Contaminated surfaces in healthcare settings contribute to the transmission of several pathogens including Clostridioides difficile, gram-negative bacilli, and norovirus. Reference Weber, Anderson and Rutala1–Reference Otter, Yezli and French6 Adequate environmental cleaning is important in preventing transmission of these organisms and in reducing healthcare-associated infections (HAIs). Reference Leas, Sullivan, Han, Pegues, Kaczmarek and Umscheid2,Reference Donskey7 However, effective cleaning practices vary considerably. Reference Mitchell, Farrington and Allen9–Reference Vaughn, Saint and Greene13 Standardized environmental cleaning practices have been developed to improve cleaning efficacy and compliance. 14–Reference Siegel, Rhinehart, Jackson and Chiarello16 Our team identified a need for standardized environmental cleaning practices and cleaning monitoring to improve cleaning compliance and reduce HAIs. Evaluation of daily environmental cleaning and disinfection practices in veterans affairs acute and long-term care facilities. Reference McKinley, Goedken, Balkenende, Clore, Hockett, Bartel, Bradley, Judd, Lyons, Rock, Rubin, Shaughnessy, Reisinger, Perencevich and Safdar17 Despite these tools, environmental management services (EMS) staff still perceive barriers to environmental cleaning, including staffing, having adequate supplies and equipment, as well as education. Reference Maciel, Baraldi and Boszczowski18
The Systems Engineering Initiative for Patient Safety (SEIPS) framework has been used extensively in healthcare to evaluate elements of the work system that can affect processes and outcomes. Reference Carayon, Schoofs Hundt and Karsh19 The SEIPS framework was developed by human-factors engineers to guide the study of work systems, specifically people, organizations, tools and technology, tasks, and the physical environment. The SEIPS framework guided this study; each domain within SEIPS plays a vital role in the complex and often challenging process of environmental cleaning. Reference Boyce, Havill, Lipka, Havil and Rizvani8,Reference Mitchell, Farrington and Allen9 Limited data exist regarding EMS staff perceptions of barriers and facilitators to an effective EMS program,Reference Yanke, Moriarty, Carayon and Safdar20 particularly on the interventions developed to improve their job performance, which largely target EMS staff behavior through training and monitoring. We focused specifically on the “people” domain of SEIPS, particularly EMS staff and supervisors and their experiences and perceptions surrounding environmental cleaning as a first step in describing perceived challenges and ideas to promote an effective environmental services program.
Methods
Setting and participants
As part of a larger study on environmental cleaning practices, we conducted individual semistructured interviews with key stakeholders (ie, EMS staff, nursing, and infection prevention) at 2 mixed, acute-care and long-term care facilities (ie, community living centers) and 1 acute-care facility within the Department of Veterans’ Affairs Healthcare System (VAHCS) from January to June 2019. For this study, we focused on EMS staff interviews only. The study was approved by the VA Central Institutional Review Board (no. CIRB#18-10) and the Research and Development Committee at the Iowa City VAHCS. Informed consent was reviewed with all participants.
Data collection
Prior to conducting the interviews, research coordinators at each of the 3 sites participated in ∼10 hours of didactic training. The training was both skills based (n = 8 hours) and knowledge based (n = 2 hours), ranging from how to conduct qualitative interviews to identification and familiarization with environmental cleaning practices and general knowledge of infectious disease. Trainings were conducted by experts in each of the content areas. In addition, coordinators were assigned a mentor possessing qualitative method and implementation expertise. At the end of the didactic training, research coordinators performed practice interviews with their mentor and, when approved by their mentor, conducted study interviews with participants.
Interview guides were developed by the research team with questions informed by the SEIPS framework and facility environmental cleaning practices (Appendix 1). Interviews were conducted on day shifts during the work week when research coordinators were typically assigned to work and EMS staff availability was greatest. Interviews lasted 48 minutes on average and were audio-recorded using encrypted recorders and transcribed verbatim. One interview was not recorded due to participant refusal; therefore, detailed notes were used in analysis. Data collection stopped when thematic saturation was reached. Reference Guest, Bunce and Johnson21
Data analysis
Transcripts were uploaded into MAXQDA, a qualitative data management and analysis software program (VERBI Software, Berlin, Germany). We conducted a thematic content analysis by first focusing on inductive codes, which were later mapped onto domains of the SEIPS framework (ie, people, environment, organization, tasks, tools). Reference Carayon, Schoofs Hundt and Karsh19,22,23 This process allowed the research team to prioritize EMS staff language and perceptions in the initial analysis, and then examine when and how inductive codes aligned with SEIPS while also highlighting content outside the framework. Our interdisciplinary team included trained social scientists from anthropology (H.S.R. and S.H.S.) and public health (M.K., C.C.G., E.B., and L.M.), including an infection control nurse (L.M.) with experience in environmental cleaning.
Among the transcripts, 64% were coded via group consensus (L.M., C.C.G., S.H.S., and E.B.), a process that involved all team members coding transcripts prior to meetings and the final coding consensus was entered into MAXQDA during group discussion. The remaining 36% were coded by paired members of the analysis team who followed the same process of independently coding transcripts and then meeting to reach consensus and enter final coding in MAXQDA. Paired consensus coding meetings started after the code book was developed. Group and paired consensus meetings continued throughout the analysis period. This process of continuous dialogue increases the validity and reliability of the coding process by refining the content boundaries of codes and improving coding consistency. For paired coding, unresolved questions were brought to the larger group analysis team (L.M., C.C.G., S.H.S., E.B., H.S.R., and M.K.) for resolution.
For this study, we focused on the codes for EMS staff, culture, staffing, value in work, and recommendations, which directly related to EMS staff perceptions and experiences with EMS programs. These codes mapped onto the “people” and “organization” SEIPS domains.
Results
In total, 11 interview sessions were conducted with 13 EMS staff, including supervisors. Participant demographics are shown in Table 1. One of the predominant themes that emerged from the interviews were the challenges EMS staff perceived as hindering their ability to be effective at their jobs. EMS staff we interviewed felt they understood their job requirements and were dedicated to their work; however, they described challenges related to feeling undervalued and staffing issues. They also shared ideas for expanding opportunities for EMS staff and how to integrate EMS staff as valued as members of a comprehensive healthcare team. Additional representative quotations can be found in Table 2.
Table 1. Characteristics of Interviewees
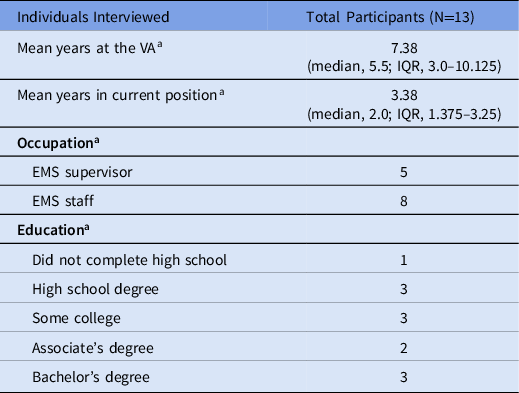
Note. IQR, interquartile range.
a Missing 1 observation.
Table 2. Supplementary Quotations of Key Themes From Semistructured Interviews With EMS Staff

Participants at all sites viewed environmental cleaning as a vital component in HAI prevention.
“(…) Without environmental cleaning, (…) you’re not breaking the chain of infection. Our job is to break that chain of infection and that’s what we teach in our service meeting that the virus or bacteria or pathogen (…), it has to get from a carrier to a receptor (…) our job is to remove that barrier. (…) our primary function is transmission prevention infection control (…).” (EMS supervisor, site B)
“(…) Reinforcing to staff that the criticality of their position and how what they do in their job, how that affects the overall outcome of patient care, so everybody likes to say that housekeeping staff are not a patient care or patient contact workforce, but I don’t know of anyone besides the RNs [who] spend more time with the patients of this facility than the housekeeping staff, and what they do on a day-to-day basis likely does have a direct impact on the outcome of that person’s visit.” (EMS staff, site B)
Despite perceptions that the EMS role is critical for infection control, EMS staff believed their role was undervalued by the broader healthcare team and within the organization.
“I think that housekeepers are undervalued by the general staff (…) because people either sound fake when they’re saying, ‘Oh, you do such a great dah dah dah dah.’ You know? Or they truly believe it and you don’t know which is which. I don’t know that people even pay much attention. I think we kinda blend into the background.” (EMS staff, site B)
“I know that people will tell you, ‘Hey, we couldn’t run this place without you.’ But when you watch actions it’s like I care less whether you [are] here or not.” (EMS staff, site C)
Another EMS staff indicated that if they were to raise concerns regarding cleaning policies and procedures it would “fall on deaf ears” (EMS staff, site B), reenforcing the perception that EMS staff voices are undervalued and unheard.
EMS staff expressed a need to be acknowledged as having a larger role in the healthcare team, especially regarding HAI prevention practices. They also desire to receive higher pay to align with the greater knowledge of infection prevention required in their position compared to cleaning positions outside healthcare.
“(…) Housekeeping is, really should be infection control or the frontline workers for infection control, but we get categorized as the term housekeeping when we’re really trying to save lives. As much as the doctors are curing diseases, we’re trying to prevent the disease from being transmitted (…). That burden (…) fall[s] onto housekeeping, which we [get paid] the same as somebody who work[s] at the 7-Eleven or the one-story motel where there’s no infection control probably even in their thought processes.” (EMS staff, site B)
Staffing issues were also identified as barriers, including high turnover rates and staff shortages leading to challenges in workload and performance.
“Because if they got you running all over the place, well then you won’t be able to do your job. That’s not good--, if I leave my stuff to go [to another assignment] (…) ‘cause we’re short. I’m doing a half-ass job both ways. (…). ‘Cause I’m not getting my stuff done like it should.” (EMS staff, site C)
A supervisor at another site described in detail the overarching issue of turnover within the field of EMS and how it drains resources:
“(…) there’s all the lost productivity and the time and the money and energy of the three of us but then there’s our trainers, there’s the staff (…) in new employee orientation that spent 40 hours. Our trainers spend 80 hours. HR [Human Resources] spends hundreds of hours. We do interviews for hundreds of hours. (…) There’s so much lost productivity. Turnover is so expensive (…) I don’t know if anybody’s calculated how much it costs to turnover one housekeeping aide. (…) On an annual basis, I think I turnover maybe (…) between 40 and 50 housekeepers?” (EMS supervisor, site B)
Further barriers were noted on the allocation of EMS staff time. For example, they are required to dedicate a significant amount of time to noncleaning activities such as completing computer-based trainings or attending in-person meetings. Without protected time to participate in required educational trainings and meetings, these activities can lead to EMS cleaning work being interrupted. This requirement may contribute to feeling undervalued, if EMS are not given adequate time to complete trainings that are essential for their job.
“(…) ‘Cause basically how the eight hours is (…) we on our feet we have a lot of stuff to keep up with. It’s not like we have a desk job where they say, ‘Hey, you take off an hour [Name] and work on your TMS [Talent Management System, VA employees training website].’ So you gotta kinda squeeze this in and we do ‘em in meetings sometimes in the evening.” (EMS staff, site C)
“Trying to figure out a way where I can get all the supervisors sitting down in one room at one time together and that’s a very difficult thing to do when you’re a seven-day-a-week, 24-hour-a-day operation, (…) on rare occasion that I do make that happen, somebody’s gotta get up in the middle of their night and (…) attend a meeting.” (EMS supervisor, site B)
Despite the challenges of meeting the standardized training requirements, EMS staff expressed an interest in additional education and training to expand their knowledge and improve their interactions with patients and families.
“(…) It might be nice if they could find other avenues to train or give us the opportunity, at least, to HAVE other avenues (…) I’ve thought about possibly for people who are working or going to work in community living centers on the hospice side, having some kind of, you know, one or two-day training on hospice and you know, a grief training. (…) just because it makes us more capable of not saying the wrong thing at the wrong time.” (EMS staff, site B)
Participants had additional suggestions on ways to improve perceptions of their value and to boost morale related to expanded opportunities, including incorporating certifications or a reward system. However, both come with challenges within the federal human resources regulations around training and the options for staff rewards.
“(…) We’ve worked towards getting certifications for our housekeepers. There’s [a] program (…) CHEST (…) Certified Healthcare Environmental Services Technician, we wanted to get all of our housekeepers certified with that program. Our training instructor is a certified trainer for that CHEST program, but due to VA regulations (…) because it comes with a certification, the VA won’t pay for that training (…) [CHEST certification] which sets us aside from, we’re not the janitor at the high school or Arby’s or the 7-Eleven. (…) we really want to be seen as Environmental Services Technicians instead of housekeeping in a hotel.” (EMS supervisor, site B)
“So more than 50% of the staff that work in this department [EMS] work either the PM or night shift so their contact and involvement with operation of the facility is small. There’s not a [regular] basis they see their direct supervisors and other than that, they don’t have too much of any contact with hospital management or nursing management (…) once a year the Infection Control Nursing staff come and give them some education (…) the federal system itself just prevents any real opportunity or any meaningful opportunity to reward staff for doing a good job (…) one of the few ways for me to show appreciation to, for my staff is to dig into my own pocket and come up with some, you know, pizza or something like that on an occasion.” (EMS supervisor, site B)
Finally, one EMS program developed its own system to enhance communication and improve opportunities for EMS staff voices to be heard. This was accomplished by making space for EMS employee concerns and incorporating an EMS employee suggestion box.
“At our service meetings. (…) we always open the floor to are there any questions? Are there any comments? Are there any suggestions? We do have a suggestion box.” (EMS supervisor, site B)
Discussion
EMS staff play a critical role in environmental cleaning and HAI prevention in healthcare settings. In our study, EMS staff clearly understood this critical role, but they did not believe it was recognized or valued by the larger healthcare team. It is important to identify and understand work-system barriers and facilitators that EMS staff encounter as emphasized in frameworks such as SEIPS; however, perceptions and satisfaction of individual actors within a system are also important.
Similar to recent environmental cleaning literature, our findings suggest that EMS staff believe that environmental cleaning is an important aspect of infection prevention Reference Mitchell, White and Farrington10,Reference Pedersen, Masroor and Cooper24,Reference Jennings, Sitzlar and Jury25 that affects patient safety. Reference Bernstein, Salsgiver and Simon26 However, we found high turnover, staff shortages, workload pressures, and feelings of undervalue. In 2016, Bernstein et al, Reference Bernstein, Salsgiver and Simon26 also reported challenges in workload and workflow, specifically lack of time to perform cleaning tasks, as well as EMS staff feeling underappreciated by other healthcare workers. Another qualitative study reported that EMS staff attitudes and beliefs about their job may influence their intent to clean, including key themes such as “me versus them” and lack of appreciation. Reference Matlow, Wray and Richardson27 These feelings of exclusion may stem from societal issues—the value, or rather lack of value, society places on the environmental services workforce. In 2021, the findings of Hewage et al Reference Hewage, Cao, Jones and Fraser28 emphasized that EMS staff have low social status. As described in another recent study, “Environmental services is still an occupation that receives little attention in society and carries low occupational prestige in the United States.” Reference Diamond29 This larger issue of how society views EMS staff likely contributes to their feelings of undervalue and lack of appreciation, which also leads to high turnover among EMS staff. Reference Peters, Otter, Moldovan, Parneix, Voss and Pittet30
Our findings highlight EMS interest in receiving certifications, such as CHEST certification or Certified Healthcare Environmental Services Professional (CHESP), which may boost feelings of self-worth and improve how EMS staff are seen by other healthcare workers. 31,32 Furthermore, technician certification can add to knowledge, skills, and abilities required for classifying positions for higher pay grades, which may in turn increase retention. Reference Peters, Otter, Moldovan, Parneix, Voss and Pittet30 EMS suggestions of certifications and ideas to expand their knowledge and communication may be linked to improving EMS job satisfaction and reducing turnover, which could result in more effective EMS outcomes. Furthermore, providing these opportunities and advancements may help change the overarching societal ways in which EMS staff are perceived. Healthcare organizations and leadership should consider incorporating these opportunities to improve EMS job satisfaction and foster culture changes to include EMS staff within the healthcare team.
In our interviews, EMS staff indicated the desire for acknowledgment as having a more significant role within the healthcare team. Collaboration between infection control and prevention teams and EMS has been shown to be associated with improved cleaning practices and reduced rates of antibiotic-resistant organisms. 33–Reference Pyrek35 Van Tiem et al Reference Van Tiem, Friberg, Goedken, Pineles, Reisinger, Morgan and Solimeo36 suggested that infection control and prevention teams may find EMS staff to be allies in identifying opportunities to improve infection control policies.
Our study is not without limitations. First, our study is restricted to EMS staff within the VA Healthcare System. Other non-VA healthcare systems may interact with EMS department staff differently. Second, our sample was a convenience sample restricted to EMS staff involved with environmental cleaning available on days and shifts that coincided with study team availability, and night and weekend shift EMS staff might have differing experiences. Also, overall, the sample consisted of experienced EMS staff with many years of experience. Voluntary response bias may have occurred given that our sample included only volunteers, which could have resulted in only those individuals with strong opinions on environmental cleaning being interviewed. EMS have jobs with limited access to e-mail or a private phone; thus, some staff may be disadvantaged in terms of recruitment to participate. Finally, perceptions and opinions may differ based on power differentials between EMS staff and EMS supervisors; however, we interviewed EMS staff and supervisors separately to reduce the potential for bias by this power differential.
Our qualitative findings suggest the need to create a workspace for EMS staff where they feel like a valued member of the healthcare team. Feelings of undervalue, along with low pay and limited career advancement, often lead to high turnover rates. EMS staff provided ideas for improving feelings of value and job satisfaction, including higher pay, opportunities for certifications and advancement, as well as greater integration within the larger healthcare team. Healthcare organizations should focus on utilizing these suggestions to improve the EMS work climate, which has potential to address the underlying societal issues surrounding EMS staff and may increase job retention and improve patient safety through lower HAI rates.
Supplementary material
To view supplementary material for this article, please visit https://doi.org/10.1017/ash.2022.261
Acknowledgments
We thank the VA employees who participated in the interviews for their time and willingness to share their experiences. We thank Ms. Trina Zabarsky, MSN, RN, CIC, FAPIC, Chair of VHA Environmental Programs Service Director’s Advisory Board for her review of this manuscript. The views presented in this manuscript are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans’ Affairs or the United States government.
Financial support
This work was supported by the VA-CDC Practice-Based Research Network, which was funded collaboratively by the VA Health Services Research & Development Service (HSR&D) service, the Centers for Disease Control & Prevention (CDC), and the Collaborative Research to Enhance and Advance Transformation and Excellence (CREATE) program (CRE 12-289, HSR) from the VA HSR&D.
Conflicts of interest
All authors report no conflicts of interest relevant to this article.






