Antibiotic-resistant infections are a serious healthcare concern in the United States; they cause an estimated 2.8 million infections and 35,000 death each year. 1 Two of the most concerning organisms are carbapenem-resistant Enterobacterales (CRE) and multidrug-resistant Pseudomonas aeruginosa (MDRPA). 1 CRE is classified as an urgent threat by the Centers for Disease Control and Prevention (CDC) 1 ; it infects ∼13,000 people annually with an 8% mortality rate. MDRPA is defined as a serious threat by the CDC; it causes >32,000 infections each year, of which ∼2,700 are fatal. 1 Common antibiotic treatments for these infections have historically involved the use of carbapenems, aminoglycosides, and colistin. Reference Nørgaard, Jensen, Aalestrup, Vandenbroucke-Grauls, de Boer and Pedersen2,Reference Sheu, Chang, Lin, Chen and Hsueh3 However, the growing concern for antibiotic resistance, as well as treatment-limiting side effects, has led to the development of new combination antibiotics with either cephalosporins or carbapenems and a β-lactamase inhibitor.
Ceftolozane/tazobactam (C/T), is a combination fourth-generation cephalosporin and β-lactamase inhibitor that was approved for use by the FDA in 2014. Reference Motsch, Murta de Oliveira and Stus4 C/T is primarily used for the treatment of MDRPA, but this combination can also be used to treat infections caused by extended-spectrum β-lactamase (ESBL)–producing organisms. Reference Lagacé-Wiens, Walkty and Karlowsky5,Reference Escolà-Vergé, Pigrau and Almirante6 Ceftazidime/avibactam (C/A), a combination third-generation cephalosporin and a novel β-lactamase inhibitor, was approved for use in 2015. C/A is primarily used for the treatment of CRE but is also used to treat infections caused by other multidrug-resistant gram-negative organisms (MDRGNOs). Reference Lagacé-Wiens, Walkty and Karlowsky5,Reference van Duin and Bonomo7 Meropenem/vaborbactam (M/V) and imipenem/relebactam (I/R) both combine a carbapenem with a novel β-lactamase inhibitor effective against Klebsiella pneumoniae carbapenemase (KPC)–producing Enterobacterales. They received FDA approval in 20188,9 and 2019, Reference Campanella and Gallagher10 respectively.
All of these new combination antibiotics are used to treat infections from several different sources including, but not limited to, complicated intra-abdominal and complicated urinary tract infections (c-IAI and c-UTI) and hospital- or ventilator-associated bacterial pneumonia (H/VABP). Reference Sheu, Chang, Lin, Chen and Hsueh3,Reference Goodlet, Nicolau and Nailor11 Clinical trials have individually shown that these medications are not inferior to standard therapies. Reference Motsch, Murta de Oliveira and Stus4,Reference Ackley, Roshdy and Meredith12,Reference Solomkin, Hershberger and Miller13 However, a pooled analysis and comparison of the effectiveness of all these newer medications combined has not been conducted previously. Furthermore, the clinical trials that were conducted focused primarily on the treatment of infections from the same source and did not focus on the use of these drugs in patients with MDR infections. The goal of this study was to determine the effectiveness of these new combination antibiotics, with a particular focus on effectiveness in patients infected with CRE and MDRPA.
Methods
Article search
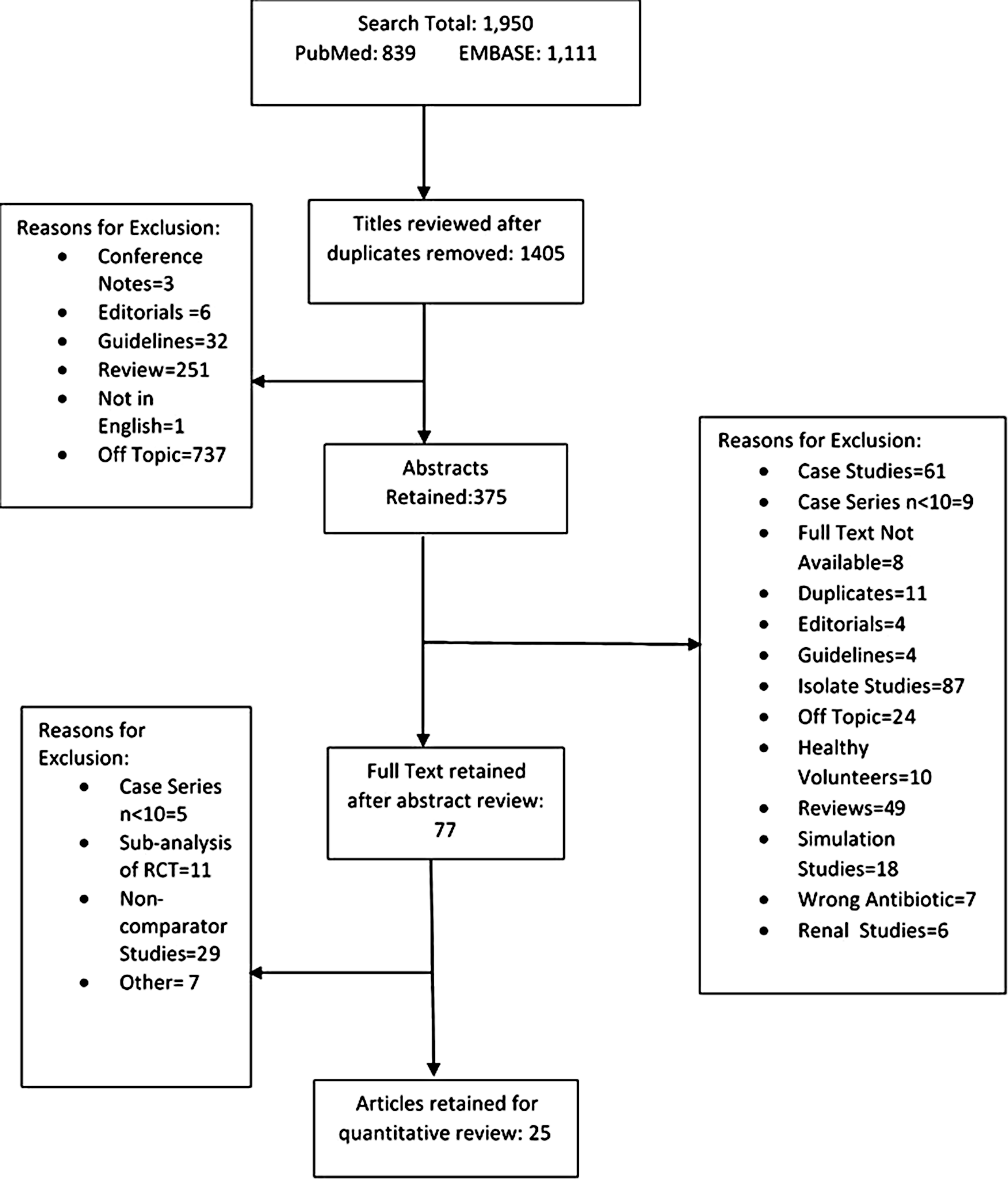
This systematic review was conducted using the Meta-analysis of Observational Studies in Epidemiology (MOOSE) criteria. Reference Stroup, Berlin and Morton14 PubMed and EMBASE were searched from January 1, 2012, through September 2, 2020, for studies that detailed the use of C/T, C/A, M/V, or I/R for the treatment of gram-negative infections. The following search terms were used to search both databases: “relebactam/tazobactam,” “ceftazidime/avibactam,” “imipenem/relebactam,” “meropenem/vaborbactam,” “cephalosporin/beta-lactamase inhibitor,” “Pseudomonas aeruginosa,” “ESBL organisms,” “multi-center study,” “beta-lactam,” “observational study,” “randomized control trial,” and “retrospective study.” The following study types were excluded: in vitro studies, non-English studies, animal studies, case studies, studies that did not evaluate either C/T, C/A, M/V or I/R, and studies that did not report a clinical success rate. Researchers G.W., K.W., and M.F. evaluated the studies for inclusion.
Data abstraction and quality assessment
Researchers G.W., K.W., and M.F. all independently abstracted data from the included studies. The following information was collected from each article: patient demographics and medical comorbidities, infection characteristics, clinical and microbiological outcomes, adverse events, and mortality.
Observational studies were quality assessed using the Risk Of Bias for Non-randomized Studies of Intervention (ROBINS-I) tool Reference Sterne, Hernán and Reeves15 developed by the Cochrane Collaboration. Randomized control trials (RCTs) were evaluated using the companion tool Revised Cochrane Risk-of-Bias tool for randomized trials (RoB-2). Reference Sterne, Savović and Page16 Studies were evaluated regarding the following domains: confounding, selection and randomization, intervention, missing data, outcomes, and reporting bias. Studies with a score of moderate risk of bias in 3 domains or high risk of bias in 1 domain were considered to have an overall moderate risk of bias. Those with a score of moderate in ≥4 domains or high in 2 or more domains were considered to have an overall high risk of bias. The confounding domain was not included on the RoB-2, so the RCTs were not scored on this topic.
Outcome definitions
Clinical success was defined according to the definition provided by the study and was similarly defined across studies. Microbiological success was defined as a negative result from a culture that was taken from the site of infection at the conclusion of the antibiotic treatment for all infection sites except c-UTI. For c-UTI, microbiological success was defined as a bacterial concentration <104 colony-forming units (CFU)/mL present in follow-up urine culture. Clinical success was evaluated by study type, sample size, quality, infection source, and study drug. A subanalysis of studies in which most of the study population had a multidrug-resistant organism (MDRO) infection was also performed.
Statistical analyses
Pooled analysis was done using the Review Manager 5.3 program developed by the Cochrane Review group. Because of the variability in study design and intervention, random-effects models were generated using Mantel-Haenszel (M-H) weighting. Because consistent adjustments could not be made across all studies, unadjusted point estimates were pooled. The heterogeneity of each pooled comparison was assessed using an I2 value. The overall significance was determined by evaluating the P value for the pooled-effect estimate. For stratified analyses, significant differences between the groups were determined by comparing the pooled-effect estimate of each group via χ Reference Nørgaard, Jensen, Aalestrup, Vandenbroucke-Grauls, de Boer and Pedersen2 analysis. A funnel plot was created for the overall main analysis to determine whether publication bias existed among the included articles. All results were reported as pooled odds ratios (ORs) with 95% confidence intervals (CIs).
Results
In total, 1,950 articles were retrieved using our search terms: 839 from PubMed and 1,111 from EMBASE (Fig. 1). After applying the inclusion and exclusion criteria, 25 studies were retained: 17 randomized control trials Reference Motsch, Murta de Oliveira and Stus4,Reference Solomkin, Hershberger and Miller13,Reference Bradley, Broadhurst and Cheng17–Reference Wunderink, Giamarellos-Bourboulis and Rahav31 and 8 observational studies. Reference Ackley, Roshdy and Meredith12,Reference Castón, Lacort-Peralta and Martín-Dávila32–Reference Vena, Giacobbe, Mussini, Cattelan and Bassetti38 The duration of the randomized control trials was significantly shorter than the observational studies, with an average time of 23.0 months compared to 49.6 months (Table 1). C/A was the most evaluated antibiotic combination (11 studies), followed by C/T (7 studies), I/R (4 studies), and M/V (3 studies). The observational studies included were mostly based in the United States (5 of 8 studies) as opposed to the RCTs, which were all global with 1 exception. Carbapenems (primarily meropenem) were the most common comparison antibiotic (64% of studies), followed by colistin/polymyxins (32%) and aminoglycosides (20%). All of the observational studies primarily included patients with MDRO infections as opposed to the RCTs, in which infection source was emphasized over organism susceptibility. The primary organisms reported were Klebsiella pneumonia, Escherichia coli, Enterobacter spp, and Pseudomonas aeruginosa. Some studies did report the percentage of isolates that were nonsusceptible to the study drug, but because it was unclear whether these isolates met the criteria to be considered CRE or MDRPA, they were not included in the subanalyses. Patient comorbidities were not widely reported in the RCTs. Among the observational studies, the most frequently reported comorbidities across all studies were type 2 diabetes (29.6%), cancer (16.9%), and kidney disease (16.5%) (Table 2).

Fig. 1. Search diagram for included studies.
Table 1. Demographic Information for Included Studies

Note. RCT, randomized control trial.
Table 2. Clinical Features of Included Studies

Note. c-IAI, complicated intra-abdominal infection; c-UTI, complicated urinary tract infection; NR, not reported.
a Percentage of study population with drug resistant infection.
b Observational study.
c Carbapenem-resistant Enterobacteriaceae.
d Multidrug-resistant Pseudomonas aeruginosa.
The pooled effect of the new combination antibiotics was not inferior to older therapies for the main outcome of clinical success (pooled OR, 1.21; 95% CI, 0.96–1.51; P = .11). We detected a moderate level of heterogeneity among the included studies (I2 = 56%) (Fig. 2). The funnel plot did not show evidence of publication bias (Fig. 3). Also, 12 studies evaluated the secondary outcome of microbiological success. Among these studies, we detected increased odds of microbiologic success associated with the use of the new combination therapies (pooled OR, 1.27; 95% CI, 1.04–1.56; P = .02) (Table 3). We detected less heterogeneity in this comparison (I2 = 35%). When comparing results for the 8 observational studies to the 17 RCTs, the new combination antibiotics were associated with significantly greater odds of clinical success in the observational studies (pooled OR, 2.56; 95% CI, 1.43–4.58; P = .04), whereas we detected no significant association in the RCTs (pooled OR, 0.98; 95% CI, 0.82–1.17; P = .15).

Fig. 2. Pooled analysis of clinical success in all included studies. (A) Pooled analysis of all randomized control trials. (B) Pooled analysis of all observational studies.

Fig. 3. Funnel plot for all included studies.
Table 3. Stratified and Subanalyses of the Pooled Odds of Clinical Success

Note. CI, confidence interval; RCT, randomized control trial. C/A, ceftazidime/avibactam; C/T, ceftolozane/tazobactam; MDRPA, multidrug-resistant Pseudomonas aeruginosa; CRE, carbapenem-resistant Enterobacterales.
Moreover, 11 studies (3 RCTs and 8 observational studies) primarily enrolled patients with either MDRPA or CRE. The pooled odds ratio for clinical success among the 3 MDRPA/CRE RCTs showed a stronger association compared to the overall RCT result (pooled OR, 1.48; 95% CI, 0.61–3.63; P = .39); however, it was not statistically significant. We detected moderate heterogeneity in this subanalysis (I2 = 40%), and 1 large RCT accounted for 49.7% of the comparison. Among these 11 studies, 6 studies enrolled patients with MDRPA, 4 studies included a CRE study population, and 1 study enrolled patients with both infections (Table 3). We detected a stronger association between the new combination antibiotic and clinical success in the MDRPA studies (pooled OR, 2.22; 95% CI, 1.45–3.39; P = .0002) compared to the CRE studies (pooled OR, 3.14; 95% CI, 0.93–10.57; P = .06). C/T and C/A were each evaluated in 4 studies, M/V was studied in 2 studies, and I/R was evaluated in 1 study. A stratified subanalysis of the 4 studies of C/A versus C/T revealed that both antibiotic combinations were strongly associated with clinical success: C/A pooled OR of 3.53 (95% CI, 1.06–11.73; P = .04) versus C/T pooled OR of 2.21 (95% CI, 1.40–3.48; P = .0006). We detected significantly more heterogeneity among the C/A studies than the C/T studies: I2 = 71% and 0%, respectively.
The studies included 3 main infection sources: hospital- or ventilator-associated pneumonia (H/VABP), complicated urinary tract infection (c-UTI), and complicated intra-abdominal infection (c-IAI). Studies in which the patient population consisted of a majority of any one of these infection types were included in a stratified analysis. New combination antibiotics were not associated with significantly increased odds of clinical success in H/VABP (pooled OR, 1.40; 95% CI, 0.86–2.26; P = .17); however, they were associated with increased odds of clinical success in c-UTI (pooled OR, 1.31; 95% CI, 1.01–1.71; P = .04). For c-IAIs, the new combination antibiotics were associated with a decreased odds of clinical success compared to the older therapies (pooled OR, 0.74; 95% CI, 0.55–0.99; P = .04). In this comparison, we detected an overall significant difference between the pooled effects of clinical success by infection source (P = .0008) as well as a large amount of heterogeneity (I2 = 79.2%).
A second stratified analysis of each antibiotic (C/A, C/T, I/R, and M/V) was also completed (Table 3). However, we detected no association between any 1 antibiotic and odds of clinical success. We also found no difference between the groups regarding this comparison (P = .79). According to the quality assessment, 19 studies had a low risk of bias compared to 6 with a moderate risk of bias. No studies were considered to have a high risk of bias (Table 4). We detected a stronger association among the studies with a low risk of bias compared to those with a moderate risk of bias: pooled OR of 1.34 (95% CI, 1.03–1.61; P = .03) versus pooled OR of 0.95 (95% CI, 0.59–1.53; P = .85). However, we detected significantly more heterogeneity among those studies with a low risk of bias compared to those with moderate risk: I2 = 66% versus 0%, respectively.
Table 4. Quality Assessment of Included Studies

Note. N/A, not applicable.
a Confound bias domain is not included in the RoB-2 for randomized control studies.
b Domain is labeled as selection bias in the ROBINS-I tool and randomization in the RoB-2.
To determine the effect of study sample size on association, a final stratified analysis was conducted comparing studies with cohorts of >150 patients versus those with <150 patients. We detected a stronger association among those studies with study cohorts of <150 (pooled OR, 1.96; 95% CI, 1.11–3.44; P = .02) compared to larger studies with cohorts of >150 (pooled OR, 1.03; 95% CI, 0.84–1.27; P = .72). The heterogeneity between these 2 groups was comparable: I2 = 49% versus 50% respectively. Among the 25 included studies, 9 measured 28- or 30-day mortality. We detected a protective association between the use of new combination antibiotics and mortality (pooled OR, 0.50; 95% CI, 0.33–0.75; P = .0007) and a low level of heterogeneity among these studies I2 = 23%.
Discussion
In this meta-analysis of 25 studies that evaluated the clinical success of C/A, C/T, I/R, and M/V for the treatment of gram-negative infections, these therapies were not inferior to older standard therapies (pooled OR, 1.21; 95% CI, 0.96–1.51; P = 0.11). In patient populations with CRE and MDPRA infections, the new combination antibiotics proved superior to standard therapies (pooled OR, 2.20; 95% CI, 1.60–3.57; P = .001). These results agree with those of previous studies we have completed. A meta-analysis of 29 studies evaluating C/T, C/A, and M/V, the pooled clinical success rates for those antibiotics was 73.3% (95% CI, 68.9%–77.5%). Reference Wilson, Fitzpatrick and Walding39 However, that analysis did not include studies with a comparator group and therefore could not analyze the performance of the new combination antibiotics compared to older therapies. Reference Wilson, Fitzpatrick and Walding39 Additionally, the clinical effectiveness of I/R was not included in that analysis. A review of MDRGNO bloodstream infections found a decrease in 30-day mortality associated with C/A use. Reference Bassetti, Vena, Sepulcri, Giacobbe and Peghin40 C/A and C/T were associated with an increased odds of clinical success among cancer patients with CRE and MDRPA infections. Reference Criscuolo and Trecarichi41
The 2020 Infectious Diseases Society of America (IDSA) guidelines for the antimicrobial treatment of gram-negative infections Reference Tamma, Aitken, Bonomo, Mathers, van Duin and Clancy42 recommend C/A, I/R, and M/V as preferred treatments for CRE infections. The guidelines also list I/R, C/A, and C/T as preferred treatments for MDRPA infections. The results from our meta-analysis support the use of the new combination antibiotics for CRE and MDRPA infections over older treatments such as carbapenems, for which there is growing incidence of resistance, and polymyxins, for which toxicity can limit treatment. Reference Tamma, Aitken, Bonomo, Mathers, van Duin and Clancy42
Although we detected no statistical association between the new combination antibiotics and clinical success, there was a significant association between the combination antibiotics and microbiological success (pooled OR, 1.27; 95% CI, 1.04–1.56; P = .02). The lack of evaluation for microbiological success in our included studies could be related to the difficulty of retrieving repeat cultures from some body sites (c-IAI and H/VABP). However, 50% of the studies that evaluated microbiologic success were studies evaluating c-UTI in which retrieving a repeat culture was a noninvasive procedure.
Interestingly, we detected a difference in the association between clinical success and infection type. We detected no association between clinical success with the newer antibiotics for H/VABP. However, the newer antibiotics were more effective against c-UTI, whereas the older therapies were more effective against c-IAI. These differences may be driven by infection-related factors. c-IAI infections are more difficult to treat because they are more dependent upon adequate source control and are often polymicrobial, requiring treatment with antimicrobials active against both gram-positive and gram-negative organisms. Reference Bradley, Broadhurst and Cheng17,Reference Mazuski, Gasink and Armstrong23 Further evaluation of these antibiotics for the treatment of c-IAI is needed to determine additional contributing factors to this association. Fewer included studies have focused on H/VABP infections; thus, more clinical trials focused on this infection type may yield a stronger association.
Although there is significant overlap between the types of infections treated by each of these new medications, there are some differences in the organisms targeted by each antibiotic. C/A, M/V, and I/R are recommended for the treatment of CRE infections, whereas C/A, C/T, and I/R are recommended for the treatment of MDRPA. To account for these differences in target organism, a stratified analysis of each study drug was conducted. However, the result showed no differences between the association of any 1 drug with patient outcomes. Finally, we detected a strong association between 28- and 30-day mortality and the use of the newer antibiotics. This association may be driven by studies that focused on the patient populations with MDRO infections because 7 of the 9 included studies in this subanalysis were of patients with resistant infections.
This meta-analysis offers an in-depth review of the new combination antibiotics approved for the treatment of complicated and drug-resistant infections. One strength of this article is the comparative analysis of the performance of these drugs in different patient populations (MDRO and infection source). Another is the evaluation of the results by different study designs. The inclusion of global studies is important because MDRGNO rates differ geographically.
This study also has several limitations. We did not include observational and MDRGNO studies for M/V and I/R. Because these antibiotics were recently approved, significantly fewer studies detailed their effectiveness. A future update may yield more publications focused on M/V or I/R. Additionally, the stronger association observed between the new combination antibiotics and clinical success among the observational studies maybe due to residual confounding in these studies that was not present in the RCTs. More RCTs evaluating these drugs in MDRGNO patient populations are needed to confirm this. RCTs may also have shown less significant clinical success rates due to enrollment of healthier patients who were more likely to survive infections regardless of antibiotic treatment. Lastly, we did not assess the adverse drug events associated with the newer versus older therapies, and this factor could be key. Even though efficacy was not inferior, the safety of the newer therapies could have been superior to older therapies.
In conclusion, this systematic review and meta-analysis showed that the use of new β-lactam/β-lactamase inhibitor combination antibiotics yielded comparable clinical success rates and better microbiologic success rates compared to older standard therapies across multiple infection types. Furthermore, the new combination antibiotics were associated with greater odds of clinical success in studies focused on MDRGNO infections, such as CRE and MDRPA. These results support the most recent IDSA guidelines that recommend these antibiotics as the preferred treatment option for CRE and MDRPA. However, these studies were primarily conducted on C/A and C/T, and more studies are needed to evaluate I/R and M/V in patients infected with MDRGNOs.
Acknowledgments
The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans’ Affairs or the US government.
Financial support
This work was supported by The Department of Veterans’ Affairs, Veterans’ Health Administration, Office of Research and Development, Health Services Research and Development (grant no. IIR 16-028, primary investigator Charlesnika Evans, and grant no. RCS 20-192 to Charlesnika Evans).
Conflicts of interest
All authors report no conflicts of interest relevant to this article.