Chronic pain affects between one-third and one-half of the population of the UK (Fayaz et al., Reference Fayaz, Croft, Langford, Donaldson and Jones2016). Chronic musculoskeletal pain, defined as pain arising from muscles, bones, joints or surrounding soft tissues and persisting for more than three to six months (Treede et al., Reference Treede, Rief, Barke, Aziz, Bennett, Benoliel, Cohen, Evers, Finnerup, First and Giamberardino2015), makes up the majority of this burden (Breivik et al., Reference Breivik, Collett, Ventafridda, Cohen and Gallacher2006; Goldberg and McGee, Reference Goldberg and McGee2011; Fayaz et al., Reference Fayaz, Croft, Langford, Donaldson and Jones2016). One in six adults in the UK has a common mental disorder (comprising different types of depression and anxiety) (McManus et al., Reference McManus, Bebbington, Jenkins and Brugha2016).
There is extensive evidence of the reciprocal relationship between chronic musculoskeletal pain and anxiety and/or depression, with the presence and severity of one, impacting the prevalence and trajectory of the other (Ruoff, Reference Ruoff1996; Gambassi, Reference Gambassi2009; Ang et al., Reference Ang, Bair, Damush, Wu, Tu and Kroenke2010; Fujii et al., Reference Fujii, Oka, Katsuhira, Tonosu, Kasahara, Tanaka and Matsudaira2018; Mather et al., Reference Mather, Ropponen, Mittendorfer-Rutz, Narusyte and Svedberg2019). Individually both chronic musculoskeletal pain and mental health disorders are associated with increased rates of cardiovascular disease (Oliveira et al., Reference Oliveira, Maher, Franco, Kamper, Williams, Silva and Pinto2020) and health risk behaviours which can negatively impact future morbidity and mortality, for example, increased smoking, low physical activity and unhealthy alcohol consumption (Scott and Happell, Reference Scott and Happell2011; Van Hecke et al., Reference Van Hecke, Torrance and Smith2013). What is less clear is whether the combination of chronic musculoskeletal pain and anxiety/depression is associated with the excess prevalence of the key health risk behaviours associated with future cardiovascular disease and a range of other causes of morbidity and premature mortality.
Significant focus within primary care goes towards proactively identifying those at higher risk of future disease in order to target preventative advice and treatment, for example, in the UK, NHS Health Checks and opportunistic use of cardiovascular risk scores (National Health Service, 2020). Recent evidence from an evaluation of the NHS Health Check suggests that those with physical disability and those with mental illness do have equitable attendance for these checks (Patel et al., Reference Patel, Barnard, Thompson, Lagord, Clegg, Worrall, Evans, Carter, Flowers, Roberts and Nuttall2020), but this analysis only specifically looked at attendance of those with ‘severe mental illness’, that is, those with schizophrenia, bipolar and other psychotic disorders, not depression and anxiety. Evidence suggests that those with mental illness, in general, are less likely to receive routine checks like blood pressure and cholesterol (Naylor et al., Reference Naylor, Das, Ross, Honeyman, Thompson and Gilburt2016; Mental Health Foundation, 2021), and a lack of motivation, a symptom of mental illness, can serve as a barrier to effective behavioural change, even if health risk behaviours are discussed in primary care (Nordentoft et al., Reference Nordentoft, Krogh, Krogholm, Lange and Moltke2013). In addition, there is some evidence to suggest that traditional lifestyle interventions may not be as effective in those with chronic pain and may need to be more intense or tailored to the individual (Van Hecke et al., Reference Van Hecke, Torrance and Smith2013). Given the high rates of health risk behaviour and potential under-recording of these behaviours in those with mental illness or chronic pain, it is possible that those with both morbidities may have an unrecognised additive or multiplicative prevalence, that is, higher rates of health risk behaviour then would be expected by adding or multiplying the prevalence in those with each isolated morbidity together. Understanding the prevalence in the comorbid group could serve as useful population health intelligence to aid general practice in proactively identifying and targeting health risk behaviours, when consulting with this group, or inviting patients for health checks. An understanding of the burden of health risk behaviours in this group could inform research to better understand how to tailor these interventions to ensure efficacy in this group.
Research aims
-
1. To estimate the prevalence of obesity, smoking, unhealthy alcohol intake and inactivity, in those with comorbid chronic musculoskeletal pain and anxiety/depression and those with either/neither of these morbidities.
-
2. To explore whether any association between lifestyle factors and comorbid chronic musculoskeletal pain and anxiety/depression compared with those with each isolated morbidity is attenuated after adjustment for age, gender, ethnicity, deprivation, employment status and higher education.
-
3. To examine for interaction between chronic musculoskeletal pain and anxiety/depression in the association with risk behaviours (ie, to assess if any association between chronic musculoskeletal pain and anxiety/depression is greater than that expected by adding or multiplying the risks of the two individually).
To explore whether any association between chronic pain, anxiety/depression morbidity/comorbidity and health risk behaviours varied at different stages of adulthood.
Methods
Study design and setting
A cross-sectional survey of the general adult population aged 35 years and over registered with 26 general practices in West Midlands, England. Data were combined from three surveys (PRELIM Pilot, PRELIM Main and HILL) conducted between November 2017 and October 2019, which used similar methods and data collection instruments.
Sampling, recruitment and data collection
This is a secondary analysis of data from three cross-sectional studies which set out to collate data on key patient-reported outcomes and psychosocial vital signs with a focus on common disabling musculoskeletal disorders. Adults over the age of 35 years and continuously registered at 26 participating West Midlands general practices for at least 10 years were selected using either random (PRELIM Main and HILL) or census (PRELIM Pilot) sampling. The derived sample was mailed a pen-and-paper questionnaire. Practices were selected to provide a range of deprivation and socio-economic status in these studies. Paper-and-pen questionnaires were mailed out to sampled patients using Docmail©. The study packs they received contained an invitation letter, the survey, a pre-paid envelope, a participant information leaflet and a contact number for a member of the research team to answer any further questions.
In PRELIM Pilot and Main, non-responders were contacted after two weeks with a duplicate study pack and the opportunity to complete the survey online. A further study pack was sent to non-responders at four weeks with an abridged ‘minimum data collection’ version of the survey. In HILL, non-responders were sent a duplicate pen-and-paper survey at three weeks. In both studies, non-responders at six weeks were presumed to have declined to participate.
Study instruments
The surveys collected data on a wide range of health determinants and outcomes (a description of the full survey instrument can be found at Wilkie et al., Reference Wilkie, Yu, Jordan, Peat, Protheroe, Jinks, Dunn, Mamas, Blackburn, Dent, Judge, Prieto-Alhambra, Silman and Walker-Bone2020 ). The survey content was reviewed by members of Keele University’s Patient and Public Involvement and Engagement Research Users Group (RUG).
Chronic musculoskeletal pain and anxiety/depression
Chronic musculoskeletal pain was assessed using the item, ‘In the past 6 months, how often did you have pain’ (Dahlhamer, Reference Dahlhamer2018) and defined as responding ‘most days’ or ‘every day’, consistent with recent recommendations (Kroenke et al., Reference Kroenke, Krebs, Turk, Von Korff, Bair, Allen, Sandbrink, Cheville, DeBar, Lorenz and Kerns2019). We verified our assumption that this would be predominantly musculoskeletal in origin, by demonstrating that 92.4% of respondents classed as having chronic pain by this definition reported pain that was present for most/every day in the last six months in the back, neck, shoulder, hand/wrist, hip, knee or foot/ankle.
Anxiety and depression symptoms were assessed using the Hospital Anxiety and Depression Score (HADS). We defined the presence of anxiety/depression as a score of 11 or more on either subscale. A threshold of 11 has been used to ensure differentiation of ‘probable’ from ‘possible’ cases of depression or anxiety so that this definition focuses on those most likely to have clinically significant symptoms (Zigmond and Snaith, Reference Zigmond and Snaith1983; Hansson et al., Reference Hansson, Chotai, Nordstöm and Bodlund2009).
Health risk behaviours
Current body mass index (BMI) was assessed by self-reported height and weight, and obesity was defined as BMI ≥30 kg/m2.
Self-reported smoking status was classed as ‘current’ versus ‘never’/’former’ (last smoked over 12 months ago).
Current physical activity was assessed using the General Practice Physical Activity Questionnaire (GPPAQ), a seven-item screening tool designed to assess physical activity in adults in primary care. Respondents were categorised as ‘inactive’, ‘moderately inactive’, ‘moderately active’ or ‘active’. For the current analysis, we dichotomised responses into ‘inactive’/‘moderately inactive’ versus ‘moderately active’/‘active’ (NHS, 2009).
Alcohol consumption was assessed by self-reported number of glasses of wine, pints of beer/cider or 25 ml measures of spirits per week, multiplied by the alcohol unit content. Alcohol intake of >14 units/week was classed as an unhealthy level of consumption (Department of Health and Social Care, 2016).
Covariates
Covariates included:
-
– Patient age (continuous variable)
-
– Gender
-
– Ethnicity (White, Black-Caribbean, Black-African, Black-Other, Indian, Pakistani, Bangladeshi, Chinese, and Other)
-
– Index of Multiple Deprivation (IMD) (Department for Communities and Local Government, 2016), an area-level measure which ranks all neighbourhoods (local super output area, mean population 1500) in England on relative deprivation based on multiple indicators from seven domains – income, employment, education, skills and training, health and disability, crime, barriers to housing and services, and living environment. For analysis, IMD rank associated with respondents’ residential address was categorised by quintile ranks
-
– Employment status, working-age participants (currently in paid employment or self-employed versus other)
-
– Educational attainment (school only versus full-time higher education or university).
Data analysis
All participants who provided complete data on the presence of chronic musculoskeletal pain and anxiety or depression (96%) were included in the current analysis.
Survey respondents were classified into four mutually exclusive categories:
-
Group 1 – Participants without chronic musculoskeletal pain, anxiety or depression
-
Group 2 – Participants with anxiety or depression without chronic musculoskeletal pain
-
Group 3 – Participants with chronic musculoskeletal pain without anxiety or depression
-
Group 4 – Participants with chronic musculoskeletal pain and anxiety or depression comorbidity
The characteristics of each of the four groups were described.
To estimate whether the joint presence of chronic pain and anxiety/depression was associated with the excess prevalence (ie, positive interaction on additive and multiplicative scales) of health risk behaviours after controlling for covariates, we used standardised binomial models (Richardson et al., Reference Richardson, Kinlaw, MacLehose and Cole2015). The excess prevalence on additive and multiplicative scales was assessed after standardising for age, sex, ethnicity (White versus Black, Asian and other ethnicities), deprivation and educational attainment. Additive interaction was assessed using the relative excess risk due to interaction, that is, the absolute excess prevalence in the comorbid group, beyond what we would expect if there was no interaction, reported as a difference in prevalence where prevalence is expressed as a percentage of the population, and multiplicative interaction using the ratio of prevalence ratios, that is, how many times higher the prevalence was in the comorbid group compared with what we would expect if there was no interaction between chronic musculoskeletal pain and anxiety/depression. Exploratory analyses were then performed stratified by age categories (35–49, 50–64 and 65+ years), to explore whether the combination of chronic pain and anxiety/depression varied in association with health risk behaviours at different stages in adulthood. Confidence intervals for standardised estimation were calculated by bootstrapping with 10 000 resampling. All analyses were conducted using SPSS statistics v26 and Stata v14.2.
Results
Study participants
Totally, 14 519 participants (adjusted response rate 37.8%) were included in this analysis (Figure 1). The mean age was 64 (standard deviation (SD) 13) years: 56% were female; 4% were from Black, Asian or other ethnic minority groups; and 16% were living in one of the most deprived quintile areas in the UK. The crude prevalence of chronic musculoskeletal pain was 34% overall and increased with age. The crude prevalence of anxiety/depression was 16%. The crude prevalence of comorbid chronic pain and anxiety/depression was 9% (Figure 2). Of those with chronic pain, 91.7% had pain in >1 musculoskeletal site. The most common sites were back (78.3%), knee (70.4%) and shoulder (60.8%).

Figure 1. Participant flowchart
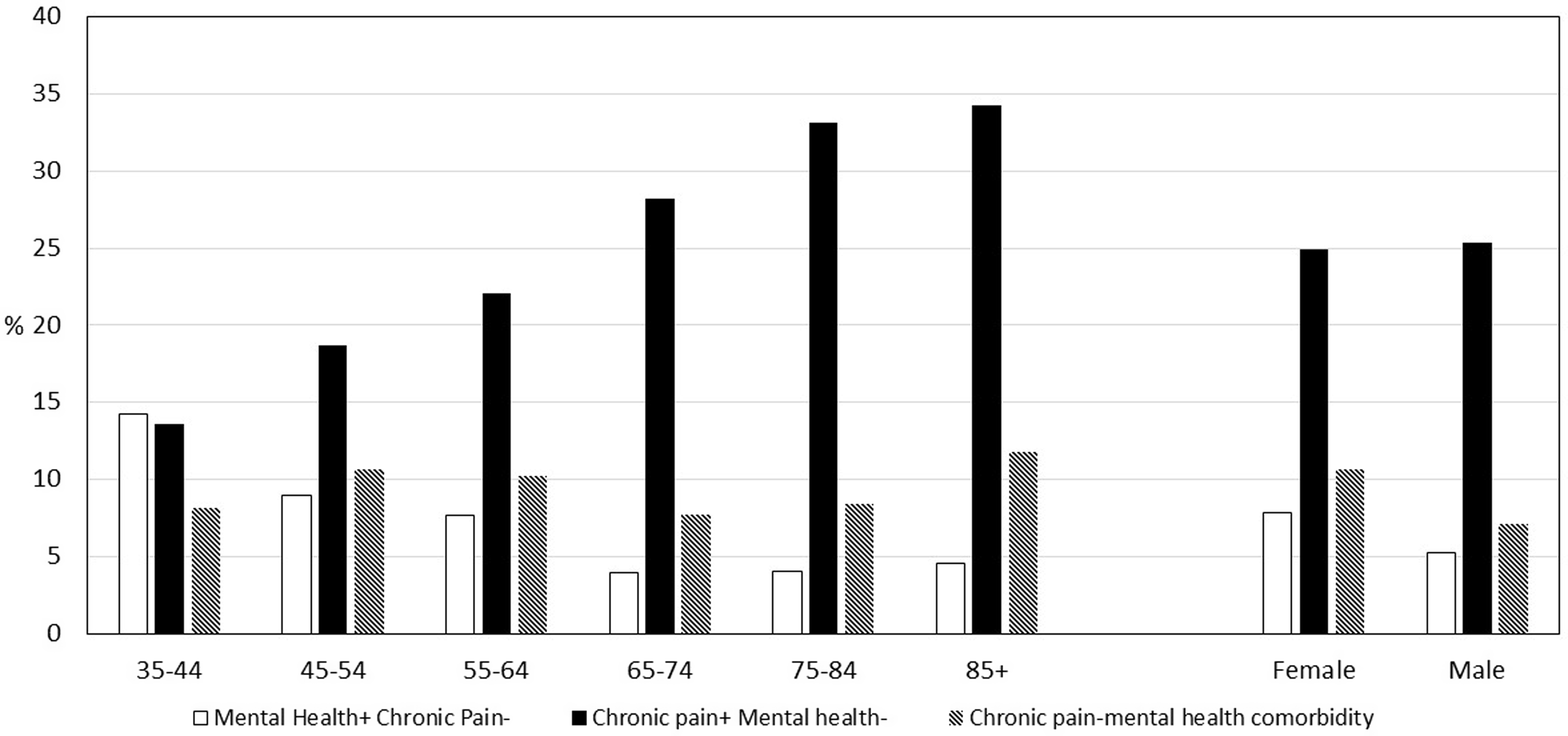
Figure 2. Crude prevalence of comorbid and non-comorbid chronic pain and mental health, by age and sex: West Midlands, 2017–2019
Descriptive characteristics of adults with comorbid chronic musculoskeletal pain and anxiety/depression
Respondents in the comorbid group had the same mean age as those in the group with neither morbidity (63 years), though were slightly younger than those with isolated chronic musculoskeletal pain and older than those with isolated anxiety/depression. Those with comorbidity and isolated anxiety/depression had a higher percentage of female respondents (66%). There was a marked difference in deprivation between the groups, with double the proportion of the comorbid group in the most deprived quintile compared with those in the group with neither morbidity (26% versus 13%) (Table 1).
Table 1. Characteristics of population subgroups of adults aged over 35 years defined by chronic pain and anxiety/depression, West Midlands, 2017–2019

BMI = body mass index; GPPAQ = General Practice Physical Activity Questionnaire.
Health risk behaviours in adults with comorbid chronic musculoskeletal pain and anxiety/depression
Of the four groups, adults with comorbid chronic musculoskeletal pain and anxiety/depression had the highest crude prevalence of obesity (41%), current smoking (16%) and physical inactivity (83%). The crude prevalence of unhealthy alcohol consumption was highest in the group with neither chronic musculoskeletal pain nor anxiety/depression (Table 1).
After standardising to the age, sex, ethnicity, deprivation and educational attainment profile of the respondent population (Supplementary Table 1), those with comorbid chronic musculoskeletal pain and anxiety/depression were almost twice as likely to be obese (39% versus 20%) and to currently smoke (15% versus 8%) than adults with neither chronic musculoskeletal pain nor anxiety/depression [standardised prevalence ratios of 1.93 (95% CI 1.76, 2.10) and 1.86 (1.58, 2.18) respectively]. They were 1.21 (1.17, 1.24) times as likely to be inactive or moderately inactive; however, they were less likely [standardised prevalence ratio of 0.81 (95 CI 0.71, 0.92)] to consume an unhealthy number of alcohol units (Table 2; Supplementary Table 2).
Table 2. Standardised prevalence of health risk behaviours in adults with chronic musculoskeletal pain and anxiety/depression comorbidity compared with adults with neither chronic musculoskeletal pain nor anxiety/depression
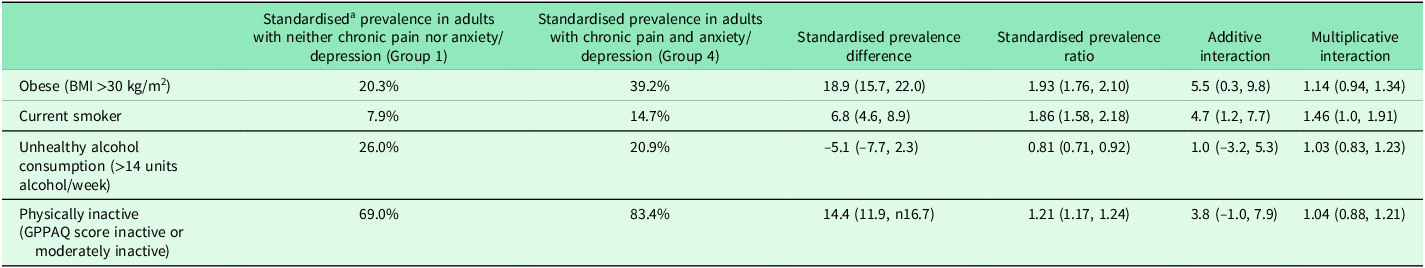
BMI = body mass index; GPPAQ = General Practice Physical Activity Questionnaire.
a Standardised for age, gender, ethnicity, deprivation and higher education.
Additive interaction = relative excess risk due to interaction, for example, interpreted as 5.5% higher prevalence of obesity in adults with comorbid chronic musculoskeletal pain and anxiety/depression than would be expected if there was no interaction between chronic musculoskeletal pain and anxiety/depression.
Multiplicative interaction = rate of prevalence ratios, for example, interpreted as 1.14 times higher prevalence of obesity in adults with comorbid chronic musculoskeletal pain and anxiety/depression than what would be expected if there was no interaction.
There was evidence on the additive scale of the excess prevalence of obesity and smoking and on a multiplicative scale of smoking due to interaction between chronic musculoskeletal pain and anxiety/depression. For example, the prevalence of obesity in adults with the comorbidity was 5.5% (95% CI 0.3, 9.8) higher than expected if there was no interaction between chronic musculoskeletal pain and anxiety/depression, and the relative risk of being a current smoker was 1.46 (95% CI 1.00, 1.91) times higher than would be expected by simply multiplying the risk in those with just anxiety/depression with the risk in those with just chronic musculoskeletal pain. No significant excess risk was seen for unhealthy alcohol consumption or physical activity (Table 2; Supplementary Table 2).
Stratification by age
In our exploratory analysis, the excess prevalence of obesity, smoking and physical inactivity due to interaction between chronic musculoskeletal pain and anxiety/depression appeared to be highest in younger age categories (Supplementary Table 3).
Discussion
Summary of findings
Our cross-sectional study of over 14 500 adults found that respondents with chronic musculoskeletal pain–anxiety/depression comorbidity have significantly higher prevalence of obesity, smoking and, to a lesser extent, physical inactivity than respondents with neither condition. These differences persisted after controlling for differences in age, sex, ethnicity and selected individual- and area-level socio-economic indicators. We found a positive interaction between chronic musculoskeletal pain and anxiety/depression, demonstrating the excess prevalence of obesity and smoking above what would be expected from simply adding the independent risks associated with chronic musculoskeletal pain and anxiety/depression alone. Contrary to expectations, we found no increased likelihood of unhealthy alcohol consumption in adults with comorbid chronic musculoskeletal pain and anxiety/depression.
Study findings in the context of previous literature
This analysis presents new evidence from a large, regional and general population sample of the sociodemographic, pain and health risk characteristics of those with comorbid chronic musculoskeletal pain and anxiety/depression, compared with those without. In the absence of any information on non-responders, we were unable to model the associations for the entire target population. By comparison to survey non-response, missing data among responders on health risk behaviour, covariates, chronic pain and anxiety/depression were low (0%–11.3%), with the exception of missing data for alcohol consumption which was an outlier with 26%. The prevalence of chronic musculoskeletal pain (34%) in this study is comparable with the prevalence estimates in the literature. Fayaz et al. estimated the rates of chronic pain in UK adults to be 35%–51%, based on pooled data from seven studies, though they used a less strict definition of pain for >3 months (not >6 months), and included estimates of chronic widespread and other non-musculoskeletal pain (Fayaz et al., Reference Fayaz, Croft, Langford, Donaldson and Jones2016). The prevalence of depression and/or anxiety in this study (16%) is also comparable with the prevalence estimates in the UK; the Adult Psychiatric Morbidity Survey 2014 estimated one in six UK adults to have a common mental disorder (McManus et al., Reference McManus, Bebbington, Jenkins and Brugha2016). Compared with 2011 Census estimates for the West Midlands, adults from Black, Asian and ethnic minorities were under-represented among survey respondents (4% versus 17%), and so too, but to a lesser extent, were men (41% versus 49%). It is also likely that older age groups are over-represented in this sample, with 50% of participants being over 65 years. However, given increased rates of chronic pain in older age groups, the findings of this study are highly relevant to this age group. Findings have been stratified by age to allow for some exploratory granular analysis of age-specific associations. The impact of lack of representativeness on prevalence estimates and interactions in this study is difficult to predict. However, over-representation of women and those >65 years of aged could have led to higher estimates of obesity and reduced estimates of smoking and alcohol (NHS Digital, 2020).
In self-reported surveys, there is a risk of information/reporting bias, given the subjective nature of data collection; however, there is a particular possibility of under-reporting when asking about risk behaviours, which are potentially stigmatising or clearly associated with negative health impacts (Livingston and Callinan, Reference Livingston and Callinan2015; Norwood et al., Reference Norwood, Hughes and Amico2016). It is possible that there is under-reporting of alcohol consumption, smoking, activity levels and weight, though provided this is not particularly the case for one group within the analysis, the standardised prevalence ratios and differences would still be valid. The most recent government obesity statistics state that 28% of UK adults are obese (Baker, Reference Baker2021), which is comparable to the 23% of participants in this study. Concerningly, the prevalence of obesity in the group with chronic musculoskeletal pain–anxiety/depression comorbidity was much higher at 41%. The prevalence of smoking in this study (9%) is comparable to the known UK prevalence of 14% (Office of National Statistics, 2019) from 2019 data. In the UK, 24% of adults are anticipated to regularly drink >14 units/week (PHE, 2016), which closely aligns with this study population where 23% of participants report drinking over recommended limits. There was no increased likelihood of unhealthy alcohol consumption in the comorbid group in our analysis. This may demonstrate that other unmeasured factors are more highly associated with drinking above recommended limits in this population or that we are seeing some effects of non-random under-reporting of weekly consumption. It is also possible that those with comorbidity are taking medications that may preclude them from unhealthy alcohol consumption. Government data from 2017/2018 estimate that 25% of people aged 16 years+ in England are physically inactive, doing <30 min of moderate-intensity activity a week (Department for Digital, Culture, Media and Sport, 2019). This prevalence is much lower than the 69% of participants in this study classed as inactive or moderately inactive. The most likely reason for this is differences in measurement. Our definition included the moderately inactive group of participants who do <1 h of exercise, so the definition is wider for ‘inactive’ then that is used in gov.uk statistics.
Despite a large number of respondents, numbers available for age-stratified analyses were limited and so must be treated as exploratory. Calculating 95CI for point estimates was time-consuming and computationally intensive and so we omitted this for the exploratory estimates. The suggestion that excess health risk behaviours may be greatest in working-age adults could have important implications for preventative action and should be investigated further in future adequately powered studies.
Implications for research and practice
Our findings indicate that chronic musculoskeletal pain and anxiety/depression comorbidity is associated with a higher prevalence of some cardiovascular health risk behaviours, specifically obesity and smoking, than adults with either or neither. The use of standardised binomial modelling to demonstrate a positive additive/multiplicative interaction between chronic musculoskeletal pain and anxiety/depression helps to highlight this comorbid group as having excess risk, after standardising for potential confounders, and should be a target group for intervention. It is unclear whether the physical health needs of this group are being under-recognised in primary care or missed by routine opportunities to target cardiovascular risk, but evidence suggests that those with mental illness, in general, are less likely to receive routine checks like blood pressure and cholesterol (Naylor et al., Reference Naylor, Das, Ross, Honeyman, Thompson and Gilburt2016; Mental Health Foundation, 2021). This study identified the need to ensure primary care assessment of cardiovascular risk and intervention in the anxious/depressed, particularly when they also have chronic musculoskeletal pain. There may be problems with those with comorbidity accessing, using and benefitting from recommended interventions for obesity reduction and smoking cessation, and more research exploring differential uptake in these services would be useful.
Over the last few years, despite increasing recognition of the importance of preventative medicine, in the context of cardiovascular risk, there has been widespread decommissioning of services directed at reducing risk. For example, between 2014/2015 and 2017/2018, local authority spending on tobacco control and stop smoking services in England fell by 30% (Cancer Research UK and Action on Smoking and Health, 2019). This is a problem when specialist, supervised stop smoking services have some of the best evidence from sustained smoking cessation (Bauld et al., Reference Bauld, Bell, McCullough, Richardson and Greaves2010). This may present a particular disadvantage for adults with comorbid chronic musculoskeletal pain and anxiety/depression, who have a higher likelihood of being a current smoker.
Conclusion
The study highlights an interaction between comorbid chronic musculoskeletal pain and anxiety/depression leading to high and excess prevalence of some health risk behaviours associated with increased cardiovascular risk. This presents not only a public health problem but also a potential target group for opportunistic assessment of health risk in primary care and intervention to reduce future cardiovascular disease. Further research into recognition, recording and management of poor health risk behaviours among adults with chronic pain–mental health comorbidity, and increased understanding of access to, and efficacy of, interventions to reduce cardiovascular risk in this group, could help facilitate important decisions around how primary care and public health initiatives can be targeted in this high-risk group.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S1463423624000070.
Financial support
The authors disclosed receipt of the following financial support for the research, authorship and publication of this article: PRELIM was funded by Versus Arthritis (21403). HILL and PRELIM Pilot were supported by the West Midlands Clinical Research Network. GP, KJ, RW and DY hold Honorary Academic Consultant Contracts from Public Health England. KJ is supported by matched funding awarded to the NIHR Applied Research Collaboration (West Midlands). We are extremely grateful for the input of our public contributors to the study. The interpretation and conclusions contained in this study are those of the authors alone.
The data for this study were from the constituent surveys: HILL, PRELIM Pilot and Main, which have the ethical approval and the approval of the Health Research Authority (IRAS Project number 187604). The PRELIM surveys were funded by a Project Grant from Arthritis Research UK, awarded in the open national competition. The HILL survey was funded with support from the West Midlands Clinical Research Network.
Competing interests
DY, RW, KJ and GP held academic consultant contracts with the Office for Health Improvement and Disparities. The authors do not have any conflicting interests to declare.









