Introduction
Non-communicable diseases (NCDs) are the leading cause of mortality worldwide and are responsible for approximately 41 million deaths each year.1 Low- and middle-income countries (LMICs) are disproportionately affected by this burden, accounting for 80% of all NCD deaths and over 85% of premature NCD deaths globally.1 These patterns are predicted to increase over the next 10 years, with a 17% rise in NCD-related mortality overall and a 27% increase in the African region.2 While most premature NCD deaths are preventable, LMICs face many barriers in combatting this rise in disease prevalence, including limited access to resources, inadequate infrastructure and a lack of local health research, interventions and policies.Reference Islam, Purnat, Phuong, Mwingira, Schacht and Fröschl3 The World Health Organization has also acknowledged regional patterns of disease burden, identifying that South-East Asia and the Western Pacific regions will have the greatest absolute number of NCD-related deaths over the next few years.4 In addition, Pacific Island countries are impacted by increasing rates of risk factors and comprise the top 10 countries in the world with the highest rates of overweight/obesity among adults.5 While NCDs and related risk factors are global issues affecting all populations, there are clear, disproportionate burdens experienced in LMICs.
Research examining factors underlying the global NCD burden has included exploration of the impacts of the early-life environment on later metabolic health.Reference Silveira, Portella, Goldani and Barbieri6,Reference Suzuki7 This paradigm, named the developmental origins of health and disease (DOHaD), asserts that adverse environmental exposures in the early-life stages, such as during infancy, pregnancy and even before conception, can influence later-life disease risk.Reference Hanson and Gluckman8 For example, a lack of balanced maternal nutrition during pregnancy, often resulting in low birth weight in offspring, has been associated with an increased risk of developing obesity and NCDs later in life, including type 2 diabetes and heart disease.Reference Baird, Jacob and Barker9,Reference Yajnik and Deshmukh10 There is also growing evidence for an intergenerational influence on NCD risk via the maternal or paternal lineageReference Yajnik and Deshmukh10,Reference Vickers11 thus perpetuating a cycle of disease across generations. Knowledge that has arisen out of DOHaD research has led to the development of interventions, such as health promotion strategies during pregnancy and school-based health literacy programmes, which target the early-life and adolescent life stages in order to promote healthier outcomes in the future.Reference Bay, Mora, Sloboda, Morton, Vickers and Gluckman12-Reference Thangaratinam, Rogozińska and Jolly15 Early-life nutrition and DOHaD-based research thus plays an important role in contributing to strategies that reduce risks associated with the development of NCDs later in life. However, to maximise effective dissemination of the knowledge gained, research must be sufficiently focused on populations with the greatest NCD burden in order to break the cycle and influence positive health outcomes.
Across all disciplines, there is an underrepresentation of research occurring in LMICs. One study retrospectively surveyed publications in five high impact health journals over 1 year, classifying articles into four regions: United Kingdom, United States of America, other Euro-American countries (including Europe, Canada, Australia and New Zealand) and the ‘rest of the world’.Reference Sumathipala, Siribaddana and Patel16 This study found that despite being comprised of 90% of the world’s population, the average research contribution from the ‘rest of the world’ category was only 6.5%.Reference Sumathipala, Siribaddana and Patel16 Research barriers identified included limited resources, lack of training and support, and difficulties getting accepted for publication.Reference Sumathipala, Siribaddana and Patel16 Despite these challenges, Patel and Sumathipala (2001, p. 406) recognised the urgent need for research ‘to reflect the diverse realities of health systems and cultural factors if research is to inform local health policy and practice’.Reference Patel and Sumathipala17
Given the potential of the DOHaD paradigm to promote early-life health to reduce risks related to NCD development, it is crucial that this research is inclusive of countries with high NCD burdens, such as LMICs. The present systematic review searches for published DOHaD research investigating associations between factors during pregnancy and at birth, such as nutrition and birth size, and later-life NCD incidence, risk factors and related mortality. The aim of this review is to identify where these DOHaD investigations take place and whether, given the burden of NCDs, this breadth of current research is appropriate and relevant.
Methods
This systematic review followed the Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) statement and used the participants, intervention/exposure, comparison, outcome, study design (PICOS) structure to identify eligible studies.Reference Liberati, Altman and Tetzlaff18,Reference Wieseler and McGauran19
Eligibility criteria
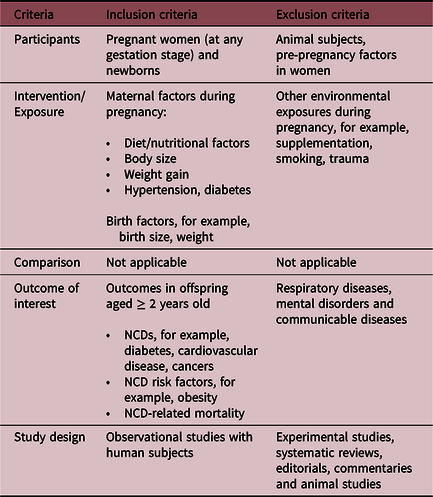
Observational studies that explored relationships between early-life factors, either during pregnancy and or at birth, with later NCD risk, incidence or related mortality, were sought for this review. Table 1 outlines the inclusion and exclusion criteria, including information on participants, exposure, outcome of interest and study design. Published journal articles from 1980 to 23 May 2018 (date of search) were eligible to be considered. Articles that were experiments, reviews, commentaries or based on animal subjects were excluded.
Table 1. Inclusion and exclusion criteria via PICOS for the selection of studies
Data sources and search strategy
The systematic search covered publications up until 23 May 2018 across three electronic databases: MEDLINE, Embase (both accessed via Ovid) and Scopus. Each search was comprised of three main groups of keywords: the early-life exposure, the later-life outcome and the stage of life. The early-life exposure keywords included DOHaD, developmental origins of health and disease, FOAD, fetal origins of health and disease, birth factor, early life, maternal diet and maternal nutrition. The later-life outcome keywords included noncommunicable disease, NCD, obesity, overweight, cardiovascular disease, CVD, diabetes, health outcome and later life. The stage of life keywords included offspring, neonate, infant, child, adolescent and adult. The Boolean operator ‘AND’ was used between each of the three groups, ‘OR’ within groups and ‘NOT’ to exclude common DOHaD animal models, such as rodents and sheep. Limits applied to each search ensured the inclusion of only journal articles written in the English language and published from 1980 onwards.
Study selection
Database results were exported to Endnote X8 reference management software, and both internal and external duplicates were removed. Titles and abstracts were independently screened based on the eligibility criteria by S.T, M.H.V and J.L.B. Any studies that could not have eligibility fully confirmed during this stage were held for full-text review. The remaining articles were independently assessed for full-text eligibility by S.T, J.L.B and M.H.V, reaching 85% agreement. All conflicts were discussed and a consensus was reached. No further information was requested from authors and articles were excluded if the full text was inaccessible.
Data extraction and risk of bias assessment
Data were extracted from each article regarding the study setting (variable of interest), early-life exposure, later-life outcome, age of participants and main study findings. Although a comprehensive search across databases was conducted, publication bias was a potential limitation, and thus, an effort was made to retrieve full texts from beyond the database, such as through university library networks. The quality of each study was assessed using the Newcastle–Ottawa star scale and adapted versions, which allowed the evaluation of cohort, case-control and cross-sectional studies.Reference Modesti, Reboldi and Cappuccio20,Reference Wells, Shea and O’Connell21 The assessment scale awards stars for factors under three main criteria: selection of study groups, comparability of groups and assessment of the outcomes.Reference Modesti, Reboldi and Cappuccio20,Reference Wells, Shea and O’Connell21 The maximum number of stars that could be achieved was eight or nine, depending on the study type.
Analysis
The countries where DOHaD investigations took place were the primary outcome of interest for this review. A total response method, commonly used in New Zealand ethnicity categorisation, was used to ensure that each different country identified within a particular study’s data set was given a single count.22 Although this meant that some studies were counted more than once if they were based on cross-country data sets, it allowed a representative overview of all the locations where DOHaD research occurred and ensured that no countries were missed. The total response method was also applied to explore age groups and country income classifications.
Results
Study selection
Fig. 1 outlines a flow diagram for the process of selecting studies. Based on the search criteria, a total of 6789 records were identified through the three databases. Internal and external duplicates (n = 3138) were removed via the Endnote software. Remaining records were screened for eligibility by title and abstract using the PICOS criteria outlined in Table 1, which resulted in the exclusion of 3498 records. Full-text articles were then assessed for the remaining records, with a final number of 136 studies included in this review (Supplementary Table S1).
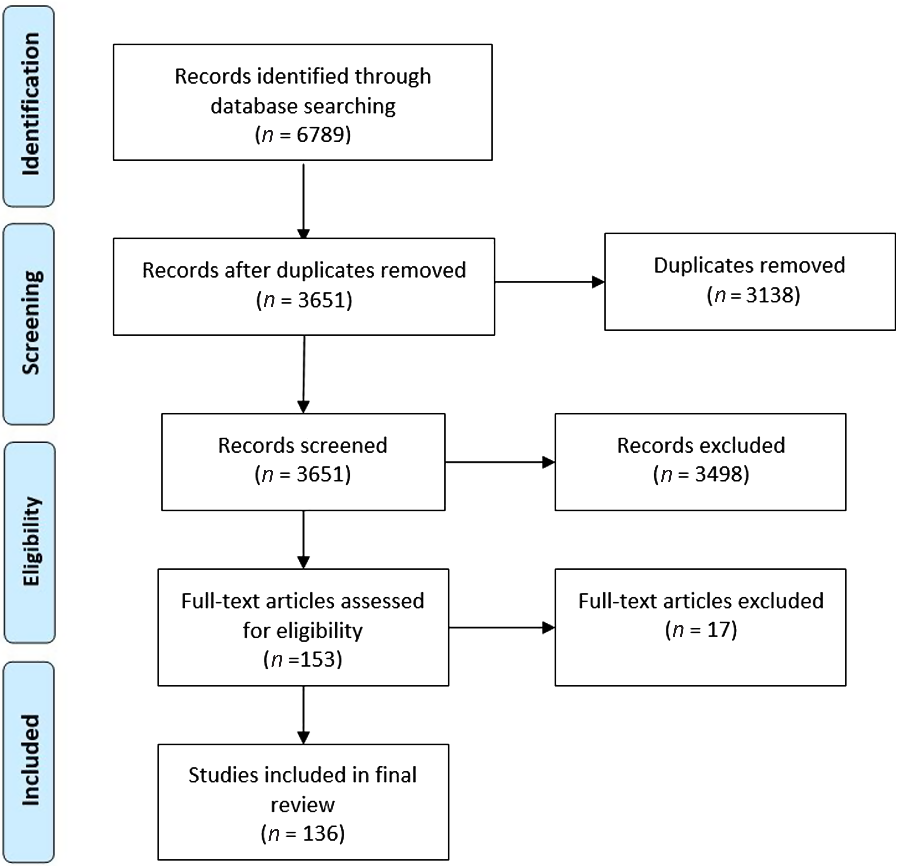
Fig. 1. PRISMA flow diagram for the selection of studies.
Study characteristics
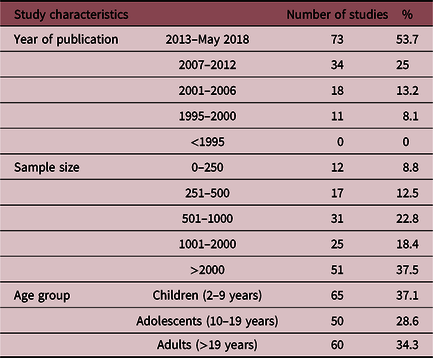
Table 2 outlines the main characteristics of the final 136 studies included in this review. It shows that DOHaD-related publications are steadily increasing over time, with the majority published in the last 5 years. Most studies in this review had sample sizes greater than 1000. The smallest study had a sample size of n = 31, while the biggest study included data from 2,133,504 people. To be eligible for this review, studies had to have explored NCD-related outcomes in participants at least 2 years of age. A total response method was used to categorise each study’s population into different age groups: children 2–9 years, adolescents 10–19 years and adults >19 years. Studies were allocated a single count for each group that included their study population’s age range. Table 2 shows that a higher proportion of DOHaD studies included data on children, followed by adults and then adolescents.
Table 2. Characteristics of the final studies included in the review
Location of DOHaD studies
This review found a total of 41 different countries across the final 136 articles, with a frequency of 157 countries studied. The highest frequency of DOHaD investigations occurred in the United Kingdom (n = 22), followed by China (n = 17), the United States (n = 16) and the Netherlands (n = 14). The 157 country frequencies were then categorised by region, as shown in Table 3. This review found that 49.7% of DOHaD investigations exploring relationships between the early-life environment and later-life NCDs were based on populations within Western Europe. And 15.9% included data from East Asia, 12.7% in North America, 8.3% in Latin America and the Caribbean, 5.1% in Australasia, 3.2% in South Asia, 1.9% in both the Middle East and the Africas, and 1.3% in Central Asia. Fig. 2 presents a map of this information, highlighting the regions with the most DOHaD research using darker green shades and regions with fewer investigations in lighter green shades. The countries in grey indicate countries where no DOHaD research was found.
Table 3. Distribution of countries and regions where DOHaD investigations have taken place
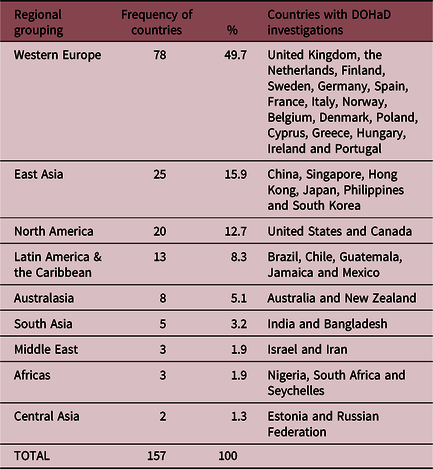
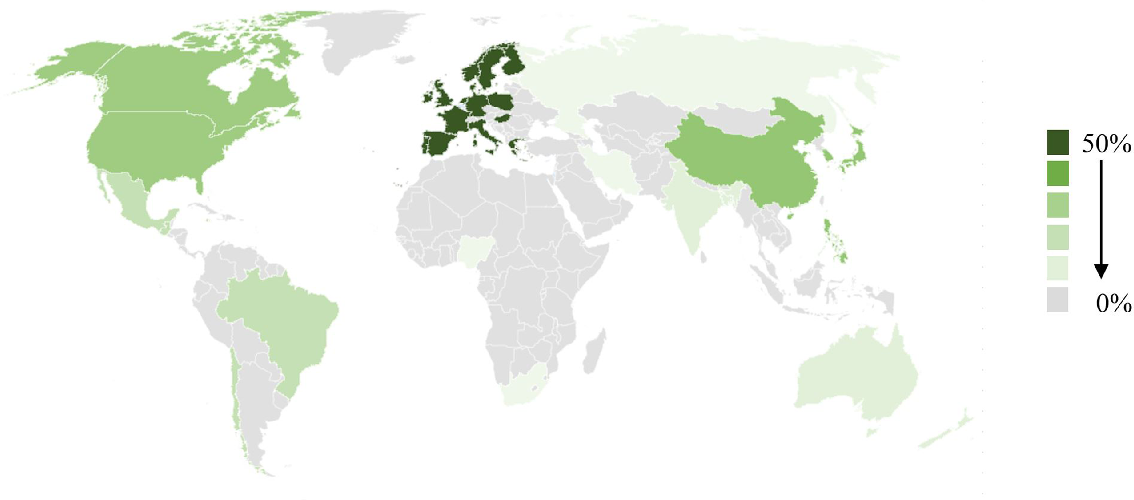
Fig. 2. Location of DOHaD studies by region.
Income classification of countries with DOHaD research
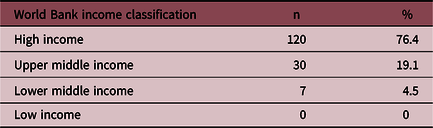
To identify the proportion of studies that included countries across each income bracket, the World Bank classifications based on gross national income (GNI) per capita were used.23 High-income economies were defined as having a GNI per capita of $12,376 or more, upper-middle-income economies were those between $3996 and $12,374, lower-middle-income between $1026 and $3995 and low-income economies as $1025 or less.23 Table 4 shows that out of the 157 frequencies of countries studied, 76.4% were high-income countries, 19.1% were upper-middle-income and 4.5% were lower-middle-income countries. This review found no DOHaD research, relating early-life factors during pregnancy and at birth to later NCD development, in low-income countries.
Table 4. Classification of countries by income
Discussion
This systematic review aimed to identify where DOHaD research was conducted and whether, given the burden of NCDs in LMICs, this breadth of current research was appropriate. The findings showed that the majority of DOHaD research has been based on populations within Western Europe. This contrasts with the regions experiencing the greatest burdens of NCDs, as identified previously, South-East Asia, Africa and the Western Pacific.4 This review found that only 19.1% of DOHaD research occurred across the East Asia and South Asia regions, 5.1% in Australasia and only 1.9% across Africa. Additionally, given that much of the NCD burden in the Western Pacific region occurs in Pacific Island countries, it is concerning that no DOHaD research has been conducted in these nations. This imbalance between the regions that produce the most research versus the regions with the greatest need has been previously identified in the literature.Reference Sumathipala, Siribaddana and Patel16,Reference Rahman and Fukui24-Reference Salager-Meyer26 A study by Rahman and Fukui explored a global profile of biomedical research and found that North America, Australia and Europe overwhelmingly had the highest number of publications per million population per year, with other regions falling far behind.Reference Rahman and Fukui24 Patel and Sumathipala corroborated this idea in their study, finding that only 6% of psychiatry literature was published from regions outside Euro-American countries.Reference Patel and Sumathipala17 This gap needs to be addressed as data should not be directly transferred from Western countries to inform on interventions in other nations without local data, as research needs to account for contextual factors, differences in population and availability of resources. DOHaD research must be prioritised in settings with high disease burdens if evidence is to inform effective interventions and policies.
Similar imbalances were found in this review regarding income level, with a high proportion of DOHaD research found in high-income countries (76.4%) and no studies based in low-income countries despite 80% of global NCD-related deaths occurring in LMICs.1 This disconnect has been identified across many disciplines, including a study on publications within general psychiatry journals.Reference Patel and Kim27 They found that from 2002 to 2004, only 3.7% of published psychiatry research originated from LMICs, and acceptance of submissions from these countries was significantly lower than high-income countries.Reference Patel and Kim27 Increased research in a setting creates a greater evidence base from which public health strategies, policies and improvements in clinical practice can result. The lack of DOHaD research in LMICs, as found in this study, may limit the development of local interventions and thus the potential to reduce the NCD burden. Guindon and colleagues explored the use of research-based evidence in clinical practice within LMIC health care providers.Reference Guindon, Lavis and Becerra-Posada28 They found that 84.6% of respondents were likely to change clinical practice if the research was performed in their own country, 66.4% if the research was performed somewhere in the region and only 55.8% if the research was performed in a high-income country.Reference Guindon, Lavis and Becerra-Posada28 These findings indicate that research conducted and published locally are more likely to influence changes in practice and interventions. There must be an increase in research in LMICs that considers contextual factors, to ensure the uptake and success of health interventions.
The DOHaD paradigm is centred on the influence of environmental exposures on later health; therefore, research must acknowledge the heterogeneity of environments. Upstream environmental drivers of place-based health inequities, such as historical factors and broader ecosystems, have been identified in the literature as ecological justice issues that need to be addressed.Reference Prescott and Logan29 This review identified that DOHaD research shows a clear preference to Western European settings, and thus, the potential for exploring heterogeneity of environmental contexts and upstream factors is limited. The lack of DOHaD research found in Pacific Island countries, for example, is concerning due to their unique environmental context and resulting health challenges. Past histories of colonisation and globalisation have influenced a rapid nutrition transition from traditional diets based on seafood and crops, to a predominance of imported, processed foods high in fat and sugar.Reference Gosling, Buckley, Matisoo-Smith and Merriman30,Reference Thow, Heywood, Schultz, Quested, Jan and Colagiuri31 Thus, the high proportion of research in Western European settings and lack of focus on LMICs found in this review demonstrates that current DOHaD research does not adequately address the breadth of environmental challenges faced across the globe. From a social justice standpoint, DOHaD research within LMIC settings must be prioritised as these populations contend with challenging environments influenced by broader upstream and historical factors.
There are many challenges to conducting and publishing important research from LMICs. While research from Western societies is often deemed worthy in its own right, some authors have discussed the tendencies of high-impact journals to only consider research from other countries if the findings indicate something unusual to that setting.Reference Patel and Sumathipala17 Difficulties can also arise with sample size issues and perceived rigour of data from non-Western countries.Reference Tu’akoi, Vickers and Tairea32 Many reviews of academic journals have found that papers from LMICs are less likely to be submitted, and, when they are, these papers are more likely to be rejected.Reference Patel and Sumathipala17,Reference Patel and Kim27 Such challenges need to be more widely recognised and addressed if there is to be increased DOHaD research in LMICs and regions with a high NCD burden. In order to encourage more DOHaD research and build capabilities within LMICs, there is great potential in bringing together collaborators from multiple LMIC settings. The Consortium of Health-Orientated Research in Transitioning Societies group is an existing example which brings together researchers and data from DOHaD cohort studies based in five LMICs: Brazil, Guatemala, India, the Philippines and South Africa.Reference Richter, Victora and Hallal33 This collaboration has enabled data to be pooled to enhance statistical power, further exploration into contextual factors common amongst LMIC environments, and has contributed to the development of DOHaD research within these settings.Reference Richter, Victora and Hallal33 Encouragement by institutions and funders to engage in similar international collaborations in other high needs areas, such as the Pacific, would be highly beneficial to develop research capacity, capabilities and, in the future, positive outcomes for these communities.
Academic journals have an obligation in ensuring research from LMICs is prioritised and promoted because, as Sumathipala, Siribaddana, and Patel (2004) outline, ‘their international success brings responsibilities to the global community they serve and profit from’.Reference Sumathipala, Siribaddana and Patel16,Reference Horton34 Considerations could be given to implementing systems that support this notion, such as fee waivers for open access and further developing and mentoring of authors from LMICs.Reference Beran, Byass and Gbakima35 Governments, funders and universities in high-income countries also have a key role in encouraging the development of collaborations with researchers and leaders in LMICs, in order to strengthen capabilities and ensure that solutions are locally led.Reference Beran, Byass and Gbakima35 In addition to promoting exposure of LMIC research in international journals, it also important to consider where this research could be published to have the greatest potential for community impact, for example, publishing locally in regional and national journals. This would also require institutions and universities to shift their preferences for researchers to publish within high-impact journals, to also considering where research might be best placed for relevancy and influencing practice. Improving research capacity in LMICs is crucial, not only for improving global health burdens and achieving publication equity, but also for advancing medical science.Reference Sumathipala, Siribaddana and Patel16
Strengths and limitations
While this review allowed exploration into global research gaps, a limitation was that this potentially masks research within countries that address high needs populations, for example, indigenous communities in high-income nations. Future research and reviews could explore this further and identify whether gaps exist in regard to the proportion of research conducted on vulnerable communities within countries. Another limitation of this review was the absence of supplementary search methods, such as backward citation searching. Previous systematic reviews have explored the usefulness of checking reference lists and found the evidence to be weak, identifying that in many cases it may not be the best use of time and resources.Reference Horsley, Dingwall and Sampson36,Reference Wright, Golder and Rodriguez-Lopez37 Although this means it is possible some eligible studies have been missed from this review, the large number of articles included in the final analysis likely provide a reasonable representation of the literature. The main strength of this study was the broad nature of the systematic search, and although preconceptional health and paternal influences were not included, the search still allowed a comprehensive overview of where DOHaD research occurs globally. This approach also enabled the inclusion of studies that may fit the DOHaD paradigm, but that do not explicitly identify with it.
Conclusion
The DOHaD paradigm identifies relationships between adverse early-life environmental influences and later-life NCD risk, emphasising the importance of a healthy start to life to optimise future health. However, it is not a ‘one size fits all’ and therefore it is crucial that LMICs and regions with high NCD burdens, such as South-East Asia, Africa and the Pacific, have local DOHaD research that can inform policy and practice. At present, the wealth of DOHaD research taking place does not correspond to where the NCD burden exists. Strengthening health research capacity in LMICs is critical for increasing local research, influencing evidence-based interventions and thus contributing to reducing the global burden of disease.
Supplementary material
To view supplementary material for this article, please visit https://doi.org/10.1017/S2040174420000276
Acknowledgements
We acknowledge the librarians from the Faculty of Medical and Health Sciences at the University of Auckland for their assistance with the systematic search.
Financial Support
S.T. was supported by a PhD scholarship from the Health Research Council of New Zealand reference #17/479.
Conflicts of Interest
None.
Ethical Standards
No ethical approvals required.








