Chen, Sun, Neradilek, Wu, Zhang, Huang, Cui, Yang, Li and Zhao2020; Shang et al., Reference Shang, Liu, Gao, Wang, Lu, Fei, Zhang, Mi, Li, Ma, Jiang, Chen, Dang, Liu and Qu2022). Lower LVEF always elevates levels of catecholamine and endothelin 1 (Macrae et al., Reference Macrae, Robinson, Graham, Reid and McCulloch1993), and decreased cerebral blood flow then causes the damage of nerve cells, which affects cognitive function. Animal experiments also demonstrated that abnormal cardiac function can cause cognitive impairment by mediating oxidative stress (Jinawong et al., Reference Jinawong, Apaijai, Piamsiri, Maneechote, Arunsak, Chunchai, Pintana, Nawara, Chattipakorn and Chattipakorn2022). Additionally, our study also found that abnormal LVEF was associated with three domains of cognitive function, including orientation, registration and language and praxis. Abnormal VC could increase the risk of cognitive impairment in older participants in this study. An explanation was that poor breathing was associated with a reduction in the lung tissues available for gas exchange; thus, it may increase the chance of hypoventilation and chronic hypoxia and hypercapnia, which may affect neurocognitive function (Giltay et al., Reference Giltay, Nissinen, Giampaoli and Kromhout2009); besides, elevated levels of systemic inflammation markers in patients with respiratory diseases, such as C-reactive protein, interleukin 6 and fibrinogen, might increase the risk of cognitive impairment (Su et al., Reference Su, Liu, Fan, Chen, Ding, Wu, Wang and Hou2016).
Higher PF and VT scores showed significant relation with better cognitive function, which mainly shown in the orientation, attention and calculation and language and praxis domains. Physical functioning mainly assessed whether health status affects daily physiological activities. Previous studies also demonstrated that appropriate physical activities can improve cognitive function (Song and Yu, Reference Song and Yu2019; Alsubaie et al., Reference Alsubaie, Alkathiry, Abdelbasset and Nambi2020), which indicated that nursing homes should focus on physical exercise of the elderly, such as setting up some exercise equipment in nursing homes. Vitality mainly evaluated individual subjective feelings about their own energy and fatigue. Prior studies also indicated that long-term fatigue and low energy had negative effect on cognitive function (Lin et al., Reference Lin, Chen, Vance, Ball and Mapstone2013; Zhang et al., Reference Zhang, Murphy, Fang and Caban-Martinez2015). Physical exercise, nutrition supplementation, yoga and meditation can be effective methods to decrease fatigue and increase energy (Bower et al., Reference Bower, Garet, Sternlieb, Ganz, Irwin, Olmstead and Greendale2012; Ng et al., Reference Ng, Feng, Nyunt, Feng, Niti, Tan, Chan, Khoo, Chan, Yap and Yap2015). Thus, more intervention trials should be performed to explore effective measures to improve PF and VT among nursing home residents.
Our study has some implications for the formulation of primary healthcare policy. Current primary health care still faces serious challenges in detection and management of cognitive impairment (Lu et al., Reference Lu, Liu, Wells and Yu2022). The cognitive impairment of nursing home residents over 80 is a problem that cannot be ignored. That requires healthcare providers to pay more attention to the health of nursing home residents, especially cardiopulmonary function and HRQOL. Thus, there is an urgent need to provide a range of support to facilitate healthcare providers to offer accessible, affordable and appropriate cognitive impairment-related primary healthcare services for nursing home residents, such as clinical practice guidelines, policy and financial support, and information infrastructures (Lu et al., Reference Lu, Liu, Wells and Yu2022).
The present study has several limitations. Firstly, cognitive impairment was identified using MMSE rather than the gold standard measures (eg, DSM-111, NINCDS-ADRDA and clinical record) and other international scales (McKhann et al., Reference McKhann, Drachman, Folstein, Katzman, Price and Stadlan1984). Secondly, a cross-sectional study may not provide evidence of causal relationship between risk factors and cognitive impairment. A longitudinal follow-up study should be conducted to fully assess the causality. Some information such as marital status and smoking status was collected based on self-report, which could be affected by recall bias. Finally, only 197 of 677 people had qualified cardiopulmonary function tests, so selection bias may have existed.
Conclusions
Cognitive impairment is still one of the major problems in elderly nursing home residents. Previous antihypertensive drug usage, abnormal LVEF, VC, PF and VT were associated with cognitive dysfunction. We recommend that healthcare professionals and nursing staff should increase attention to the improvement of cardiopulmonary function, PF and VT. Public health policy formulation should give more consideration to the health of the nursing home residents. Further prospective studies are needed to evaluate HRQOL and cardiopulmonary risk predictors of patients with cognitive impairment.
Supplementary material
To view supplementary material for this article, please visit https://doi.org/10.1017/S1463423623000075
Availability of data and materials
The data of this study are available from the corresponding author upon reasonable request.
Acknowledgments
Not applicable.
Authors’ contributions
Conception: ZTZ, LBR, JL and LJZ; Data acquisition and formal analysis: TZ, LBR, ZYZ, XTS, YTZ, YJG and WHJ; Validation: ZTZ, LBR and ZYZ; Writing – Original Draft: ZTZ, LBR and ZYZ; Writing – Review & Editing: ZTZ, JL and LJZ; Funding Acquisition: JL and LJZ. All authors read and approved it for publication.
Financial support
This work was supported by the National Natural Science Foundation of China (Grant No. 81872720) and Shanghai Municipal Health Commission (Grant No. 201840066) to Lijuan Zhang. The Shanghai Committee of Science and Technology, China (Grant No. 22ZR1463700), the Shanghai Municipal Science and Technology Major Project (Grant No. 2021SHZDZX0100) and the Fundamental Research Funds for the Central Universities to Jue Li.
Conflicts of interest
None.
Ethics approval and consent to participate
This study was approved by medical ethical review committee of Tongji University. Informed consent was obtained from all participants.