Impact statement
This study of the Health Action for Psychiatric Problems In Nigeria including Epilepsy and SubstanceS (HAPPINESS) Intervention, which aims to integrate mental health into primary care settings, adds to the growing evidence of the feasibility, preliminary evidence of possible effectiveness, and impact of the WHO’s Mental Health Gap Action Programme-Intervention Guide (mhGAP-IG)-based efforts to scale-up mental health services in Nigeria. The HAPPINESS intervention led to a significant reduction in 9-item Patient Health Questionnaire scores among patients from baseline (Md = 9.5) to 6 months (Md = 3.0) post-intervention (z = 80.5, p < 0.001), with a large effect size (r = 0.8). Additionally, it specifically highlights the potential role of mobile technology and telemedicine in supporting capacity building in mental health in Nigeria and making evidence-based interventions accessible at the community level. A critical component of task-sharing and collaborative care model is clinical supervision and support by mental health specialists. The HAPPINESS intervention’s approach to supervision and clinical support for trained healthcare workers can be the model for a national scale-up. It is important to conduct a larger, cluster-randomized trial of the HAPPINESS intervention to further test its definitive effectiveness, sustainability, scalability and cost-effectiveness.
Social media summary
The HAPPINESS Intervention increases access to care by integrating mental health care into primary health care through task sharing.
Introduction
With only 250 psychiatrists for 200 million people, one psychologist per 2 million people, one psychiatric nurse per 103,000 people, and no dedicated government funding for community mental health centers (Esan et al., Reference Esan, Abdumalik, Eaton, Kola, Fadahunsi and Gureje2014; APN, 2023), Nigeria exemplifies the severe lack of mental health specialists and services that is prominent in many low- and middle-income countries (LMICs) (Kakuma et al., Reference Kakuma, Minas, van Ginneken, Dal Poz, Desiraju, Morris, Saxena and Scheffler2011; WHO, 2020). The reasons for this paucity of mental health specialists and services are multifactorial, but an effective approach to mitigating the shortage is training nonmental health professionals to deliver packages of mental health care in a collaborative, stepped-care, task-sharing approach (Patel et al., Reference Patel, Weiss, Chowdhary, Naik, Pednekar, Chatterjee, De Silva, Bhat, Araya and King2010; Padmanathan and De Silva, Reference Padmanathan and De Silva2013; Raviola et al., Reference Raviola, Naslund, Smith and Patel2019). These trained nonspecialists are typically supported both virtually and remotely by mental health specialists through regular consultation, referral, supervision, and continuing education as has been demonstrated in the Project Extension for Community Healthcare Outcomes (ECHO) initiative across multiple countries (Serhal et al., Reference Serhal, Arena, Sockalingam, Mohri and Crawford2018; Sockalingam et al., Reference Sockalingam, Arena, Serhal, Mohri, Alloo and Crawford2018).
In line with this approach, Nigeria’s strategic policy on mental health articulated in 1991 is to integrate mental health care into primary, secondary and tertiary care settings with the responsibility of implementation delegated to local governments (Nigeria FMH, Reference Mo1991). The policy was revised in 2013 to accommodate logistic challenges of integrating mental health care within the primary health system and to make specific recommendations for primary, secondary, and tertiary care (Federal Ministry of Health, 2013). These recommendations included: (a) at the primary care level, having psychotropic medications from the essential drug list, strengthening community outreach, awareness, rehabilitation and referral/consultation processes; (b) at the secondary care level, setting up inpatient and outpatient mental health services at all hospitals and strengthening inter-sectoral governance structures to manage mental, neurological and substance (MNS) use disorder services and (c) at the tertiary care level, supporting secondary care services with mental health expertise. Furthermore, the revised policy encouraged the use of public-private partnerships to further innovate mental health service delivery. Finally, it recommended adequate training, retraining and continuing professional development activities on screening, identification, treatment and referral of MNS disorders at all levels of care for all direct care medical personnel.
Despite these long-standing, well-articulated policy goals, mental health integration into general health settings in Nigeria has not been fully implemented due to factors related to funding, training and supervision of trained nonmental health specialists (Saraceno et al., Reference Saraceno, van Ommeren, Batniji, Cohen, Gureje, Mahoney, Sridhar and Underhill2007; Petersen et al., Reference Petersen, van Rensburg, Kigozi, Semrau, Hanlon, Abdulmalik, Kola, Fekadu, Gureje and Gurung2019). Of the few states in Nigeria (Benue, Lagos, Osun and Ogun) that have successfully implemented state-wide mental health training for primary health care workers, the results are favorable, showing improvement in knowledge, enhanced capacity to treat common mental disorders and improvement in patients’ clinical symptoms (Adebowale et al., Reference Adebowale, Umukoro, Gater, Akinhanmi, Ogunlesi, Helme, Wood and Ibikunle2014; Gureje et al., Reference Gureje, Abdulmalik, Kola, Musa, Yasamy and Adebayo2015; Adewuya et al., Reference Adewuya, Ola, Coker, Atilola, Fasawe and Ajomale2019; Ryan et al., Reference Ryan, Nwefoh, Aguocha, Ode, Okpoju, Ocheche, Woyengikuro, Abdulmalik and Eaton2020).
The World Health Organization’s Mental Health Gap Action Programme-Intervention Guide (mhGAP-IG), which supports this approach to scale-up treatment and services for MNS disorders in LMICs (Keynejad et al., Reference Keynejad, Spagnolo and Thornicroft2021), has been contextualized and piloted in Nigeria and utilized in programme implementation in these states (WHO, 2010; Abdulmalik et al., Reference Abdulmalik, Kola, Fadahunsi, Adebayo, Yasamy, Musa and Gureje2013; Keynejad et al., Reference Keynejad, Dua, Barbui and Thornicroft2018). Core components of the mhGAP-IG approach are primary healthcare center (PHC)-level screening, identification, and treatment of MNS disorders, training for nonmental health specialists, specialist supportive supervision for the trainees and strengthening referral pathways between trained health care workers and specialists (WHO, 2015). However, some implementation research questions have not been addressed. For instance, few studies have focused on fidelity and sustainability of the mhGAP-IG protocols and other manualized processes for assessment, treatment and referral delivered by trained, nonspecialist workers (Gureje et al., Reference Gureje, Abdulmalik, Kola, Musa, Yasamy and Adebayo2015; Davies and Lund, Reference Davies and Lund2017; Onofa et al., Reference Onofa, Adebowale and Gater2023). There is also a need to identify how best to efficiently access specialist support, supervision, consultation and referral for trained clinicians providing mental health care in nonmental health specialist centers (Naslund et al., Reference Naslund, Kalha, Restivo, Amarreh, Callands, Chen, Gomez-Restrepo, Hamoda, Kapoor and Levkoff2021). Furthermore, there is limited data on the rate of adoption of mhGAP-IG-based collaborative care models in primary, secondary and tertiary care centers in Nigeria (Timothy et al., Reference Timothy, Umukoro, Maroh, Gater, Adegboyega, Daniel, Funmi, Modupe, Karmorudeen and Smith2018; Faregh et al., Reference Faregh, Lencucha, Ventevogel, Dubale and Kirmayer2019).
This study evaluates the implementation and patient-level clinical impact of the mhGAP-IG-based Health Action for Psychiatric Problems including Epilepsy and SubstanceS (HAPPINESS) intervention pilot integrating mental health into PHCs in Imo State Nigeria from October 2019 to September 2021. We hypothesized that the HAPPINESS intervention would be delivered with fidelity by the trainees and that the intervention would improve patients’ symptoms as measured by the 9-item Patient Health Questionnaire (PHQ-9) and Brief Psychiatric Rating Scale (BPRS).
Methods
Study design
This study used a quasi-experimental design (single cohort with pre- and post- measures) to assess changes in psychiatric symptoms using patients’ scores on the PHQ-9 and BPRS, which were documented by PHC clinicians at baseline and 6 months post-intervention for all patients treated through the HAPPINESS intervention. PHQ-9 is a multipurpose instrument for screening, diagnosing, monitoring, and measuring the severity of depression (Levis et al., Reference Levis, Benedetti and Thombs2019). BPRS is a rating scale used to measure psychiatric symptoms such as psychosis, depression and anxiety (Overall and Gorham, Reference Overall and Gorham1988). Both the PHQ-9 and BPRS have been validated and widely used for research in Nigeria (Adewuya et al., Reference Adewuya, Ola and Afolabi2006; Gureje et al., Reference Gureje, Oladeji, Montgomery, Bello, Kola, Ojagbemi, Chisholm and Araya2019). Although the mhGAP-IG training includes modules on other mental disorders, substance use disorders and epilepsy, for the purpose of this pilot study, we chose to use the PHQ-9 and BPRS to measure symptoms of depression, anxiety and psychosis as these are the most common presentations in the community. Measures of HAPPINESS intervention feasibility (site recruitment, training completion); adoption (rate of implementation) and fidelity (delivery of screening, assessment, treatment, referral and consultation according to the intervention protocol) were assessed through administrative data review completed at 12 months post HAPPINESS intervention roll out at each primary care site (Appendix 1 of the Supplementary Material).
Setting
Imo State has a population of about 4 million people (National Population Commission, 2020) with 527 PHCs staffed by 453 nurses, 76 community health officers and 864 community health extension workers spread across the State’s urban and rural areas. Data obtained during the needs assessment indicated that each center had a part-time or full-time covering physician. Additionally, health services at the PHCs are free at point of care although access to essential medications is limited and patients often pay for medications out-of-pocket. During planning meetings, 3 additional PHCs were added to the initial 10 PHCs from 5 local government areas of the state that were selected for the pilot study. The PHCs were selected based on the availability of staff in the clinics and to ensure equitable geopolitical representation of the three senatorial districts of the state as recommended by the stakeholders. A total of 25 nurses (10 with prior in-service training in mental health and 15 with no prior in-service training in mental health) from 13 participating PHCs were invited for the HAPPINESS intervention mhGAP-IG 5-day training and 1-day 6-month refresher training, including training on the use of mobile apps for continuing medical education, specialist consultation and referral. All HAPPINESS intervention clinical services including screening, assessment, treatment and care coordination were delivered in the community PHCs. As is generally the case in Imo State, most of the patients live within 1–2.5 km from the participating PHCs (Charles-Akalonu et al., Reference Charles-Akalonu, Ikpong and Amadi2021), making the HAPPINESS intervention accessible.
Study population and sample
The target population for the study was all patients attending PHCs for routine medical care and services in the participating 13 PHCs. Medical records reviewed during the planning phase of the project showed that the PHCs served a total of 2,756 adult patients in the preceding 12 months. These patients came for services like antenatal care, immunization and general medical care. The study sample included adults who screened positive for MNS disorders based on clinical assessment, PHQ-9 and BPRS scores.
Health care workers training
Details of the HAPPINESS intervention components, including Training, Refresher Training, Clinical Practice, Support Supervision, Community Engagement and the Drug Revolving Fund (Appendix 2 of the Supplementary Material), have been previously published and summarized in Figure 1 (Chu et al., Reference Chu, Roxas, Aguocha, Nwefoh, Wang, Dike and Iheanacho2022). In summary, for the mhGAP-IG training, we chose the following modules: Essential Care and Practice, Depression, Psychoses/Mania, Epilepsy and Substance Use Disorders and made relevant adaptations based on local needs and context. The training was conducted in English, the official language in Nigeria, and delivered in person, facilitated by the mhGAP-IG master and trained trainers. It was an 8-h per day, 5-day training (with scheduled breaks) with didactics, group workshops and role-plays. Post-training certification was based on 100% attendance to all training activities, a score of at least 90% on the post-training knowledge test, and a “pass” grade on the observed practice session as scored by trainers according to pre-set competency rubrics (patient assessment, patient education, diagnosis and treatment).

Figure 1. Key components of the Health Action for Psychiatric Problems in Nigeria including Epilepsy and SubstanceS (HAPPINESS) intervention.
Post-training support supervision, consultation and referral
Supportive supervision was conducted in person (when feasible) and virtually (WhatsApp® video call/regular mobile phone call) with the covering psychiatrist completing at least once a month, 1-h check-in with the HAPPINESS intervention-trained nurses in the PHCs. Consultation and referral between the PHCs nurses and supporting psychiatrists were conducted in person when feasible or using one of three mobile applications: WhatsApp® Messaging, voice or video call,“one2one” and/or VULA health app (Gloster et al., Reference Gloster, Mash and Swartz2021; one2one), depending on internet availability. The one2one and VULA mobile telehealth applications were specifically developed for LMICs in Africa to improve access to health care, particularly in community settings with few numbers of specialists. For the HAPPINESS intervention pilot, primary health nurses were trained to use both apps to deliver clinical care, consult and make specialist referrals when feasible and appropriate. Continuing medical education was conducted at least once a month using WhatsApp®Group Messaging or Zoom® Meetings. Detailed data collection on the staff, patients’ and specialists’ utilization of mobile technology in the HAPPINESS intervention is ongoing.
Clinical tool kit and standard operating procedure
The HAPPINESS intervention Clinical Tool Kit and Standard Operating Procedure outlined screening, assessment and treatment protocol. It also included clinical documentation, data entry, appointment management, referral and consultation processes (Appendices 1 and 2 of the Supplementary Material).
Data collection
Using the HAPPINESS project implementation checklists, guided by Proctor et al.’s implementation outcomes framework (Proctor et al., Reference Proctor, Silmere, Raghavan, Hovmand, Aarons, Bunger, Griffey and Hensley2011) and chart review, data were abstracted from training reports, PHC monthly reports (prepared by the nurses as part of their routine PHC reports), clinic registers of new patients and notes on treatment and follow-ups (Figure 2). Patients’ diagnoses and scores on PHQ-9 and BPRS questionnaires at baseline and 6 months post-intervention were documented and collated using a project data sheet.
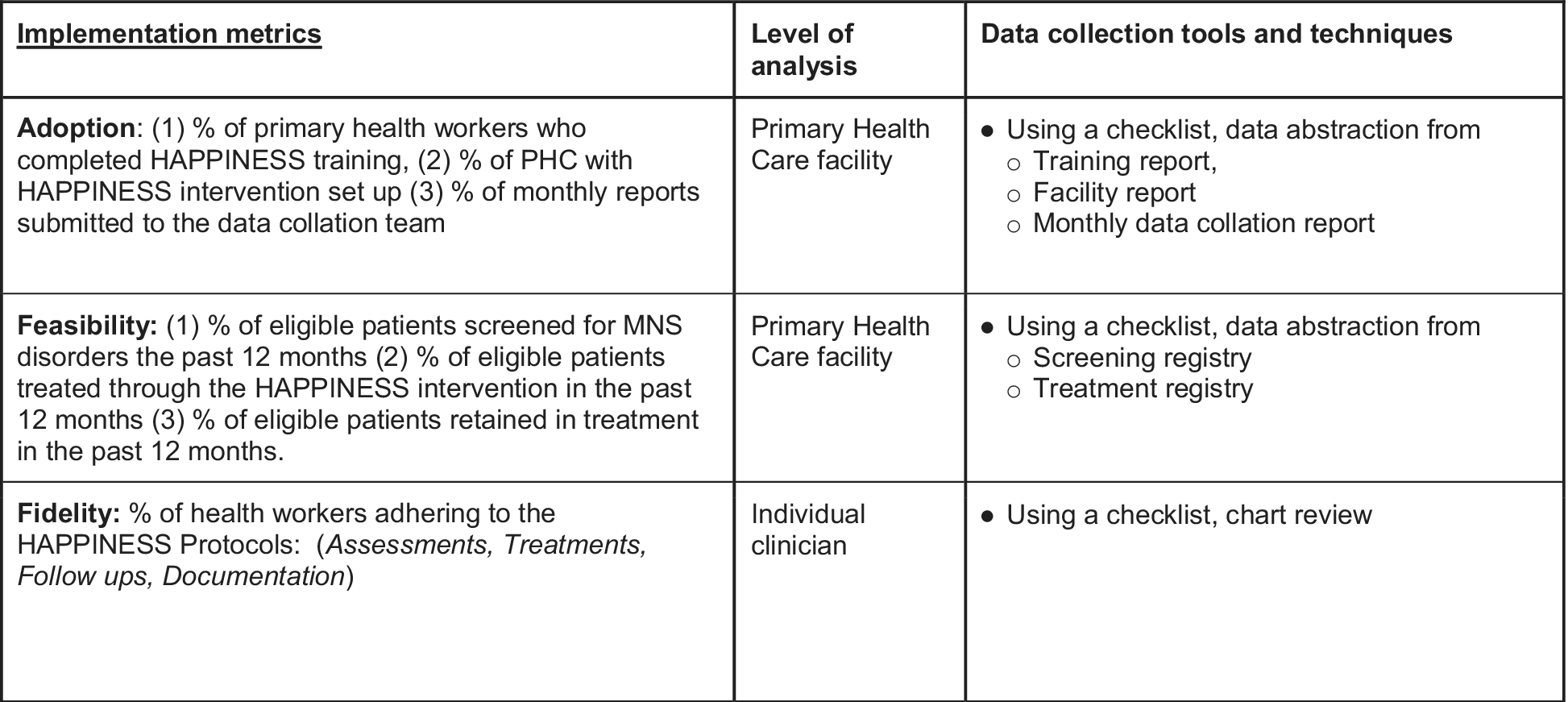
Figure 2. Implementation data collection metrics and tools.
Data analysis for clinical outcomes
We conducted the Mann–Whitney U and Kruskal–Wallis tests, which are nonparametric statistical tests used to compare medians of independent samples, to compare differences between sex, marital status, presence of anxiety and/or depression and nurse type for baseline or post-intervention PHQ-9 and BPRS scores, separately. We also conducted the Wilcoxon signed-rank test, which is a nonparametric test used to compare medians of dependent samples to compare baseline or post-intervention median scores for the PHQ-9 and BPRS overall and separately per category. We used the R statistical software (Thomas et al., Reference Thomas, Vaughan and Lello2013) to conduct all analyses and calculated associated effect sizes, which are the rank-biserial correlation coefficient (r) for Wilcoxon signed-rank, the standardized difference between two groups’ ranks (dividing the test statistic by its maximum value, which is the product of the Ns for the two groups) for Mann–Whitney U (Conroy, Reference Conroy2012) and eta-squared (η2) for Kruskal–Wallis.
The study was approved by Yale University Institutional Review Board (#2000022691) and Imo State University Teaching Hospital’s Ethics Committee.
Results
All invited 25 primary care nurses from 13 primary care clinics, drawn from 5 out of the 27 Local Government Areas of Imo State, completed the HAPPINESS intervention training in the assessment and management of the following MNS priority conditions: depression, mania/psychosis, epilepsy and substance use disorders. The HAPPINESS intervention was successfully implemented in 11 out of the 13 primary care clinics (84%). Two clinics could not implement the intervention at their sites because the trained nurses at those sites unexpectedly relocated. Out of the expected 132 monthly reports, 6 were missing from one clinic and 126 reports were obtained from the 11 active clinics over the 12-month pilot period (completion rate of 95%), which is a good measure of service penetration.
A total of 1,573 primary care clients were screened for MNS disorders over the 12-month period, with 196 identified and treated for MNS conditions. At 6 months, 178 patients (91%) were engaged in treatment, and at 12 months, 168 patients (86%) were still engaged in treatment.
A random chart review of 44 patient records (4 from each clinic) to assess fidelity to the HAPPINESS intervention protocol using the clinical tool kit checklist (Appendix 1 of the Supplementary Material) showed completion of Assessments, Treatments, Follow ups and Documentation in 36 of the records (81%).
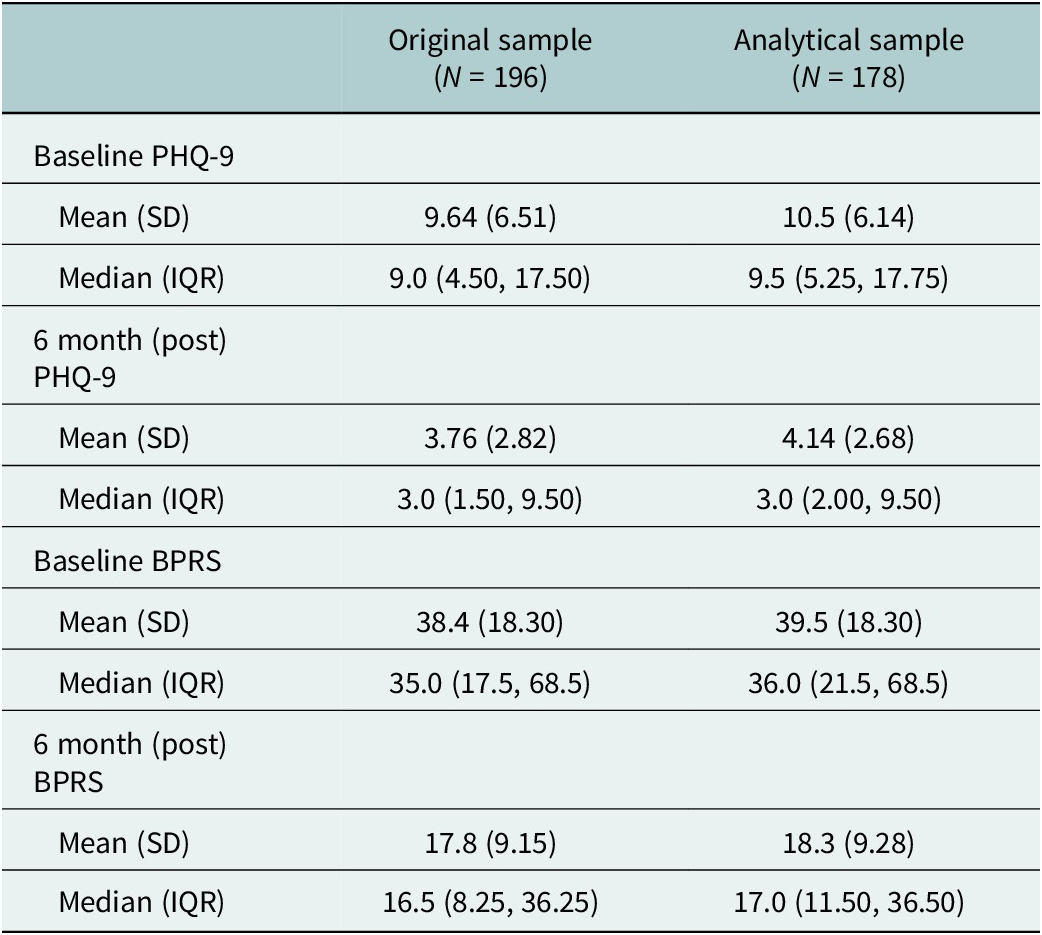
Out of the data collected from 196 patients, only 178 had complete records of baseline and post-intervention PHQ-9 and BPRS and could be used in the analysis. Table 1 shows the demographic and other relevant clinical characteristics of the overall sample and the analytical sample. The analytical sample’s mean age was 37.5 years, 53.4% of individuals identified as female, and most individuals were single (52.2%) or married (42.7%). Over a quarter of the patients received care from the HAPPINESS intervention mhGAP-trained nurses with prior psychiatric in-service training (Psych Nurses) (26.4%), and the rest received care from HAPPINESS intervention mhGAP-trained nurses with no prior psychiatric in-service training (Non-Psych Nurses) (73.6%). For psychological diagnoses, 36% of the sample had anxiety and/or depression, 39.3% had psychosis, 21.3% had epilepsy and 7.9% had substance use disorder. Table 2 shows the mean and median overall PHQ-9 and BPRS scores at baseline and at 6 months post-intervention for the original and analytical samples. Overall, the PHQ-9 and BPRS mean and median scores decreased post-intervention, with slightly higher scores in the analytical sample.
Table 1. Demographic and medical characteristics of the original and analytical samples

Note: The number of individuals and percent of the sample are reported in parentheses.
* Medical diagnoses included malaria, hypertension, diabetes and chronic pain.
Table 2. Overall means and averages of PHQ-9 and BPRS scores
The data for PHQ-9 and BPRS were not normally distributed and skewed, as assessed by Shapiro–Wilk tests for pre- (baseline) and 6 months post-intervention (pre-PHQ-9: W = 0.957, p < 0.001 and post-PHQ-9: W = 0.827, p < 0.001; pre-BPRS: W = 0.917, p < 0.001 and post-BPRS: W = 0.886, p < 0.001), thus our decision to conduct Mann–Whitney U (MacFarland et al., Reference MacFarland, Yates, MacFarland and Yates2016) and Kruskal–Wallis tests (Ostertagova et al., Reference Ostertagova, Ostertag and Kováč2014).
Results from the Wilcoxon signed-rank test (Table 3) showed a statistically significant reduction in PHQ-9 scores from baseline (Md = 9.5) to 6 months (Md = 3.0) post-intervention (z = 80.5, p < 0.001), with a large effect size (r = 0.8). It also showed a statistically significant reduction in BPRS scores from baseline (Md = 36.0) to 6 months (Md = 17.0) post-intervention (z = 128.5, p < 0.001), with a large effect size (r = 0.9). The same was seen for each sex category and nurse type, with significant differences between baseline and post-intervention scores that have a large effect size.
Table 3. Wilcoxon signed-rank test results for baseline and post-intervention, overall and by sex and nurse type

Note: Effect sizes close to 1 suggests a strong association (close to 0 suggests a weak or no association).
* Denotes a significant p-value at the 0.05 level.
The results of the Mann–Whitney U and Kruskal–Wallis tests (Table 4) show that baseline PHQ-9 scores alone were not significantly different by sex, nurse type, or marital status categories. It was, however, significantly different between those with and without a depression or anxiety diagnosis, with a large effect size (U = 4,471, p < 0.05, effect size = 0.613). Baseline BPRS scores were not significant for any of the categories.
Table 4. Mann–Whitney U and Kruskal–Wallis test results for baseline and post-intervention scores by sex, nurse type, depression or anxiety diagnosis, and marital status
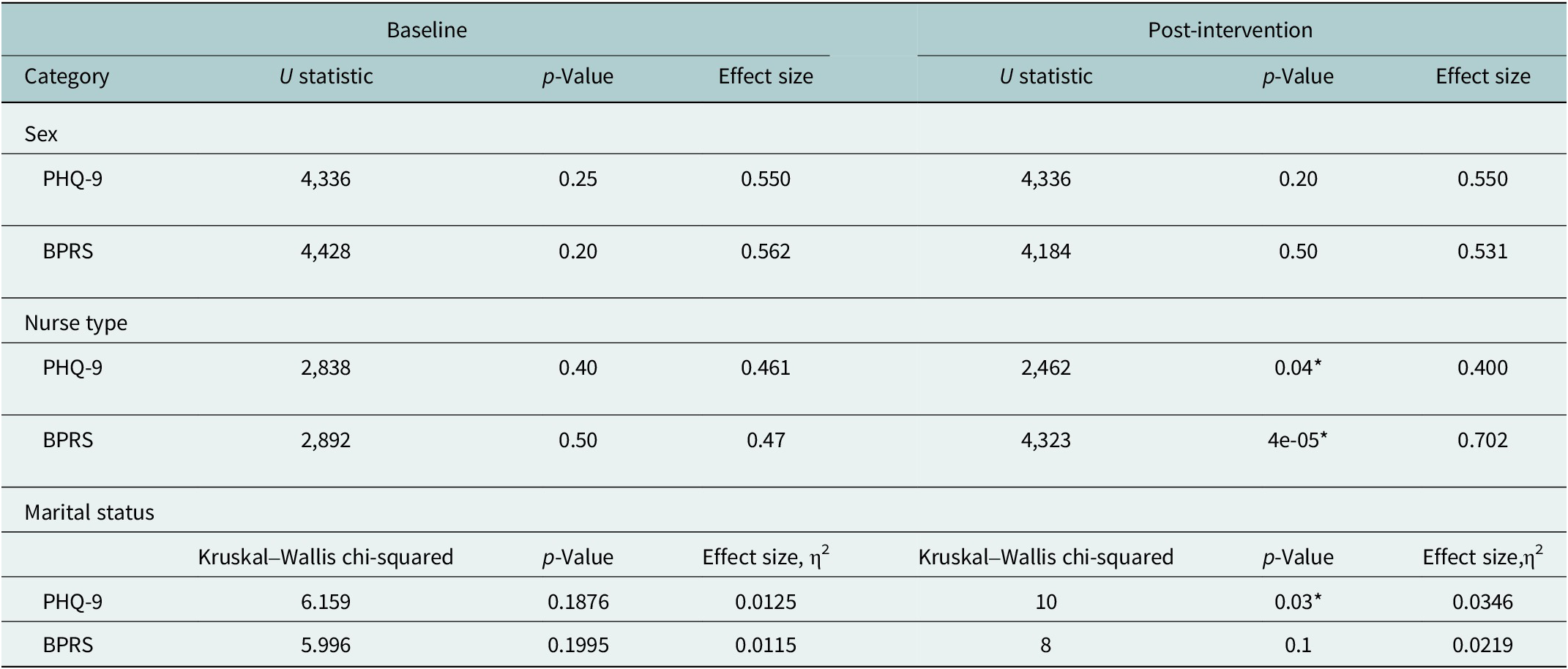
Note: All comparisons for two subcategories (sex, nurse type, depression or anxiety) were analyzed using the Mann–Whitney U test. Marital status included more than two categories; thus, it was analyzed using the Kruskal–Wallis test. For the Mann–Whitney, effect sizes near 1 suggests a large difference between the groups (close to 0 suggest small or negligible differences). For Kruskal–Wallis, η2 between 0.01 and 0.06 indicates small effect), between 0.06 and 0.14 is moderate and greater than 0.14 is large.
* Denotes a significant p-value at the 0.05 level.
On the other hand, post-intervention PHQ-9 scores alone were not significantly different by sex or depression or anxiety diagnosis. However, they were significantly different by nurse type with a moderate effect size (U = 2,462, p < 0.05, effect size = 0.400) and marital status with a small effect size (χ2(4) = 10, p < 0.05, η2 = 0.0346). Post-intervention BPRS scores were not significantly different by sex, depression or anxiety diagnosis or marital status. However, they were significantly different by nurse type with a large effect size (U = 4,323, p < 0.05, effect size = 0.702).
Discussion
Results from the pilot implementation of the HAPPINESS intervention showed a high rate of adoption (84%), penetration (service report completion rate of 95%) and fidelity (81%) as well as patient engagement (91%) and retention in care at 12 months (86%). These promising results add to the initial findings of high acceptability and feasibility of the HAPPINESS intervention (Chu et al., Reference Chu, Roxas, Aguocha, Nwefoh, Wang, Dike and Iheanacho2022). They are also in keeping with other studies of mhGAP-based integration of mental health into primary care in Nigeria and other LMICs (Gureje et al., Reference Gureje, Abdulmalik, Kola, Musa, Yasamy and Adebayo2015; Petersen et al., Reference Petersen, van Rensburg, Kigozi, Semrau, Hanlon, Abdulmalik, Kola, Fekadu, Gureje and Gurung2019). These implementation outcomes also provide needed data and basis for further development and testing of the HAPPINESS intervention in a larger cluster randomized controlled trial (RCT) to determine its definitive effectiveness compared to usual care and potential for sustainment and scale-up nationally.
The HAPPINESS intervention also led to significant improvements in patients’ BPRS and PHQ-9 scores at 6 months post-intervention across all demographics and diagnoses. This finding adds to the growing evidence that collaborative, task-shifting, stepped-care model of mental health care delivery using the WHO’s mhGAP-IG can be an effective approach to scaling up mental health in Nigeria and increasing access to evidence-based care in the community for people with common mental disorders (Adewuya et al., Reference Adewuya, Ola, Coker, Atilola, Fasawe and Ajomale2019; Gureje et al., Reference Gureje, Oladeji, Montgomery, Bello, Kola, Ojagbemi, Chisholm and Araya2019). The HAPPINESS intervention is particularly relevant as its key components: remote specialists’ supervision, consultation and referral as well continuing medical education for the trainees, utilized telemedicine and mobile technology. The option of remote, virtual supervision, consultation and continuing education allowed the inclusion of psychiatrists in Nigeria and Nigerian psychiatrists in the diaspora. This model of remote expert clinical support and continuing education has been well-studied in the Project ECHO model in high-income countries and LMICs (Hager et al., Reference Hager, Hasselberg, Arzubi, Betlinski, Duncan, Richman and Raney2018; Sockalingam et al., Reference Sockalingam, Arena, Serhal, Mohri, Alloo and Crawford2018). It offers a pathway for many psychiatrists and mental health specialists originally from LMICs currently in the diaspora to potentially support clinical education, capacity building and mental health care delivery in their home countries.
When looking at improvement in patients’ scores on the PHQ-9 and BPRS across time, patients who were treated by nurses with prior mental health experience and those who were treated by nurses without prior mental health experience had significantly different baseline and post-intervention scores, showing that both groups of patients benefited from the intervention over time. However, further comparison of post-intervention PHQ-9 and BPRS scores between the two groups of patients show that the treating nurses with prior mental health experience had a substantial impact on the scores. The baseline and post-intervention medians, along with the results of the Mann–Whitney U (Tables 2 and 4) show that there is a high probability that a randomly chosen patient who was treated by a nurse with prior mental health experience will have a lower (and more favorable) post-intervention score than a randomly chosen patient who did not receive care from a nurse with prior mental health experience. The magnitude of this effect was larger for BPRS than PHQ-9. Altogether, this means that although patients treated by either nurse type improved over time, post-intervention scores were lower among individuals who received care from nurses with prior mental health experience (a difference that was not present at baseline). While we are unable to determine exactly the reason for this difference, we speculate that prior experience in treating patients with mental illness, including the use of basic counseling skills gained through specialized training and practice, may have contributed to the nurses’ capacity to provide more robust psychosocial support. It also highlights the need for the trainees to continue to practice the skills they learned during this pilot project to solidify their learning and further enhance their clinical competence (Kazantzis et al., Reference Kazantzis, Calvert, Orlinsky, Rooke, Ronan and Merrick2010).
As expected, baseline PHQ-9 scores significantly differed between those with and without a depression/anxiety diagnosis, with a moderate effect size. This difference was not seen in post-intervention scores, indicating that improvement in symptoms following treatment for those with depression or anxiety led to reduced PHQ-9 scores, and the psychosocial support delivered as part of the HAPPINESS intervention benefitted even those without depression or anxiety. This supports the need to include psychosocial support and counseling as part of a basic package of care for people with MNS use disorders, irrespective of specific diagnoses. Post-intervention PHQ-9 scores were also significantly different by marital status, but the small effect size indicates that only a small proportion of the variance in the PHQ-9 scores can be explained by marital status.
Limitations
First, this was a quasi-experimental study with baseline and 6 months post-intervention assessments. Therefore, there is a risk of confounding, which limits the confidence in establishing causality compared to an RCT. However, the study provides robust data to support a larger cluster RCT that can support measures to mitigate against confounders.
Second, due to the non-normal nature of the data, we could not conduct parametric tests (i.e., a mixed ANOVA) to compare the main and interaction effects between time (baseline and post-intervention) and different categories or factors of interest (e.g., gender).
Third, although we attempted to include representative primary care centers from the three geopolitical zones of the state, this was a relatively small patient sample size compared to the general population of the state. Thus, we are unable to confidently generalize the findings.
Fourth, although there were significant improvements in PHQ-9 scores among patients who received treatment, we were unable to determine if the improvement in symptoms of anxiety, depression or psychosis were due to psychosocial support plus medication or psychosocial support alone. In depression, for example, the general recommendation is “watchful waiting” and psychoeducation for PHQ-9 scores of 5–9 and counseling, follow-up and/or pharmacotherapy for PHQ-9 scores of 10–14 and above (Iglesias-González et al., Reference Iglesias-González, Aznar-Lou, Peñarrubia-María, Gil-Girbau, Fernández-Vergel, Alonso, Serrano-Blanco and Rubio-Valera2018); however, the data entry in our pilot sites did not differentiate those who received psychoeducation plus medication or psychoeducation/counseling alone based on their scores. In our subsequent planned, larger RCT, we plan to gather more details to enable the evaluation of the effects of psychosocial support versus the addition of medication management.
Finally, due to budget constraints, we were only able to assess limited implementation outcomes, including measures of adoption, fidelity and retention in treatment. As we plan and propose a larger, more robustly funded study, we will include additional implementation outcome measures focused on sustainability, cost-effectiveness and potential for a national scale-up using a mixed-method approach.
Conclusion
This pilot implementation study shows that it is feasible to integrate mental health into primary care with fidelity and a high adoption rate. It also shows that primary care nurses trained with mhGAP-IG and provided specialist clinical support physically and remotely using mobile technology can lead to improvement in patients’ symptoms with a high rate of retention and engagement in care.
Open peer review
To view the open peer review materials for this article, please visit http://doi.org/10.1017/gmh.2024.4.
Supplementary material
The supplementary material for this article can be found at http://doi.org/10.1017/gmh.2024.4.
Data availability statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Acknowledgments
The authors are grateful to their volunteer project support staff especially Ms. Obianuju Ukaigwe for her dedication and diligence in coordinating data collection from all participating primary health care centers. The authors would also like to acknowledge the support provided Imo State Primary Care Development Agency, Imo State University Teaching Hospital, Imo State Ministry of Health and HHC Foundation.
Author contribution
TI, CA, EN and CD were responsible for the design of the HAPPINESS intervention and training. TI and CA also contributed to data collection. CC and TI conducted data collation and data analysis. All authors provided significant input and approved the final manuscript.
Financial support
Funding for this study was provided by the Yale Institute of Global Health Hecht Faculty Award.
Competing interest
The authors declare none.
Ethics statement
Ethical approval was granted by Yale University’s Institutional Review Board and Imo State Teaching Hospital’s ethics committee. Both institutions assessed that the research posed no more than minimal risk of harm to subjects and involves no procedures other than administrative, clinical chart review and data abstraction.












Comments
To the Editor, Global Mental Health
September 3, 2023
Dear Editor,
We wish to submit an original research article entitled “Integrating mental health into primary care in Nigeria: Implementation outcomes and clinical impact of the HAPPINESS intervention” for consideration by Global Mental Health journal.
We confirm that this manuscript has not been published elsewhere, nor is it currently under consideration by another journal.
In this paper, we evaluate implementation outcomes of the HAPPINESS intervention pilot that utilized the World Health Organization’s Mental Health Gap Action Programme Intervention Guide (mhGAP-IG) to train primary care teams to provide treatment for mental, neurological and substance use disorders in the community. Mobile technology and telehealth apps were used for clinical support, consultation, and referral.
We believe that this manuscript is appropriate for publication by Global Mental Health because it transparently highlights the challenges and successes of a mental health innovation and system strengthening strategy in a low and middle-income country. Our study comes at a time in Nigeria when a new mental health legislation has been passed with emphasis on integration of mental health care into primary care. Thus, our findings show a potential model for scaling up mental health care across the country.
All authors have approved the manuscript and agree with its submission. We also have no competing interests to disclose.
Thank you for your consideration of this manuscript.
Sincerely
Theddeus Iheanacho, M.D.
Associate Professor of Psychiatry, Yale University School of Medicine
Visiting Professor of Psychiatry,
Imo State University
Director, Yale Global Mental Health Program
Department of Psychiatry,
Yale University School of Medicine
Director, Global Mental Health Promotion Program
Center for Methods in Implementation and Prevention Science (CMIPS)
Yale School of Public Health
Chair of Psychiatry and Director of Behavioral Health Services
Trinity Health of New England/Saint Francis Hospital
Email: theddeus.iheanacho@yale.edu
Tel: +14752029380
https://medicine.yale.edu/psychiatry/happiness/