Introduction
There is increasing concern about high clinical and subclinical rates of psychological distress and mental health disorders among young people (Hyland et al. Reference Hyland, Vallières, Shevlin, Bentall, Butter, Hartman, Karatzias, Martinez, McBride, Murphy and Fox2022). The global burden of disease from the World Health Organisation (WHO) indicates that psychiatric disorders are the leading cause of disability for young people aged 10–24 years (WHO, 2022). In Ireland, the prevalence of mental health disorders is high, with 18.5% of the population recorded as having a mental health disorder in 2016 (OECD/European Union, 2016). It is estimated that over half of Ireland’s population will have encountered a mental health disorder before the age of 25 (McGorry, et al. Reference McGorry, Trethowan and Rickwood2019).
A significant percentage of young people experiencing difficulties with mental health do not seek or receive treatment, despite evidence that previous experience with mental health strongly predicts later mental health problems and that receiving support from a health professional significantly reduces later need for treatment (Fusar-Poli Reference Fusar-Poli2019). Many factors contribute to this, including poor awareness of the symptoms of mental health problems among parents and young people, resulting in a lack of help-seeking. In addition, there are structural and cultural flaws within existing care systems, such as the unavailability of electronic health records in the health system, a discontinuity between child and adult services and a lack of an integrated financial management system for mental health (parliamentary question PQ22266 21) (McGorry et al. Reference McGorry, Mei, Chanen, Hodges, Alvarez-Jimenez and Killackey2022).
Community-based mental health services for young people in Ireland
In recent years, there has been a global effort to improve psycho-social interventions for young people by increasing access to and engagement with services (O’Reilly et al. Reference O'Reilly, O'Brien, Moore, Duffy, Longmore, Cullinan and McGrory2022). To this end, several models have been developed internationally to provide youth-specific services focusing on early interventions for subsyndromal forms of mental health disorders in a community-based, non-judgmental setting (Ambresin et al. Reference Ambresin, Bennett, Patton, Sanci and Sawyer2013; McGorry et al. Reference McGorry, Mei, Chanen, Hodges, Alvarez-Jimenez and Killackey2022). In Ireland, Jigsaw – the National Centre for Youth Mental Health (McGorry et al. Reference McGorry, Bates and Birchwood2013), has provided support for young people based on free, one-to-one clinical interventions. Since 2010, Jigsaw has provided access and care to over 62,000 young people. Similar community-based early intervention mental health services have been established elsewhere for example, in Australia (Headspace), the Netherlands (@ease), the United States (allcove) and the United Kingdom (Norfolk) (McGorry et al. Reference McGorry, Mei, Chanen, Hodges, Alvarez-Jimenez and Killackey2022).
Mindspace Mayo service
Mindspace Mayo, similar to Jigsaw, is an early intervention mental health service – funded by the Health Service Executive – that supports young people in Ireland between 12 and 25 in County Mayo through an interagency and partnership approach. The service was established in 2015 and operates under national policy and guidelines from strategies such as A Vision for Change, Connecting for Life, Healthy Ireland Framework 2013–2025 and the Healthy Ireland Strategic Action Plan 2021–2025. The Mindspace service comprises a team of healthcare professionals, including a project manager, clinical team leader, senior clinician, clinical support workers, administration support officers and youth engagement officer. Mindspace operates from the central hub in Castlebar and has two outreach sites in Ballina and Erris. The core objective of the service is to provide evidence-informed youth mental health support to individuals who display subsyndromal forms of mental health disorders and/or those at risk of developing mental health conditions.
MindSpace Mayo therapeutic service
The Mindspace model of therapeutic support is brief and evidence-informed. Referrals to the service can be made by the young person (self-referral), their families, school, local general practitioner (GP), or other health agencies/organisations. The initial assessment is based on a bio-psycho-social framework and is carried out over two sessions to determine the nature of the presenting issue, the young person’s strengths and resources, developmental issues, educational and social history and a mental state exam. The assessment also includes a thorough risk assessment. Individuals who present with moderate to severe mental health issues beyond the service’s scope are referred to another mental health service, such as CAMHS or AMHS. These cases are discussed among the team at the weekly clinical team meetings. Following this initial intake and assessment, indiviuduals are offered up to eight further sessions of goal-focused therapeutic support; the average is 5.9. All staff receive internal supervision (one-to-one) monthly and external supervision (one-to-one) monthly to maintain their own professional accreditation.
The professional qualification backgrounds of staff draw from a wide range of mental health training backgrounds, including Mental Health Nursing, Social work, Psychology (Clinical, Counselling, Educational), Counselling/Psychotherapy or Occupational Therapy with experience in mental health. In each case, clinicians came to Mindspace with previous experience of working with other clinical services. In terms of the therapeutic approach used, while the ethos of the service is to provide a solution-focused, evidence-based approach, no single therapeutic approach is adopted across the service. Instead, individual therapists offer input based on their background and expertise. Examples include psychoeducation, cognitive behaviour therapy, solution-focused brief therapy, mindfulness-based stress reduction, motivational interviewing, harm reduction and relapse prevention, person-centred counselling and guided problem-solving.
The present study
The availability of electronic records from services such as Mindspace Mayo provides important information about pathways to care and clinical response to community-based brief interventions for improving mental health and offers the opportunity to evaluate youth-focused primary care interventions. Given the recognised need for objective data to inform future delivery of youth mental health services, we analysed electronic data collected within Mindspace Mayo since it began delivering service in 2015. We aimed to describe the demographic and clinical characteristics of young people who engaged with the service, their treatment pathway, and their clinical response to the brief psycho-social intervention provided as part of routine care. We further sought to establish whether demographic or clinical variables were predictive of better treatment outcomes.
Methods
Participants
When the study commenced in April 2022, data were available for 1,343 individuals who were initially referred to the service. Those who were redirected prior to being seen by Mindspace were excluded from the analysis. The analysis was conducted on 1,184 individuals who had engaged with the Mindspace Mayo service from its inception in February 2015 until February 2022. Out of the participants, 207 individuals required continued support after the Mindspace intervention and were referred to the CAMHS or AMHS. While the services expected a full intervention to consist of between six to eight sessions, all participants who had any duration of therapeutic contact (1–8 sessions) were included in the study. The data was recorded in Mindspace’s online database system, an eCASS Salesforce platform.
Measures
Demographic variables such as age, gender, and living situation were recorded on the system. Living situation was categorised as living with family, friends, parents, alone or other. A standardised approach within the service was used to gather information regarding the presenting issue of the client by the Mindspace clinician at the time of initial assessment. Data were collected by selecting from a pre-defined list of over 40 complaints generated within the service (see Table 1). Psychological distress was measured at baseline by trained therapists using the Clinical Outcomes in Routine Evaluation (CORE) and again following brief therapeutic intervention to the Mindspace Mayo service. Referral information, including source and reason were obtained at the initial assessment. The number of sessions attended within the Mindspace Mayo service was recorded.
Table 1. Demographic and clinical information for the total sample and across age groups

The CORE was used within the Mindspace service to rate the severity of a young person’s level of psychological distress before and after receiving support from the service. Of the multiple versions of the CORE available, the two versions used within the Mindspace service were (1) the YP CORE, used to measure psychological distress in young people aged 12–16, and (2) the CORE-10, used with young people aged 17 or older. For the YP CORE, scores greater than 10 indicate clinically significant symptoms of distress in 12–13-year-old males, whereas for those aged 14–16 and for girls aged 12–16, scores greater than 15 indicate clinically significant symptoms (Twigg et al. Reference Twigg, Cooper, Evans, Freire, Mellor-Clark, McInnes and Barkham2016). For the CORE-10, scores below 10 indicate low/no distress, with clinically significant levels of distress described as follows; 10–15 indicating mild distress, 15–20 indicating moderate distress, 20–25 indicating moderately severe distress and 25–30 indicating severe psychological distress (Barkham et al. Reference Barkham, Bewick, Mullin, Gilbody, Connell, Cahill and Evans2013). Gender effects have been found for the items scores on the YP CORE, with women generally scoring higher than men, and consequently, gender-specific cut-off scores have been recommended by some authors (Evans et al. Reference Evans, Connell, Barkham, Margison, McGrath, Mellor-Clark and Audin2002; Palmieri et al. Reference Palmieri, Evans, Hansen, Brancaleoni, Ferrari, Porcelli and Rigatelli2009).
Statistical analyses
Data were analysed using the Statistical Package for Social Sciences (version 27). Descriptive statistics were calculated for demographic variables and clinical variables. A Chi-Square test was used to identify the most common source of referral, presenting complaints and living situation for the total group as well when grouped according to age (i.e.: 12–16-year-olds and 17+ year olds). A between-subjects t-test was conducted to examine differences in the CORE scores pre and post-intervention across both age groups. Between-groups ANOVA was used to examine whether CORE scores differed across males and females. Bonferroni correction was used to control for multiple testing for the separate age groups (α = 0.05/2 = 0.125). Following this, regression analyses were used to investigate whether (1) demographic and clinical outcomes would predict intervention outcomes, and (2) whether clinical distress post-intervention would be predicted by an individual’s presenting issue and/or complexity of presentation to the service. For clinical cut-off scores, participants displaying moderate-severe distress (i.e., > 15) were included for CORE-10 and YP CORE for females. For the current sample, no males aged 12–13 were reported to have scores < 15. As such, there was no need to group these individuals separately.
Results
Demographic & clinical characteristics
The main demographic and clinical characteristics of the sample are presented in Table 1. Participant ages (available for n = 1,184 individuals) ranged from 12 to 25 years (see Fig. 1).
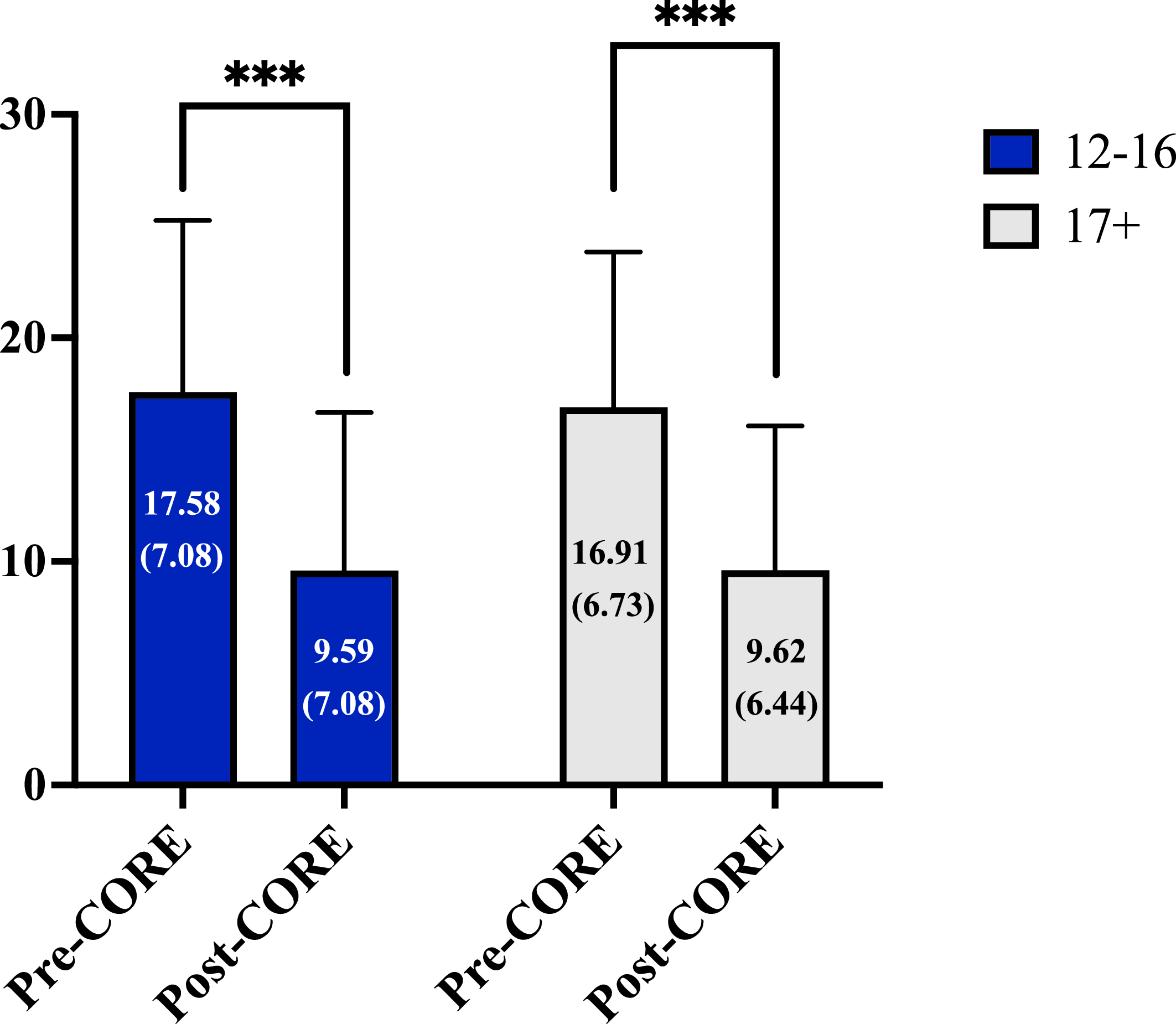
Figure 1. Psychological distress as measured by the Clinical Outcome in Routine Evaluation (CORE) pre and post-invention to the Mindspace service. Blue bars represent participants aged 12–16. Grey bars represent participants aged 17 and over.
Of the total sample, 3% (n = 36) were aged 12–14, 49% (n = 582) were aged 15–17, 29% (n = 346) were aged 18–20 and 19% (n = 219) were aged 21–25. To facilitate analysis according to the CORE measures, participants were grouped across the following age groups: between 12 and 16 years (M = 15.33, SD = 0.764) and between 17 and 25 (M = 19.27, SD = 2.27). The average number of sessions attended was 5.9 (SD = 3.86). Upon initial referral, 59% of participants aged 12–17 reported clinically significant levels of distress (males = 73, females = 235). For individuals over the age of 17, 20% (n = 93) reported low/no psychological distress, 21% (n = 98) mild distress, 23% (n = 107) moderate distress, 26% (n = 118) moderately severe distress and 10% (n = 44) reported severe psychological distress.
Referral pathway
Referral pathway information was available for 1,167 individuals. Across the total sample, the majority of individuals were either referred by a parent (40%) or self-referred (38%). A small percentage of participants were referred through the second-level education system (e.g. teacher, guidance counsellor or other member of staff, 6.9%) or through their general practitioner (5.2%). The remaining individuals were referred either by social work (1.8%), friend (1.2%) or other services, which included the following: TUSLA, Jigsaw, the Mayo Mental Health Association, the Child and Adolescent Mental Health Service (CAMHS) and the Adult Mental Health Service (AMHS). The frequency of referral pathways for males and females overlapped, but females were more likely to self-refer than males (42% versus 32%, respectively), while GP referral was slightly more prevalent among males compared to females (6.3% versus 4.8%). Increased self-referral was evident in the older age group and this difference was statistically significant (F (1, 1165) = 16.85, p < 0.001) (Figure S1).
Clinical characteristics
A wide range of presenting issues were identified across the cohort; these were grouped into sub-categories to facilitate analysis. Reasons for referral to Mindspace included mood and anxiety difficulties, relational difficulties (e.g. family difficulties), behavioural difficulties (e.g. use of alcohol and drugs), health-related issues and school-related difficulties. Individuals may have had more than one presenting complaint. Table 2 presents a breakdown of reasons for referral and the domains into which they were categorised. Percentage frequencies of the issues across each domain are displayed in supplementary Figures 1–8. Note that individuals could present with more than one reason for referral.
Table 2. Most common presenting issues to the Mindspace service subgrouped across doamins

Mood and anxiety complaints
Across the total sample, the most frequent reason for referral was related to mood and anxiety (n = 1080). Of these, anxiety represented the most common issue in this group (n = 1,015), followed by low mood (n = 680), low self-esteem (n = 515), stress (n = 514), sleep changes (n = 480) and grief/loss (n = 355). Suicidal thoughts were present in 179 individuals, and 127 individuals presented with thoughts of hurting themselves. Panic attacks (n = 216), anger (n = 203) and emotional distress (n = 288) were also common causes for initial presentation. A small number of individuals presented with an elated mood (n = 7).
Family and school-related difficulties
The second most common presenting issue was family and relational difficulties (n = 648). The most frequent issues reported were family problems (n = 425) and parent youth conflict (n = 216). Difficulties with school were the third most common reason for referral across the whole sample, and of these, the most frequent difficulty was exam stress (n = 274), followed by academic problems (n = 211) and transition difficulties (n = 192). Other issues presented included lack of social and recreational outlets (n = 175), educational difficulties (n = 149), school avoidance (n = 63) and learning difficulties (n = 35).
Behavioural and peer-related issues
In terms of behavioural issues, use of alcohol was the most common (n = 92), followed by self-injurious behaviour (n = 76), drug use (n = 66) and behavioural problems (n = 41). Among peer-related issues, bullying was the most commonly reported complaint (n = 294). A small number reported issues of peer conflict (n = 48) and exclusion (n = 6).
Other presenting complaints
In terms of health, 76 individuals reported having a health condition and 39 with a physical condition. A small number of individuals presented with anxiety surrounding COVID-19 (n = 17) and 69 individuals had health anxiety. Less common issues were around gender and sexual identity. Twenty-four individuals presented with gender identity issues, 16 with sexual orientation issues and five individuals identified as LGBTIQ+. A small minority of individuals presented with the following issues: body image (n = 74) and eating concerns (n = 6). Retrospective disclosure of abuse with noted for 15 individuals. Nineteen individuals had been subjected to sexual assault.
Clinical outcomes
Level of psychological distress at referral and immediately post-intervention was quantitatively measured using the CORE assessment measure for both age groups. At initial presentation, individuals aged 12–16 had significantly higher CORE scores (M = 17.58, SD = 7.672) compared to post-intervention (M = 9.59, SD = 7.082), and this difference was statistically significant (t (306) = 12.805, p = <0.001, Cohens d = 0.52594) (Fig. 1). A significant difference (f (3,340) = 4.387, p = 0.005) was also found between males (M = 14.97, SD = 7.13) and females (M = 17.81, SD = 7.00) aged 12–17 for the initial CORE scores. Females reported higher levels of distress. No significant differences between males and females aged 12–17 were observed on the CORE scores post-intervention (Fig. 2).

Figure 2. Clinical Outcome in Routine Evaluation (CORE) scores pre and post-intervention for males and females attending the MindSpace Mayo service in younger and older age groups.
For young people over the age of 17, a significant difference (t (273) = 15.196, p = <0.001, Cohens d = 1.3795) between initial CORE scores (M = 16.91, SD = 6.940) and post-intervention CORE scores (M = 9.62, SD = 6.439) was found, whereby lower levels of clinical distress were reported after attending the Mindspace Mayo service (Fig. 1). A significant difference was also found between males and females over the age of 17 for both the initial (f (3,638) = 5.193, p = 0.002) and post-intervention CORE scores (f (3,382) = 2.717, p = 0.044). Males reported significantly lower levels of distress compared to females. When evaluating the level of symptom reduction observed against normative data for CORE, distress was observed to reduce to minimal/non-clinical levels across the sample (Fig. 3).
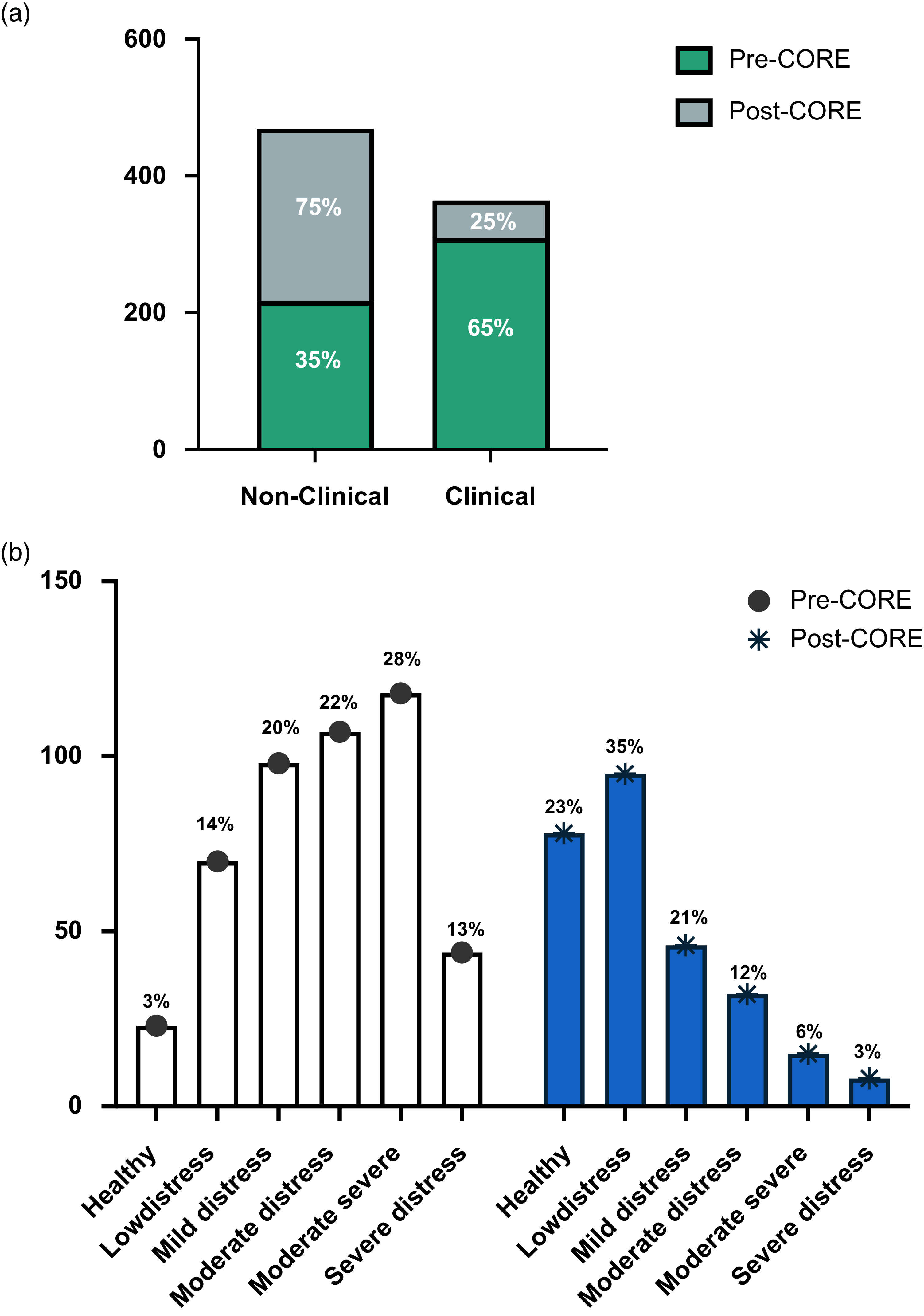
Figure 3. Changes in levels of clinical distress reported at initial assessment (pre-core) and post-intervention (post-core) to the Mindspace Mayo service. ( a ) Green bars represent level of clinical distress in individuals aged 12–17 as measured on the Clinical Outcome in Routine Evaluation (CORE) before attending the Mindspace Mayo service. Grey bars represent level of clinical distress as measured on the CORE after attending the Mindspace Mayo service ( b ) Grey bars represent level of clinical distress in individuals aged 17+ as measured on the CORE before attending the Mindspace Mayo service. Blue bars represent level of clinical distress as measured on the CORE after attending the Mindspace Mayo service.
We examined the frequency of individuals who attended the Mindspace service prior to (2015–2019) and during (2020–2021) the COVID-19 pandemic. Between 2015 and 2017, there was a steady increase in individuals attending the service, followed by a decline during the year 2018, which remained steady during the COVID-19 pandemic (see supplementary figure 10). The numbers attending the service rose again in 2021. We next compared changes in CORE scores across these two-time points using an independent samples t-test. Results revealed a significant difference (t (1, 579) = 5.28, p = 0.022), whereby a greater change in CORE scores was observed for those attending Mindspace pre-COVID (M = 7.28, SD = 6.91) compared to those who attended the service during the pandemic (M = 5.80, SD = 7.19).
Predicting outcomes
A regression analysis was used to investigate whether demographic or referral information would predict intervention outcomes. Analyses were conducted separately for the two age groups. After controlling for baseline CORE scores, neither living situation (B = −0.032, p= 0.589), referral pathway (B = 0.090, p = 0.153), nor source of referral (B = 0.074, p = 0.240) were observed to predict outcomes in those over the age of 17. Similarly, living situation (B = 0.073, p = 0.942), referral pathway (B = −0.038, p = 0.513) and source of referral (B = −0.039, p = 0.498) were not significant predictors of change in CORE score in those aged 12–17.
Following this, a logistic regression was conducted separately for younger and older age groups to examine if clinical distress post-intervention could be predicted by an individual’s presenting issue and/or complexity of presentation to the service. The criterion variable was clinically significant symptoms of distress (non-clinical/clinical) following intervention on the CORE score. For both age groups, CORE scores post-intervention were categorised into the following: scores greater than 15 were classified as clinical distress post-intervention and less than 15 were classified as non-clinical. Presenting issues included the following five sub-categories; affective, relational, behavioural, school/work and other. Complexity was based on the number of issues presented at the time of assessment as per the domains presented in Table 2. Complexity scores ranged from 0 to 7, with higher scores indicating greater complexity.
A test of the full model with all predictors was statistically reliable for the older age group (χ2 (3) = 6.388, p = 0.041). The model correctly classified 82% of individuals displaying clinical distress symptoms. Examination of the Wald statistics indicated that complexity (Wald = 3.88 p = 0.049), but not presenting issue (Wald = 1.556, p = 0.041), significantly predicted clinical distress post-intervention. In the younger age group, neither presenting issue (Wald = 2.039, p = 0.153) nor complexity (Wald = 2.26, p = 0.226) significantly predicted clinical distress on the CORE score.
Discussion
The enormous burden of mental health difficulties facing young people, reported both prior to and since the COVID-19 pandemic, continues to underline the need for access to appropriate services (McGorry et al. Reference McGorry, Mei, Chanen, Hodges, Alvarez-Jimenez and Killackey2022). At the same time, the high incidence and prevalence of mental health difficulties in young people has made scaling services to meet current needs extremely difficult. In response, a variety of organisations have evolved outside of traditional mental health services, including the Mindspace Mayo service reported here. The purpose of the present study was to provide empirical data regarding referral pathways, reasons for referral and response to intervention of young people attending the Mindspace Mayo service in the West of Ireland.
Reason for referral
Based on electronic data available for over 1,100 young people, we observed that a majority of referrals came from young people themselves and their parents, and predictably most often for issues related to mood and anxiety difficulties. This finding is consistent with other similar service evaluation reports in Ireland, including the My World Survey (Dooley and Fitzgerald Reference Dooley and Fitzgerald2012) and Jigsaw (O’Keeffe et al. Reference O’keeffe, O’Reilly, O’Brien, Buckley and Illback2015), which reported that mood and anxiety were the most frequent complaints among young people attending community-based mental health supports. Other common reasons for referral included family, school and peer-related issues. The frequency of presenting issues overlapped among males and females. However, females were more likely to present with mood and anxiety symptoms, health-related issues and other concerns (i.e., body image, sexual assault, eating concerns). These findings are largely in line with prior reports showcasing that females present with more frequent concerns of anxiety and mood (O’Keeffe et al. Reference O’keeffe, O’Reilly, O’Brien, Buckley and Illback2015; Cannon et al. Reference Cannon, Coughlan, Clarke, Harley and Kelleher2013), eating and body image-related issues (Burton et al. Reference Burton, Hamilton, Iorfino, La Monica, Scott and Hickie2022) and sexual assault (Clarke et al. Reference Clarke, Hyde and Caswell2023).
Source of referral
Similar to previous reports (O’Keeffe et al. Reference O’keeffe, O’Reilly, O’Brien, Buckley and Illback2015), the most common sources of referral to Mindspace were self and parent referrals. A notable trend was that self-referral increased with age across the group. Compared to previous research (O’Reilly et al. Reference O’Reilly, McKenna and Fitzgerald2021; O’Keeffe et al. Reference O’keeffe, O’Reilly, O’Brien, Buckley and Illback2015), a slightly higher proportion of individuals referred themselves to the Mindspace service compared with GP referrals, particularly among females. These findings suggest that young people may be more comfortable self-referring to community services. Individuals aged 15–17 were the most frequent users of the Mindspace service. Given that this is a period where a discontinuity occurs in Ireland between child and adult services (Scholz et al. Reference Scholz, Battams, Platania-Phung and Happell2019; Islam et al. Reference Islam, Ford, Kramer, Paul, Parsons, Harley and Singh2016; Paul et al. Reference Paul, Ford, Kramer, Islam, Harley and Singh2013), community-based interventions such as Mindspace may be an important mental health resource for young people seeking support during this time period or if they transitioning services. Unfortunately, this study did not have access to CAMHS/AMHS data, including wait times to draw on for analysis for comparison.
Psychological distress reduction
In terms of clinical severity, upon initial presentation to the Mindspace Mayo service, females displayed higher levels of clinical distress compared to males, which was evident across both age groups. For the older age group, levels of clinical distress were also higher in females post-intervention – findings of which are largely consistent with prior work (O’Reilly et al. Reference O’Reilly, McKenna and Fitzgerald2021). Across both age groups, reductions in CORE symptoms were both statistically and clinically significant, irrespective of differences in referral source and cause of distress. In line with similar studies (O’Keeffe et al. Reference O’keeffe, O’Reilly, O’Brien, Buckley and Illback2015; O’Reilly et al. Reference O’keeffe, O’Reilly, O’Brien, Buckley and Illback2015), ∼65% of individuals at initial assessment reported clinical levels of distress. This number reduced to 22% following intervention to the Mindspace service. Further, results revealed a greater change in CORE scores for participants attending Mindspace pre-COVID compared to those who attended the service during the pandemic. One likely explanation for this finding is that changes in the service during the pandemic (i.e., telehealth versus face-to-face contact) resulted in an overall reduction of improvement in psychological distress for those attending Mindspace.
Of note regarding reduction in clinical distress as measured by CORE, the statistically and clinically significant improvements observed did not appear to be specific to presentation type. Neither was outcome predicted by other demographic variables, including living situation or referral agency. However, the complexity of presenting issues was found to be a significant predictor of level of clinical distress post-intervention in the older age group. That is, individuals who presented with a greater number of issues at initial assessment were less likely to show improvements post-intervention as measured by the CORE score. It is worth mentioning here that high levels of self-reported distress do not necessarily indicate the presence of a mental health disorder. When a young person contacts the service with moderate/severe levels of psychological distress that suggest a significant mental health issue, Mindspace supports them in accessing a service that is more suitable for their needs.
Strengths and limitations
Strengths of this study include a large sample of young people and the wide range of information gathered, including referral sources and pathways as well as clinical outcome variables. Having data that enables us to address whether brief community-based mental health interventions are effective in alleviating distress, as was available for Mindspace, is vital to establishing whether such services adequately respond to the needs of young people. Furthermore, it underlines the value of electronic records providing information about who can access services, how they might access these and to what end.
Our study has some limitations which must be considered. First, presenting complaints of the service users were not recorded using the language of diagnosis and it was difficult to determine to what extent individuals with more severe mental health disorders. Secondly, as the data was collected by the clinicians who provided the service, ratings were not blinded and no untreated comparison group was available. In providing what was collected as part of routine care, a trade-off exists between the carefully controlled trial conditions typical of a randomised controlled trial and from which conclusions about treatment efficacy can be made, versus evidence of effectiveness from a youth mental health intervention when delivered in a real-life community setting. Further, improvement in psychological distress may have occurred due to factors unrelated to the intervention or study period i.e., due to participant characteristics, natural resolution of symptoms and external events that could not be controlled for.
Future research
While the results of this study are promising, further investment is needed for youth mental health services in Ireland as well as governance and outcome evaluation. This will help develop service delivery models that can address the full spectrum of difficulties young people face, including severe problems and high levels of psychological distress. Finally, qualitative accounts of the experiences of young people and their families (e.g. in terms of ease of access) are a key objective for future research. The fact that 40% of referrals made to the service were by family members should provide pause for thought. Frequently, once a young person turns 18 years of age, services often focus almost exclusively on the young person with little or no direct contact with parents. This is despite the fact that parents are often keen to support the young person in accessing services and the family provides an important context for the recovery journey (Goodyear et al. Reference Goodyear, Allchin, Burn, von Doussa, Reupert, Tchernegovski and Maybery2022). Whether or how family members feel included or excluded in this journey therefore represents an important focus of future study.
Conclusions
Given the limited information currently available regarding treatment delivery and outcomes in youth mental health primary care settings in Ireland, the present study based on the Mindspace Mayo service on ∼ 1,100 participants provides important new knowledge regarding sources of referral, reasons for referral and treatment effectiveness. In so doing, this study highlights the value of recording electronic data to track referral pathways, reasons for referrals and intervention response over time.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/ipm.2023.48.
Author contribution
Emma Corley and Ellen Moran contributed equally to this work.
Competing interests
None.
Ethical standard
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committee on human experimentation with the Helsinki Declaration of 1975, as revised in 2008. The study procedures were approved by the Clinical Research Ethics Committee at University Hospital Galway, and all participants were treated in accordance with legal and ethical standards, including obtaining parental consent for those under the age of 18 and ensuring standard components of informed consent.
Financial support
This study was generously funded by a Health Research Board Leadership Award to GD (grant no. RL-2020-007) and research funding provided by MINDSPACE Mayo.









