Introduction
Hepatitis B is a highly infectious disease caused by the hepatitis B virus (HBV). Despite the availability of an effective vaccine, HBV is considered a major public health problem in developing countries [Reference Stanaway1]. Globally, around 2.57 billion people are estimated to be infected with HBV and among them, more than 250 million are chronically infected with an increased risk of developing HBV-related liver diseases, including liver cirrhosis (LC) and hepatocellular carcinoma (HCC) [Reference Schweitzer2, Reference Terrault3]. According to the global burden of disease, almost 887 000 deaths occurred in 2015 due to acute and chronic HBV infections and 17%, 40% and 43% of deaths were caused by acute infections, LC and HCC, respectively [Reference Schweitzer2]. The prevalence of HBV infection is highly heterogeneous throughout the world and classified as high prevalence areas wherein more than 8% of the people is positive for hepatitis B surface antigen (HBsAg); high intermediate prevalence areas wherein 5–7.99% of the people HBsAg positive; low intermediate prevalence areas wherein 2–4.99% of the people is HBsAg positive; and low prevalence areas wherein less than 2% of the people is positive for HBsAg [Reference André4, Reference Shepard5].
Bangladesh is a densely populated developing nation of South Asia, according to the first report in 1984, the prevalence of HBV infection was 7.60% in Bangladesh and indicated as a country with a high intermediate prevalence of hepatitis B [Reference Islam6]. The major difficulties for hepatitis B elimination in Bangladesh, including a lack of reliable data to guide policy, low awareness and barriers to early diagnosis, transmission via infected blood products, unsafe injections and nosocomial transmission and a lack of treatment availability. However, recent studies from 2005 onwards, reported that the prevalence of HBV infection in Bangladesh is at a decline. In 2003, Bangladesh Government included the hepatitis B vaccine in the Expanded Programme of Immunisation (EPI), intending to provide a timely birth dose to newborn babies. It was identified as the most effective HBV immunisation programme across the country with a reported successful HBV vaccination rate of 95% in children [Reference Uz-Zaman7]. However, the scenario was different for adults, who were not included in the free vaccination campaign that ran from 2003 to the present day in Bangladesh. According to studies conducted in 1991, 1997, 2008 and 2011, the reported prevalence of hepatitis B were 8.6%, 6.4%, 5.5% and 6.5%, respectively in adults [Reference Alam8]. Besides, details are scarce on the prevalence of HBV infection throughout the general community of Bangladesh and no studies have been carried out at the country level.
Therefore, as there is currently no comprehensive study in this regard in Bangladesh, the present meta-analysis was performed to estimate the current prevalence of HBV infection in the general population of Bangladesh based on the data previously published from 1995 to 2021.
Methods
Literature search strategy
This systematic review and meta-analysis on the prevalence of hepatitis B in Bangladeshi people were conducted according to the guidelines of Preferred Reporting Items for Systematic Review and Meta-Analyses (PRISMA) [Reference Liberati9] (Supplementary file 1). The four international databases (PubMed, Google Scholar, Scopus and Web of Science) and the national databases (Bangladesh Journals Online) were searched for all published studies up to April 2021. The following keywords such as ‘hepatitis B’, ‘hepatitis B virus, ‘HBV’, ‘HBsAg’, ‘prevalence’, ‘prevalent’, ‘epidemiology’, ‘Bangladesh’ and ‘Bangladeshi people’ were used during the search. Additionally, the native journals that could not be accessed online were searched manually and unpublished studies were retrieved from the library of Noakhali Science and Technology University, Bangladesh.
Inclusion and exclusion criteria
We adopted cross-sectional studies reporting on the prevalence of hepatitis B in the Bangladeshi people. The listed inclusion criteria were the following: (1) study published in a peer-reviewed journal in English; (2) reported studies were accessible in full text (editorial, conference abstracts, case reports not included); and (3) all articles were published from 1995 to 2021. The exclusion criteria were the following: (1) study published in other languages than English; (2) study populations coinfected with HBV, HCV and HIV and (3) study design with non-random sampling like conducted on blood donors, sex workers and connected to other clinical studies.
Data extraction
The data extraction was conducted independently by three authors (AG, KYG and HD) based on study design and inclusion criteria. After reviewing a full-text article, the following data were extracted from each study including first author name, publication year, year of data collection, study design, sample size, study setting (urban or rural), gender, age, sample size, number of HBsAg positive individuals and HBsAg test methods. Any inconsistencies during the data extraction were solved through careful discussion with other authors (AD and SB).
Quality assessment
For evaluating the quality of all included studies, further, we assessed the articles using the Cross-Sectional/Prevalence Study Quality Assessment Forms which were suggested by the Agency for Healthcare Research and Quality (AHRQ) [Reference Rostom10]. This AHRQ form has eleven questions (Supplementary file 2: Table S1), of which ten questions are fitted for cross-sectional studies, and the questions were answered with ‘Yes’, ‘No’ and ‘Unclear’. ‘Yes’ represented a score of 1 and ‘No’ or ‘Unclear’ represented a score of 0. The total score of ten questions in the AHRQ form was used to assess the quality of each article in this systematic review and meta-analysis.
Statistical analysis
The Freeman–Tukey double arcsine transformation of proportions was used to estimate the pooled prevalence of HBV infection [Reference Barendregt11, Reference Yuan12]. DerSimonian-Laird random-effects models were followed to conduct the meta-analysis with a 95% confidence interval (95% CI). We conducted subgroup analyses on the included studies based on age groups, genders and marital status. The existence of heterogeneity across studies was evaluated using both the Cochrane chi-square Q-test and I2 index with its resultant P-value. A value of I2 25%, 50% and 75% was used to define the heterogeneity of low, medium and high, respectively. Standard error was estimated from the sample size according to Wan et al. [Reference Wan13] method. Finally, the funnel plot was used to assess the possible publication bias graphically and formally by Begg's and Egger's test (significant at P < 0.05). All analyses were carried out by MetaXL software (meta-analysis in Microsoft Excel) and Review Manager 5.4 (RevMan 5.4, the Cochrane Collaboration, Oxford, United Kingdom).
Results
Search result
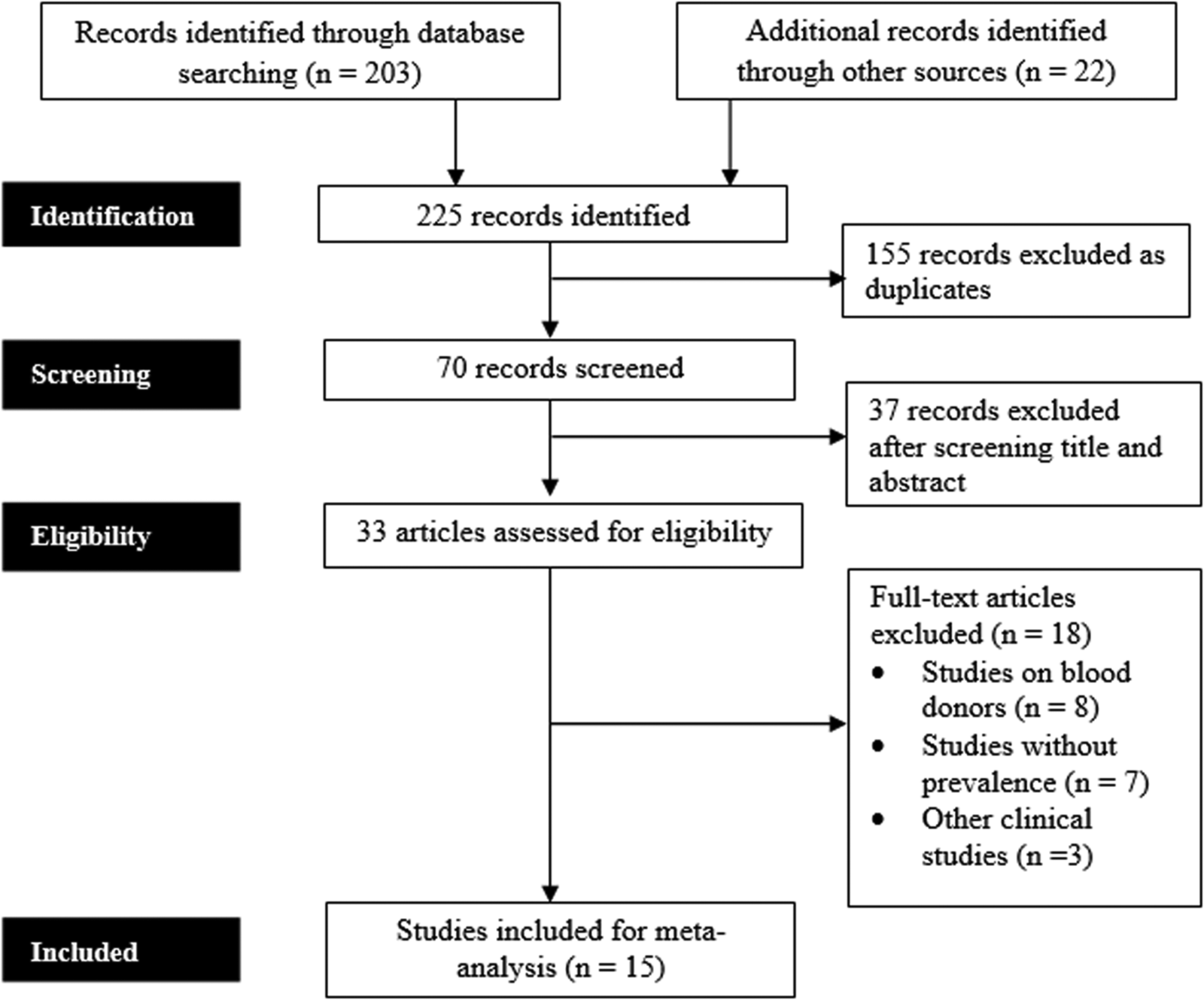
A total of 225 articles were identified through various databases searches. After the removal of duplicate records, additional screening and analysis of the titles and abstracts, 33 articles were retrieved for final assessment. Among 33 studies, 15 articles met the eligibility criteria and were finally included in the meta-analysis. Figure 1 shows the process of the literature review, screening and eligibility assessment of the study articles.
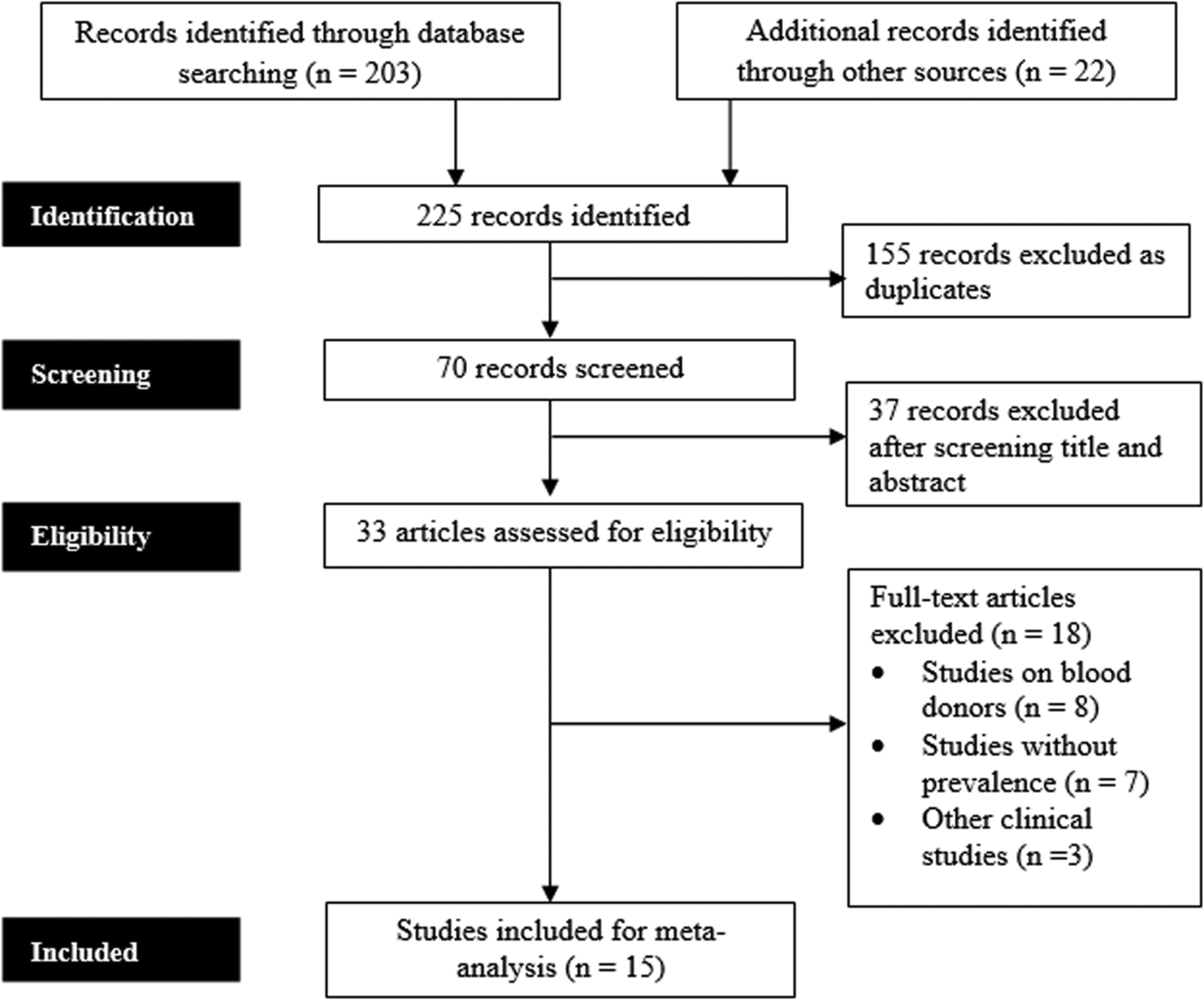
Fig. 1. Flowchart showing the literature searching process of the study according to PRISMA guidelines.
Characteristics of included studies
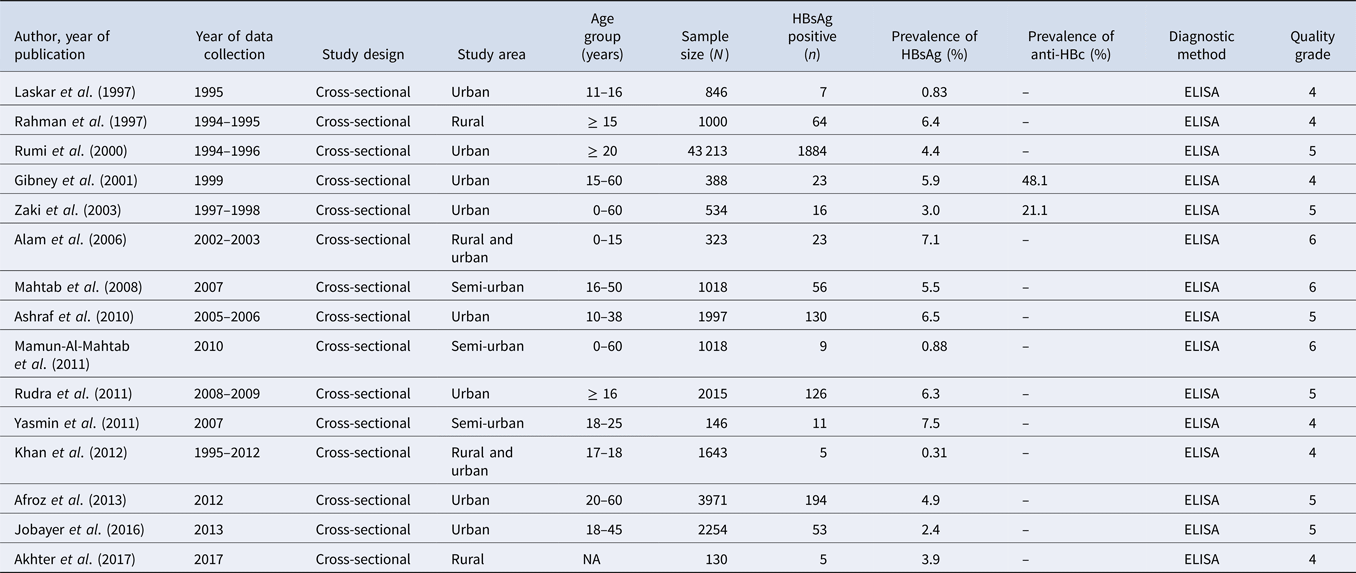
The included 15 studies with a total sample size of 60 496 reported the prevalence of hepatitis B in Bangladesh and the characteristics of all studies are presented in Table 1. All the included articles [Reference Akhter14–Reference Zaki28] were cross-sectional studies and conducted throughout the period ranging from 1995 to 2017. The smallest sample size was 130 [Reference Akhter14] and the largest sample size was 43 213 [Reference Rumi26]. Eight studies were conducted in urban settings [Reference Ashraf16–Reference Jobayer19, Reference Laskar21, Reference Rudra25, Reference Rumi26, Reference Zaki28], three in semiurban settings [Reference Mahtab22, Reference Mamun-Al-Mahtab23, Reference Yasmin27], two in rural settings [Reference Akhter14, Reference Rahman24] and two studies covered both rural and urban areas [Reference Alam15, Reference Khan20]. In terms of quality, all studies rated as high quality and had a total quality score higher than 4 (Supplementary file 2: Table S2).
Table 1. Characteristics of the studies included in the meta-analysis, order by year of publication and alphabetically within the same year

Meta-analysis
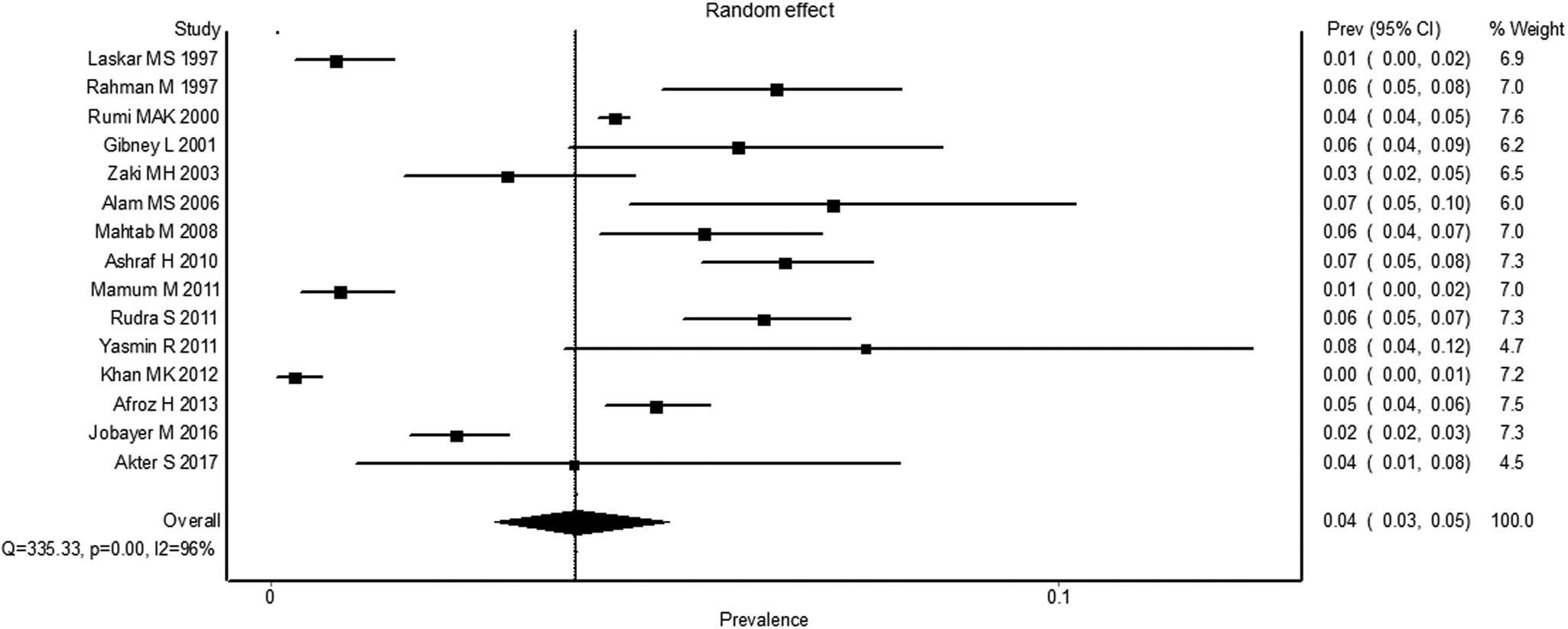
The pooled estimated prevalence of HBV infection in the general people of Bangladesh was 4.0% (95% CI 3.0–5.1) (Fig. 2). The results of the heterogeneity test showed that the included studies were significantly heterogeneous (I2 = 96%, P < 0.0001). Figure 3 shows the results of subgroup analysis of HBV infection among the included studies based on age groups, gender and marital status. The estimated prevalence of hepatitis B was higher in people of age <25 years compared to the people of age >25 years [odds ratio (OR) 1.25, 95% CI 0.72, 2.17, P = 0.42] with heterogeneity I 2 78%. The prevalence of hepatitis B was higher in females in comparison to the males (OR 1.20, 95% CI 0.48, 2.97, P = 0.70) with heterogeneity I 2 95%. The results also demonstrated that the prevalence of hepatitis B was significantly higher in married people than unmarried/single people (OR 2.16, 95% CI 1.51, 3.10, P < 0.0001) with heterogeneity I 2 68%. Finally, the funnel plot (Fig. 4) and Egger's linear regression (P = 0.584) and Begg and Mazumdar's rank correlation test (P = 0.054) for the prevalence of HBV infection indicated that there was no evidence of possible publication bias in all studies.

Fig. 2. The pooled prevalence of HBV infection in the general people of Bangladesh.

Fig. 3. Sub-group meta-analysis reporting HBV prevalence in Bangladesh. (A) between gender, (B) between age groups and (C) between married and unmarried people.

Fig. 4. Funnel plot of the meta-analysis.
HBV infection in Bangladesh over time
Based on the publications included in the present study, we examine the changes in the reported prevalence of HBV infection in the general population of Bangladesh over time (Fig. 5). According to studies, the prevalence of HBV infection in Bangladesh was 7.12% between 2001 and 2003. In Bangladesh, a decreasing trend in the prevalence of HBV infection was seen after the implementation of EPI, which started in 2003. According to the most current research, which was conducted in 2017, the reported prevalence of HBV infection in Bangladesh was 3.85%.

Fig. 5. Prevalence trend of HBV infection in Bangladesh over time after the implementation of EPI.
Discussion
Worldwide, hepatitis B is a major public health concern and around 3.5% of people are identified as chronic HBV carriers according to a report of 2015 [Reference Asrani29]. To obtain the latest data on the prevalence of hepatitis B in the general population of Bangladesh, this systematic review and meta-analysis were performed based upon the published data in the years 1995–2021. According to our systematic review, the pooled prevalence of HBV infection in the general population of Bangladesh was 4% (95% CI 3.0–5.1), which is considered as a low intermediate prevalence rate and indicated a higher prevalence rate in Bangladesh than the global prevalence rate (3.5%). It is also mentioned that a decreasing trend in the prevalence of HBV infection was observed in Bangladesh after the implementation of EPI, which started in 2003 (Fig. 5). Most of the studies (8 studies) included in the present study showed a prevalence rate in the range of 5–8% (high intermediate prevalence), 4 studies which have a range of 2–4% (low intermediate prevalence) and 3 studies have the prevalence rate <2% (low prevalence) (Fig. 2). The scenario of other Asian countries is also variable in most studies. The reported prevalence rates in South Asian countries like Pakistan, Bhutan and Nepal were 2.76%, 5.84% and 0.9%, respectively [Reference Schweitzer2, Reference Shedain30]. Whereas, the prevalence of hepatitis B was higher in South East Asian countries of Thailand (5.1%) and Malaysia (4%) [Reference Leroi31, Reference Muhamad32]. In the case of comparison with East Asian countries, China has a higher intermediate prevalence rate (6.89%) [Reference Wang33] and Japan has a lower prevalence rate (1.02%) [Reference Schweitzer2]. Therefore, it is confirmed that the prevalence rate of HBV infection varies significantly with countries and regions. The potential causes for this discrepancy could be due to the socio-cultural status, level of awareness and infection prevention practice by the community of different countries. The identified major factors for a moderate prevalence rate of HBV infection in Bangladesh are lack of education, lack of awareness regarding HBV vaccination, limited reliable data to guide policy, poverty, lack of blood screening/cross-checking, perilous sexual activity, vertical transmission from mother to child, costly treatment of HBV infection and lack of proper health care facilities [Reference Uz-Zaman7, Reference Hasan34–Reference Sheikh37].
The findings of the research included in this study are very heterogenous, owing to the fact that they were conducted on a variety of different populations and that the screening methods used were inconsistent. However, subgroup analysis was performed to reduce this heterogeneity and provided more details on HBV infection. According to subgroup analysis, we found people of age <25 years had a 1.25 times higher prevalence of HBV infection than the people of age >25 years (OR 1.25, 95% CI 0.72, 2.17, P = 0.42). Even though younger individuals had greater vaccine coverage, the majority of children and young people had increased prevalence as a consequence of hepatitis B transmission from mother to baby, sexual activity and, most importantly, illegal drug use via intravenous injection. Recent studies reported that drug addiction is much higher among Bangladesh's young than the elderly population [Reference Uz-Zaman7, Reference Gani35]. We found hepatitis B was significantly more prevalent in married people than the unmarried/single people (OR 2.16, 95% CI 1.51, 3.10, P < 0.0001). Consistent with this study, a higher prevalence of HBV infection was reported in married people in Iran [Reference Fathimoghaddam38] and Pakistan [Reference Basit39] than the unmarried people due to the lack of awareness and education about sexual practices between husband and wife, as HBV is transported through semen and vaginal secretions [Reference Franco40]. The results of subgroup analysis also revealed that the prevalence of hepatitis B was 1.20 times higher in females than males (OR 1.20, 95% CI 0.48, 2.97, P = 0.70). Women could be infected due to unprotected sex with her husband or partners and during pregnancy, their modified immune system cannot fight against viral hepatitis load [Reference Borgia41]. In contrast, a recent study of China reported the prevalence of HBV infection was higher in males than females (5.88% vs. 5.05%) might be due to occupational risk factors, drug usage and male homosexuality [Reference Wang33].
This meta-analysis has the following limitations behind the importance of the study. The prime limitation of this meta-analysis is that most of the articles had a lower number of participants. Secondly, the inconsistency of screening methods might have contributed to the heterogeneity of pooled prevalence estimates. Finally, the information regarding subgroup analysis was only limited to gender, age and marital status, but not included other socio-economic conditions of the participants.
Conclusion
According to our report, Bangladesh has a low intermediate prevalence rate of HBV infection (4.0%) with an inflated prevalence rate in female, married and younger adults. As the analysis covered vast numbers of studies, it represents the existing prevalence and epidemiology of hepatitis B in the country that could be beneficial for public health leaders to decision-makers. More comprehensive research with larger sample sizes should be conducted to improve the understanding and identification of HBV epidemiology in Bangladesh. In order to achieve hepatitis B elimination in Bangladesh, it is recommended to improve the scope of the national immunisation programme to ensure the vaccination of people at all levels.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S0950268822000061.
Financial support
This study didn't receive any specific grant from any organisations like the public or commercial.
Conflict of interest
The authors declare no conflict of interest.
Ethical standards
Not required.
Informed consent
No informed consent was necessary.
Data availability statement
The authors confirm that the datasets used for this study are available on request from the corresponding author.