Introduction
Group CBT (gCBT) is recognised as a strong, evidence-based psychological intervention for depression in adults (National Institute for Health and Clinical Excellence, 2022). The goal of gCBT is to teach coping skills by educating clients on how thoughts, beliefs, behaviours and feelings interact (National Institute for Health and Clinical Excellence, 2022). Research suggests that peer support and the therapeutic alliance are also important factors in symptom reduction during gCBT (Laska et al., Reference Laska, Gurman and Wampold2014). It has also been shown that high therapeutic alliance ratings can be maintained in therapy provided through videoconferencing (Berger, Reference Berger2017). This study aims to add to the body of literature on the effectiveness of gCBT delivered via video conferencing.
The COVID-19 pandemic changed people’s ways of socialising, working and living (Wu et al., Reference Wu, Jia, Shi, Niu, Yin, Xie and Wang2021). Globally, it led to increased mental health problems (Wu et al., Reference Wu, Jia, Shi, Niu, Yin, Xie and Wang2021). Although mental health problems increased since the outset of the pandemic, access to mental health services became more difficult, due to government restrictions (Wu et al., Reference Wu, Jia, Shi, Niu, Yin, Xie and Wang2021). In Ireland, many services had to be halted due to the threat of contracting COVID-19. In-person group therapy was deemed unsafe, and therefore adapting to an online format became crucial. Thus, online therapy quickly became the new normal.
This paper focuses specifically on the gCBT for depression conducted in the context of a secondary adult mental health service in Ireland. At the outset of the pandemic, the original 12-session, 2.5-hour face-to-face group was reduced to an 8-session, 1.5-hour online format. This reduction was due to the presumption that it would be more difficult to sustain attention and engagement with the online format. However, preliminary analysis of the effectiveness of this shortened online gCBT suggested that it was not as effective as the longer face-to-face group. Reasons for this may have been the pandemic negatively impacting people’s mental health, due to the online format, or due to the change in dose of therapy. When analysing the differences between the groups, it was noted that the online group consisted of 600 hours of therapy, whereas the face-to-face group consisted of 1800 hours. Thus, the dose of therapy in the online group was one-third the dose provided in the face-to-face group. Hence, the focus of this study was to directly compare the online and face-to-face format of 12 sessions×2.5 hours.
Our research questions were as follows:
-
(1) Is an online CBT group for depression as effective as a face-to-face group once the dose of therapy is equal?
-
(2) Does the increased dose of therapy enhance the effectiveness of the online CBT group for depression?
Method
Intervention
The gCBT programme was developed and delivered by a clinical psychologist with over 30 years of experience. This clinical psychologist (third author of this paper) ran each group within the three conditions (face-to-face, online 8-session and online 12-session), apart from one 12-session online group, which was replaced by another experienced clinical psychologist for four sessions. Two assistant psychologists co-facilitated each group, and these individuals varied across the three conditions. The groups consisted of behavioural activation, cognitive restructuring, and lifestyle management. The content remained consistent across all three conditions, with less time spent on each topic during the 8-session online group. Therapeutic alliance was also a focus of the group. Pre-group assessments were aimed to be completed in person where possible, to foster this. Individual support was also available throughout the group if needed. Clients were given adequate time to speak and connect with both the therapists and other group members throughout the sessions.
In developing the online gCBT, additional videos were created and/or sourced and presentation slides were included. These included role plays of cognitive techniques as well as diagrams to explain different concepts. This was to stimulate engagement within the sessions. Zoom breakout rooms were used as a tool to mimic smaller group/pair discussions, which would be commonly used in the face-to-face group, to engage peer support. Quick Inventory of Depression Symptomatology (QIDS) questionnaires were completed by clients prior to each session. This was to combat the additional challenge of gauging emotional wellbeing via videoconferencing.
Participants
Potential group members were referred by their clinical team for assessment. Originally all clients were referred to the face-to-face groups, as that was the only mode of intervention. All face-to-face data are from 2018–2019. Due to COVID-19, no in-person groups were allowed, therefore the online format was developed.
The initial online group was shorter (8 sessions×1.5 hours) as it was felt that both the staff and the clients would not tolerate the session length that was used for face-to-face groups. All 8-session group data is from 2020. As the staff became more skilled, and the clients became more used to Zoom, the number of sessions and the session length was extended, so that it mirrored the face-to-face groups (12 sessions×2.5 hours). All 12-session online group data are from 2021–2022. Clients were deemed suitable for the group if depression was their primary issue at the time, and if they displayed a readiness to engage in therapy. No other inclusion criteria were used.
One hundred and twelve participants (65 women, 47 men) were recruited (mean age=41.85, SD=13.08). Forty-two participants from the face-to-face group interventions (23 female, mean age=42.0, SD=15.5), 21 participants from the 8-session online groups (14 female, mean age=42.9, SD=13.34) and 49 participants from the 12-session online groups (28 female, mean age=41.7, SD=13.7) were analysed.
Design
This is a between-groups naturalistic treatment outcome study. Pre- and post-intervention measures include the Beck Depression Inventory-II (BDI-II), Beck Anxiety Inventory (BAI), and the World Health Organisation Quality of Life Scale (WHOQoL-Bref). Written informed consent was obtained from all participants. Protocol adherence was assessed with session checklists and a treatment manual.
Analyses
A mixed between-within subjects analysis of variance was performed to assess the impact of the three different interventions (12 sessions×2.5-hour face-to-face group, 8 sessions×1.5-hour online group and 12 sessions×2.5-hour online group) on participant scores for each of the outcome measures (anxiety, depression and QoL) over time.
Results
All three groups showed reductions in depression following the intervention, as there was a substantial main effect for time; Wilks’ lambda=.53, F 2,87=78.27, p<.001, partial eta squared=.474 (see Table 1). For depression, there was no significant interaction between intervention type and time; Wilks’ lambda=.93, F 2,87=1.27, p=.285, partial eta squared=.028. There was no significant difference between the three intervention groups regarding the impact on depression scores, as the main effect comparing the three types of intervention was not significant; F 2,87= 1.47, p=.24, partial eta squared=.033.
Table 1. Depression, anxiety and quality of life scores at pre- and post-intervention
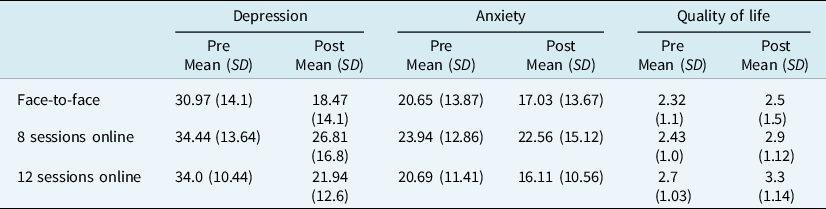
All three groups showed significant reductions in anxiety following the intervention (see Table 1), as there was a substantial main effect for time; Wilks’ lambda=.94, F 2,87=5.83, p=.018, partial eta squared=.063. For anxiety, there was no significant interaction between intervention type and time; Wilks’ lambda=.99, F 2,87=.422, p=.65, partial eta squared=.01. There was no significant difference in the impact on anxiety scores between the three groups, as the main effect comparing the three types of intervention was not significant; F 2,87=1.13, p=.33, partial eta squared=.025.
All three interventions were associated with higher quality of life following the intervention as there was a substantial main effect for time; Wilks’ lambda=.9, F 2,87=9.46, p=.003, partial eta squared=.098 (see Table 1). For QoL, there was no significant interaction between intervention type and time; Wilks’ lambda =.97, F 2,87=1.16, p=.32, partial eta squared=.026. There was no significant difference in the impact on QoL between the three interventions, as the main effect comparing the three types of intervention was not significant; F 2,87=3.1, p=.052, partial eta squared=.067.
Attendance rates were also compared across all three groups. The 12-session online group had the highest rate of attendance (85.10%), followed by the eight-session online group (79.99%) and the face-to-face group (72.80%).
Discussion
All three interventions significantly improved anxiety, depression and QoL scores. There was no significant difference between the three groups in terms of impact on the outcome measures. This research supports published data showing that effective and acceptable group therapy can be delivered online. Online therapy offers new opportunities. It allows for increased inclusivity, flexibility, and the use of new materials (e.g. videos, PowerPoints). It allows for clients to participate who otherwise may not have been able to due to work, mobility, health, childcare and transport considerations. The 12-session groups showed slightly greater improvement in QoL, but this effect was not statistically significant (p=.052). Further research using a larger sample size may give further insight into whether a greater number of sessions results in better QoL outcomes. Interestingly, the 12-session online group had a higher attendance rate than the 8-session online group. One hypothesis for this could be that the longer group allows for a greater connection to be made between the participants, therefore making it more likely that they will attend each week. Conversely, the face-to-face group has the lowest attendance rate, which solidifies client feedback that the online group was easier to attend. Our sample is too small to make any conclusions about this, therefore further research should be done to investigate this finding.
This project is limited by its small non-randomised sample, and the fact that it is a single-site study. Future research should target an increased sample size, along with multi-site data collection to make results more generalisable, and to compare results with other populations, e.g. adults in primary care. Another limitation is that the groups were not randomised and therefore there may be a selection effect. Additional analysis should also be considered to look at potential confounding variables, e.g. age, cultural backgrounds, and socioeconomic status. Extra measures should be put in place to ensure that people are not excluded due to the therapy mode. For example, devices should be made available to clients who do not have access to one, therapy rooms should also be considered for those who do not have adequate privacy in their homes, and comprehensive training should be provided to those who are not familiar with technology.
This study provides preliminary evidence that online gCBT can be as effective as in-person therapy, with further research needed into the impact of therapy dose as well as therapy mode.
Data availability statement
The data that support the findings of this study are available on request from the corresponding author, D.R. The data are not publicly available due to the data containing information that could compromise the privacy of research participants.
Acknowledgements
The authors would like to thank the service users who contributed to this study.
Author contributions
Dearbhail Ryan: Data curation (lead), Formal analysis (supporting), Methodology (equal), Project administration (equal), Writing – original draft (lead), Writing – review & editing (lead); Clodagh Cogley: Formal analysis (lead); Lucy Moore: Investigation (lead), Project administration (lead), Resources (lead), Supervision (lead), Writing – review & editing (equal).
Financial support
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Competing interest
All authors declare that they have no competing interests.
Ethical standard
This study was approved by the Research and Ethics Committee of Cluain Mhuire Community Services. All procedures were in accordance with the ethical standards of the research committee and with the 1964 Helsinki declaration and its later amendments. Informed consent was obtained from all individual participants included in the study.






Comments
No Comments have been published for this article.