Acute otitis media (AOM) is the most cited indication for antibiotics in children. Reference Lieberthal, Carroll and Chonmaitree1 Even though up to 81% of AOM episodes will resolve without antibiotic treatment, 95% of children with AOM are prescribed an antibiotic and most children 2 years and older are prescribed antibiotics for longer than recommended durations. Reference Venekamp, Sanders, Glasziou, Del Mar and Rovers2,Reference Frost, Lou, Keith, Byars and Jenkins3
Several strategies have been proposed to reduce unnecessary antibiotic use including observation, delayed prescribing, and prescribing shorter durations of antibiotics. Reference Lieberthal, Carroll and Chonmaitree1 In clinical trials, observation and delayed prescribing reduced antibiotic utilization and had similar parent satisfaction compared to immediate prescribing. Reference Spurling, Del Mar, Dooley, Foxlee and Farley4 However, these strategies are rarely employed in clinical practice. Reference Frost, Lou, Keith, Byars and Jenkins3,Reference Frost, Monti and Andersen5,Reference Norlin, Fleming-Dutra and Mapp6 Furthermore, though caregiver satisfaction is a cited as a key driver of prescribing, Reference Mangione-Smith, McGlynn, Elliott, Krogstad and Brook7 caregiver preferences for management of AOM are poorly understood. We evaluated caregivers’ understanding of AOM and antibiotic-associated risks, preferences for management, and behavior if prescribed a delayed antibiotic.
Methods
This study was conducted at Denver Health (DHHA) in Denver, Colorado, from September to November 2020. DHHA is a large, diverse, federally qualified health center system. Caregivers, including parents or primary medical decision makers (eg, grandparents) of children aged 6 months to 12 years who had a diagnosis of AOM in the prior 2 years, who had a documented phone number and spoke English or Spanish were included.
A descriptive survey was developed that assessed caregiver knowledge, attitudes, and beliefs regarding AOM across 4 domains: factors associated with risk of AOM, potential harms associated with antibiotics, preferences for management, and predictive behavior with delayed prescribing (Supplementary Material). The survey was reviewed by a community advisory panel and 7 caregivers from diverse backgrounds prior to distribution. The final survey was developed in REDCap and was sent to eligible caregivers via text message. The survey remained open for 45 days and up to 3 reminders were sent to nonresponders. Descriptive statistics and weighted averages for relevant questions were computed.
The DHHA Quality Improvement Committee, which is authorized by the Colorado Multiple Institutional Review Board at the University of Colorado–Denver, reviewed the project and determined that it was not human subjects research because it was part of a quality improvement project.
Results
The survey was sent to 2,447 eligible caregivers and 101 completed it (response rate, 4.1%) Similar to nonrespondents, respondents were largely female (n = 75, 91%), Hispanic/Latinx (n = 58, 71%), and had public insurance or were self-payers (n = 53, 65%) (Supplementary Material).
Understanding of risk factors
More than half of caregivers knew that smoke exposure (secondhand, n = 58, 58%; residue, n = 54, 54%) or sleeping with a bottle (n = 56, 56%) increased the risk of AOM. More caregivers understood that breastfeeding (n = 69, 69%), receiving the influenza vaccine (n = 67, 67%) and regular childhood vaccines (n = 61, 61%) reduced the risk of AOM (Table 1).
Table 1. Caregiver Understanding of Ear Infections and Perceived Complication Risks Associated With Treating and Not Treating With Antibiotics a
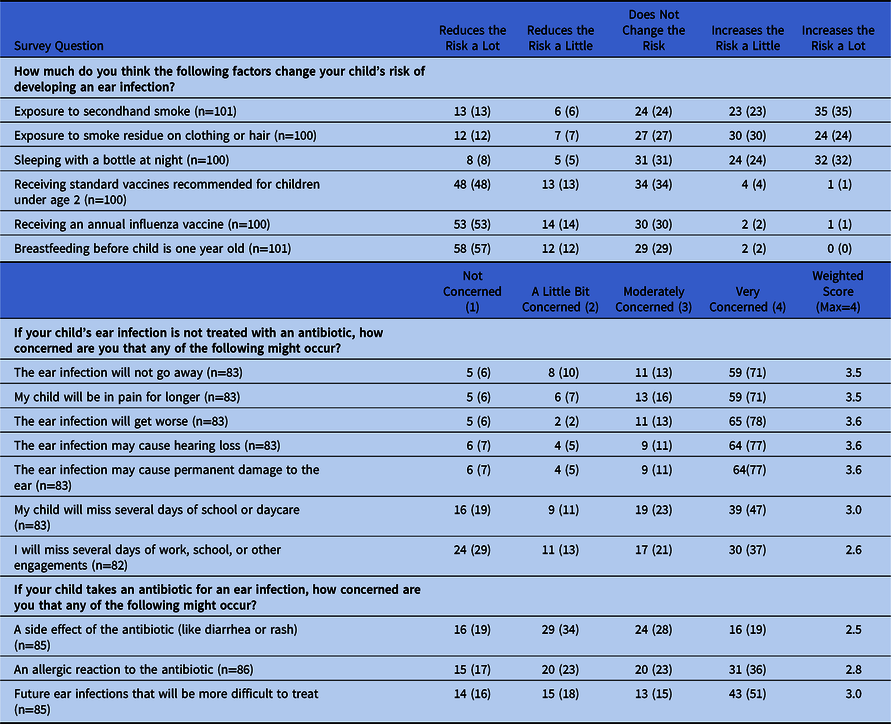
a All results are represented as no. (%) unless otherwise noted.
Perception of AOM complications and antibiotics
Most caregivers (n = 70, 84%) were moderately or very concerned that if their child was not treated with antibiotics the infection would not go away, the child would be in pain for longer (n = 72, 87%), develop hearing loss (n = 73, 88%), or have permanent damage to the ear (n = 73, 88%). In contrast, caregivers were more likely to be moderately or very concerned about risk of future infections that are more difficult to treat (n = 56, 66%) or allergic reaction (n = 51, 59%) than side effects (n = 40, 47%) associated with antibiotics.
Preferences for AOM Management
Caregivers were more likely to be moderately or very satisfied with an immediate antibiotic (n = 73, 82%) than a delayed antibiotic prescription (n = 62, 69%). More than half of caregivers stated they would be very unsatisfied or only a little bit satisfied with observation with in-person (n = 57, 64%) or phone follow up (n = 52, 58%) if needed. Most caregivers 66 (77%) indicated they would fill a delayed antibiotic prescription immediately; 47 (55%) would fill and give the antibiotic immediately and 19 (22%) would fill the antibiotic but only give it if needed. Caregivers did not have strong preferences for duration of therapy. In total, 62 (70%) would prefer whatever length was recommended by the doctor and 14 (16%) wanted the shortest duration needed to treat the infection. More than 90% of caregivers felt a pain management plan was important (Table 2).
Table 2. Caregiver Preferences for Management of Acute Otitis Media a
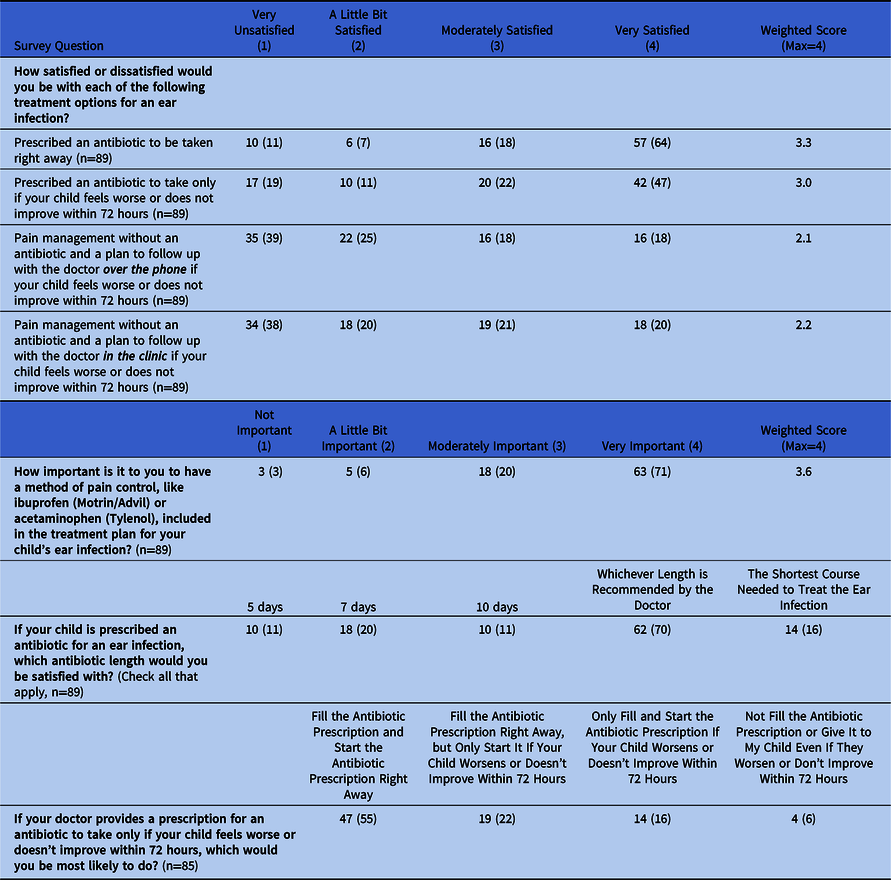
a All results are represented as no. (%) unless otherwise noted.
Discussion
Similar to prior studies, caregivers were highly concerned about potential complications and pain from untreated or delayed treatment and had misconceptions about the need for antibiotics. Reference Kautz-Freimuth, Redaèlli, Samel, Civello, Altin and Stock8,Reference Hansen, Howlett, Del Mar and Hoffmann9 In contrast, caregivers were less concerned about risks associated with antibiotics. Caregivers expressed strong preferences for immediate antibiotics and most caregivers stated they would immediately fill prescriptions written as delayed. Conversely, caregivers did not have a strong preference for antibiotic duration; most wanted whichever length was recommended by their provider. Parental pressure is often cited as a key driver of antibiotic prescribing, Reference Mangione-Smith, McGlynn, Elliott, Krogstad and Brook7 and education for caregivers on the risks and benefits of antibiotic treatment for AOM is likely needed to reduce misconceptions and curtail prescribing.
In contrast to prior clinical trials, caregivers in a community health center environment had low satisfaction with observation and delayed prescribing and were very likely to immediately fill prescriptions written as delayed. Pragmatic studies that broadly examine antibiotic use and satisfaction with observation or delayed prescribing in typical clinical practice environments are needed. Similarly, we previously reported that providers were less likely to use delayed prescribing or observation than immediate prescribing. Reference Frost, Lou, Keith, Byars and Jenkins3 Further studies are warranted to assure that national approaches to AOM management and antibiotic stewardship align with the needs of caregivers and willingness of providers to follow them.
Comparatively, caregivers did not have strong preferences for duration of therapy. We previously found that providers preferred to prescribe the shortest duration of antibiotics needed. Reference Frost, Lou, Keith, Byars and Jenkins3 Shorter durations of antibiotics have been shown to be equally effective for most children aged ≥2 years with AOM and are associated with reduced adverse drug events. Reference Kozyrskyj, Klassen, Moffatt and Harvey10 Thus, prescribing a shorter duration of antibiotics for children aged ≥2 years is likely to substantially reduce overall antibiotic exposure in a way that is acceptable to caregivers and providers.
The strengths of this evaluation include responses from a diverse population in a community-based health system. This evaluation also has limitations. Because this was a single-center project, the data are not generalizable to other organizations and evaluation of patients from diverse settings is warranted. Selection bias likely influenced the results; respondents were more likely to identify as a race other than White or Black and were more likely to have commercial insurance than nonrespondents. In addition, the response rate was low and caregivers who felt strongly about AOM management may have been more likely to respond to the survey. The low response rate may be attributed to the characteristics of our diverse patient population including technology barriers, recruitment using text messages, concerns about being identified, literacy barriers, mistrust of the medical establishment, or lack of an incentive to respond.
In conclusion, careful evaluations of caregivers’ preferences for management and providers’ willingness to adopt recommendations across diverse practice settings and populations are needed to guide AOM management and antibiotic stewardship recommendations. In particular, studies to better understand antibiotic utilization and satisfaction with observation and delayed prescribing in typical clinical practice would be beneficial. In the interim, optimizing the duration of antibiotics prescribed is likely to be a pragmatic mechanism to reduce antibiotic use in a way that is aligned with caregiver preferences.
Acknowledgments
Financial Support
This study was funded by the Denver Health Pilot Grant Program (no awardee number, to H.F). H.F. received salary support from the Eunice Kennedy Shriver National Institute of Child Health & Human Development of the National Institutes of Health (grant no. K23HD099925). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Conflicts of Interest
All authors report no conflicts of interest relevant to this article.
Supplementary material
To view supplementary material for this article, please visit https://doi.org/10.1017/ash.2021.242






