Improving treatment rates for common mental disorders is a challenge for all governments. Australia has instituted a number of primary mental healthcare reforms in response to the high level of burden and low levels of treatment associated with affective and anxiety disorders. Reference Andrews, Sanderson, Slade and Issakidis1,Reference Andrews, Henderson and Hall2 The most recent and largest of these is the Better Access to Psychiatrists, Psychologists and General Practitioners through the Medicare Benefits Schedule (Better Access) initiative, which was introduced in November 2006 Reference Littlefield and Giese3 and is similar in scope and intent to the UK's Improving Access to Psychological Therapies initiative. Reference Clark, Layard, Smithies, Richards, Suckling and Wright4 Under Better Access, a range of new psychological services was made available through Medicare, Australia's universal health insurance system. Medicare now covers all or part of the costs of a capped number of psychological services delivered by psychologists and selected social workers and occupational therapists in the community, on referral from a general practitioner (GP), psychiatrist or paediatrician. Previously, these costs would have been borne by the consumer, either directly or through private health insurance. Uptake has been substantial – more than 1.2 million Better Access psychological services (59 per 1000 total population) were provided by allied health professionals in the first year, Reference Whiteford, Doessel and Sheridan5 with the number almost doubling (105 per 1000) in the second year 6 – suggesting that the initiative is addressing a previously unmet need. A potential risk of demand-driven programmes such as Better Access is that they may create, or widen existing, disparities in mental health service use. Limited population-level evaluation of the programme has been conducted to date. However, it has been suggested that the initiative is providing services to a number of people who may not have affective or anxiety disorders, and who live in affluent and urban areas (where most allied health professionals practice), whereas at-risk groups (e.g. young people, people in rural areas or poorer urban areas, people with low income) with legitimate need may be missing out. A further concern is that, rather than providing access to services for previously untreated individuals, the initiative is providing funding for people already receiving care from psychologists or other allied health providers. Reference Rosenberg, Hickie and Mendoza7–Reference Dunbar, Hickie, Wakerman and Reddy10 These criticisms are based on evidence drawn from analyses of Medicare claims data, however the person-level data collected by Medicare captures only limited demographic data. This makes it difficult to profile service recipients, particularly with respect to clinical characteristics. This paper explores whether Better Access is contributing to mental healthcare disparities using epidemiological data from the 2007 National Survey of Mental Health and Wellbeing. The survey collected detailed information on sociodemographic and clinical characteristics as well as service use for mental health problems.
Method
Research questions
Our research questions were aligned with the nominated concerns about Better Access. Two populations were of interest for the current study: people who had consulted a Medicare-funded psychologist or other allied health specialist for a mental health problem in the past 12 months (Better Access psychological services users); and a community sample of people with 12-month affective and anxiety disorders regardless of service use, who are the primary target of Better Access. Among the Better Access psychological service users, we sought to determine: is there evidence of overservicing of people without potential need; and are users without affective or anxiety disorders more socioeconomically advantaged than those with these disorders? Among the community sample with any 12-month ICD–10 affective or anxiety disorder we sought to determine: are there any population subgroups who appear to be missing out on Better Access psychological services; is Better Access selectively providing services to people already receiving equivalent treatment; and is there perceived need for treatment among people who do not receive services?
Sampling and procedure
The 2007 National Survey of Mental Health and Wellbeing was conducted by the Australian Bureau of Statistics between August and December 2007. The population in scope was usual residents of private dwellings across Australia, aged 16–85 years. A random sample of private dwellings was identified using a stratified, multistage area probability sampling technique. Information about household composition was obtained and an algorithm developed by the Australian Bureau of Statistics used to randomly select one person in the household aged 16–85 years to be interviewed. Younger people (16–24 years) and older people (65–85 years) were oversampled in order to improve the reliability of estimates for these groups. Of 14 805 eligible households identified, interviews were completed with 8841 (60%) of respondents. The survey methodology is described in detail elsewhere. 11,Reference Slade, Johnston, Oakley Browne, Andrews and Whiteford12
Defining the populations of interest
Diagnostic assessment
The current version of the World Mental Health Composite International Diagnostic Interview (CIDI 3.0) Reference Kessler and Üstun13 was used to assess the prevalence of lifetime diagnoses according to ICD–10 14 criteria. Questions about symptoms experienced during the 12 months prior to interview were combined with lifetime diagnosis information to determine 12-month prevalence. The survey assessed the following classes of mental disorder: affective disorders – depression, dysthymia and bipolar affective disorder; anxiety disorders – panic disorder, agoraphobia, social phobia, generalised anxiety disorder, obsessive–compulsive disorder and post-traumatic stress disorder; and substance use disorders – harmful use and dependence syndrome separately for alcohol, opioids, cannabinoids, sedatives and stimulants.
Measurement of service use for mental health problems
The service use module of the 2007 National Survey of Mental Health and Wellbeing gathered information about respondents’ 12-month and lifetime use of services for mental health problems. Respondents were asked whether they had consulted any of the following professional groups for mental health problems: GPs; psychiatrists; psychologists; mental health nurses; other mental health specialists (including social workers, occupational therapists and counsellors); other specialist doctors or surgeons; other professionals providing general services; and complementary/alternative therapists. For each type of professional consulted, respondents were asked whether they had consulted within the past 12 months for mental health problems, the number of consultations within the past 12 months for mental health problems, how these services were paid for and their age at first ever consultation. Payment source was classified into non-mutually exclusive categories: public hospital out-patients, public community health services or public community mental health services; paid or refunded in full by Medicare; paid or refunded in part by Medicare; paid or refunded in full by private insurance; paid or refunded in part by private insurance; paid in full by respondent, a friend or family member; and paid in part by respondent, a friend or family member. Age at first ever consultation was coded by the Australian Bureau of Statistics into ranges (psychologists: <16, 16–17, 18–21, 22–25, 26–29, 30–32, 33–37, 38–42, 43–47, 48–54, 55 years and over; other mental health specialists, <18, 18–23, 24–29, 30–36, 37–50, 51 years and over). Respondents were also asked whether they had been hospitalised for a mental health problem, or had used self-management strategies including internet support groups or chat rooms, self-help groups and telephone counselling.
Better Access psychological services users
To identify likely Better Access psychological services users, we selected respondents who had consulted a psychologist or other mental health specialist for a mental health problem in the past 12 months, and who reported that these services were paid for in full or in part by Medicare. We considered this strategy appropriate for two reasons. First, although psychologists, social workers and occupational therapists are able to claim Medicare subsidies for a limited range of non-Better Access mental health and other services, these represented only 2% of all Medicare-subsidised mental health services provided by these groups in 2007. Reference Whiteford, Doessel and Sheridan5 Second, although the other mental health specialist group included counsellors, counsellors are not able to claim Medicare subsidies.
Identifying disability, clinical status, treatment need and sociodemographic characteristics
Disability measures
Disability was assessed using the 12-item version of the World Health Organization Disability Assessment Schedule (WHODAS–II), 15 which asks respondents how much difficulty they had in the preceding 30 days in performing a range of activities. A score at or above the seventy-fifth percentile indicates a high level of disability. Disability was also assessed using a measure of ‘days out of role’. Respondents were asked how many days in the previous 30 they were totally unable to perform their normal activities, and how many days they had to cut down what did they did because of health problems. Total ‘days out of role’ was calculated as the weighted sum of total plus partial days out of role.
Clinical measures
Respondents with a 12-month ICD–10 disorder were classified into one of three severity categories – mild, moderate or severe – using criteria adapted from the World Mental Health Survey Initiative. 11,Reference Slade, Johnston, Oakley Browne, Andrews and Whiteford12 Psychological distress during the 30 days prior to interview was assessed using the Kessler Psychological Distress Scale (K10). Reference Kessler and Mroczek16 Respondents were also asked whether they had any of the following chronic physical conditions: diabetes, asthma, coronary heart disease, stroke, cancer and arthritis.
Treatment need
Respondents were classified on a gradient of potential need for treatment, using criteria adapted from Druss and colleagues. Reference Druss, Wang, Sampson, Olfson, Pincus and Wells17 The gradient comprised three hierarchically ordered groups: any 12-month ICD–10 disorder; one or more of the following indicators of potential need – a lifetime ICD–10 disorder, 12-month symptoms (but no lifetime diagnosis) for at least one disorder, or lifetime hospitalisation for a mental health problem; and none of the preceding indicators of potential treatment need. The Perceived Need for Care Questionnaire (PNCQ) Reference Meadows, Harvey, Fossey and Burgess18 assessed the extent to which identified treatment needs were met among respondents who had received services in the past 12 months. It was also used to assess perceived need for treatment and reasons for not receiving treatment among those who had not received services.
Sociodemographic characteristics
Sociodemographic information included respondents’ age, gender, marital status, labour force status, highest level of education attained, country of birth, language spoken at home, area of residence and household income. Respondents were classified into deciles on the Index of Relative Socioeconomic Disadvantage, 19 based on information about the geographic location of their household. The Index of Relative Socioeconomic Disadvantage provides a continuum of advantage (high values) to disadvantage (low values).
Data analysis
For analyses involving the Better Access psychological services users, we used binomial logistic regressions analyses to compare individuals with and without a 12-month ICD–10 affective or anxiety disorder on a range of sociodemographic, mental health service use and treatment need measures. For analyses involving the sample with any ICD–10 12-month affective or anxiety disorder, we used multinomial logistic regression analyses to compare three service use groups on various sociodemographic and clinical factors: Better Access psychological service users (those who received Medicare-subsidised allied health services, with or without other mental health service use); other mental health service users; and non-service users. Univariate analyses first assessed the unadjusted associations between each predictor and the dependent variable. In order to identify the most parsimonious model for predicting membership in service use groups, a multivariate analysis was then undertaken. Variables that failed to make a significant independent contribution to model fit were removed from analysis, based on the Wald chi-squared statistic (P<0.05). Multicollinearity was assessed by inspecting correlations between variables, tolerance and variance inflation factors. Binomial logistic regression analyses were also used to compare Better Access and other mental health service users on interventions received and proportion of potentially new cases to treatment.
Data were made available by the Australian Bureau of Statistics via the Basic Confidentialised Unit Record File (April 2009 version). Analyses were conducted using STATA version 10.1 for Windows. Standard errors (s.e.) and 95% confidence intervals were calculated using jackknife repeated replication, which provides unbiased estimates of the sampling error arising from complex sample selection procedures. Estimates with relative standard errors between 25% and 50%, indicating some limitations to reliability, were identified as per Australian Bureau of Statistics practice. 20 Statistical tests were two-tailed. P-values less than 0.05 were considered statistically significant.
Results
Overservicing
We looked at whether there was evidence that Better Access is overservicing people without potential need.Figure 1 shows the relative size of and overlap between the populations of Better Access psychological services users and the community sample with any 12-month affective or anxiety disorder. Of the total sample of 8841 respondents, 175 had used Better Access psychological services in the 12 months prior to interview, which roughly corresponds to the first year of the programme. This equates to an estimated population count of 290 140 persons, or 1.8% of Australian adults aged 16–85 years. Three-quarters (74.7%, s.e. = 5.4) received these services exclusively from a psychologist, a fifth from other mental health specialists only (21.1%, s.e. = 5.1), and less than one in twenty from both a psychologist and another mental health specialist (4.3%, s.e. = 2.6). Better Access users represented 37.3% (s.e. = 3.5) of all adult Australians who received services from these providers.
Among Better Access psychological services users, 50.1% (s.e. = 6.2) had a 12-month ICD–10 affective disorder and 60.9% (s.e. = 5.4) had a 12-month ICD–10 anxiety disorder (categories not mutually exclusive). An estimated 14.2% (s.e. = 4.9) had a 12-month ICD–10 substance use disorder, however the majority of these (78.4%, s.e. = 9.5) were comorbid with 12-month ICD–10 affective or anxiety disorders. Almost one in five (18.3%, s.e. = 3.3) Better Access users did not have a 12-month ICD–10 disorder.
The majority of Better Access users had a potential need for treatment: 81.7% (s.e. = 3.3) had a 12-month ICD–10 affective, anxiety or substance use disorder; 11.5% (s.e. = 2.1) had at least one other indicator of potential need (lifetime disorder, 12-month symptoms or lifetime hospitalisation for a mental disorder); and 6.8% (s.e. = 2.2) had no indicator of potential need.
Socioeconomic profile
We examined whether Better Access users without a 12-month ICD–10 affective or anxiety disorder (21.3%, s.e. = 3.5) had a different socioeconomic profile than users with these disorders (78.7%, s.e. = 3.5). There were no statistically significant differences between the groups (Table 1).
Table 1 Sociodemographic correlates of 12-month ICD–10 affective or anxiety disorder status among Better Access psychological services usersa
| No 12-month ICD–10 affective or anxiety disorder (N = 51) b | Any 12-month ICD–10 affective or anxiety disorder (N = 124) b | ||||||
|---|---|---|---|---|---|---|---|
| n b | % (s.e.) | n b | % (s.e.) | OR c (95% CI) | P | ||
| Female | 36 | 64.5 (8.6) | 94 | 67.1 (6.1) | 1.1 | (0.4–3.0) | 0.813 |
| Age group | |||||||
| 16–34 years | 14 | 31.7 (7.7) | 47 | 40.5 (6.3) | 1.0 | ||
| 35–54 years | 21 | 40.6 (7.0) | 54 | 45.4 (6.7) | 0.9 | (0.3–2.2) | 0.777 |
| 55–85 years | 16 | 27.7d (7.4) | 23 | 14.1d (3.6) | 0.4 | (0.1–1.2) | 0.108 |
| Married | 16 | 34.9 (7.7) | 33 | 36.6 (7.5) | 1.1 | (0.4–3.1) | 0.889 |
| Born in Australia | 37 | 71.0 (7.6) | 102 | 85.3d (3.9) | 2.4 | (0.8–7.1) | 0.121 |
| Lives in major urban area | 33 | 68.1 (8.1) | 81 | 76.3d (4.3) | 1.5 | (0.6–3.7) | 0.365 |
| Least socioeconomic disadvantage (IRSED deciles 7–10) | 23 | 41.6 (8.3) | 57 | 40.2 (6.1) | 0.9 | (0.4–2.3) | 0.893 |
| Post-school qualification | 35 | 62.1 (8.5) | 71 | 53.5 (6.7) | 0.7 | (0.3–1.6) | 0.395 |
| Employed | 33 | 58.0 (7.1) | 69 | 52.1 (6.9) | 0.8 | (0.4–1.7) | 0.524 |
| High level of income (household income deciles 7–10)e | 17 | 35.2 (8.5) | 31 | 26.0 (6.4) | 0.6 | (0.2–1.9) | 0.421 |
A greater proportion of Better Access users with 12-month ICD–10 affective or anxiety disorders received 10 or more consultations for a mental health problem in the past year, but there were no differences in types of help received or whether perceived needs for treatment were met (Table 2).
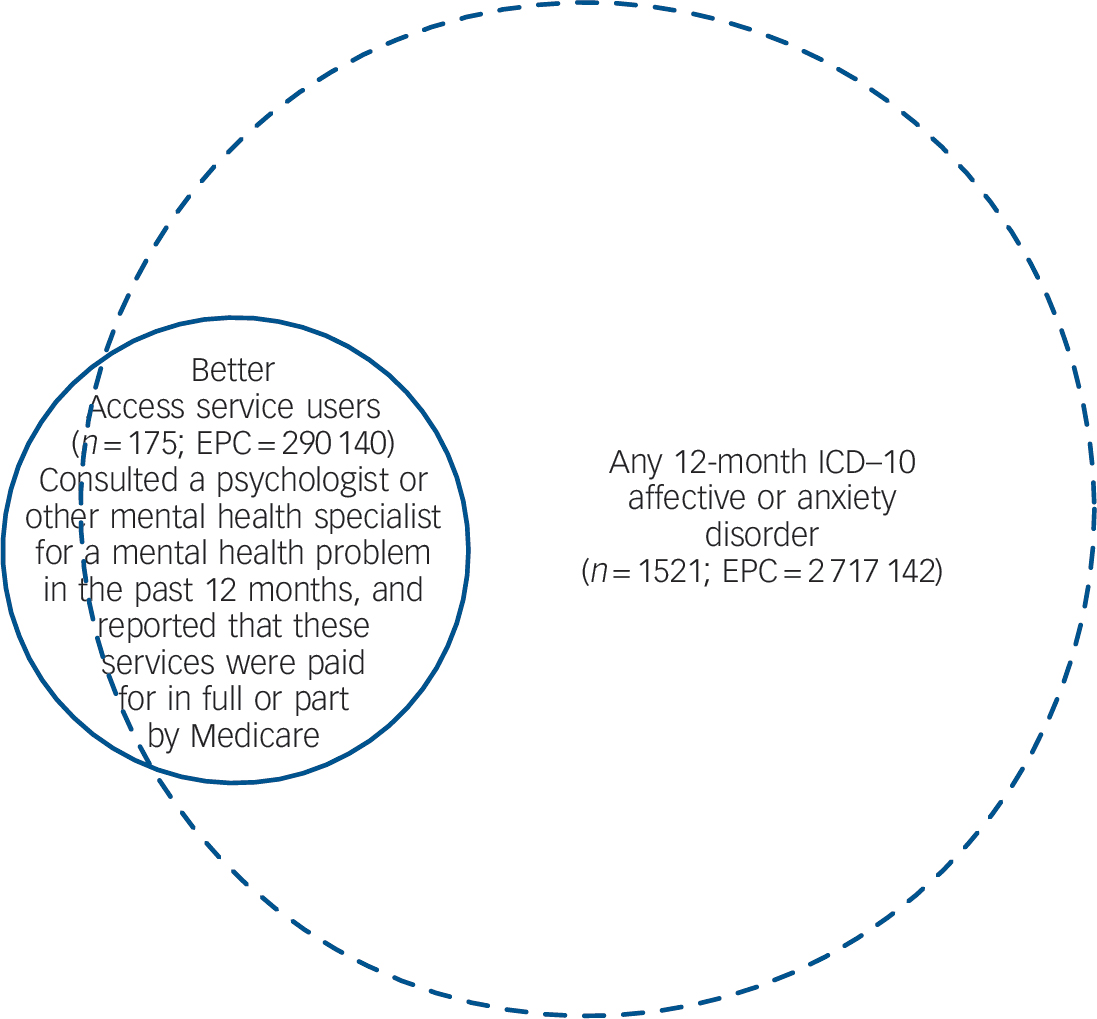
Fig. 1 Overlap between Better Access psychological services users and the community sample with any 12-month ICD–10 affective or anxiety disorder.
n, unweighted number of respondents; EPC, estimated population count.
Table 2 Treatment correlates of 12-month ICD–10 affective or anxiety disorder status among Better Access psychological services usersa
| No 12-month ICD–10 affective or anxiety disorder (N = 51) b | Any 12-month ICD–10 affective or anxiety disorder (N = 124) b | ||||||
|---|---|---|---|---|---|---|---|
| Consultations for mental health problems | n b | % (s.e.) | n b | % (s.e.) | OR c (95% CI) | P | |
| Number of consultations with any professional in past 12 months | |||||||
| 1–4 | 20 | 42.6 (8.6) | 26 | 20.1 (4.6) | 1.0 | ||
| 5–9 | 15 | 26.2 (6.0) | 27 | 17.4 (4.6) | 1.4 | (0.5–3.9) | 0.504 |
| 10 or more | 16 | 31.1 (7.1) | 71 | 62.4 (7.0) | 4.2 | (1.4–12.9) | 0.012 |
| Type of help | |||||||
| Information about treatment and illness | 23 | 49.4 (8.3) | 74 | 66.5 (5.3) | 2.0 | (0.8–4.9) | 0.112 |
| Medicine or tablets | 25 | 49.4 (8.8) | 85 | 67.6 (6.7) | 2.1 | (0.8–5.7) | 0.126 |
| Psychotherapy | 12 | 22.4d (6.4) | 45 | 42.9 (7.9) | 2.6 | (0.9–7.9) | 0.091 |
| Cognitive–behavioural therapy | 21 | 38.3 (8.8) | 64 | 46.1 (7.1) | 1.4 | (0.6–3.4) | 0.477 |
| Non-specific counselling | 40 | 77.7d (6.8) | 101 | 82.3 (4.4) | 1.3 | (0.5–3.7) | 0.570 |
| Social support or other help | 14 | 31.6d (8.6) | 37 | 35.6 (7.5) | 1.2 | (0.4–3.3) | 0.725 |
| Perceived need for treatment | |||||||
| Need(s) fully met | 32 | 56.9 (8.5) | 62 | 50.4 (7.3) | 0.8 | (0.3–2.0) | 0.582 |
Underservicing
Among the community sample with any ICD–10 12-month affective or anxiety disorder, we looked at whether there were any population subgroups who appear to be missing out on Better Access psychological services.Figure 2 shows the rates of service use for a mental health problem in the past 12 months among people with and without 12-month ICD–10 affective or anxiety disorders. Notably, 8.4% of people with these disorders actually used Better Access psychological services, and 21.5% of those who used any services for a mental health problem in the past 12 months used Better Access.
The remaining analyses focused on the community sample with any 12-month ICD–10 affective or anxiety disorder. Tables3 and4 summarise the associations between sociodemographic, clinical and disability measures and membership in three different service use groups – Better Access, other service use and no service use. There were no differences between Better Access psychological service users and other service users on any of these measures. There were, however, a number of differences between the Better Access and non-service user groups. Non-service users had twice the odds of being employed compared with the Better Access group (Table 3). They had 3.6 times the odds of having an anxiety disorder as their only 12-month mental disorder but only a quarter of the odds of having a 12-month affective disorder, either alone or in combination with another disorder. Non-service use was also negatively associated with severity, days out of role and psychological distress (Table 4).
Table 3 Sociodemographic correlates of service use among the community sample with any 12-month ICD–10 affective or anxiety disorder
| Better Access psychological services use (N = l24) a | Other mental health service use (N = 502) a | No mental health service use (N = 895) a | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n a | % (s.e.) | n a | % (s.e.) | OR b (95% CI) | P | n a | % (s.e.) | OR b (95% CI) | P | ||||||
| Female | 94 | 67.1 | (6.1) | 362 | 66.4 | (3.8) | 1.0 | (0.5–1.9) | 0.926 | 551 | 57.5 | (2.4) | 0.7 | (0.4–1.2) | 0.200 |
| Age group | |||||||||||||||
| 16–34 years | 47 | 40.5 | (6.3) | 170 | 33.5 | (2.3) | 1.0 | 361 | 40.2 | (2.1) | 1.0 | ||||
| 35–54 years | 54 | 45.4 | (6.7) | 229 | 48.7 | (2.4) | 1.3 | (0.7–2.4) | 0.397 | 324 | 42.4 | (2.3) | 0.9 | (0.5–1.7) | 0.835 |
| 55–85 years | 23 | 14.1 | (3.6) | 103 | 17.8 | (2.0) | 1.5 | (0.7–3.2) | 0.259 | 210 | 17.4 | (1.4) | 1.2 | (0.6–2.5) | 0.534 |
| Married | 33 | 36.6 | (7.5) | 140 | 37.8 | (3.2) | 1.0 | (0.5–2.0) | 0.892 | 322 | 43.3 | (2.5) | 1.3 | (0.6–2.7) | 0.435 |
| Born in Australia | 102 | 85.3c | (3.9) | 391 | 77.6 | (2.9) | 0.6 | (0.3–1.1) | 0.090 | 703 | 77.8 | (2.0) | 0.6 | (0.3–1.2) | 0.155 |
| Lives in major urban area | 81 | 76.3 | (4.3) | 333 | 68.2 | (2.6) | 0.7 | (0.4–1.1) | 0.127 | 569 | 66.0 | (2.3) | 0.6 | (0.3–1.1) | 0.076 |
| Least socioeconomic disadvantage (IRSED deciles 7–10) | 57 | 40.2 | (6.1) | 193 | 37.8 | (3.1) | 0.9 | (0.5–1.6) | 0.723 | 375 | 43.0 | (2.6) | 1.1 | (0.7–1.8) | 0.633 |
| Post-school qualification | 71 | 53.5 | (6.7) | 287 | 52.6 | (3.1) | 1.0 | (0.6–1.7) | 0.892 | 502 | 53.1 | (2.4) | 1.0 | (0.5–1.8) | 0.950 |
| Employed | 69 | 52.1 | (6.9) | 298 | 57.5 | (2.9) | 1.2 | (0.7–2.3) | 0.488 | 598 | 68.7 | (1.9) | 2.0 | (1.2–3.5) | 0.014 |
| High level of Income (household income deciles 7–10)d | 31 | 26.0 | (6.4) | 131 | 27.5 | (3.1) | 1.1 | (0.5–2.2) | 0.828 | 314 | 39.2 | (2.9) | 1.8 | (0.9–3.6) | 0.072 |
Table 4 Clinical correlates of service use among the community sample with any 12-month ICD–10 affective or anxiety disorder
| Better Access psychological services use (N = l24) a | Other mental health service use (N = 502) | No mental health service use (N = 895) | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n a | % (s.e.) | n a | % (s.e.) | OR b (95% CI) | P | n a | % (s.e.) | OR b (95% CI) | P | ||||||
| 12-month ICD–10 affective disorder | |||||||||||||||
| No affective disorder | 51 | 36.3 | (6.8) | 234 | 47.3 | (3.2) | 1.0 | 681 | 75.1 | (2.3) | 1.0 | ||||
| Affective disorder only | 23 | 20.6c | (6.0) | 80 | 14.9 | (2.0) | 0.6 | (0.2–1.3) | 0.172 | 97 | 10.8 | (1.4) | 0.3 | (0.1–0.6) | 0.002 |
| Affective disorder plus other ICD–10 12-month disorder | 50 | 43.1 | (7.8) | 188 | 37.8 | (2.8) | 0.7 | (0.3–1.3) | 0.255 | 117 | 14.0 | (1.5) | 0.2 | (0.1–0.3) | <0.001 |
| 12-month ICD–10 anxiety disorder | |||||||||||||||
| No anxiety disorder | 26 | 22.5c | (6.0) | 88 | 16.5 | (2.3) | 1.0 | 112 | 13.6 | (1.9) | 1.0 | – | |||
| Anxiety disorder only | 45 | 31.0 | (6.5) | 211 | 42.6 | (3.3) | 1.9 | (0.8–4.4) | 0.143 | 622 | 68.2 | (2.3) | 3.6 | (1.5–8.6) | 0.004 |
| Anxiety disorder plus other ICD–10 12-month disorder | 53 | 46.5 | (7.7) | 203 | 40.9 | (3.1) | 1.2 | (0.5–2.9) | 0.675 | 161 | 18.2 | (1.5) | 0.6 | (0.3–1.5) | 0.312 |
| Any chronic physical conditiond in past 12 months | 39 | 23.7 | (4.6) | 166 | 33.1 | (3.3) | 1.6 | (0.9–2.9) | 0.134 | 281 | 30.4 | (2.4) | 1.4 | (0.8–2.5) | 0.256 |
| Severe disorder, compared with mild or moderate | 58 | 47.6 | (7.7) | 193 | 37.8 | (3.2) | 0.7 | (0.3–1.3) | 0.223 | 120 | 13.5 | (1.9) | 0.2 | (0.1–0.4) | <0.001 |
| Duration of disorder, years since onsete | |||||||||||||||
| 0–10 | 42 | 30.0 | (5.6) | 142 | 24.7 | (2.4) | 1.0 | 289 | 32.0 | (2.2) | 1.0 | ||||
| 11–20 | 26 | 17.5 | (4.0) | 112 | 26.4 | (3.1) | 1.8 | (0.9–3.8) | 0.102 | 208 | 25.6 | (2.3) | 1.4 | (0.7–2.8) | 0.357 |
| 21–more | 55 | 52.5 | (6.5) | 246 | 48.9 | (3.6) | 1.1 | (0.6–2.2) | 0.709 | 392 | 42.3 | (2.5) | 0.8 | (0.4–1.4) | 0.379 |
| High level of disability (WHODAS–II)f | 57 | 45.5 | (7.1) | 235 | 51.9 | (3.2) | 1.3 | (0.7–2.6) | 0.453 | 226 | 35.9 | (3.2) | 0.7 | (0.4–1.3) | 0.214 |
| 7 or more days out of role in past 30 daysg | 38 | 28.1 | (6.2) | 147 | 30.1 | (2.8) | 1.1 | (0.6–2.1) | 0.769 | 124 | 12.9 | (1.5) | 0.4 | (0.2–0.8) | 0.010 |
| High or very high psychological distress (K10) | 64 | 45.9 | (7.2) | 241 | 49.9 | (3.0) | 1.2 | (0.6–2.3) | 0.633 | 205 | 23.5 | (2.0) | 0.4 | (0.2–0.7) | 0.003 |
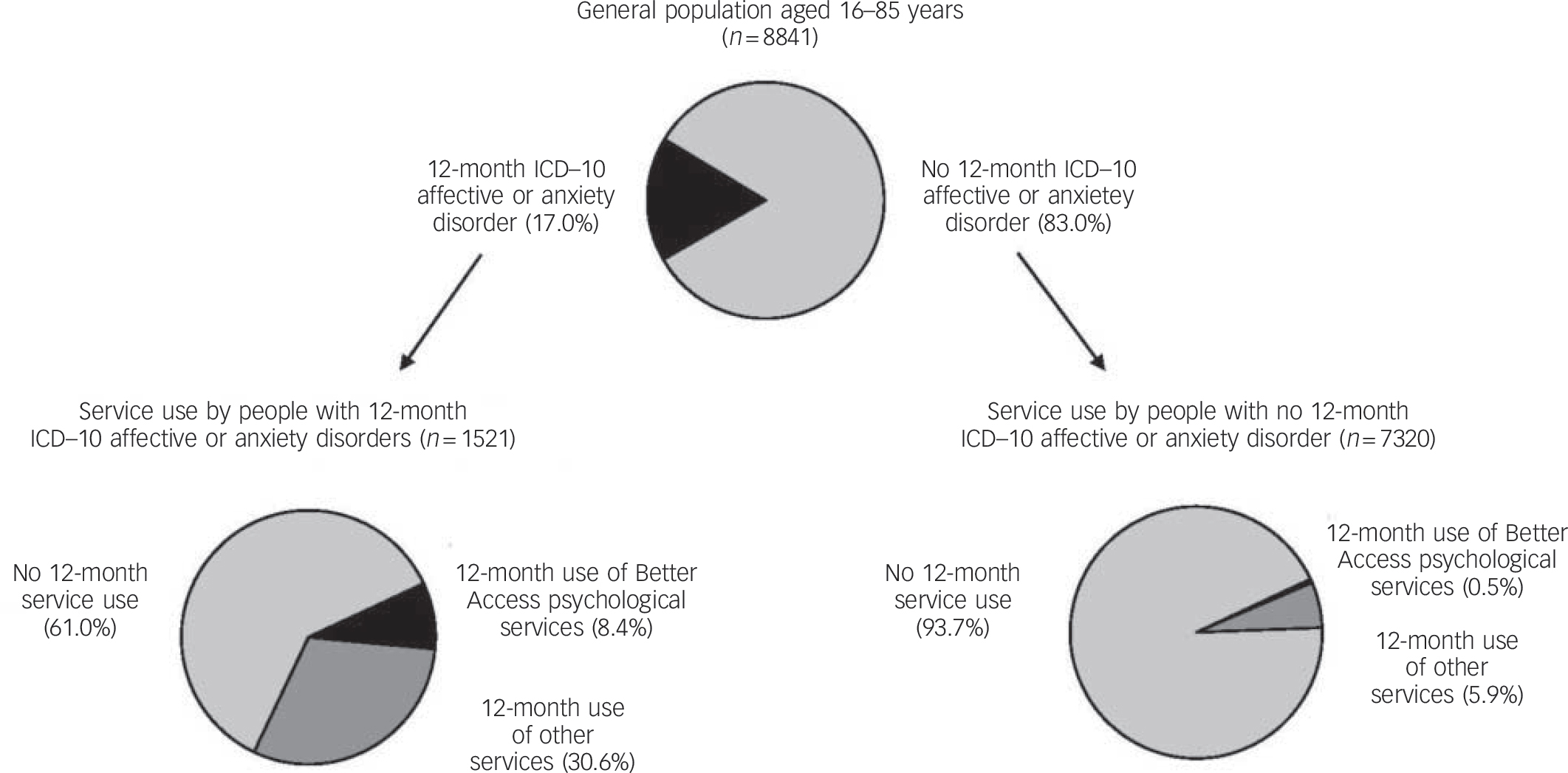
Fig. 2 Use of services for a mental health problem in the past 12 months among people with and without a 12-month ICD–10 affective or anxiety disorder.
n, unweighted number of respondents. Percentages may not sum to 100 because of rounding.
The multivariate multinomial analysis showed, however, that two variables were the key determinants of whether a person with 12-month affective or anxiety disorder was a non-service user, compared with being a Better Access user. These were: lower odds of having a severe disorder (adjusted odds ratio (OR) = 0.3, 95% CI 0.2–0.6, P = 0.002); and lower odds of having a 12-month ICD–10 affective disorder, either alone (adjusted OR = 0.3, 95% CI 0.1–0.8, P = 0.016), or in combination with another disorder (adjusted OR = 0.3, 95% CI 0.1–0.6, P = 0.001), compared with not having an affective disorder. Because the sample for this analysis comprises individuals with an affective or anxiety disorder, respondents in the reference category ‘no affective disorder’ are those who had an anxiety disorder that is not comorbid with an affective disorder.
We were also interested in whether service use patterns differed between the Better Access and other service user groups. Binomial logistic regression analyses showed a monotonic increasing association between Better Access service use and number of mental health consultations in the past 12 months. Better Access users also had twice the odds of reporting receipt of information about illness and treatment and almost four times the odds of reporting receipt of non-specific counselling than other service users. There were no significant differences in self-reported rates of receipt of other interventions, including cognitive–behavioural therapy (CBT) (Table 5).
Table 5 Treatment correlates of service use among the community sample with any 12-month ICD–10 affective and anxiety disorder
| Other mental health service use (N = 502) | Better Access psychological services use (N = 124) | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| n a | % (s.e.) | n a | % (s.e.) | OR b (95% CI) | P | ||||
| Consultations for mental health problems | |||||||||
| Number of consultations with any professional in past 12 monthsc | |||||||||
| 1–4 | 261 | 52.4 | (3.1) | 26 | 20.1 | (4.6) | 1.0 | – | |
| 5–9 | 94 | 17.6 | (2.3) | 27 | 17.4 | (4.6) | 2.6 | (1.2–5.6) | 0.017 |
| 10 or more | 143 | 29.9 | (3.1) | 71 | 62.4 | (7.0) | 5.4 | (2.7–11.0) | <0.001 |
| Consulted GP for mental health problem in past 12 monthsd | 369 | 73.9 | (2.2) | 95 | 73.1 | (5.6) | 1.0 | (0.5–1.8) | 0.892 |
| Intervention type | |||||||||
| Information about illness | 239 | 48.2 | (3.1) | 74 | 66.5 | (5.3) | 2.1 | (1.2–3.7) | 0.008 |
| Medicine or tablets | 335 | 66.9 | (3.0) | 85 | 67.6 | (6.7) | 1.0 | (0.5–1.9) | 0.924 |
| Psychotherapy | 143 | 29.4 | (3.0) | 45 | 42.9 | (7.9) | 1.8 | (0.9–3.8) | 0.121 |
| Cognitive behavioural therapy | 154 | 32.5 | (3.7) | 64 | 46.1 | (7.1) | 1.8 | (0.9–3.5) | 0.095 |
| Non-specific counselling | 274 | 55.0 | (2.5) | 101 | 82.3 | (4.5) | 3.8 | (1.8–8.0) | 0.001 |
| Social support or other help | 126 | 26.1 | (3.0) | 37 | 35.6 | (7.5) | 1.6 | (0.8–3.0) | 0.168 |
| Received medication appropriate for affective/anxiety disorder | 248 | 51.2 | (3.4) | 68 | 51.7 | (7.0) | 1.0 | (0.6–1.8) | 0.942 |
| Needs for care met | |||||||||
| Need(s) fully met | 235 | 43.4 | (3.0) | 62 | 50.4 | (7.3) | 1.3 | (0.7–2.6) | 0.401 |
New to treatment
Ideally, the question of whether Better Access is selectively providing services to people already receiving equivalent treatment would be examined by determining the proportion of Better Access service users who had seen a psychologist or other mental health specialist for the first time in the past year. However, as data on age at first ever consultation was only available in ranges, we could not calculate the exact period elapsed since first consultation. Hence, we took the following approach. Current age was recoded into age ranges equivalent to those used to report age at first consultation, separately for each type of professional consulted because the available age ranges differed by provider type. Individuals whose age ranges matched were deemed to be potentially ‘new’ cases. We then compared the proportion of potentially new cases in the Better Access group with the other service user group. Among individuals who had consulted a psychologist in the past 12 months (n = 336), there was a significantly greater proportion of potentially new cases in the Better Access group (54.4%, s.e. = 7.5) than in the other service user group (30.5%, s.e. = 4.3, OR = 2.7, 95% CI 1.3–5.9, P = 0.011), but no difference in the subsample (n = 177) who had seen another mental health specialist (48.0% (s.e. = 13.6) v. 44.2% (s.e. = 6.3); OR = 1.2, 95% CI 0.3–4.1, P = 0.812). When results for psychologists and other mental health specialists were combined (n = 412), we found a significantly greater proportion of potentially new cases in the Better Access group compared with the other service users (62.3% (s.e. = 6.7) v. 38.7% (s.e. = 3.5), OR = 2.6, 95% CI 1.4–4.9, P = 0.003).
Perceived need for treatment among non-service users
One in six people with 12-month ICD–10 affective and anxiety disorders who did not use services reported a perceived need for treatment (Table 6). A greater proportion of those with severe disorder had a perceived need (36.1%, s.e. = 6.8), compared with those with mild or moderate disorders (9.2%, s.e. = 1.7, OR = 5.6, 95% CI 2.7–11.7, P<0.001).
Table 6 Perceived needs for treatment for people and reasons for not seeking help among the community sample with any 12-month ICD–10 affective or anxiety disorder who did not use services (n = 895)a,b
| Perceived needs for treatment | n b | % (s.e.) | |
|---|---|---|---|
| Any perceived need | 143 | 16.1 | (1.8) |
| Type of intervention needed (if any perceived need) | |||
| Information about illness | 63 | 42.9 | (6.7) |
| Medicine or tablets | 24 | 15.3c | (3.7) |
| Psychotherapy, cognitive–behavioural therapy or non-specific counselling | 110 | 74.5 | (5.1) |
| Housing or money | 33 | 25.1 | (6.4) |
| Work | 34 | 23.3 | (5.3) |
| Personal care | 20 | 13.4 | (3.9) |
| Social support or other help | 36 | 18.3 | (2.8) |
| Reason for not seeking help (if any perceived need) | |||
| I preferred to manage myself | 79 | 54.4 | (6.0) |
| I didn't think anything could help | 28 | 13.9 | (3.0) |
| I didn't know where to get help | 26 | 17.0c | (4.6) |
| I was afraid to ask for help or what others would think of me if I did | 29 | 17.9 | (3.4) |
| I couldn't afford the money | 24 | 18.8c | (5.0) |
| Other reasonsd | 20 | 14.8c | (4.5) |
Among those who identified any perceived need, the most common need was for ‘talking’ therapies. When asked their reasons for not seeking help for their need(s), the most common response selected by respondents was that they preferred to manage themselves. Cost was identified as a barrier by less than one in five people.
Non-service users did not report any use of complementary therapies. In addition, only 1.3% (s.e. = 0.3) used self-management strategies, a significantly lower proportion than the Better Access service users (17.9%, s.e. = 5.6, OR = 16.0, 95% CI 5.4–47.2, P<0.001) or the other service user groups (13.4%, s.e. = 2.3, OR = 11.3, 95% CI 5.4–23.5, P<0.001).
Discussion
Summary and interpretation of findings
This study provides evidence regarding five sources of potential failure in the implementation of the Better Access initiative. First, the majority of Better Access service users had a 12-month ICD–10 mental disorder (81.7%) or another indicator of treatment need (11.5%). Prevalence of 12-month disorder was higher than among service users generally (58.7% in the 2007 National Survey of Mental Health and Wellbeing Reference Slade, Johnston, Teesson, Whiteford, Burgess and Pirkis21 and 61.2% in the National Comorbidity Survey Replication in the USA) Reference Wang, Aguilar-Gaxiola, Alonso, Angermeyer, Borges and Bromet22 suggesting that referrals being made to allied health providers under Better Access are appropriate. The estimate of 6.8% without an indicator of need is similar to US estimates of 8.0% among service users generally. Reference Druss, Wang, Sampson, Olfson, Pincus and Wells17 It is possible that the true figure for Better Access psychological services is even lower, as the 6.8% may have included people with disorders not assessed by the 2007 National Survey of Mental Health and Wellbeing or indicators of treatment need not assessed by this study (e.g. simple phobias, psychotic disorders, personality disorders, or subthreshold symptoms of these disorders). Regardless, it has been suggested that a false-positive treatment rate of this magnitude is acceptable. Reference Druss, Wang, Sampson, Olfson, Pincus and Wells17
Second, Better Access users without 12-month ICD–10 affective or anxiety disorders were not more socioeconomically advantaged. They tended to include fewer people born in Australia and more older people, but these differences were not statistically significant, possibly because of small numbers. Better Access users with a disorder received a higher intensity of treatment than those without. They also tended to receive more psychoeducation, medication and psychotherapy; but again small numbers may have limited the possibility of finding these differences statistically significant. Taken together, these findings indicate that resources are not being inappropriately diverted from people with genuine need.
Third, our analyses among the community sample with 12-month ICD–10 affective or anxiety disorders did not indicate social inequalities in the use of Better Access psychological services, but did suggest that access may be better for some clinical groups than others. Even after controlling for severity of disorder, people with affective disorders were more likely to use Better Access psychological services than to not use services, whereas the reverse was true for people who had anxiety disorders that were not comorbid with affective disorders.
Evidence from population-based surveys and large studies of mental health service users suggest that there may be unequal access to psychological therapies and services provided by allied health professionals. Younger age, Reference Kessler, Demler, Frank, Olfson, Pincus and Walters23 being separated Reference Kessler, Demler, Frank, Olfson, Pincus and Walters23,Reference Parslow and Jorm24 or single, Reference Kessler, Demler, Frank, Olfson, Pincus and Walters23 poorer education level, Reference Kessler, Demler, Frank, Olfson, Pincus and Walters23 employment, Reference Issakidis and Andrews25 higher income, Reference Issakidis and Andrews25 and being Black or Asian Reference Raleigh, Irons, Hawe, Scobie, Cook and Reeves26 have been found in some, but not all Reference Bebbington, Brugha, Meltzer, Jenkins, Ceresa and Farrell27 studies, to predict receipt of these treatments. In our study, type and severity of disorder were the only predictors of Better Access psychological service use compared with no service use. Geographical location, level of socioeconomic disadvantage and demographic factors were not significant predictors, after taking the effects of clinical factors into account. Moreover, there were no factors differentiating Better Access from other service use. Our findings suggest that Better Access is providing equitable access to people in need. However, our ability to draw comparisons with previous findings is limited by differences in the samples used for analysis (diagnostic groups, service users), study settings (general population, primary care) and in the definitions of the services being examined.
Better Access psychological services users more frequently reported receiving psychoeducation and non-specific counselling, but not CBT, than those who used other services. The CBT finding was contrary to expectation, given that Better Access was intended to promote the use of evidence-based therapies such as psychoeducation, CBT and interpersonal therapy. Reference Whiteford, Doessel and Sheridan5 This finding may suggest that other services provide more CBT than expected, or that Better Access services provided greater levels of other therapies than expected. Alternately, it may reflect shortcomings in population mental health literacy relating to the correct labelling of specific interventions.
Fourth, although we were unable to derive precise estimates of the proportion of Better Access users whose first consultation with an allied health provider had occurred in the preceding year, our estimate of 62% is broadly consistent with findings from independent surveys of Australian psychologists who report that around 70% of their Better Access clients have not previously consulted a psychologist. Reference Giese, Littlefield and Mathews28,Reference Forsyth and Mathews29
Fifth, we found that 61.0% of people with 12-month affective or anxiety disorders had not used services. Although this group could potentially benefit from Better Access, they reported low rates of perceived need for treatment (16.1%) and did not seek treatment alternatives. Even among the 13.5% of non-service users with severe disorders, only a third perceived a need for treatment. Of those who did perceive a need for treatment, cost was identified as a barrier to receiving services by only one in five. Factors such as knowledge or beliefs about the availability and effectiveness of treatments, and stigma, appear to collectively have a stronger influence on perceptions of treatment need.
Levels of perceived need among non-service users (of whom 86.4% had anxiety disorders) were much lower than those previously reported from the 1997 National Survey of Mental Health and Wellbeing among people with full-threshold 12-month anxiety disorders, but similar to those with subthreshold anxiety disorders. Reference Issakidis and Andrews30 This may be due to less strict operationalisation of diagnostic criteria in the 2007 National Survey of Mental Health and Wellbeing. Reference Slade, Johnston, Oakley Browne, Andrews and Whiteford12
Threats to validity
Are the Better Access service use estimates valid?
We estimated that 290 140 adults are likely to have received Better Access psychological services from allied health professionals in the first year of the programme, but note that the survey measures of health service use, including use of Medicare-funded services, rely on unverified, retrospective self-report. We derived similar estimates of 295 000 and 305 000 from independently published analyses of Medicare claims data. Reference Whiteford, Doessel and Sheridan5,31 The slightly lower survey-based estimate reflects the timing of the survey, which meant that not all respondents would have accrued a full year of opportunity to receive Better Access services, and because it was limited to people aged 16–85 years. We found good agreement with published Medicare data Reference Issakidis and Andrews30 with respect to rates of Better Access treatment by age, gender and urbanicity. Comparisons by type of professional consulted suggest that the survey may overestimate rates of Better Access treatment by social workers or occupational therapists and underestimate those from psychologists. This may indicate shortcomings in the general public's ability to reliably identify the specific disciplines of mental health professionals, and may also reflect previous findings that counsellors are identified by more people as helpful for depression than psychologists. Reference Jorm, Christensen and Griffiths32 Overall, however, the comparisons lend support for the validity of the survey-based estimates of Better Access service use.
Other methodological considerations
Other potential limitations to the study require comment. First, the survey response rate of 60% may have introduced selection biases, however we do not know whether these may have affected participation rates among people with mental disorders. Second, the extent to which inferences about causality can be made is limited by the cross-sectional nature of the survey. 11,Reference Slade, Johnston, Oakley Browne, Andrews and Whiteford12 Third, the survey did not ask respondents about use of Better Access services by name. However, as we do not know whether consumers would correctly identify the services they received as being part of Better Access, we consider that asking individuals about the professionals consulted and means of payment is the most accurate way to determine Better Access service use under survey conditions. As noted earlier, this method may have captured people receiving Medicare-subsidised allied health services provided under other programmes, however the number is considered negligible. Fourth, membership of service use groups was hierarchical and allocated anyone who reported receiving Medicare-subsidised allied health services to the Better Access group, even though they may have had multiple payers for one consultation, or had multiple payers across multiple consultations. Finally, as already noted, the relatively small numbers available for some comparisons of Better Access users may have limited the power of our study to detect some differences in sociodemographic profile and treatments received as statistically significant. Importantly, we followed standard best practice in reporting estimates from population surveys. We identified a small number of estimates with relative standard error percentages above the 25% threshold but in each of these cases the relative standard error percentage was not greater than 30%, thus any limitations to reliability can be considered relatively small.
Policy and research implications
The high personal, social and economic costs associated with common mental disorders have led governments to implement major primary mental healthcare reforms such as Better Access and Improving Access to Psychological Therapies to improve access to psychological treatments. However, the potential for such programmes to create, or widen, existing disparities in mental health service use is of concern. Reference Clark, Layard, Smithies, Richards, Suckling and Wright4,Reference Rosenberg, Hickie and Mendoza7–Reference Crosbie and Rosenberg9,33,Reference Ghosh34 Our findings suggest two implications for policy. First, although Better Access appears to be providing equitable access, people who have anxiety disorders that are not comorbid with affective disorders appear to be a group for whom detection and/or referral to Better Access psychological services could be improved. Second, a substantial number of people with affective or anxiety disorders, who could potentially benefit from Better Access services, did not use these or any other services. Non-service was not associated with socioeconomic or geographical factors, but perceived need for treatment in this group (even among those with severe disorders) was low. Mental literacy efforts may be more helpful in improving treatment rates among this group than increasing opportunities for access to treatment.
Our findings also have research implications. To reduce the burden of common mental disorders it is necessary to not only increase treatment coverage to populations in need, but also to ensure that evidence-based treatments are being delivered to those who gain access. Reference Andrews35,Reference Whiteford36 At a clinical level, longitudinal studies of Better Access consumers are needed to examine the quality, outcomes and technical efficiency of the programme. At a population level, findings from the 1997 and 2007 National Survey of Mental Health and Wellbeing suggest that although overall rates of service use by people with affective and anxiety disorders did not change over the intervening decade, treatment by psychologists doubled, Reference Burgess, Pirkis, Slade, Johnston, Meadows and Gunn37 presumably due to Better Access and other reforms. Reference Whiteford and Groves38 Using epidemiological data from the 1997 National Survey of Mental Health and Wellbeing, coupled with evidence and expert opinion, Andrews and colleagues estimated the number of psychological services required to provide optimal treatment at optimal coverage to people with affective and anxiety disorders. Reference Andrews35,Reference Andrews, Issakidis, Sanderson, Corry and Lapsley39 Future analyses of the 2007 National Survey of Mental Health and Wellbeing may inform whether large-scale primary mental healthcare reforms such as Better Access can contribute to improvements in treatment quality and coverage for these disorders.
Funding
The 2007 National Survey of Mental Health and Wellbeing was funded by the Australian Government Department of Health and Ageing, and conducted by the Australian Bureau of Statistics.











eLetters
No eLetters have been published for this article.