Introduction
On 11 March 2020, the World Health Organization (WHO) declared that the coronavirus disease 2019 (COVID-19) outbreak could be characterized as an international pandemic as the virus had spread increasingly worldwide (WHO, 2020). COVID-19 is a severe and persistent virus, by 19 March 2021, the morning after the Israeli government announced the fourth step out of the third nationwide lockdown, 826 217 Israeli citizens had been tested positive for COVID-19, with 6071 deaths, most of them older adults (Ministry of Health, Israel, 2021). The aging population in particular has been one of the most vulnerable, with a high number of older adults infected globally (Niu et al., Reference Niu, Tian, Lou, Kang, Zhang, Lian and Zhang2020). Preliminary data have attested that COVID-19 has adverse psychological outcomes (Qiu et al., Reference Qiu, Shen, Zhao, Wang, Xie and Xu2020) such as depressive symptoms, anxiety, and high levels of worries and stress (Wang et al., Reference Wang, Pan, Wan, Tan, Xu, Ho and Ho2020a; Palgi et al., Reference Palgi, Shrira, Ring, Bodner, Avidor, Bergman, Cohen-Fridel, Keisari and Hoffman2020b). Likewise, COVID-19 has resulted in fear (Ahorsu et al., Reference Ahorsu, Lin, Imani, Saffari, Griffiths and Pakpour2020a, Reference Ahorsu, Lin and Pakpourb), depression, anxiety (Palgi et al., Reference Palgi, Shrira, Ring, Bodner, Avidor, Bergman, Cohen-Fridel, Keisari and Hoffman2020b), and death anxiety (Ring et al., Reference Ring, Greenblatt-Kimron and Palgi2020) among the older population. However, older adults suffering from chronic medical conditions related to increased risk of death due to COVID-19 were not found to be at higher risk for depressive and anxiety symptoms (Palgi et al., Reference Palgi, Shrira, Ring, Bodner, Avidor, Bergman, Cohen-Fridel, Keisari and Hoffman2020b).
In a systematic review of 43 studies on the mental health consequences of the COVID-19 pandemic, the researchers found a high level of post-traumatic stress symptoms and depressive symptoms among COVID-19 patients (Vindegaard & Benros, Reference Vindegaard and Benros2020). Moreover, patients with preexisting psychiatric disorders experienced a deterioration of symptoms. Studies revealed an increase in psychiatric symptoms such as depression, anxiety, psychological distress, and poor sleep quality among health care workers. Studies also showed lower psychological well-being and higher levels of anxiety and depression in the general public than before the COVID-19 pandemic (Vindegaard & Benros, Reference Vindegaard and Benros2020). Nevertheless, there is minimal evidence available on the mental health implications of prior medical pandemics (Tsang et al., Reference Tsang, Scudds and Chan2004; Sood, Reference Sood2020). Consequently, an urgent plea to the academic world was made to conduct trauma research during the COVID-19 pandemic (Horesh and Brown, Reference Horesh and Brown2020). This is particularly important among older adults, which the trauma literature has understudied throughout the years. The present study, therefore, aimed to provide data that would shed light on the role that views of aging play in the traumatic distress experienced among the older population during the COVID-19 pandemic. Specifically, the study aimed to examine subjective accelerated aging as moderating the link between COVID-19 health worries and peritraumatic distress among older adults.
Peritraumatic distress
Peritraumatic distress relates to cognitive and emotional distress throughout and immediately following a traumatic event (Brunet et al., Reference Brunet, Weiss, Metzler, Best, Neylan, Rogers, Fagan and Marmar2001; Palgi et al., Reference Palgi, Dicker-Oren and Greene2020a). A person's peritraumatic encounter is determined by several determinants, such as the continuance of exposure and proximity to the event (Kannis-Dymand et al., Reference Kannis-Dymand, Carter, Lane and Innes2019). Peritraumatic distress symptoms have been positively correlated with posttraumatic stress disorder (PTSD) symptoms (e.g. Thomas et al., Reference Thomas, Saumier and Brunet2012; Palgi et al., Reference Palgi, Dicker-Oren and Greene2020a) after both human-made (Simeon et al., Reference Simeon, Greenberg, Knutelska, Schmeidler and Hollander2003) and natural catastrophes (Basoglu et al., Reference Basoglu, Kihk, Salcioglu and Livanou2004; Hollifield et al., Reference Hollifield, Hewage, Gunawardena, Kodituwakku, Bopagoda and Weerarathnege2008). Prior examinations of mass events, such as natural catastrophes, typically are accompanied by adverse effects on mental health, in particular with PTSD (Makwana, Reference Makwana2019). It has already been noted that the unexpected outbreak of a disease bears a threat to the mental health of the population, as demonstrated in China during the initial stages of the COVID-19 breakout (Ahmed et al., Reference Ahmed, Ahmed, Aibao, Hanbin, Siyu and Ahmad2020). Therefore, the current pandemic is a high-risk emergency for psychiatric morbidity (Sood, Reference Sood2020), with a major concern being the development of PTSD (Banerjee, Reference Banerjee2020). As mentioned, peritraumatic distress is known to be associated with PTSD (e.g. Palgi et al., Reference Palgi, Dicker-Oren and Greene2020a); thus, we examined peritraumatic distress among older adults, who are considered at higher risk for severe COVID-19 complications (Emami et al., Reference Emami, Javanmardi, Pirbonyeh and Akbari2020) and may, therefore, report COVID-19 worries. We thus sought to explore the relationship between COVID-19 health worries and peritraumatic distress among older adults.
COVID-19 health worries
Worries refer to fundamental cognitive features of anxiety, characterized by the repeated occurrence of ideas, thoughts and images about possible adverse events, which are relatively uncontrollable (Borkovec et al., Reference Borkovec, Robinson, Pruzinsky and DePree1983; Williams, Reference Williams2013). Worries may impact well-being and mental health if they appear repeatedly, resulting in a harmful level of anxiety (Reis et al., Reference Reis, Ramiro and de Matos2019). Nevertheless, worries are not confined to patients with anxiety disorders or to a particular emotion, but are rather relationally rooted in distinct settings (Lutz and White, Reference Lutz and White1986). Worries have been found to be a focus in health-related issues, with numerous studies reporting an association between worries and medical illnesses, such as cancer patients (e.g. Roy et al., Reference Roy, Janse, Janssen, Meara, Presley, Kneuertz, Ferris and Bridges2019), patients with heart failure (e.g. Bagheri et al., Reference Bagheri, Yaghmaei, Ashktorab and Zayeri2018), Crohn's disease patients (Wåhlin et al., Reference Wåhlin, Stjernman and Munck2019), and individuals suffering from asthma (e.g. Islamovic et al., Reference Islamovic, Silver and Reznik2019). During an influenza outbreak, 10–30% of the general public reported being very or moderately worried about the probability of contracting the virus (Rubin et al., Reference Rubin, Potts and Michie2010). In line with this notion, recent studies have indicated that since the outbreak of COVID-19, levels of fears and worries have increased (Lin, Reference Lin2020). The rise in health worries is understandable, due to the relatively high morbidity risk of COVID-19 (Kobayashi et al., Reference Kobayashi, Jung, Linton, Kinoshita, Hayashi, Miyama, Anzai, Yang, Yuan, Akhmetzhanov, Suzuki and Nishiura2020; Sood, Reference Sood2020), the vagueness of the situation, fears about the safety of the new vaccine in Israel, the leading country to operate a COVID-19 vaccine program, regarding the vaccine's long-term effects (Ministry of Health, Israel, 2021), and the need for quarantine for undetermined periods (Ahmed et al., Reference Ahmed, Ahmed, Aibao, Hanbin, Siyu and Ahmad2020).
Since the COVID-19 breakout, constant worrying has already been noted in the population, with differences in severity (Sihag and Kumar, Reference Sihag and Kumar2020). Moreover, as old age has been determined to be a major risk factor for COVID-19 complications (Emami et al., Reference Emami, Javanmardi, Pirbonyeh and Akbari2020; Wang et al., Reference Wang, He, Yu, Hu, Bao, Liu, Zhou and Jiang2020b), it has also been proposed that older adults are expected to have higher stress levels during the COVID-19 pandemic (Kar, Reference Kar2020). The rationale for examining the potential link of accelerated aging with COVID-19 worries is based on several issues. First, higher levels of stress were observed in older adults due to COVID-19 (Kar, Reference Kar2020). Second, older adults are at higher risk for COVID-19 complications (Santesmasses et al., Reference Santesmasses, Castro, Zenin, Shindyapina, Gerashchenko, Zhang, Kerepesi, Yim, Fedichev and Gladyshev2020). Third, PTSD which is closely linked with peritraumatic stress has been addressed as a secondary COVID-19 outcome (Dutheil et al., Reference Dutheil, Mondillon and Navel2020). Fourth, the recent findings (Palgi, Reference Palgi2020) showing positive linkage between trauma exposure, challenges of aging, and accelerated aging.
Subjective accelerated aging
The term subjective age refers to how old people perceive themselves to be (Stephan et al., Reference Stephan, Sutin and Terracciano2015). Studies have reported an association between subjective age and adverse mental and physical outcomes (e.g. Choi and DiNitto, Reference Choi and DiNitto2014), including traumatic exposure (Schafer, Reference Schafer2009), acute stress disorder (Hoffman et al., Reference Hoffman, Shrira and Grossman2015) and PTSD symptoms (Solomon et al., Reference Solomon, Helvitz and Zerach2009; Hoffman et al., Reference Hoffman, Shrira, Cohen-Fridel, Grossman and Bodner2016). An older subjective age has also been reported as both moderating the PTSD-posttraumatic growth link (Palgi, Reference Palgi2016), as well as strengthening the adverse effect of posttraumatic symptoms on successful aging (Shrira et al., Reference Shrira, Palgi, Ben-Ezra, Hoffman and Bodner2016).
Based on the subjective weathering hypothesis, which asserts that subjective aging is a key aspect of the stress process (Benson, Reference Benson2014), it may be assumed that people tend to cognitively divert their internalized clock and form an older age identity due to traumatic events (Hoffman et al., Reference Hoffman, Shrira, Cohen-Fridel, Grossman and Bodner2016; Palgi, Reference Palgi2016). Moreover, a similar psychological process paralleling the biological process of accelerated aging occurs (Palgi, Reference Palgi2020). Accordingly, age identity has been reported not as a defined measure, but rather an identity that may oscillate during difficult life events (Schafer and Shippee, Reference Schafer and Shippee2010). Based on these theories, Palgi (Reference Palgi2016) suggested that coping with trauma exposure, while coping with the challenges of aging, may bring people to feel their aging process is accelerated. This has been demonstrated among ex-prisoners of war with high levels of PTSD symptoms, who demonstrated shortened telomere length – an indicator of neural accelerated aging (Tsur et al., Reference Tsur, Levin, Abumock and Solomon2018) as well as an older subjective age (Avidor et al., Reference Avidor, Benyamini and Solomon2016). Yet, given the abovementioned association between objective and subjective measures of accelerated aging, indicating the awareness people have to their physical aging process, subjective accelerated aging can be examined directly (at a single time point) to assess one's feeling of aging acceleration across time. This assumption is based on previous studies, which examined the effects of subjective age on older adults, and which found subjective age to be a better predictor of psychological and health-related functioning (Kotter-Grühn et al., Reference Kotter-Grühn, Kleinspehn-Ammerlahn, Gerstorf and Smith2009) than chronological age was. Nevertheless, to the best of our knowledge, only two studies to date specifically asked whether participants experienced accelerated aging (Bergman and Palgi, Reference Bergman and Palgi2020; Palgi, Reference Palgi2020); results reveal that accelerated aging was linked with both higher levels of PTSD symptoms and lower levels of positive mental health with this single item querying subjective accelerated aging in a cross-sectional manner.
In summary, based on the above, the present study aimed to assess if COVID-19 worries are linked with peritraumatic distress symptoms in older adults. Additionally, we asked if subjective accelerated aging would moderate this link. It was first hypothesized that higher levels of COVID-19 health worries would be related to peritraumatic distress among older adults. The second hypothesis maintained that subjective accelerated aging would moderate this association. Namely, relative to lower levels of accelerated aging, for persons with higher levels of accelerated aging, there would be a stronger positive relationship between COVID-19 health worries and peritraumatic distress among older adults.
Method
Participants and procedure
The current study used data drawn from an online survey in Israel between 16 March and 14 April 2020. On 14 April 2020, the last day of data collection, 12 046 Israeli citizens were tested positive for COVID-19, with 123 deaths, most of them older adults (https://www.worldometers.info/coronavirus/country/israel/). Participants included 277 older adults between the ages of 60 and 92, with an average age of 69.58 (s.d. = 6.73). The majority of the participants were women (n = 191, 69.0%), married/living with a partner (n = 204, 73.6%), and had tertiary academic education (n = 201, 72.8%). Almost half of the participants self-rated their health as good/very good (n = 178, 64.5%). Less than half of the participants reported having chronic diseases which are associated with increased medical complications due to COVID-19 (n = 115, 42.9%). The data collection process began after receiving IRB approval from the Ethics Committee at Bar-Ilan University. All participants signed an electronic informed consent form before completing the questionnaire. The background characteristics of the study sample are presented in Table 1.
Table 1. Descriptive statistics for the study variables (N = 277)

a Women.
b Married or living with partner.
c Has chronic diseases.
*p < 0.05, **p < 0.01, ***p < 0.001.
Measures
Background characteristics included age, gender, marital status rated as 1 (single, widow, divorced) and 2 (married or leaving with a partner), level of education was classified into one of six categories in line with the International Standard Classification of Educational Degrees (ISCED-97) (United Nations Educational, Scientific, and Cultural Organization, 1997) ranging from 1 (without formal education) to 6 (formal tertiary education) and health status rated from 1 (not at all good) to 5 (very good). In addition, participants were asked if they suffered from chronic diseases (i.e. cardiovascular disease, diabetes, chronic respiratory disease, hypertension, and cancer), which have been associated with increased medical complications due to COVID-19.
Exposure to COVID-19 was assessed by respondents answering yes or no to six questions regarding exposure to the coronavirus (i.e. currently or previously being in quarantine, having had coronavirus, knowing people, family members, or friends in quarantine or who had coronavirus). The exposure score was the sum of events the participant was exposed to.
COVID-19 health worries were assessed by a four-item scale designed for this study. Participants rated their levels of health worries about self or close relatives and friends developing COVID-19, or infecting others by COVID-19 (i.e. how worried are you about: being infected by the coronavirus, about people close to you likely to have been infected by the coronavirus, about one of your family members likely to be infected by the coronavirus, about carrying the coronavirus, and about infecting those close to you) on a five-point scale from 1 (completely disagree) to 5 (completely agree). In this study, Cronbach's α for COVID-19 health worries was 0.78.
Subjective accelerated aging was assessed by a single item (adapted from Palgi, Reference Palgi2020). Participants rated their subjective accelerated aging on a five-point scale, by answering the question ‘On the whole, I feel that due to the COVID-19: 1 (my aging rate is very slow) to 5 (my aging rate is very fast)’. Higher scores indicate higher subjective accelerated aging.
Peritraumatic distress symptoms were assessed by the 13-item Peritraumatic Distress Inventory (PDI; Brunet et al., Reference Brunet, Weiss, Metzler, Best, Neylan, Rogers, Fagan and Marmar2001). Participants rated their symptoms by referring to COVID-19 outbreak on a five-point scale from 0 (not at all) to 4 (extremely true). The peritraumatic distress score was the sum of ratings, with higher scores indicating greater distress. Cronbach's α in a previous study that used the Hebrew translation was 0.87 (Palgi et al., Reference Palgi, Dicker-Oren and Greene2020a). In this study, Cronbach's α for peritraumatic distress was 0.84.
Data analysis
First, Pearson correlations were conducted to establish preliminary associations between the study variables. Next, examination of the moderation model was conducted using the IBM SPSS statistic package (SPSS-25) to conduct a hierarchical regression analysis, where peritraumatic tress was regressed on the following variables across steps: Background characteristics were entered in the first step of the multiple hierarchical regression, COVID-19-related covariates (chronic diseases and exposure to COVID-19) in the second step, COVID-19 health worries and subjective accelerated aging in the third step, and finally the interaction between COVID-19 health worries and subjective accelerated aging was entered in the fourth step. The moderation model (Model 1) was tested, using the PROCESS 3.1 macro for SPSS (Hayes, Reference Hayes2017). A preliminary multicollinearity test was performed to confirm that the regression hypotheses were met. Results showed that the tolerance of all independent variables (age, gender, education, self-rated health, marital status, chronic diseases, health worries, and subjective accelerated aging) ranged from 0.654 to 0.970; the variance inflation factor ranged from 1.031 to 1.526, revealing no multicollinearity (O'Brien, Reference O'Brien2007).
Results
COVID-19 health worries were positively associated with subjective accelerated aging (r = 0.15, p < 0.05) and with peritraumatic distress (r = 0.40, p < 0.01). Subjective accelerated aging was positively associated with peritraumatic distress (r = 0.38, p < 0.01). It was important to control for these background characteristics as they were associated with at least one of the study's variables and there has been some variability regarding participants' exposure levels to various forms of COVID-19 stressors (e.g. isolation) (for further information, see Table 1).
In order to examine the study's hypotheses, a multiple hierarchical regression was conducted. The results showed that older adults who reported higher levels of COVID-19 health worries also reported higher levels of peritraumatic distress symptoms (β = 0.345, t = 5.879, p < 0.001). In addition, those who reported higher levels of subjective accelerated aging also reported higher levels of peritraumatic distress symptoms (β = 0.301, t = 5.134, p < 0.001). Finally, the interaction between COVID-19 health worries and subjective accelerated aging predicted peritraumatic distress (B = 2.186, β = 0.299, t = 5.298, p < 0.001). This interaction explained an additional 7.74% of the variance (see Table 2).
Table 2. Summary of the moderation model for variables predicting peritraumatic distress among older adult (N = 277)
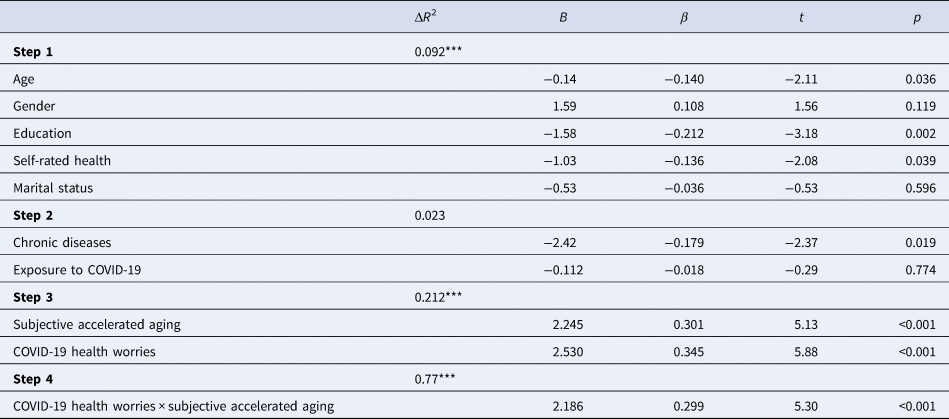
Total R 2 = 0.404***.
Note: Gender (dummy): 1 – male, 2 – female.
*p < 0.05, **p < 0.01, ***p < 0.001.
Probing this interaction, it was found that for older adults who reported a slow rate of aging (i.e. 1 s.d. below the mean; lower subjective accelerated aging), each additional point in COVID-19 health worries score was associated with a non-significant increase of 0.72 points in peritraumatic distress symptoms (B = 0.72, t = 1.35, p = 0.18). However, for older adults reporting a faster rate of aging (i.e. 1 s.d. above the mean; high subjective accelerated aging), each additional point in COVID-19 worries score was associated with a significant increase of 4.64 points in the level of peritraumatic distress symptoms (B = 4.64, t = 8.16, p < 0.001) (see Fig. 1).
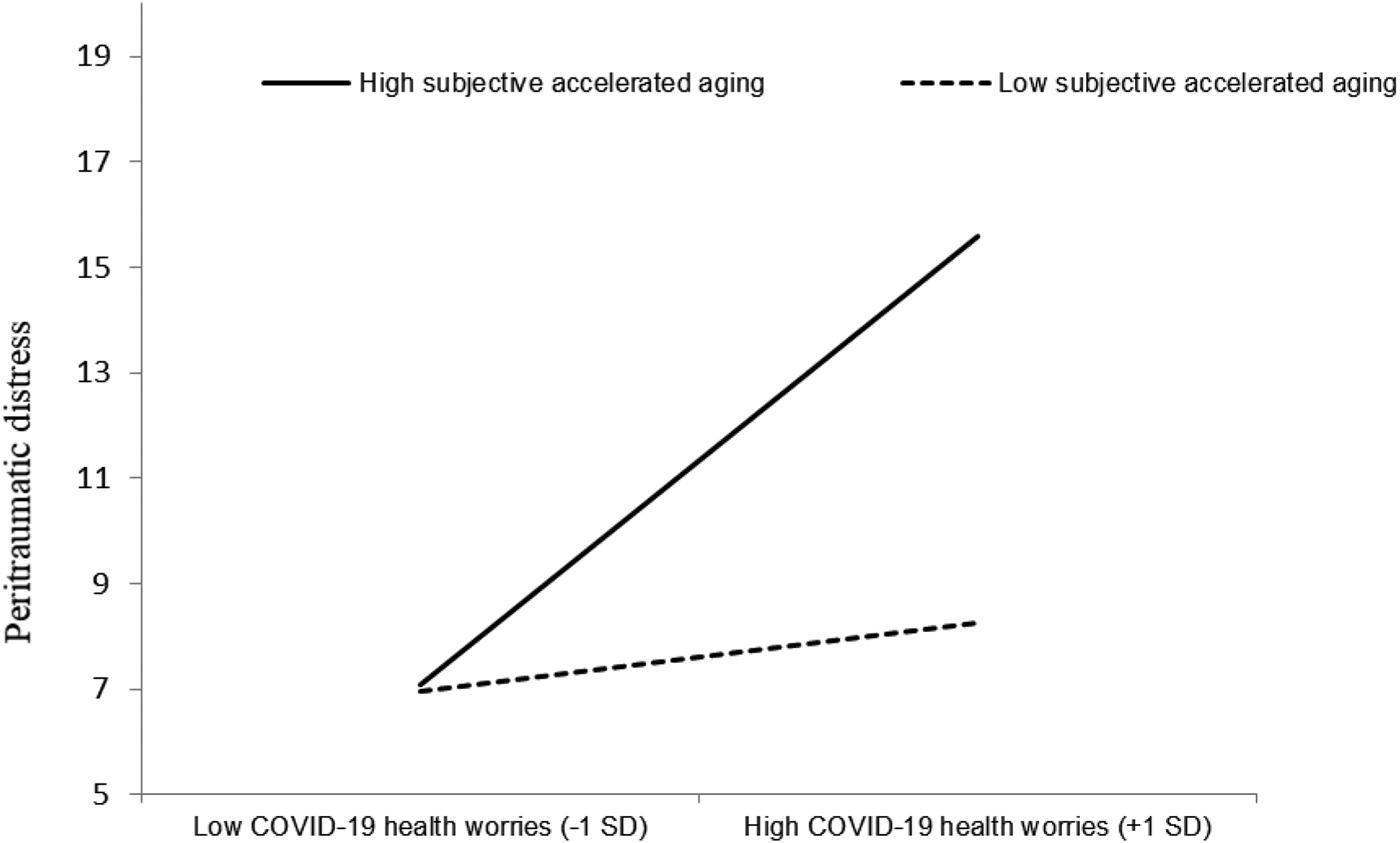
Fig. 1. The moderating effect of subjective accelerated aging on the association between health worries and peritraumatic distress.
Discussion
To the best of our knowledge, the present study is the first to examine the relationship between COVID-19 health worries and peritraumatic distress among older adults, and in particular, the moderating role of subjective accelerated aging in this relationship. As hypothesized, older adults who reported higher levels of COVID-19 health worries also reported higher levels of peritraumatic distress symptoms. Moreover, those who felt they were aging fast (i.e. higher subjective accelerated aging levels) reported a higher level of peritraumatic distress symptoms. Finally, the interaction between these measures accentuates that the relationship between COVID-19 health worries and peritraumatic distress was stronger among people who reported the feeling they were aging faster. The significance of these findings will now be discussed in detail.
In line with the first hypothesis, high levels of COVID-19 health worries among older adults were found to be related to higher levels of peritraumatic distress. This association highlights the physical and psychological distress older adults experience during a pandemic. The present findings are in line with the association found between exposure to mass trauma events, such as natural catastrophes and adverse mental health outcomes, in particular PTSD (Makwana, Reference Makwana2019). In addition, the present findings are consistent with preliminary findings among adults during the pandemic that showed associations between higher levels of COVID-19 health worries and anxiety (Bergman et al., Reference Bergman, Cohen-Fridel, Shrira, Bodner and Palgi2020) and between higher levels of COVID-19 health worries and death anxiety (Ring et al., Reference Ring, Greenblatt-Kimron and Palgi2020).
Consistent with our second hypothesis, older adults who felt they were aging faster also reported higher levels of peritraumatic distress. The findings underscore the effect of subjective accelerated aging when coping with stressful life events, such that older adults who sense their aging has accelerated are less resilient in the context of coping with COVID-19. The current findings align with the association found between subjective age and neurobiological accelerated aging (e.g. Tsur et al., Reference Tsur, Levin, Abumock and Solomon2018), as well as the association found between subjective accelerated aging and PTSD symptoms (Palgi, Reference Palgi2020). In addition, as noted by Palgi (Reference Palgi2020), the concept of subjective accelerated aging appears to be an integrated part of the concept of subjective views of aging (Wurm et al., Reference Wurm, Diehl, Kornadt, Westerhof and Wahl2017) and these findings demonstrate its utility as an additional aspect of this concept.
In interpreting the interaction found in the present study between COVID-19 health worries and subjective accelerated aging, it can be speculated that older adults who felt they were aging faster were more vulnerable to the negative concomitants of COVID-19 worries, i.e. those who viewed themselves as rapidly progressing toward old age, an age at higher risk for severe COVID-19 illness, had no buffer against COVID-19 worries. Therefore, it seems that under the current context, where medical circumstances emphasized older ages as a risk factor for a severe illness, feeling one's aging process as slower is a potential resource that can render one more immune to the effects of health worries. It may be that the term accelerated aging is oversensitive to physical health worries due to the health risk involved. Moreover, peritraumatic distress was not associated with any vulnerability measures of the COVID-19 pandemic (i.e. chronological age, chronic disease, exposure to COVID-19 stressors), but rather only to the subjective measure of subjective accelerated aging. This finding coincides with previous studies that revealed that older chronological age is not associated with worse mental health outcomes during the COVID-19 pandemic (e.g. Pieh et al., Reference Pieh, Budimir and Probst2020). In this light, the present study highlights the effect that subjective accelerating aging and excessive worrying may have on mental health outcomes in the older population during a pandemic (see Fig. 1).
The study has several limitations. First, it used a cross-sectional design; therefore, causality cannot be inferred from the current findings. Second, the study sample was based on an online design, and may be biased toward older adults with technological knowledge. Third, there was no measurement of pre-pandemic levels of health worries or levels of PTSD symptoms (the participants were asked to report their level of health worries and peritraumatic symptoms since the COVID-19 outbreak). Fourth, COVID-19 health worries were assessed by a scale that was previously published (Bergman et al., Reference Bergman, Cohen-Fridel, Shrira, Bodner and Palgi2020; Ring et al., Reference Ring, Greenblatt-Kimron and Palgi2020; Grossman et al., Reference Grossman, Hoffman, Palgi and Shrira2021), nevertheless this measure is not standardized. Future studies should use standardized measures (e.g. Ahorsu et al., Reference Ahorsu, Lin, Imani, Saffari, Griffiths and Pakpour2020a, Reference Ahorsu, Lin and Pakpourb; Bitan et al., Reference Bitan, Grossman-Giron, Bloch, Mayer, Shiffman and Mendlovic2020; Lee, Reference Lee2020; Taylor et al., Reference Taylor, Landry, Paluszek, Fergus and McKay2020). Finally, similar to other views of aging (e.g. distance to death, subjective age), accelerated aging is also a single item. Future studies may focus on unpacking this concept into further potential domains.
Conclusions
The present study is the first to examine the concept of subjective accelerated aging and its relationship with peritraumatic distress during the COVID-19 pandemic among older adults. The findings have theoretical and practical implications for the prevention of peritraumatic distress during the COVID-19 pandemic, as well as other natural disasters.
Theoretically, the findings rejoin earlier results reviewed above and further demonstrate that similar to the biological process of accelerated aging, there appears to be a psychological process by which individuals assess the rate of their aging, which seems to be linked with psychiatric symptoms. We recommend future studies to examine the directionality of this relationship and its contribution to mental health. We also recommend that future prospective studies investigate the mechanisms connecting subjective and objective measures of accelerated aging.
On a practical level, the rise in health worries since the COVID-19 outbreak is understandable (Kobayashi et al., Reference Kobayashi, Jung, Linton, Kinoshita, Hayashi, Miyama, Anzai, Yang, Yuan, Akhmetzhanov, Suzuki and Nishiura2020); therefore, the findings in the current study offer preliminary support for the potential relevance of suitable interventions during the COVID-19 pandemic that are aimed at reducing health worries. In particular, the findings underscore the importance of identifying health worries among older adults, and more so among those who experience subjective accelerated aging in the face of the COVID-19 pandemic. The combination of health worries together with subjective accelerated aging pinpoints a group at higher risk for developing increased levels of peritraumatic distress symptoms. Preventative interventions for adverse psychological effects can be implemented among this group. Finally, another potential approach is to focus on the subjective feeling of accelerated aging; the development of suitable interventions for promoting the feeling of aging in a less accelerated fashion should be promising for older adults during stressful life events.
Financial support
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Conflict of interest
None.
Ethical standards
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.








