The Facts
Overall Incidence of Multifetal Pregnancies
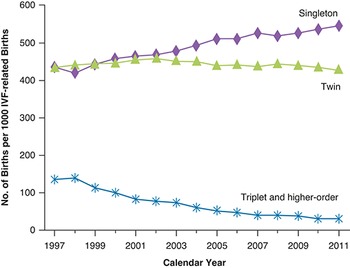
From the introduction of modern record-keeping in the early 1900s until the 1970s, the combined incidence of multiple births in the United States was stable at around 2%. Of these, twins occurred in 18.9 per 1,000 live births and higher-order multiples (triplets and above) in 32.3 per 100,000 births.1 In the 1980s, the widespread introduction of assisted reproductive technologies (ART) and shifting maternal demographics led to a steady increase in multiple pregnancies. From 1980 to 2009, twin births in the United States rose 76% to 33.2 per 1,000 births among women of all ages. Higher-order multiples increased 400%, peaking at 193.5 per 100,000 births in 1998.Reference Martin, Hamilton and Osterman2 In the late 1990s, concerns over the rising rates of multiple pregnancies led to the introduction of professional societal guidelines to reduce the number of multifetal gestations attributable to ART. Higher-order multiple pregnancy rates began to fall shortly thereafter and, in 2018, higher-order multiples occurred in only 93.0 per 100,000 births, a 52% decrease from 1998, but still nearly threefold higher than during the pre-ART era.Reference Martin, Hamilton, Osterman and Driscoll3 The twin birth rate was slower to stabilise, settling at around 33 per 1,000 births between 2007 and 2014. In 2014, for the first time in three decades, the twin birth rate began to decline and, in 2018, represented 32.6 out of 1,000 live births (Figure 1.1).Reference Martin, Hamilton, Osterman and Driscoll3–Reference Norwitz, Diamond and DeCherney6
Incidence of Twin Pregnancies
Twin pregnancies are classified according to their zygosity (genetic make-up) and chorionicity (anatomic arrangement of the placentas and fetal membranes).
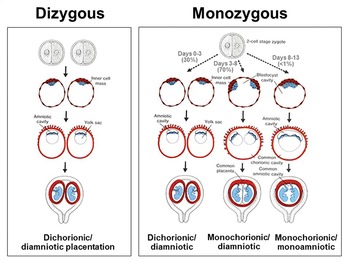
Dizygous (non-identical) twins arise from the fertilisation of two separate oocytes ovulated during the same menstrual cycle and comprise ~70% of spontaneous twin pregnancies. The dizygous (DZ) twin rate is impacted by numerous risk factors (discussed later in this chapter). While data regarding pregnancies conceived by in vitro fertilisation (IVF) are collected nationally, pregnancies arising from clomiphene citrate treatment or ovulation induction/intrauterine insemination (OI/IUI) are not. As such, the true rate of spontaneous DZ twins is difficult to determine. All DZ twins have dichorionic-diamniotic placentation (Figure 1.2).Reference Norwitz, Diamond and DeCherney6
Monozygous (identical) twins arise from the fertilisation of a single oocyte followed by a fission event shortly thereafter. Monozygous (MZ) twins represent the remaining 30% of twin pregnancies or around 0.45% of all gestations. Monozygotic twinning is a random event that occurs once every 250 to 300 conceptions. Such pregnancies are classified according to their chorionicity, which is the single most important determinant of pregnancy outcome in MZ twins and dictates management.Reference Lee, Wylie, Simpson and D’Alton7 If the zygote divides before day 3 post conception, which occurs in 30% of MZ twins, the placentation is dichorionic-diamniotic, identical to that in DZ twins. If the zygote divides between days 3 and 8 post conception, which is the most common timing, occurring in ±70% of MZ twins, the placentation is monochorionic-diamniotic. This means that the twins share a single blood supply. Division between days 8 and 13 post conception results in monochorionic-monoamniotic placentation, which occurs in only <1% of MZ twins (Figure 1.2).Reference Norwitz, Diamond and DeCherney6 Division after day 13 results in incomplete separation and conjoined twins. This is a rare condition complicating only 1 out of 60,000 pregnancies.
‘Vanishing twin’ refers to a singleton pregnancy that began as twins with a subsequent spontaneous reduction so early in pregnancy that no evidence of the twin remains. Close monitoring during IVF has shown that this phenomenon is far more common than previously recognised, occurring in 10.4–18.8% of twin pregnancies. Because 80% of these losses occur prior to 9 weeks’ gestation and thus prior to ultrasound examination, the rate of vanishing twins is likely under-reported in spontaneous pregnancies. Interestingly, male fetuses are at higher risk of spontaneous reduction than female fetuses. This may explain the difference in male-to-female gender ratios between singleton (1.05), twin (0.98) and triplet pregnancies (0.82).Reference Ein-Mor, Mankuta, Hochner-Celnikier, Hurwitz and Haimov-Kochman8
Incidence of Higher-Order Multiples
Triplets constitute more than 90% of higher-order multiples and occur spontaneously in approximately 1 in 8,000 pregnancies. Pregnancies with four or more fetuses occur spontaneously in only 1 out of 70,000 pregnancies. The vast majority of higher-order multiple pregnancies arise from ART.
Types and Incidence of Atypical Twinning
Several atypical forms of twins have been reported.Reference Mcnamara, Kane, Craig, Short and Umstad9 Heterotopic pregnancies occur when twins implant in different locations, most commonly one intrauterine and one ectopic. With ART, approximately 1 in 3,900 pregnancies are heterotopic. Superfetation refers to the fertilisation and implantation of a second conceptus during an existing pregnancy. Although well documented in other animal species, superfetation has not been definitively demonstrated in humans. Complete moles with a coexisting twin occur in 1 out of 22,000–100,000 pregnancies. Fetus in fetu is extremely rare (1 in 500,000 births) and results when a partially formed fetus is enveloped within the body of its surviving twin. It can be distinguished from a teratoma by the presence of vertebrae and limb alignment.
Risk Factors for Monozygotic Twinning
Monozygotic twinning is a random event that occurs once every 250 to 300 conceptions for an overall incidence of 0.45% of spontaneous conceptions. There are no historic or demographic risk factors, and the incidence of MZ twins is the same throughout the world. The only known risk factor for MZ twinning is ART, which increases the rate threefold (range 2–12 fold) to around 1.2%.Reference Gee, Dickey, Xiong, Clark and Pridjian10 The precise mechanism by which ART leads to MZ twinning is not clear. One theory is that embryos cultured in vitro in artificial media have a hardened zona pellucida and that when the embryo hatches from the zona between days 4 and 5 post conception, it is more likely to get caught on the zona and divide. This is most obvious clinically following a single embryo transfer during IVF, but accounts for only 0.5% of IVF twins. Monozygotic twinning is likely a significant contributor to IVF higher-order multiples, with up to 28.8% of triplets and 64.7% of quadruplets following the transfer of fewer than three and four embryos, respectively.Reference Gee, Dickey, Xiong, Clark and Pridjian10 This risk appears to be elevated even further with blastocyst transfer and remains a significant area of ongoing research.
Risk Factors for Dizygotic Twinning
Race/ethnicity. Spontaneous multiple pregnancy rates vary greatly worldwide, ranging from a low of 1.3 per 1,000 births in Japan to a high of approximately 50 per 1,000 births in Nigeria. Pre-ART era data indicate that the spontaneous DZ twinning rate in African-American women is 1 in 80 pregnancies as compared with 1 in 100 pregnancies in Caucasian women and 1 in 155 pregnancies in Asian women.
Maternal age. Even after controlling for ART, increasing maternal age is a major risk factor for DZ twinning. Women aged 35 are twofold to threefold more likely to conceive DZ twins than their 15-year-old counterparts. This is thought to be due to increasing circulating levels of follicle-stimulating hormone (FSH) and diminishing ovarian reserve with increasing maternal age, leading to the recruitment of more follicles each month and the potential for multiple ovulation events. As the maternal population in the United States ages, maternal age is becoming an increasingly important contributor to the total number of multiple gestations. Between 1980 and 2009, the percentage of total births to women older than age 30 rose from 20% to 35%. In 2016, it was estimated that delayed childbearing accounted for 24% and 38% of the national plural birth excess for non-Hispanic white and black women, respectively. Approximately one-third of the total increase in twin pregnancy rates from 1980 to 2009 is attributed to delayed childbearing independent of ART.Reference Adashi and Gutman11,12
Endogenous levels of gonadotropins. Circulating levels of FSH and luteinising hormone (LH) are elevated in women who delivered DZ twins as compared to those who delivered singletons. The underlying cause of elevated gonadotropins is not well understood and is a focus of ongoing research.
Parity. Increasing parity is associated with an increased likelihood of DZ twinning independent of maternal age.
Family and personal history. Dizygotic twinning is known to run in families. Although the precise mode of inheritance remains unknown, the risk appears to be conferred through both the maternal and paternal lineages. Women with sisters who have DZ twins have a risk of 1.7 compared to the general population, and the offspring of female DZ twins have a risk of 2.5.Reference Hoekstra, Zhao, Lambalk, Willemsen, Martin, Boomsma and Montgomery13 A family history of DZ twins in the male partner or sperm donor is also a risk factor for DZ twins, but the effect appears to be much weaker.
Genetic factors. Taken together, the risk of recurrent DZ twins, the association with a positive family history and the racial/ethnic disparity suggest that genetic factors are involved. However, the identification of the ‘twin gene(s)’ remains elusive. The FSH and FSH receptor genes have been energetically investigated given the known contribution of gonadotropins to follicular development, but studies thus far have failed to show such an association. A number of other genes have been identified through familial genome mapping and genome-wide association studies. These include the growth differentiation factor 9 (GDF9) gene variant that appears to double the risk of DZ twinning. However, this variant is found in less than 4% of the population and as such is not believed to be a significant driver of twinning.Reference Hoekstra, Zhao, Lambalk, Willemsen, Martin, Boomsma and Montgomery13 The fragile X mental retardation 1 (FMR1) gene has also been implicated in DZ twinning, though this association is confounded by the premature ovarian failure phenotype and elevated FSH levels in FMR1 gene carriers. In sum, no clinically significant or actionable genes for twinning have thus far been identified, although this is a focus of intense study with particular interest in genes encoding components of the hypothalamic-pituitary-ovarian axis.
Maternal body composition. Both increased maternal height and body mass index (BMI) have been found to independently increase the risk of DZ twinning.Reference Reddy, Branum and Klebanoff14 Much of these data were gleaned from pre-ART-era databases and prior to the obesity epidemic in the United States, which suggests that such factors may be increasingly important in years to come.
Seasonal variation. Rates of DZ twinning appear to vary in a predictable fashion through the year with more twins conceived in summer/autumn and more twins born in winter, although not all studies have confirmed this association. Interestingly, of the studies that demonstrated seasonal variation, the impact appears to have been stronger in the 19th century as compared with the 20th.
Diet. A number of nutritional factors have been associated with higher rates of multiple pregnancies, such as folic acid supplementation and β-carotene. However, these associations are relatively weak and not consistent in the literature.
Assisted reproductive technology. By far the most important driver of DZ twinning is ART. In the United States, infertility affects 15.5% of reproductive-aged couples and approximately 1.7% of births result from ART. Currently, 36% of twin and 77% of triplet pregnancies occur in the setting of infertility treatment, and two-thirds of the plural birth excess in the United States is attributable to ART. Initially, the high incidence of multiple pregnancies was due to the transfer of two or more embryos in a given IVF cycle. As IVF technology developed, the risk of multiple pregnancies increased dramatically, particularly in association with gamete intrafallopian transfer (GIFT) and zygote intrafallopian transfer (ZIFT), procedures now abandoned. After the release of the first set of practice guidelines aimed at reducing ART-related multiple gestations in 1998, the rate of higher-order multiple pregnancies decreased, although the absolute numbers continued to climb due to increased use of ART.15 More recently, use of pre-implantation genetic screening (PGS) has been shown to reduce the risk of multiple gestation, primarily by promoting the use of single embryo transfer in older patients. Ovulation induction using clomiphene citrate, letrozole (a non-steroidal aromatase inhibitor) or exogenous gonadotropins also increases the risk of multifetal gestation. This is due to ovarian hyper-stimulation leading to multiple ovulation. The risk of DZ twinning with OI/IUI is higher than that with traditional IVF, although pregnancy outcomes with OI/IUI are not tracked as closely as IVF and, as a result, multiple rates may be underreported.
Other risk factors. Factors such as smoking, lower socio-economic status, oral contraceptives and coital frequency have been associated with a higher rate of DZ twinning. However, the evidence in support of these associations is inconsistent and frequently confounded.
Risk Factors for Higher-Order Multiple Pregnancies
Similarly to DZ twinning, triplet and higher-order multiple rates are affected by race/ethnicity, family history, maternal age and parity. However, the vast majority of such pregnancies are attributable to ART. Despite a significant decline in the rate of higher-order multiples since the implementation of practice guidelines a decade ago, the rate of higher-order multiple pregnancies is still threefold higher than that before the ART era.
The Issues
Most of the risk factors for twin and higher-order multiple pregnancies are not modifiable and as such cannot be actively managed. The one exception is ART, which has been the major driver of the increase in multiple pregnancies over the past 30 years (Figure 1.1). In the United States, the American Society for Reproductive Medicine (ASRM) and the Society for Reproductive Technology (SART) first reported ART practice data in 1988. Until 1992, submission of ART outcome data to the SART registry was voluntary. In 1992, Congress passed the Fertility Clinic Success Rate and Certification Act, which mandated creation of a federal data registry of pregnancy success rates from all ART centres as well as the certification status of embryo laboratories. In collaboration with the ASRM/SART, the US Centers for Disease Control and Prevention (CDC) is responsible for implementing the Fertility Clinic Success Rate and Certification Act. To be a member of the ASRM/SART, an ART programme must agree to submit their IVF procedure activity data to the registry and make them publicly available. This is not necessarily true of other infertility procedures, such as OI/IUI. In the United Kingdom, the Human Fertilisation and Embryo Authority (HFEA) collects the data and statistics of all the IVF treatment cycles on a yearly basis and publishes them for the use of patients, researchers and clinicians. The last year for which data were published was 2018 (published in June 2020). Data are currently available from all years, from the first year of collection of 1991 to 2018.
The major rate-limiting factor for ART is implantation. Although critical to survival of the species, implantation in humans is relatively inefficient. Maximal fecundity (the likelihood of getting pregnant each cycle) peaks at 30%. Only 50% of conceptions advance beyond 20 weeks’ gestation, and of all unsuccessful pregnancies, 75% represent a failure of implantation. Despite exhaustive research, the factors responsible for optimal implantation are not well understood. Interestingly, humans are one of only a few mammalian viviparous species in which endometrial decidualisation (priming) occurs spontaneously during each menstrual cycle and is therefore independent of the conceptus. This suggests that the health of a pregnancy is determined even before the blastocyst arrives, which offers physicians a unique opportunity for intervention. Research in this area is ongoing at the population and cellular levels. A better understanding of these factors may help to further reduce multiple gestations arising from ART.
Management Options
As discussed, most risk factors for multiple pregnancies are not modifiable with the exception of ART. The goal of ART is a single, healthy, take-home baby. The ASRM recognises that multifetal gestations, particularly higher-order multiples, should not be regarded as a success but as a failure of ART. The Committee on Ethics of the American College of Obstetricians and Gynecologists (ACOG) states that ‘the first approach to the problem of multifetal pregnancies should be prevention’.16,17
Assisted Reproductive Technology Methodology
A number of precautions can be taken to reduce the risk of multifetal gestation with ART. The use of low-dose ovarian stimulation protocols whenever possible will reduce the risk of superovulation. Regardless of the stimulation protocol used, the patient should be followed with serial serum estradiol-17β levels and follicle number by transvaginal ultrasound and the cycle cancelled if too many follicles develop to minimise the risk of ovarian hyper-stimulation syndrome (OHSS). The ASRM consensus guidelines also offer recommendations for embryo transfer number based on predicted IVF success rates with the stated goal of reducing rates of higher-order multiple pregnancy.15,17 These recommendations are based on characteristics associated with a more favourable prognosis, including embryo number and quality, first IVF cycle, prior IVF success and donor oocytes from women younger than 35 years of age. Women younger than 35 with favourable prognostic indicators should be offered single embryo transfer and should not have more than two embryos transferred. A third embryo may be transferred in women older than age 35, especially if they have poor-quality embryos or have suffered multiple failed IVF cycles, but this should be the exception, not the rule.15 In the United Kingdom, the HFEA, working with other British obstetrics and scientific governing bodies, updated its advice in 2019 for IVF to ideally limit embryo transfer to one per treatment cycle to minimise the risk of multiple pregnancy. In older women or in those with poor-quality embryos, two may be transferred with a maximum of three in those older than 40 years. Care should be taken to avoid financial influences when making decisions around embryo transfer.16 In the United States, in states with no mandate for health insurance coverage of infertility treatments, patients must pay out of pocket. They are therefore often incentivised to maximise the success rate of each cycle, leading them to advocate for the transfer of more embryos and driving up the multiples rate. Strategies to reduce these barriers include petitioning state governments to change their insurance mandates and/or offering alternative payment plans through the clinics.
Multifetal Pregnancy Reduction
The ASRM and the ACOG recognise the increase in morbidity and mortality associated with multifetal gestation for both the pregnant patient and the fetuses (Table 1.1).1,Reference Lee, Wylie, Simpson and D’Alton7,12,Reference Hoekstra, Zhao, Lambalk, Willemsen, Martin, Boomsma and Montgomery13,15,16 Moreover, medical costs for twins quadruple that of their singleton counterparts, while triplet costs are tenfold higher.Reference Callahan, Hall, Ettner, Christiansen, Greene and Crowley18 Higher rates of maternal depression and child abuse have also been reported with multiples. Given the potential adverse consequences of multiples, multifetal pregnancy reduction (MFPR) is sometimes recommended. This refers to the termination of one or more fetuses in the setting of a multifetal gestation with a view to optimising the outcome for the surviving fetuses. It is most typically performed in higher-order multiple pregnancies and involves the intra-cardiac injection of potassium chloride. Multifetal pregnancy reduction has been shown to significantly reduce spontaneous pregnancy loss, preterm birth and neonatal death for the surviving fetus(es) as well as maternal medical complications associated with higher-order pregnancy. Multifetal pregnancy reduction is in contrast to selective fetal reduction, in which one or more fetuses are selectively terminated due to an underlying structural, genetic or metabolic disorder.
| Characteristic | Single | Twins | Triplets | Quads |
|---|---|---|---|---|
| Preterm birth | 10–12% | 40–50% | 85–95% | 100% |
| Gestational age (week) | 39.5 | 35.3 | 32.2 | 29.9 |
| Birth weight (gram) | 3,500 | 2,347 | 1,687 | 1,309 |
| Fetal growth restriction | 10% | 15–25% | 50–60% | 50–60% |
| NICU admission | 5–10% | 25% | 75% | 100% |
| NICU length of stay | 1–3 days | 18 days | 38 days | 58 days |
| Congenital anomalies | 3–4% | 6–15% | 20% | - |
| Major handicap | < 1% | 7% | 20% | 40–50% |
| Risk of cerebral palsy | reference | 4 × singles | 17 × singles | - |
| Risk of neonatal death | reference | 7 × singles | 20 × singles | - |
Multifetal pregnancy reduction raises a host of complex and deeply personal social, economic, ethical and medical issues. Appropriate counselling is critical. The ACOG recommends that ‘nondirective patient counselling should be offered to all women with higher-order multifetal pregnancies and should include discussion of the risks unique to multifetal pregnancy as well as the option to continue or reduce the pregnancy’.1,16 Consultation with experts in maternal fetal medicine, neonatology, support groups and family planning or other providers with expertise in the procedure is advised. The ACOG further recommends that if MFPR is not in alignment with a provider’s personal beliefs, a timely referral should be offered.
Key Points
Widespread introduction of ART and shifting maternal demographics led to a steady increase in multiple pregnancies, which plateaued after the 2010s with the implementation of societal guidelines aimed at reducing multifetal gestations.
Dizygotic (non-identical) twins comprise approximately 70% of spontaneous twin pregnancies; the remaining 30% are MZ (identical).
Monozygotic twinning is a random event occurring in 1 out of 250 to 300 pregnancies.
Dizygotic twinning is influenced by many factors, including maternal age, race/ethnicity, parity, family history and use of ART. The only risk factor for MZ twinning is IVF.
Both IVF and OI/IUI increase the risk of multifetal gestation, with OI/IUI carrying a slightly higher risk.
Multifetal pregnancy, particularly higher-order multiple pregnancy, is recognised as an undesirable outcome by both the ASRM and the ACOG due to increased maternal and fetal morbidity and mortality.
Providers should seek to prevent multifetal gestation by using low-dose ovarian stimulation protocols and carefully monitoring ovulation induction cycles.
When performing IVF, single embryo transfer should be considered whenever possible.
When a higher-order multifetal gestation is encountered, the patient should be offered non-directive and multidisciplinary counselling regarding MFPR.