As of September 2023, over 695 million cases and more than 6.9 million deaths have been reported worldwide following infection with coronavirus (severe acute respiratory syndrome coronavirus 2 [SARS-CoV-2]). 1 The coronavirus disease 2019 (COVID-19) pandemic has undoubtedly posed the biggest threat to global health and well-being in living memory. Reference Boukhris, Hillani and Moroni2,Reference Faghy, Owen and Thomas3 This resulted in international governments and global health systems being placed under unforeseen and insurmountable pressure due to a surge in demand for inpatient care. Reference Remuzzi and Remuzzi4 During 2020, ∼20% of confirmed COVID-19 cases resulted in hospitalization due to the high transmission rate and virulence, Reference McCabe, Schmit and Christen5,Reference Adil, Rahman and Whitelaw6 forcing health services globally into a shortage of resources including staff, supplies, equipment, and bed space. Reference Kadri, Sun and Lawandi7 Within the United Kingdom (UK), the health-care crisis provoked governments to introduce public health measures, including quarantining, social distancing, and mandatory mask-wearing to control the spread of the virus, in line with World Health Organization guidelines. 8 Figure 1 displays the timeline of COVID-19 guidelines, including a visual representation of the tightening and easing of restrictions that took place in the United Kingdom. 9–Reference Brown, Kirk Wade and Baker17
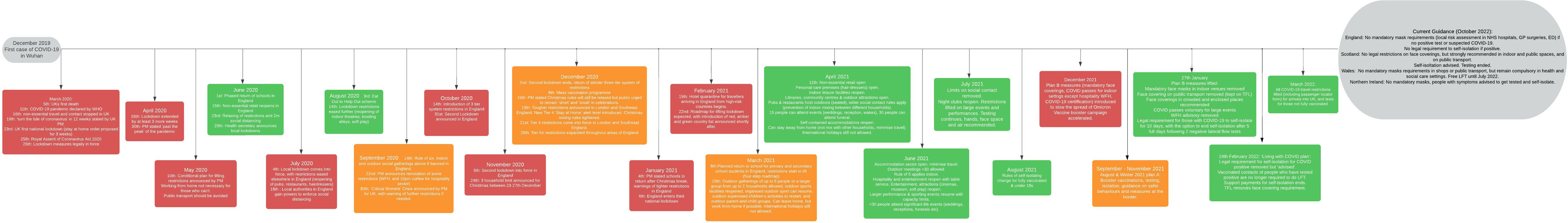
Figure 1. The timeline of COVID-19 guidelines, including a visual representation of the tightening and easing of restrictions that took place in the United Kingdom.
From March 2022, all restrictions including the legal obligation to test, and self-isolate were removed as part of the UK Government’s plans to “live with” COVID-19, 18 an approach which has since been replicated worldwide. This decision was contentious, as there can be no doubt that sustained transmissions, future variants of concern and the disabling impacts of post-COVID-19 syndrome, or long COVID, continue to affect public and global health and well-being and will likely do so for years to come. 19 Although clinical services have somewhat been restored, the aftermath of the pandemic is still being felt, including a backlog of patients requiring routine procedures coupled with over 10 million patients with undiagnosed or untreated health needs that occurred during the pandemic. 19,Reference Bagenal20 Confounded by prior years of investment cuts, Reference Filip, Gheorghita Puscaselu and Anchidin-Norocel21 the COVID-19 pandemic left the UK National Health Service (NHS) and other global health-care systems inadequately prepared to address this unforeseen and global threat to public health, which likely indirectly contributed to adverse patient outcomes and mortality.
Clinical manifestation and features of acute COVID-19 presentation, including pathophysiology, diagnosis, and symptom profiling have been extensively investigated to inform the response to treatment and intervention strategies. Reference Missel, Bernild and Christensen22,Reference Rofail, McGale and Podolanczuk23 However, research that captures the lived experience during the acute phase of COVID-19 infection, and more broadly the pandemic, is limited. Existing literature explores the lived experience of hospitalized patients with COVID-19 Reference Venturas, Prats and Querol24,Reference Liu and Liu25 ; however, the voices of those not hospitalized are yet to be heard. One study by Missel and colleagues Reference Missel, Bernild and Christensen22 explored the lived experience of 5 hospitalized and 10 not hospitalized individuals, with a confirmed diagnosis of COVID-19 during the first phase of the pandemic. The aforementioned study identified 3 themes relating to the meaning of COVID-19 from the participants’ perspective: COVID-19 as (1) a threat to existence; (2) a threat to bodily perception; and (3) an interference in ordinary social relationships. Importantly, participants shared their feelings of threat from the novel virus, about existential thoughts and death. Due to the inaccessibility and limitations of testing methods throughout the pandemic, the important voice of those who were unable to or did not receive a confirmed COVID-19 diagnosis has not been heard. The need to document and understand the lived experience of patients is pivotal to increasing holistic preparedness for future health pandemics. Accordingly, the current study aimed to explore the lived experience during the acute phase of COVID-19 infection during the pandemic, such as testing, diagnosis, clinical status, and care, including individuals who did not receive a confirmed diagnosis.
Methods
Following institutional ethics approval from the College of Science and Engineering Research Ethics Committee (ETH2021-4335), an online Web-based survey (with collection of informed consent) was distributed between October 2021 and January 2022 by means of social media, word-of-mouth, and Patient and Public Involvement and Engagement (PPIE) networks. Participant inclusion criteria included testing positive or suspecting COVID-19, understanding written English, and being >18 y old. Participants were invited to leave an email address to be contacted for future research, but responses were anonymized using unique identification codes.
The survey consisted of 6 sections, including 65 questions in the areas of acute and long COVID. This study focuses on 16 questions (open and closed) across 3 sections that relate to the experience of COVID-19 in the acute phase of infection (testing, diagnosis, and clinical status [hospital admission, management of condition, impact of testing on treatment]), and adequacy of care. The full survey is available in the Supplementary Material.
Patient and Public Involvement
PPIE was used throughout the research process including developing the research question, and during the creation and design of the survey. The PPIE network and research team developed the questionnaire using a roundtable approach, with PPIE representatives reviewing the survey to determine survey length, content, terminology, and format before distribution. PPIE representatives supported the circulation of the survey by sharing it within their long COVID networks. The PPIE network are established partners of the long COVID research group and long COVID physiotherapy network, external from the University of Derby.
Data Analysis
Closed-ended questions were analyzed according to frequency counts and percentages. Braun and Clarke’s reflexive thematic analysis framework Reference Braun and Clarke26 was used to adopt an inductive, data-driven approach. Open responses were uploaded to NVivo 12 pro (Version 12.7 QSR International, Doncaster, Australia) where following familiarization of the data, initial codes were generated, and data were organized into groups. Codes were analyzed, and initial themes were identified. The themes were then reviewed by the research team and defined. Word frequency was also analyzed in NVivo 12 pro, identifying the most frequently occurring words within open responses throughout the survey, and is presented as % followed by “count”.
Results
One hundred thirty-two responses were used for analysis, with 85.6% female, 32.6% of participants aged 18-40 y, 65.9% aged 41-65 y, and 1.5% >65 y. Within the sample, 77.3% of participants were white British, 12.9% from other white backgrounds, 5.3% white Irish, and 0.8% mixed white and black Caribbean, other Black, African, or Caribbean backgrounds, Indian, Pakistani, Bangladeshi, or other mixed or multiple ethnic backgrounds. Furthermore, 16.7% had a pre-existing auto-immune condition, and 14.4% reported being registered with a disability.
Within the sample, 59.1% (n = 78) had COVID-19 confirmed by a positive test, and 40.2% (n = 53) did not report a positive test but had symptoms consistent with COVID-19 and, therefore, suspected infection. Of those who did not have a positive test, 22% (n = 29) believe that this impacted them receiving medical help. Within the sample, 88% (n = 116) of respondents recovered in a community setting, whereas 9% (n = 12) were admitted to hospital (4.5% [n = 6] <1 wk, 4.5% [n = 6] >1 wk, 4% [n = 5] admitted to an intensive care unit), and 3% (n = 4) did not respond to this question. The median month of participants’ positive test was December 2020, ranging from March 2020 to January 2022.
The thematic analysis resulted in 5 themes and 3 sub-themes throughout the survey relating to the lived experience during the acute phase of COVID-19 infection. Participants described how they managed their condition during their infection, which was often accompanied by a description of the symptoms they were experiencing and any contact with medical support.
Theme 1: Varying Symptom Profiles
Participants in the study reported varying symptom profiles at the acute stage, ranging from mild, to moderate and severe. The term “symptoms” had the highest weighted percentage (1.28%; count 113), followed by covid (1.25%; count 110), pain (1.18%; count 104), and rest (1.13%; count 100). When including stemmed words, the term “breathing” (breath, breathe, breathing) had the highest weighted percentage (1.61%; count 142), followed by “rest” (rest, resting, rested) (1.48%; count 130), and “pains” (pain, painful, pains) (1.45%; count 128). When stemmed, “symptoms” had a weighted percentage of 1.36% (count 120).
The term “mild” had a weighted percentage of 0.16% (count 14), with participants describing:
“Very mild, no fever, no respiratory symptoms”; “very mild initial illness with some fatigue”
Comparatively, the term “severe” had a weighted percentage of 0.48% (word count 42), as well as further descriptions of:
“I thought I died at one point”; “It was so horrific with racing heartbeats, breathlessness that felt like I’d suffocate, pain in my abdomen that felt like I must be dying, fever, hallucinations, GI symptoms of diarrhoea and acid reflux with swelling in abdomen…”.
Theme 2: Management and Treatment of Symptoms
Participants described how they managed their condition regarding symptom severity, which ranged from home management to requiring medical support (calling 111, an ambulance or a general practitioner [GP]) due to the varying symptom profiles. The term “hospital” (stemmed) had a weighted percentage of 0.51% (word count 45), with 111 services having a weighted percentage of 0.40% (word count 35).
Sub-Theme 1: Home Management of Symptoms
Participants with mild-moderate symptom profiles described managing their symptoms independently with the use of over-the-counter medications which predominantly included “painkillers” such as paracetamol (weighted percentage 0.57%, count 50). Other self-management methods were described which included resting, taking time off work, and staying hydrated:
“I took 2 weeks off sick initially and then worked from home but struggled. I slept between meetings. I had lower back pain and tinnitus, my body aches all over. I could barely keep my eyes open sometimes”.
“Lay still. Drink lots of liquid. Rest near an open window. Vitamin D. Raise head of bed.”
In more moderate-severe cases, participants described how their symptoms left them “bedbound” or on “bed rest”. The term “bed” had a weighted percentage of 0.68% (word frequency 60):
“Didn’t leave bed for first 2 days”; “Bed bound for 3 months”.
Additionally, 1 participant described that they felt “completely debilitated”, and another stated that:
“At the height of it I could not get out of bed. If I got up, I struggled to keep upright or walk and got dizzy”.
Sub-Theme 2: Receiving Medical Advice or Treatment
For more moderate-severe-critical cases, participants report requiring medical assistance, and receiving support and intervention from nurses and GPs:
“Regular discussion with asthma nurse by phone”. “Managed by GP who knew me well, medication to help breathing, bring down fever, coughing etc, inhaler for a time, referrals made to specialist departments like ENT.”
Other participants reported receiving advice from 111 and NHS services:
“Had to call ambulance 2 times due to breathing and chest pains. Called 111 due to migraine pains being unbearable”.
“I called 111, and they advised me to come to A&E but I felt too ill and didn’t want to spread it… looked on the NHS website (there was little to no info at the time)…kept warm, took Lemsip, ate and was in an elevated position”.
However, 1 participant reported:
“Hospital full so advised to recover at home and call 111 if oxygen dropped… antibiotics for pneumonia, high dose vitamin C, D, B”.
Theme 3: Receiving Inadequate Support
Although 88% (n = 116) of participants recovered in community settings and 9% (n = 12) were admitted to hospital, 55% (n = 73) of all participants report that they do not believe they received adequate care during the acute phase of infection. Inadequate experiences were described by participants, where they felt they had to “beg” for support. Furthermore, participants felt like they were disbelieved, and/or not taken seriously.
One participant described:
“I felt I had to beg to be seen and felt disbelieved …I felt as though I had been left to die at home despite seeking care. Nobody took over my care medically to look after me… It was some weeks before I saw someone or had any tests, likely more than 6 weeks.”
Similar experiences were described by other participants:
“I feel as though I was not believed. I was struggling to function at home and despite calls to 111 and my GP I could not gain medical help…”
“Sought emergency care but was denied as I could speak a whole sentence and could get myself outside of my front door if needed, although with difficulty and unable to do anything once there”.
“had minimal medical help, 111 did not answer and GPs were overwhelmed”.
Additionally, experiences of being sent home after seeking care were reported:
“Paramedics … tried to take me to hospital but they wouldn’t let me in so they had to take me back home.”
“I called 111… mostly on hold for 3 hours … no help told me to call ‘when you are struggling to breathe or speak’. Next time my husband called them … I was struggling to breathe and speak. After several hours … they directed me to A&E, but — opposite to what they said they would do — did not inform the A&E, who did not expect me. I got sent back from A&E, who told me I had COVID, without help. Back home I passed out, and I can’t remember much of the days afterwards, except that I expected to die and didn’t.”
Negative experiences with GP services were also described:
“Only contact with a GP was when I phoned, seemed little interest in what I was experiencing”; “GP literally hung up on me”; “Struggled to speak to the same GP”.
However, it seemed this was dependent on the GP as 1 participant described:
“GPs did not care about my symptoms despite how much I was struggling and did not examine me… Only when I moved back home was I then seen at a different practice when things were worse and I then received excellent care as well as at A&E.”
Sub-Theme 3: Relying on Family for Medical Support
Due to the lack of care received by health-care services, participants described the importance of relying on family to support them:
“If he (husband) hadn’t been there … don’t think I would have survived. I should not have been left without treatment or care to develop pneumonia and manage that at home without help for weeks”; “Family had to care for me”; “My husband cared for me during this period.”
Theme 4: Severe Struggle and Fear
Throughout the acute phase, participants with severe symptoms made references to death and planning their funeral. The term “struggling” had a weighted percentage of 0.31% (count 27), and “extreme” 0.19%, (count 17):
“I really thought my kids were going to find me dead by morning”; “Decide to relax and accept death gently”; “I thought I was going to die and planned my funeral.”
Participants also described their feelings of fear and being scared:
“Never been as scared in my life and at times felt like I would not make it through”; “I was very scared”.
Theme 5: Novelty of the Virus
Although participants described receiving inadequate support, they also referred to the novelty of the virus, and the potential impact this had on why they may have received insufficient medical care:
“nobody knew what we were dealing with then”; “GPs were overwhelmed”; “I was told I would be safer at home than in hospital”; “They advised me that under normal circumstances they would have taken me to hospital.”
Discussion
To our knowledge, this study is the first to explore the lived experience of individuals with confirmed or suspected COVID-19, during the acute phase of infection. Varying symptom profiles and a lack of knowledge and evidence of effective treatment strategies meant that some patients were left to convalesce in community settings with an apparent lack of access to medical care and support services. It is acknowledged that health services were placed under unprecedented strain at various times throughout the pandemic, which resulted in patients being left feeling stranded and even worrying if they were going to survive. Although the circumstances were unprecedented, this study highlights the perceived inadequacy of management and support when requiring medical assistance and reassurance.
Over half of the participants in this study believed that they did not receive adequate care in the acute phase of infection, with patients being sent home from the hospital and in some cases not being able to be admitted to the hospital due to services being overburdened. Data here provide a novel insight into the patient perspective, which adds a different dimension to the findings that have been published by those working in frontline health-care settings. Reference Eftekhar Ardebili, Naserbakht and Bernstein27,Reference Vindrola-Padros, Andrews and Dowrick28 The sample of the current study is made up of 88% of individuals who were not hospitalized; however, open text responses such as “Hospital full so advised to recover at home”, “Advised that under normal circumstances they would have taken me to hospital” and “I was told I would be safer at home than in hospital” suggest that this may not be because all individuals had mild symptoms, but because medical support was not available due to capacity issues. Although participants referred to the “novelty” of the virus, existing research states that the nature of pandemics makes them unpredictable, and sufficient planning and preparation can support their management. Reference Stenseth, Dharmarajan and Li29 When considering these findings, it is important to be mindful of the pressure on frontline health-care workforces who worked tirelessly out of routine, often with inadequate personal protective equipment (PPE), were commonly redeployed and suffered mentally. Reference Eftekhar Ardebili, Naserbakht and Bernstein27,Reference Vindrola-Padros, Andrews and Dowrick28,Reference Fearnley and Qureshi30 To be clear, the question of preparedness is not solely aimed at health-care organizations and their staff as this must include a whole-systems viewpoint and consider the relevant and necessary stakeholders that are involved in the decision-making relating to planning, funding, and organization.
Furthermore, the Independent Panel for Pandemic Preparedness and Response reported that the global COVID-19 pandemic “was a preventable disaster, with weak links at every point in the chain of preparedness and response”. 31 Specifically, the panel reports that years of warnings highlighting an inevitable pandemic that threatened public health were ignored, and when the Public Health Emergency of International Concern was declared, a “wait and see” approach was widely adopted, compounding the inevitable global health disaster that unfolded. An aggressive containment strategy that may have prevented the global pandemic 31 could have resulted in improved patient outcomes and health-care experiences for all patients. The continued disregard and absence of political leadership had a major impact on the global response to the pandemic, 31 in addition to several other factors contributing specifically to the UK’s response. Reference Faghy, Arena and Hills32,Reference Gaskell, Stoker and Jennings33 These factors include the decision to delay the implementation of lockdown procedures; shortages of PPE for frontline workers; an insufficient number of ventilators; confusion in communications to the general public; and an improper track and trace system, all undoubtedly contributing to the experience described by the participants in this study. Consequently, the UK Government has launched a COVID-19 Public Enquiry, which is ongoing and due to share its findings by 2024.
This is reinforced by public health-related decisions that have seen access to free testing removed despite widespread community transmission which continues to result in hospital admissions. There are also no planned clinical assessments or follow-ups for patients with COVID-19, Reference Goyal, Mansab and Naasan34 which is partly caused by deep and systemic backlogs across the health-care system. As of September 2023, it is estimated that 7.1 million people are waiting for routine treatments from the UK NHS with those living in the most deprived areas adversely impacted by these waiting lists. Reference Morris, Schlepper and Dayan35 Additionally, the lowest level of patient satisfaction with health services in the United Kingdom has been recorded, with 51% of respondents to the Kings Fund survey dissatisfied with their experience and/or treatment. Reference Morris, Schlepper and Dayan35 Furthermore, the strain on staff from responding to the pandemic is alarming and has resulted in greater sickness absences than before the pandemic, 19 as well as ∼110,000 job vacancies across the health-care sector, with thousands more in primary care. Reference Deakin36 Subsequently, only 27% of staff within the health-care services believe that they can do their jobs properly, Reference Deakin36 which is concerning for patients receiving care. This may be represented in the drop in public satisfaction with the health-care service Reference Morris, Schlepper and Dayan35,Reference Wellings, Jefferies and Maguire37 and is further evidenced in our findings. As understood among the participants in the present study, a novel virus allows for a reasonable understanding of restricted access to health care during a pandemic; however, the continuation of the UK’s health-care restrictions is alarming, and unknown future variants Reference Fontanet, Autran and Lina38 and long COVID pose a further threat to the health-care sector.
Infection associated with chronic illness is common following viral/fungal infections where a sub-set of patients develop chronic and persistent symptoms, Reference Islam, Cotler and Jason39,Reference Prasso and Deng40 and this includes persistent symptoms following a COVID-19 infection. In the United Kingdom alone, an estimated 2 million people are living with long-term, disabling, and episodic symptoms that present as a complex clinical manifestation, affecting multiple body systems 41 which broadly impact functional status and quality of life and can persist beyond months postinfection. Reference Faghy, Owen and Thomas3,Reference Faghy, Maden-Wilkinson and Arena42–Reference Owen, Ashton and Skipper46 Although the long-term consequences are outside the scope of the current study, it must be acknowledged that the impacts that have been documented here have the potential to exceed the acute phase of infection and widely impact population health and wellbeing.
Our study highlights the impact on individuals suffering from varying symptom profiles during the early stages of the COVID-19 pandemic and raises alarm about the initial response to the pandemic within the United Kingdom, much of which was mirrored globally. Although this survey took place in the United Kingdom, the relevance of these data and the contextualization in terms of pandemic preparedness and long-term impacts is likely relevant globally. Future pandemics are inevitable and expected to occur more frequently. Reference Haileamlak47 Thus, health services must be able to prepare for well-timed action and mitigation strategies to prevent the catastrophes that have occurred following the outbreak of COVID-19, and to ensure medical intervention and care are available when needed, even in less critical cases. Furthermore, Coccolini and colleagues Reference Coccolini, Cicuttin and Cremonini48 state that resilient health systems must be built as part of pandemic preparedness, to promptly detect, assess, report, and respond to novel outbreaks. Pandemics cannot be controlled by science alone, with management requiring an integrated approach coordinating science, public outreach, and policy-makers to improve the control of public health emergencies. Reference Stenseth, Dharmarajan and Li29
Limitations
Data were obtained from across the United Kingdom, with the survey available only in English, meaning the experiences of those who do not understand English were not shared. The sampling bias of the study should also be considered as 86% of respondents were female and 95% of respondents were white. The disproportionate impact of COVID-19 on African American and Indigenous people, Reference Aldridge, Lewer and Katikireddi49,Reference Vasquez Reyes50 as well as the male gender being a predictor of higher mortality, Reference Nguyen, Chinn and De Ferrante51 reflects a critical need for further research to understand the experience throughout the early stages of the pandemic of these groups. Furthermore, the survey was distributed through social media and established COVID-19 support groups, which further contributed to a non-heterogeneous sample and data set. Although this is characteristic of COVID-19/long COVID research, further attempts must be taken to engage and learn from groups that represent a broader and representative demographic profile, to consider and document the broad challenges that were experienced throughout the pandemic. Finally, the survey also required participants to recall their personal experiences, which may have caused additional challenges due to cognitive impairment that is a key symptom associated with COVID-19 infection.
Conclusions
This study explored the lived experience of patients during the acute phase of COVID-19 infection during the earlier stages of the COVID-19 pandemic. It is apparent that symptoms, severity, and necessary treatment varied substantially among patients now. Since then, the management of acute infection for COVID-19 has been bolstered with knowledge of effective treatment strategies, and there remains further learning that can take place to ensure preparedness for future pandemics and global health threats.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/dmp.2023.197



