Introduction
Evidence-based psychological treatments (PTs) are recommended as the first line of treatment for depression and alcohol use disorders (AUD) – two leading causes of global burden of mental disorders for women and men respectively (World Health Organization, Reference Weobong, Weiss, McDaid, Singla, Hollon, Nadarni, Park, Bhat, Katti, Anand, Dimidjian, Araya, King, Vijayakumar, Wilson, Velleman, Fairburn and Patel2015). Worldwide, brief PTs delivered by non-specialist providers (NSPs) have been successful at treating adult depression and AUDs (Van Ginneken et al., Reference Van Ginneken, Tharyan, Lewin, Rao, Meera, Pian, Chandrashekar and Patel2013; Hoeft et al., Reference Hoeft, Fortney, Patel and Unutzer2016; Singla et al., Reference Singla, Kohrt, Murray, Anand, Chorpita and Patel2017). Despite their effectiveness, it remains unclear how these treatments achieve their effects. Identifying temporal pathways of how key treatment and patient variables influence clinical outcomes may illuminate how PTs operate, guiding clinicians, and researchers to predict individual patient trajectories and develop more effective interventions (Cook et al., Reference Cook, Heather and McCambridge2015; Kraemer, Reference Kraemer2016).
The current study explored specific treatment- and patient-level variables that may influence the effectiveness of lay counselor delivered treatments for depression and harmful drinking. Each treatment was the subject of a randomized controlled trial (RCT), delivered in primary care settings in Goa, India. The Healthy Activity Program (HAP) – a brief, culturally adapted version of behavioral activation (BA) treatment for depression (Chowdhary et al., Reference Chowdhary, Anand, Dimidjian, Shinde, Weobong, Balaji, Hollon, Rahman, Wilson, Verdeli, Araya, King, Jordans, Fairburn, Kirkwood and Patel2016) – was found to be more effective than enhanced usual care (EUC) in reducing depressive symptoms and improving remission rates at the primary end-point of 3-months (Patel et al., Reference Patel, Weobong, Weiss, Anand, Bhat, Katti, Dimidjian, Araya, Hollon, King Mm Vijaykumar, Park, McDaid, Wilson, Velleman, Kirkwood and Fairburn2017). Similarly, the Counselling for Alcohol Problems (CAP) Program – a brief, motivational interviewing (MI)-informed PT for harmful drinkers (Nadkarni et al., Reference Nadkarni, Velleman, Dabholkar, Shinde, Bhat, McCambridge, Murthy, Wilson, Weobong and Patel2015) – was found to be more effective than EUC in increasing abstinence and remission rates at 3-months post-enrollment (Nadkarni et al., Reference Nadkarni, Weiss, Weobong, McDaid, Singla, Park, Bhat, Katti, McCambridge, Murthy, Wilson, Kirkwood, Fairburn, Velleman and Patel2017a, Reference Nadkarni, Weobong, Weiss, McCambridge, Bhat, Katti, Murthy, King, McDaid, Park, Wilson, Kirkwood, Fairburn, Velleman and Patelb).
As per Magill et al. (Reference Magill, Gaume, Apodaca, Walthers, Mastroleo, Borsari and Longabaugh2014, Reference Magill, Kiluk, McCrady, Tonigan and Longabaugh2015), we defined treatment variables as treatment processes or counselor skills that predict patient behaviors or long-term effects. Patient behaviors were those enacted by the patient that were potentially associated with the outcomes of interest (i.e. average daily drinking scores and depressive symptoms at 3-months, post enrollment). Fig. 1 shows the study's hypothesized pathways of change in each trial, whereby both treatment-specific and general skills in early sessions would influence the subsequent patient behaviors (patient activation in HAP or change and counterchange talk in CAP) which would, in turn, influence the clinical outcome post-treatment. We also hypothesized that patient behaviors would mediate the effects of therapy quality on clinical outcomes.
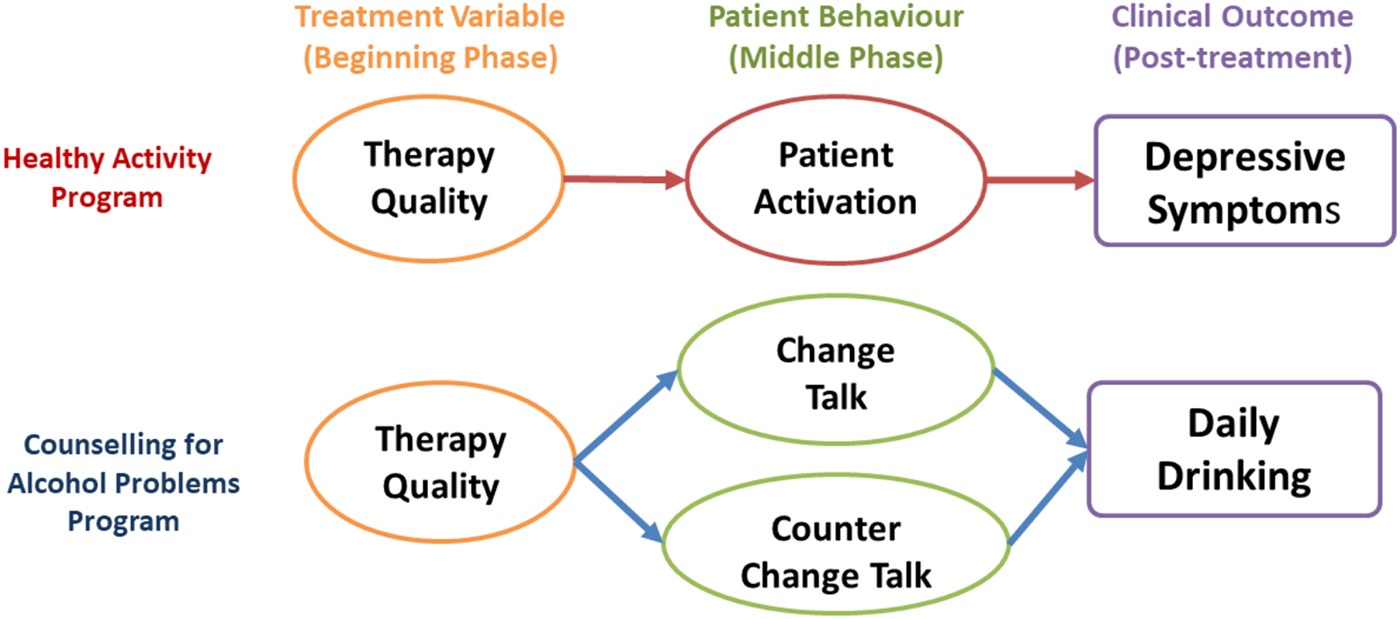
Fig. 1. Hypothesized temporal pathways of change.
Treatment variable
In both HAP and CAP, our treatment variable was therapy quality – the degree to which the counselors have ‘done the right things well’ (Fairburn and Cooper, Reference Fairburn and Cooper2011). Therapy quality included both general skills (e.g. empathy, collaboration, and expressing warmth) and treatment-specific skills (e.g. activity monitoring, scheduling, and homework completion in HAP and avoiding confrontation, providing affirmations and emphasizing personal choice in CAP; Singla et al., Reference Singla, Weobong, Nadkarni, Chowdhary, Shinde, Anand, Fairburn, Dimijdan, Velleman and Weiss2014). In the depression literature, therapist behaviors account for around 5–10% of unexplained variance in patient outcomes and hold in different therapy models and after controlling for confounding patient variables (Kim et al., Reference Kim, Wampold and Bolt2006). Similarly, across the MI literature, growing evidence suggests that high levels of treatment-specific therapy quality (or ‘MI-consistent’ skills) are favorably linked to within-session patient behaviors (Magill et al., Reference Magill, Apodaca, Barnett and Monti2010). A recent RCT demonstrated that higher treatment-specific therapy quality showed better patient outcomes, irrespective of the level of experience of the counselor in treatment delivery (Gaume et al., Reference Gaume, Magill, Longabaugh, Bertholet, Gmel and Daeppen2014a).
Patient behaviors
In HAP, the patient variable specified by theory was patient-reported activation (patient activation). Patient activation levels have been found to mediate the effects of BA treatments on depression outcomes (Gaynor and Harris, Reference Gaynor and Harris2008), including the sustained effects seen in the larger HAP effectiveness trial (Weobong et al., Reference Weobong, Weiss, McDaid, Singla, Hollon, Nadarni, Park, Bhat, Katti, Anand, Dimidjian, Araya, King, Vijayakumar, Wilson, Velleman, Fairburn and Patel2017); but no study to date has examined the potential relations between patient activation, therapy quality and depression outcomes.
In CAP, patient behaviors were change talk and counter-change talk. Both theory and research suggest a positive relationship between MI-consistent skills and patient change talk (Miller and Rose, Reference Miller and Rose2009), and a negative relationship between MI-consistent skills and patient counter-change talk (Moyers et al., Reference Moyers, Martin, Houck, Christopher and Tonigan2009; Gaume et al., Reference Gaume, McCambridge, Bertholet and Daeppen2014b; Magill et al., Reference Magill, Gaume, Apodaca, Walthers, Mastroleo, Borsari and Longabaugh2014; Pace et al., Reference Pace, Dembe, Soma, Baldwin, Atkins and Imelz2017). There is inconclusive evidence about whether patient change talk mediates the effects of therapy quality on patient drinking outcomes (Barnett et al., Reference Barnett, Moyers, Sussman, Smith, Rohrbach, Sun and Spruijt-Metz2014). A recent meta-analysis showed that general skills (e.g. empathy, collaboration) among therapists were related to increased treatment-specific skills and to increased patient change talk but not to patient clinical outcomes (Pace et al., Reference Pace, Dembe, Soma, Baldwin, Atkins and Imelz2017).
In the current study, and in order to better understand the effectiveness of HAP and CAP treatments, we explored the potentially predictive and mediating roles of treatment and patient behaviors on depression and drinking outcomes at 3-months post-enrollment. Our research questions were:
(1) Does therapy quality (general and treatment-specific skills) predict patient behaviors (patient activation in HAP and change and counter-change talk in CAP) and clinical outcomes (depression severity in HAP and daily alcohol consumption in CAP)?
(2) Do patient behaviors predict clinical outcomes?
(3) Do patient behaviors mediate the effects of therapy quality on clinical outcomes?
Methods
Setting
This secondary analysis was conducted within the context of PREMIUM (PRogram for Effective Mental health Interventions in Under-resourced health systeMs), a research program designed to develop and evaluate brief, contextually appropriate PTs for lay counsellor delivery in primary care in Goa, India (Patel et al., Reference Patel, Weobong, Nadkarni, Weiss, Anand, Naiks, Bhat, Pereira, Araya, Dimidjian, Hollon, King, McCambridge, McDaid, Pratima, Velleman, Fairburn and Kirkwood2014). Both the HAP and CAP trials were conducted concurrently (with the two treatments being delivered by the same counselors) in 10 primary health centers. HAP patients were aged 18–65 years, with moderately severe to severe depressive symptoms on the Patient Health Questionnaire (PHQ-9; Spitzer et al., Reference Spitzer, Kroenke and Williams1999). CAP patients were male, aged 18–65 years, who were harmful drinkers, defined as scoring 12–19 on the AUDIT (Saunders et al., Reference Saunders, Aasland, Babor, De La Fuente and Grant1993). Only males were included in the CAP trial because the prevalence of AUDs is low in Indian women (Rathod et al., Reference Rathod, Nadkarni, Bhana and Shidhaye2015). Selection procedures for each trial including inclusion and exclusion criteria, patient characteristics, and outcomes are detailed elsewhere (Nadkarni et al., Reference Nadkarni, Weiss, Weobong, McDaid, Singla, Park, Bhat, Katti, McCambridge, Murthy, Wilson, Kirkwood, Fairburn, Velleman and Patel2017a; Patel et al., Reference Patel, Weobong, Weiss, Anand, Bhat, Katti, Dimidjian, Araya, Hollon, King Mm Vijaykumar, Park, McDaid, Wilson, Velleman, Kirkwood and Fairburn2017). The manuals for both HAP (http://www.sangath.in/wp-content/uploads/2015/08/Healthy%20Activity%20Program_Manual.pdf) and CAP (http://www.sangath.in/wp-content/uploads/2015/08/Counselling%20for%20Alcohol%20Problems_Manual.pdf) and training website (http://premium.nextgenu.org) can be accessed online. Institutional Review Boards at Sangath, the London School of Hygiene and Tropical Medicine, and the Indian Council of Medical Research provided ethical approval.
Procedures
Samples
Two subsamples were randomly selected from the active treatment arm of each trial. Both samples included treatment arm participants only because relevant variables were not collected in the control group of the larger effectiveness trials. Random sampling was used to ensure that the selection of tapes was not biased. Due to the resource-intensive nature of independently rating transcripts, only a subset of the larger group of eligible participants was used in this secondary analysis; however, our methods met the conditions suggested by other mediation studies including a sample size of 40 or more participants, temporally focused relations between mediator and outcome, independent raters of variables of interest, and examined within randomized designs (MacKinnon and Pirlott, Reference Mackinnon and Pirlott2015; Lemmens et al., Reference Lemmens, Muller, Arntz and Huibers2016). A recent review of mediators in psychological treatment trials for depression (Lemmens et al., Reference Lemmens, Muller, Arntz and Huibers2016) recommended 40 or more participants after taking into account both statistical power calculations as well as the average sample sizes in the literature. In HAP, N = 50 participants were randomly selected based on their 3-month remission status (25 remitters and 25 non-remitters, where remission is defined as a PHQ-9 score < 10) from a pool of patients who had received at least two treatment sessions in the middle phase of treatment (sessions 3–5, see below). In CAP, N = 50 participants were randomly selected based on their 3-month remission status (25 remitters and 25 non-remitters where remission is defined as AUDIT score < 8) from a pool of patients who had received at least two treatment sessions (sessions 1 and 2), both of which were of good audio quality. The rationale was two-fold: (a) to include only those patients exposed to sessions in which core HAP and CAP content was delivered; and (b) to assess the temporal relations (Kazdin, Reference Kazdin2007) between therapy quality in the beginning phase (sessions 1–2 in HAP and session 1 in CAP) and patient behaviors in the subsequent session (sessions 3–5 in HAP and session 2 in CAP). No other constraints were applied.
The treatments
Lay counselors with no previous experience in mental health care were trained to deliver both HAP and CAP. Details regarding the selection, training, and supervision of the lay counselors can be found elsewhere (Singla et al., Reference Singla, Weobong, Nadkarni, Chowdhary, Shinde, Anand, Fairburn, Dimijdan, Velleman and Weiss2014).
Health Activity Program (HAP)
HAP was a six–eight session treatment, delivered in three phases (beginning, session 1; middle, sessions 3–5; and end, session 6–8). It is a BA PT (Dimidjian et al., Reference Dimidjian, Barrera, Martell, Munoz and Lewinsohn2011) adapted for the local context (Chowdhary et al., Reference Chowdhary, Anand, Dimidjian, Shinde, Weobong, Balaji, Hollon, Rahman, Wilson, Verdeli, Araya, King, Jordans, Fairburn, Kirkwood and Patel2016). Key strategies include psychoeducation, behavioral assessment, activity monitoring, activity structuring and scheduling, activation of social networks, and problem-solving (Chowdhary et al., Reference Chowdhary, Anand, Dimidjian, Shinde, Weobong, Balaji, Hollon, Rahman, Wilson, Verdeli, Araya, King, Jordans, Fairburn, Kirkwood and Patel2016).
Counseling for alcohol problems (CAP)
CAP is a manualized, MI-informed PT with cognitive-behavioral procedures incorporated. It was delivered in three phases (beginning, middle, and end) and culturally adapted for the local context (Nadkarni et al., Reference Nadkarni, Velleman, Dabholkar, Shinde, Bhat, McCambridge, Murthy, Wilson, Weobong and Patel2015). Key strategies included a detailed assessment with personalized feedback and some psychoeducation (beginning phase), helping the patient to develop problem-solving skills, managing peer pressure, drink refusal and emotional regulation strategies (middle phase), and managing potential relapses by reinforcing key skills (end phase). The therapist's role was to reflect a MI stance while implementing a patient-centered approach to facilitating change that aimed to enhance motivation while simultaneously providing warmth, empathy, and collaboration.
Outcomes
The primary outcome for HAP was depressive symptoms severity scores on the PHQ-9 (Spitzer et al., Reference Spitzer, Kroenke and Williams1999) at 3-months post-enrollment as assessed by independent evaluators who were blind to treatment status. This variable was selected over the trial's other primary outcome of remission status because depressive symptoms offered a continuous score whereas remission was defined as a binary variable (PHQ-9 scores < 10). A continuous score is recommended over binary variables in regression to capture adequate variance (MacKinnon et al., Reference Mackinnon, Lockwood, Brown, Wang and Hoffman2007b).
The primary outcome for CAP was mean daily drinking consumption (measured in grams of ethanol) in the 14 days immediately preceding the 3-month assessment, as assessed by independent evaluators who were blind to treatment status, who calculated this consumption using the timeline follow back method (Sobell and Sobell, Reference Sobell and Sobell1992). Mean daily alcohol consumption was selected as the primary outcome for most of these analyses for two reasons: it is the most widely used outcome in alcohol trials (Bertholet et al., Reference Bertholet, Daeppen, Wietlisbach, Fleming and Burnand2005); and offers a continuous score (MacKinnon et al., Reference Mackinnon, Lockwood, Brown, Wang and Hoffman2007b).
Independent variables
Treatment variable
Therapy quality was assessed by one group of four independent raters using the HAP and CAP Therapy Quality Scale (TQSFootnote †Footnote 1, Singla et al., Reference Singla, Weobong, Nadkarni, Chowdhary, Shinde, Anand, Fairburn, Dimijdan, Velleman and Weiss2014). The instrument consists of two subscales assessing general and treatment-specific skills (elements prescribed for the therapeutic modality of HAP or CAP). The general skills subscale involves 10 items (which are the same for HAP and CAP); the treatment-specific skills subscales involve up to 15 items, (different for HAP and CAP), and based on the phase-specific session being rated. The mean of each subscale (0–4) was used to independently estimate general and treatment-specific skills respectively. To ensure temporal distinction between therapy quality and patient behaviors, therapy quality was assessed using beginning phase audiotapes (session 1 in CAP and session 1 or 2 in HAP) only. Psychometric properties of TQS ratings were established in a previous study which demonstrated good concurrent validity between counselor-based ratings and expert ratings (Singla et al., Reference Singla, Weobong, Nadkarni, Chowdhary, Shinde, Anand, Fairburn, Dimijdan, Velleman and Weiss2014). While we assumed that treatment-specific skills build upon general therapeutic skills, we assessed the two separately to determine whether they uniquely contributed to hypothesized temporal pathways.
Patient behaviors were assessed by a second set of four independent raters who were not involved in the rating of therapy quality.
(1) Patient activation was assessed using the PREMIUM Abbreviated Activation Scale (PAAS), which was based on the Behavioral Activation for Depression Scale (Kanter et al., Reference Kanter, Mulick, Busch, Berlin and Martell2007). This five-item scale assessed to what extent patients reportedly engaged in healthy activities and accomplished their between-session goals, each rated on a scale of 0–5 (hence the overall PAAS scores could range between 0 and 25). Patient activation was assessed during the middle phase (sessions 3–5). Reliability estimates of PAAS ratings across four separate transcripts indicated strong inter-rater reliability during the training phase (ICC = 0.815) and internal consistency (α = 0.885).
(2) Change talk and counter-change talk were assessed using the Motivational Interviewing Skill Code (MISC), version 1.1 (Glynn and Moyers, Reference Glynn and Moyers2012). This measure is an observational coding system that categorizes and quantifies patient change language and gives separate frequency counts of change talk and counter-change talk utterances within the rated session (Glynn and Moyers, Reference Glynn and Moyers2009). We selected the MISC 1.1 because, unlike later versions of the MISC and alternative measures of change-talk (e.g. Motivational Interviewing Treatment Integrity), the MISC assessed our construct of interest (rather than additional therapist behaviors which were captured by the TQS described above), was easy to use, and had shown good predictive validity on relevant clinical outcomes (Lombardi et al., Reference Lombardi, Button and Westra2014). Change talk and counter-change talk were assessed using session 2 (middle phase) audiotapes only. Similar to other studies (Moyers et al., Reference Moyers, Martin, Houck, Christopher and Tonigan2009; Campbell et al., Reference Campbell, Adamson and Carter2010), we calculated separate summed score for change talk and counter-change talk. These four independent raters all received training in the use of the MISC 1.1 over 2 weeks. After three rounds of pilot testing, reliability estimates of MISC ratings across four transcripts among the four independent raters indicated good interrater reliability (ICC = 0.718).
Baseline sample characteristics related to the patient (age, education, marital status, occupation, and PHQ-score) and the counselor or treatment (average session duration, recruitment period) were examined as potential covariates.
Data collection
There were three groups of independent data collectors involved in this study; all assessors were blind to the ratings by other assessors. First, independent interviewers assessed primary outcomes at the 3-month endpoint. These data were recorded using tablets that were uploaded in real-time to a server with data being reviewed by independent data managers. Second, as described above under the Independent variables section, two separate groups of four counselors were all blind to outcome status and each independently assessed either therapy quality or patient behaviors from audiotaped sessions using the TQS, and the PAAS or MISC respectively. Randomly selected ratings were quality checked by expert clinicians. No counselor rated his or her own sessions.
Analyses
All analyses were exploratory, using SAS 9.4 and R-studio. First, means and confidence intervals (CIs) for each variable were estimated. Second, Pearson correlations were used to assess the associations among independent variables. If trend or significant relationships were observed (p < 0.10), variables were added to the regression models (described next) to account for maximum change in average daily alcohol consumption and for any potential confounding variables. Similar to other mediation studies that apply a lower threshold (Hayes, Reference Hayes2015), we defined significance as p < 0.10. Among CAP participants, we used baseline AUDIT scores to account for baseline problem severity (these were significantly related to mean daily alcohol consumption at follow-up, r = 0.217, p = 0.005) because mean daily alcohol consumption amounts were not collected at baseline.
Next, we used multiple linear regression to run models where the dependent variable was 3-month daily alcohol consumption in CAP or depressive symptoms in HAP. In each study sample, our models estimated, whether: (a) treatment-specific or general skills in the beginning phase predicted 3-month clinical outcomes; (b) treatment-specific or general skills predicted subsequent patient behaviors (patient activation in HAP and change or counter-change talk in CAP) in the middle phase; and, (c) middle-phase patient behaviors predicted subsequent 3-month outcomes, while accounting for treatment-specific or general skills. Variance inflation factor (VIF) was assessed for each independent variable within each model to estimate multicollinearity (VIF ⩾ 5).
If mediation conditions were metFootnote 2, we examined whether (respectively) patient activation or change talk and counter-change talk mediated the effects of therapy quality on mean depressive symptoms in HAP or daily drinking outcomes in CAP using the Monte Carlo Method for Assessing Mediation (MCMAM; Selig and Preacher, Reference Selig and Preacher2008). In this approach, a distribution of the indirect effect was used to estimate a CI around the observed value of the indirect effect (MacKinnon et al., Reference Mackinnon, Lockwood and Williams2004). MCMAM performs better than the Sobel test and comparably with bootstrap approaches (MacKinnon et al., Reference Mackinnon, Lockwood, Hoffman, West and Sheets2002; MacKinnon and Pirlott, Reference Mackinnon and Pirlott2015) and no direct effect is required of the independent variable (in this case, therapy quality) on the dependent variable (either depressive symptoms or mean daily alcohol consumption at 3-months; MacKinnon et al., Reference Mackinnon, Fairchild and Fritz2007a). In the current study, we computed a 95% CI with 20 000 repetitions.
Results
Among HAP patients (N = 50), 80.0% were female and the sample had an average age of 44.26 years (95% CI 41.21–47.34). The majority were married (72.0%), Hindu (98.0%), homemakers (66.0%), and had completed a minimum of primary level education (80.0%). The patients had received an average of 6.92 sessions (95% CI 6.65–7.19, range 0–8) that lasted an average of 38.93 min (95% CI 37.03–40.84). Mean PHQ-9 scores of 18.66 (95% CI 17.87–19.45) at baseline decreased to 9.34 (95% CI 6.70–8.57) at 3-months post-enrollment.
The CAP patients (N = 50) were, on average, 44.06 years of age (95% C 41.16–46.96). Most were married (78.0%), Hindu (88.0%), unskilled manual laborers (66%), and had completed a minimum of primary level education (70.0%). Out of a maximum four sessions, these patients had received an average of 3.06 sessions (95% CI 2.84–3.28, range 0–4) that lasted an average of 40.26 min (95% CI 38.5–42.0). At 3-months post-enrollment, their mean daily drinking was 19.96 g ethanol (95% CI 8.25–31.67) of ethanol.
The two subsamples were similar to the larger samples in terms of demographic characteristics (Nadkarni et al., Reference Nadkarni, Weobong, Weiss, McCambridge, Bhat, Katti, Murthy, King, McDaid, Park, Wilson, Kirkwood, Fairburn, Velleman and Patel2017b; Patel et al., Reference Patel, Weobong, Weiss, Anand, Bhat, Katti, Dimidjian, Araya, Hollon, King Mm Vijaykumar, Park, McDaid, Wilson, Velleman, Kirkwood and Fairburn2017).
Therapy quality, patient activation, and depression outcomes
The mean beginning phase treatment-specific and general skills scores were 2.45 (95% CI 2.30–2.61) and 2.71 (95% CI 2.60–2.81) respectively and mean PAAS scores were 13.4 (95% CI 12.41–14.35) out of a maximum score of 25. The correlation analyses indicated significant, positive associations between therapy quality treatment-specific skills and patient activation (r = 0.303, p = 0.034), therapy quality general skills and patient activation (r = 0.346, p = 0.015) as well as a significant negative association between patient activation and PHQ-9 outcome scores (r = −0.458, p = 0.0008). These, in turn, suggest medium effect sizes between independent and dependent variables of interest (Cohen, Reference Cohen1988). Recruitment period, baseline depression and treatment dose also were also significantly related to one or more key variables and were therefore added to the regression models.
Table 1 shows the results of the regression and mediation analyses. Treatment-specific and general therapy quality scores in the beginning phase of treatment did not significantly predict subsequent depression scores at the end of treatment. General skills did significantly predict subsequent middle phase patient activation scores during the course of treatment and these activation scores significantly predicted reduced depression scores. A similar but nonsignificant trend was found for treatment-specific skills and patient-activation scores (p < 0.10). The indirect effect of general skills (but not treatment-specific skills) and patient-reported behavior activation on depression outcomes was significant; therefore, increased patient activation in the middle phase mediated the effects of better general skills in the early phase on improved depression outcomes at 3-months post-enrollment. There was no evidence of multicollinearity between any independent variables in the multiple regression models (VIF < 3).
Table 1. Regression and mediating analyses of mean depressive symptoms at 3-months (N = 50)

a Beta estimates are not standardized.
b Control variables included baseline PHQ-9 scores, health counselor, recruitment period, and where relevant, therapy quality scores.
‡p<0.10. *p<0.05. **p<0.01. ***p<0.001.
Therapy quality, change talk and counter-change talk, and harmful drinking outcomes
The mean treatment-specific and general skills scores were 2.30 (95% CI 2.17–2.43) and 2.45 (95% CI 2.32–2.57) respectively in session 1 and mean frequency counts of change talk and counter-change scores were 16.05 (95% CI 13.92–18.17) and 14.97 (95% CI 12.85–17.11) respectively in session 2. Correlational analyses indicated nonsignificant trend-level or fully significant, associations between treatment-specific skills and patient change talk (r = −0.229, p = 0.095), general skills and counter-change talk (r = −0.229, p = 0.045), as well as a significant negative relation between counter-change-talk (r = 0.364, p = 0.009) and mean daily alcohol consumption outcome (r = 0.525, p = 0.0001). These, in turn, suggest small to large effect sizes between independent and dependent variables of interest (Cohen, Reference Cohen1988). Treatment-specific therapy quality skills were significantly related to general skills (r = 0.866, p < 0.001) whereas session-wise ratings of change and counter-change-talk were not (r = −0.080, p = 0.589). Patient education levels also were significantly related to one or more key variables and, along with baseline AUDIT scores and health counselor, were therefore added to the regression models.
Table 2 and Fig. 2 show the results of the regression and mediation analyses. First, there was a direct association between higher treatment-specific skills and reduced 3-month alcohol consumption at the p < 0.10 level, but not between general skills and reduced 3-month alcohol consumption. Second, at non-significant levels, higher treatment-specific skills in the beginning phase of treatment were associated with increased change talk and reduced counter-change talk in the middle phase. We also found a significant relationship between higher general skills in the early phase and increased change talk in the middle phase, and a nonsignificant relation between general skills and counter-change talk in the middle phase. Third, lower counter-change talk, but not change-talk, significantly predicted reduced mean alcohol consumption at 3-months. Finally, the indirect effect of general therapy quality skills and counter-change talk on reduced drinking was significant, thus suggesting that lower counter-change talk mediated the effect of higher general skills on reduced harmful drinking at 3-months. There was no evidence of multicollinearity between any independent variables in any of the multiple regression models (VIF < 2).
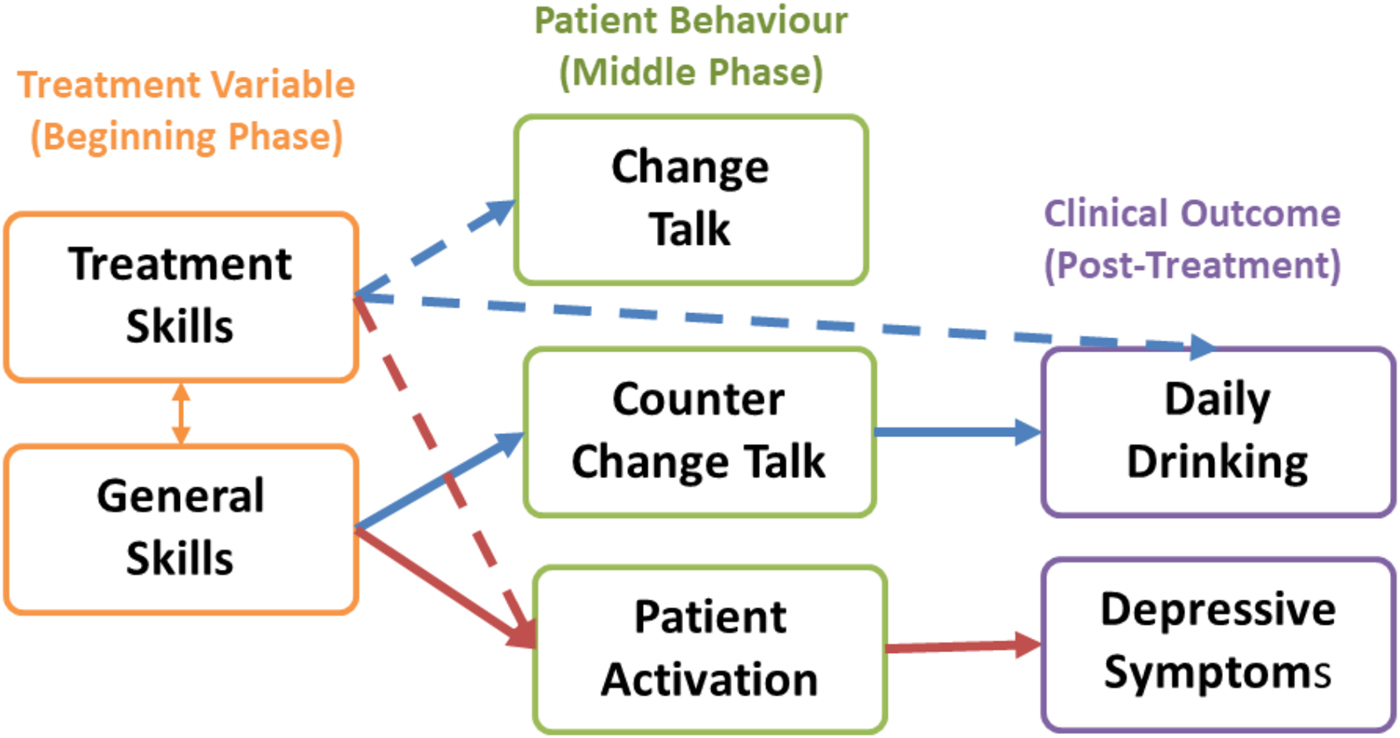
Fig. 2. Predictive and mediating roles of therapy quality, patient behaviors, and clinical outcomes for depression and harmful drinking.
Table 2. Regression and mediating analyses of mean daily alcohol consumption at 3-months (N = 50)

a Beta estimates are not standardized.
b Control variables included baseline AUDIT scores, health counselor, and patient educational level, marital status and where relevant, therapy quality subscales.
c Mediation conditions were not met (i.e. no effect of M → Y) and therefore indirect effects were not tested for mediation.
‡p<0.10. *p<0.05. **p<0.01. ***p<0.001.
Discussion
The aim of the current study was to explore the temporal pathway of change within two treatments, one for depression and the other for harmful drinking. The specific aim was to investigate the predictive and mediating roles of therapy quality, both general and specific, and patient behaviors on mean depressive symptoms and average daily alcohol consumption outcomes respectively at 3-months post enrollment.
A temporal pathway for change to reduce depressive symptoms and harmful drinking
In line with our hypotheses, we observed preliminary evidence suggesting a temporal pathway in HAP in which therapy quality in the beginning phase of treatment worked through patient activation in the middle phase to reduce subsequent depressive symptoms. Similarly, we found that the effect of general skills was mediated through decreased counter-change talk to ultimately influence mean drinking outcomes. While MI-consistent behaviors have been linked to both change talk and counter-change talk, few have disentangled treatment-specific skills from general nonspecific skills. These findings are broadly consistent with the theories of change that provide the conceptual basis for each of the treatments (Jacobson et al., Reference Jacobson, Martell and Dimidjian2001 for HAP; Magill et al., Reference Magill, Apodaca, Borsari, Gaume, Hoadley, Gordon, Tonigan and Moyers2018 for CAP).
General skills v. treatment skills
Higher levels of both treatment-specific and general skills were associated with positive effects on outcomes for both depression and harmful alcohol use. For HAP, higher levels of both sets of skills were associated with improved patient-activation levels, although only the effects of general skills on reduced depressive symptoms were mediated by patient activation. Importantly, this relation was significant when considering general skills but only evidenced a nonsignificant effect between treatment-specific and patient activation. These findings, if confirmed, highlight the importance of general common skills in determining the outcome of this PT. Similarly, for CAP, a nonsignificant trend was found between treatment-specific therapy quality skills and reduced harmful drinking. Importantly, only higher levels of general skills were mediated by decreased counter-change talk, and not change talk, in reducing drinking outcomes. These findings suggest that treatment-specific skills are contingent on general skills and that treatment-specific and general skills, while related with one another, are differentially related to both treatment outcome and patient behavior in independent ways.
Counter-change talk v. change talk
The CAP findings highlight the importance of reducing counter-change talk, rather than stimulating change talk (Magill et al., Reference Magill, Gaume, Apodaca, Walthers, Mastroleo, Borsari and Longabaugh2014; Romano and Peters, Reference Romano and Peters2016), which the current analyses suggest ultimately influences patient drinking outcomes. While others have demonstrated the importance of counter-change talk, this has often been alongside change-talk for alcohol (e.g. Moyers et al., Reference Moyers, Martin, Houck, Christopher and Tonigan2009). Our findings are consistent with research from the general psychotherapy and behavior change literature that shows that less counter-change talk in early sessions is a stronger predictor of positive outcomes than more change talk (Lombardi et al., Reference Lombardi, Button and Westra2014). The current findings are also consistent with two recent meta-analytic reviews of MI that found a robust role for counter-change talk but not change talk in relation to behavioral outcomes (Magill et al., Reference Magill, Gaume, Apodaca, Walthers, Mastroleo, Borsari and Longabaugh2014; Pace et al., Reference Pace, Dembe, Soma, Baldwin, Atkins and Imelz2017). As theorized in MI, change talk may operate only under specific conditions, with greater counselor experience and more severe alcohol problems (Gaume et al., Reference Gaume, Bertholet, Faouzi, Gmel and Daeppen2013), both of which were limited in the current study context. For this reason, counter-change talk (aka ‘sustain’ talk) is more consistently related to treatment outcomes than change talk (Magill et al., Reference Magill, Apodaca, Borsari, Gaume, Hoadley, Gordon, Tonigan and Moyers2018).
Limitations and implications
There were three main limitations. First, the sample sizes were small. Independent and larger samples are needed to replicate and extend the current findings. Second, other treatment, therapist, and patient-level variables could have been assessed. For example, we did not measure therapeutic alliance from the patient perspective – a frequently studied phenomenon in the PT literature (Ackerman and Hilsenroth, Reference Ackerman and Hillsenroth2003) – although one that garners mixed results as a potential mediator (e.g. Martin et al., Reference Martin, Garske and Davis2000; Lemmens et al., Reference Lemmens, Muller, Arntz and Huibers2016). In addition, we did not assess how cognitions may have influenced patient activation and outcomes. This has been examined in other trials (Lemmens et al., Reference Lemmens, Galindo-Garre, Arntz, Peeters, Hollon, Derubeis and Huibers2017) and the interplay of cognition and behavioral components may inform how brief PTs work. We also did not examine change or counter-change talk among HAP participants or patient activation among CAP patients. Third, in order to assess temporally distinct relations, we evaluated therapy quality only in the beginning phase of treatment and patient activation only during the middle phase of treatment. However, it is possible that they influenced one another in a reciprocal fashion and their relations over time remains unknown. Future studies need to consider the potential role and timing of multiple treatment and patient variable to expand on the temporal pathway highlighted here.
The main implication of our study is that maximizing therapy quality in early sessions is likely to mobilize patient behaviors that ultimately work to improve clinical outcomes. In HAP, our results support the BA model that highlights the central and mediating role of patient-reported activation in alleviating depressive symptoms. In CAP, our results expand on the temporal pathway model to highlight the central and mediating role of counter-change talk, but not change talk, in reducing daily alcohol consumption. These findings are particularly important when training NSPs in suggesting the role and monitoring of therapy quality on potential mediators to ultimately influence treatment effectiveness.
Acknowledgements
This research was funded by a Wellcome Trust Senior Research Fellowship grant to VP (091834). DRS is supported with a Distinguished Fellowship from the Medical Psychiatry Alliance and Academic Scholars Award from the Department of Psychiatry at the University of Toronto. CGF held a Principal Research Fellowship from the Wellcome Trust (046386). The authors also like to acknowledge the contributions of Professors Robert J. DeRubeis, Zachery Cohen, and David P. MacKinnon for their statistical consultations related to our analyses. Next, we would like to thank the diligent and conscientious efforts of our independent raters: Medha Upadhye, Akila Kalsur, Sunaina Halarnkar, Anishka Kalangutkar, Subhash Pednekar, Arati Girap, Shravani Rangapuri, Pranali Kundaikar, Mamata Gosavi, Prashila Gaonkar, and Lalan Karapurkar. Finally, we thank the patients, communities as well as the generous partnership and support from the Directorate of Health Services of the Government of Goa.
Author contributions
DRS drafted the report, in collaboration with RV, SDH, and VP. DRS, RV, VP, SDH, and BW were responsible for the design of the study, with consultation from AN and CGF. AN and AA were responsible for supervising the independent lay counselor evaluators. AN, BB, MG, and BW were responsible for database design and oversight; DRS, with assistance from BW, was responsible for analyses. All authors contributed to the interpretation of the data. All authors reviewed and approved the manuscript.






