Introduction
In 2015, the number of migrants was the highest ever in Sweden, when nearly 163,000 individuals sought asylum (SCB Statistics Sweden, 2016). The newcomers mainly originated from Afghanistan, North Africa, and Syria. This was added to the migrant population already living in Sweden, who were labor migrants that mainly immigrated during the postwar era and the 1970s, from Finland and ex-Yugoslavia. From mid-1985, the pattern of immigration changed to mainly include refugees, with a first wave from Latin America, Asia, and Africa and another peak during the 1990s from the war in ex-Yugoslavia and the Middle East. Thus, the migrant population is a mix of nationalities (>140), and the number of foreign-born is about 20% of the population (10 million; Statistics Sweden, 2019).
Much of what is known about the current content and the quality of palliative care in Sweden is based on data from the Swedish Register of Palliative Care (SRPC) (Lundström et al., Reference Lundström, Axelsson and Hedman2012). This registry contains individualized data concerning patient problems, medical interventions, and outcomes after treatment within all health care. During 2017 and 2018, 58,243 respective 55,855 deaths were reported to the SRPC, representing just over 60% of all deaths in that specific year in Sweden (The Swedish Register of Palliative Care, 2018). Studies on that data have showed that access to high-quality palliative care for people suffering from life-threatening and incurable diseases is unequal and differs in an unfair way depending on diagnosis (Brännström et al., Reference Brännström, Hägglund and Fürst2011; Ahmadi et al., Reference Ahmadi, Wysham and Lundström2016; Eriksson et al., Reference Eriksson, Milberg and Hjelm2016), place of care (Henoch et al., Reference Henoch, Strang and Löfdahl2019), and age (Lindskog et al., Reference Lindskog, Tavelin and Lundström2015). Palliative care, as delivered today, can also be unfair since it is not always based on individual needs. Moreover, people with migrant backgrounds risk not receiving the same quality and quantity of care as native Swedes, depending on different social and economic status, lack of knowledge regarding alternatives of end-of-life care, and communication difficulties. To the best of our knowledge, there are no previously published studies focusing on a variety of quality of care indicators in end-of-life care involving people with migrant backgrounds.
Studies from other countries, especially from UK and US, have investigated if ethnic status constitutes a risk for disparities in palliative care (Elkan et al., Reference Elkan, Avis and Cox2007; Cohen, Reference Cohen2008; Coupland et al., Reference Coupland, Madden and Jack2011; Evans et al., Reference Evans, Menacha and Andrew2011; Johnson, Reference Johnson2013; Garrido et al., Reference Garrido, Harrington and Prigerson2014; Worster et al., Reference Worster, Kennedy Bel and Roy2018). A register-based study on differences regarding place of death between ethnic groups showed significant differences between various ethnic groups and white patients (Coupland et al., Reference Coupland, Madden and Jack2011). However, these results are not completely applicable and valid for Swedish conditions with our specific migration patterns and the heterogeneous migrant population. A recent study from Germany, with a more comparable immigration pattern as the Swedish, showed an unequal utilization of specialized palliative care by immigrants, especially those originating from Turkey (Henke et al., Reference Henke, Thuss-Patience and Behzadi2017). Still, what is unknown is if migrants, in need of palliative care, are more often cared for in their home with support from home care delivered by the primary health care and/or the municipality than in an institution, and if the care differs in other quality indicators compared with native Swedes. Using data from the national SRPC (Lundström et al., Reference Lundström, Axelsson and Hedman2012) gives a unique opportunity to study whether care delivered was given on equal terms, and what kind of support has been given to individuals with migrant backgrounds compared with native Swedes.
The aim of this study is to use data from a national register to investigate if there are differences relating to migrant background when it comes to the quality of end-of-life care for patients dying in Sweden.
Method
Design
A retrospective, comparative study using data from the national quality register, the SRPC.
Sample
An extract of register data for all expected deaths (and do not know/missing, cases), for those over 18 years age, registered in the SRPC during 2017–2018, constitutes the study sample. A comparison of SRPC data with information from the Swedish Cause of Death Register allowed for separation according to country of birth.
Data collection and variables
Data were collected through an online end-of-life questionnaire (EOQ; Lundström et al., Reference Lundström, Axelsson and Hedman2012), with items based on different essential aspects of end-of-life care in the last week of life. The questions, which are mandatory and have to be answered before submission, are answered by the responsible registered nurse and/or physician as soon as possible following the patient's death. Data for patients reported as cases of unexpected death were excluded in this study because they lack complete data as opposed to data on patients with expected deaths. From the EOQ, data on age, gender, place of death, and 16 questions with different quality of care process indicators were retrieved. For the most part, those questions could be answered with yes, no, and do not know. Data on country of birth and medical condition were obtained from the Swedish Cause of Death Register held by the Swedish National Board of Health and Welfare.
Data processing and statistical analysis
Descriptive statistics were calculated for the individual variables with means and SD for continuous variables, and frequencies and percentages for categorical data. Comparisons were made by conducting tests of statistical significance by chi-squared test or Fisher's exact test for categorical variables, and Students t-test or Mann–Whitney U-test when appropriate for continuous variables. The two items from the Swedish Cause of Death Register were processed in nine pre-defined categories for country of birth (see Supplementary Appendix 1), and the International Classification of Diseases codes (ICD-codes) were grouped into nine categories (see Table 1).
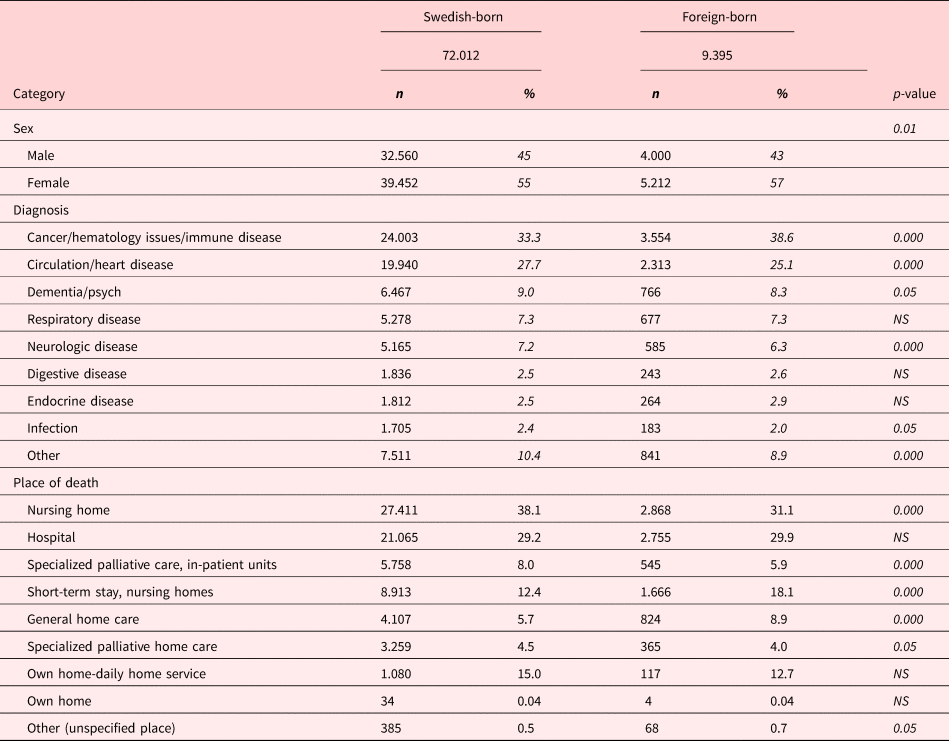
Table 1. Background data of the patients reported to the SRPC during 2017–2018
For each quality indicator, we tested whether or not its implementation in the end-of-life care could be predicted by the patient's country of birth (independent variable) using pre-defined categories. All data were dichotomized, and binary logistic regression analyses were used to calculate odds ratios (ORs) with 95% confidence intervals (CIs). The binary logistic regression analyses were theory-driven. In the first step, we entered country of birth into the model; next, we entered age and gender, followed by diagnosis. The last step in the regression analysis was to add the type of end-of-life care unit to the model. The Swedish-born patients were used as a reference group. A p-value of less than 0.05 was considered significant. Calculations were performed in SPSS version 25 (SPSS, Inc., Chicago, IL).
Ethics
The study was approved by the National Ethics Authority (EPN D-number 2019–02971). All collected data were anonymized and coded so that no specific individual might be identified. All patients were deceased, and it was not possible to obtain informed consent from the patients; however, as this was a quality register study, all patients had been informed in advance about the national quality registers, as well as about voluntary participation and confidentiality, as part of the health care routines. The SRPC management group approved the study.
Results
In total, 81,418 deceased patients, over 18 years of age, registered in the SRPC during 2017 and 2018 of expected death (or do not know/missing), were included in the study. The mean age in the study population was 82 (r 19–110) years, and it was significantly higher in Swedish-born patients compared with foreign-born, 82.5 versus 79 (p = <0.001).
Background data are described in Tables 1 and 2. Depending on place of death (Table 1), the Swedish-born group had been cared for in a nursing home (38.1% vs. 31.1%, p = <0.001), specialized in-patient palliative care (8.0% vs. 5.9%, p = <0.001), or in specialized palliative home care (4.5% vs. 4%, p = <0.05), to a higher extent than foreign-born patients. The foreign-born patient group was overrepresented in end-of-care units with short-term stay in nursing homes (18.1% vs. 12.4%, p = <0.001) and general home care (8.9% vs. 5.7%, p = <0.001), and in unspecified care, that is, a blended group, mostly consisting of intensive care units (p = <0.05).
Table 2. Areas of country of birth
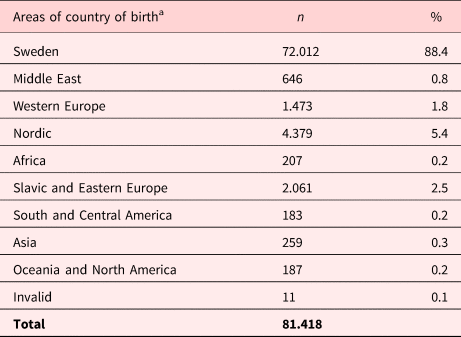
a Areas of country of birth, see Supplementary Appendix 1 for the complete list of countries included in the study.
When considering the five main groups of diagnoses, significant differences were found between Swedish- and foreign-born patients. Having a cancer diagnosis was more common in foreign-born than Swedish-born patients (38.6% vs. 33.3%, p = <0.001), while heart/circulation diseases (27.7% vs. 25.1%, p = <0.001), neurological diseases (7.2% vs. 6.3%, p = <0.001), and dementia/psychiatric diseases (9% vs. 8.3%, p = <0.05) were more prevalent in Swedish-born than foreign-born patients. No difference was found for respiratory diseases. The biggest migrant groups originated from Nordic countries as well as Slavic or Eastern European countries (Table 2).
Table 3 shows descriptive data on quality indicators. The quality indicator that reached the highest levels in both Swedish- and foreign-born patients was the prescription of rescue medicines (84.2–94.1% vs. 83.9–94.0%). Likewise, the likelihood that the patients had received some kind of consultation services was lowest among the quality indicators, in both the Swedish- and foreign-born patients (0.8–7.8% respective 0.9–7.5%).
Table 3. Description of data about quality indicators during the last week of life divided into Swedish-born and foreign-born patients
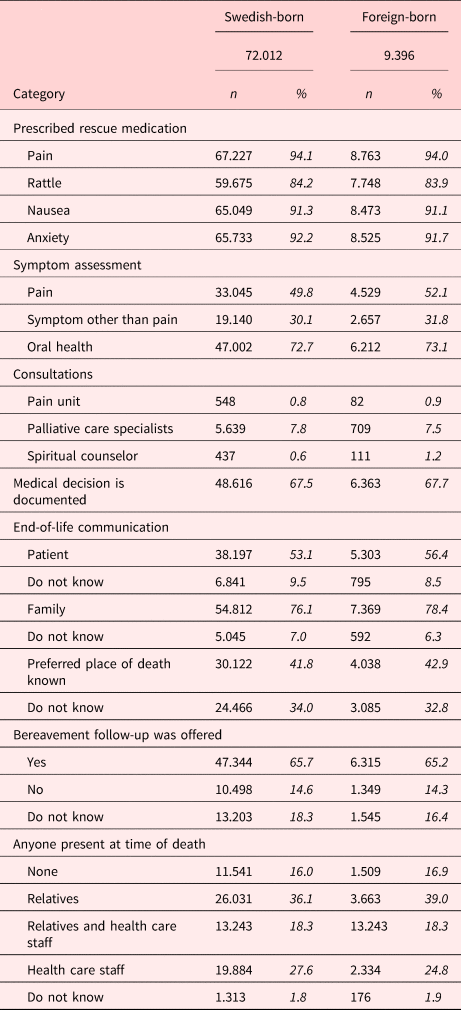
Prescribed rescue medicines and systematic assessment of end-of life symptoms
The pattern for end-of-life prescriptions of rescue medicines was inconsistent; for some indicators, the care was an advantage for the Swedish-born patients compared with the subgroups of the foreign-born patients, and for other indicators, the Swedish-born patients were disadvantaged (Tables 3 and 4). Patients born in Oceania and North America were prescribed injectable drugs for pain relief in end-of-life care significantly more often than others. Patients born in Nordic countries were prescribed anxiolytic drugs less often. They were also prescribed anticholinergic drugs to a lesser extent, similar to those from Slavic and Eastern European countries.
Table 4. End-of-life prescriptions of injectable drugs for symptom relief
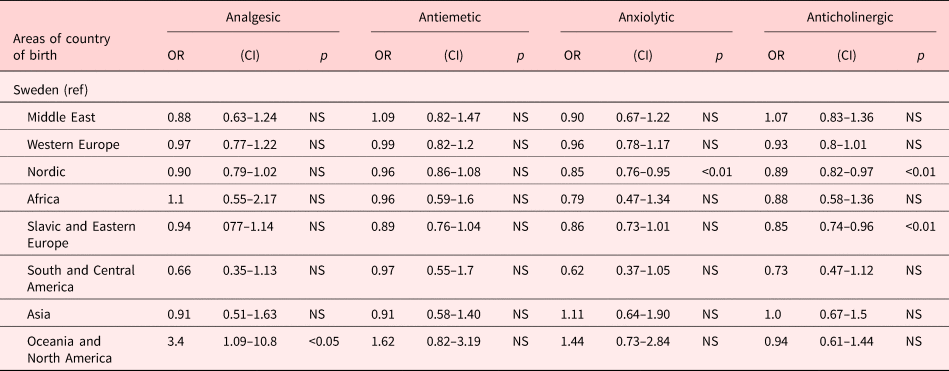
Expressed in odds ratio with 95% Cls. Presentation of model 4.
Odds ratio adjusted for age, gender, diagnosis, and the type of the end-of-life care unit.
Systematic assessment for the presence of pain by Numerical Rating Scale (NRS), Visual Analogue Scale (VAS), or other validated instrument) was performed more often in patients of Slavic and Eastern European origin and less often for patients born in Nordic countries. Moreover, systematic assessment for other symptoms than pain (by NRS, VAS, or other validated instrument) was performed significantly more often in foreign-born persons from South and Central America. Regarding assessment of oral health was done in lesser degree in patients born in Nordic and Slavic and Eastern European countries (Table 5).
Table 5. Systematic assessment of symptoms
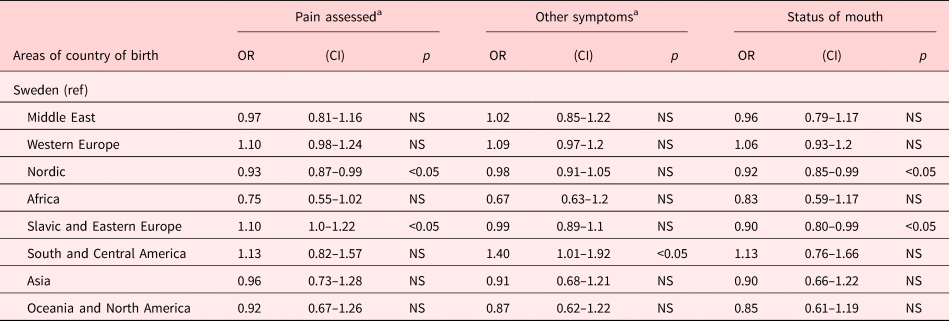
.
Odds ratio adjusted for age, gender, diagnosis, and the type of the end-of-life care unit.
a Assessed systematic by validated instruments.
Use of palliative consultation services in end-of-life care
The differences in the use of palliative consultation services in the last week of life are shown in Table 6. Consultation with a spiritual counselor took place significantly less often in Swedish-born patients compared with foreign-born groups, except a higher consultation degree than patients born in the Nordic countries. On the other hand, there was a higher degree of consultations with palliative care teams for Swedish-born patients than patients born in Africa and Asia.
Table 6. Use of palliative consultation services in end-of-life care
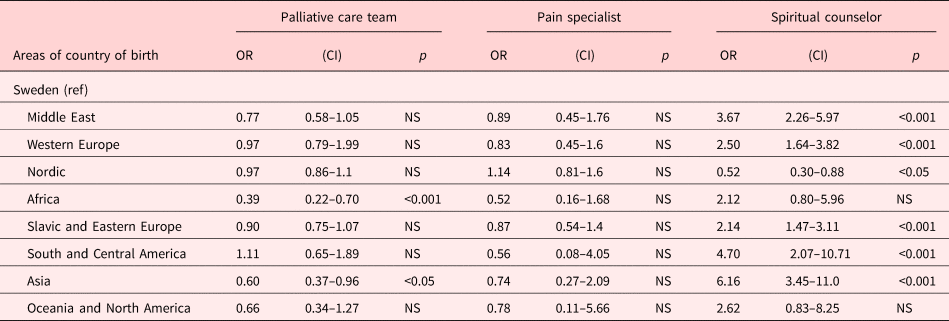
Expressed in odds ratio with 95% CIs. Presentation of model 4.
Odds ratio adjusted for age, gender, diagnosis, and the type of the end-of-life care unit.
End-of life communication, medical decision-making, bereavement support, presence at time of death, and knowledge of patients’ preferred place of death
Dialogue and end-of life discussions with the family were more often held by relatives of patients born in the Middle East. No difference was found relating to dialogue and end-of life discussions with the patients as well as the presence of a medical decision about end-of-life care in patients’ records (Table 7).
Table 7. End-of life communication and the medical decision to focus on end-of-life care are documented in patient record
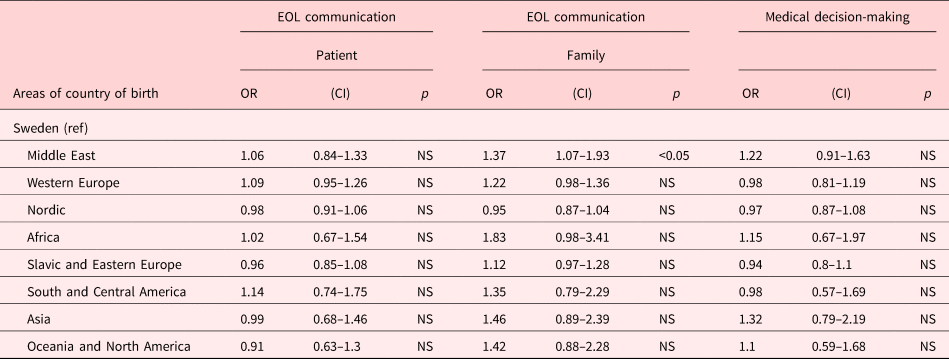
Expressed in odds ratio with 95% CIs. Presentation of model 4.
Odds ratio adjusted for age, gender, diagnosis and the type of the end-of-life care unit.
The quality indicator, presence of someone at time of death, is presented in two different panels (Table 8). The first panel shows dying in the presence of someone (either family member/health care staff or both), and the second panel shows dying in the presence of a family member (family and family member and health care staff). The likelihood of dying in the presence of family members was more frequently occurring in care of patients born in the Middle East and less often for patients born in Nordic and Slavic and Eastern European countries. Dying in the presence of someone was more likely for patients born in Middle east and less often for patients born in nordic countries. Relatives of patients born in Nordic countries were offered bereavement support in a lesser degree.
Table 8. The patients’ preferred place of death is known, someone present at time of death and bereavement support
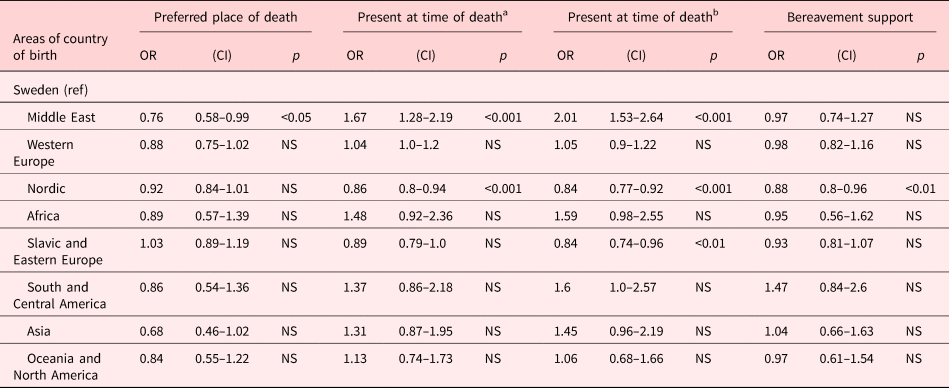
Expressed in odds ratio with 95% CIs. Presentation of model 4.
Odds ratio adjusted for age, gender, diagnosis, and the type of the end-of-life care unit.
a Either family member/health care staff or both.
b Only relatives or relatives and health care staff.
Discussion
The main result of this study was that there are no general patterns in differences in the quality of end-of-life care between Swedish-born and foreign-born patients. However, there were several significant differences in various quality indicators but not in a specific direction. Sometimes, quality indicators were an advantage for Swedish-born patients but just as often, they were favorable for foreign-born patients as well.
The results showed that foreign-born patients were less likely to be cared for in specialized palliative care units than Swedish-born patients. These results are in agreement with other studies that compare the utilization of specialized palliative care services between immigrants and native-born persons (Koffman et al., Reference Koffman, Ho and Davies2014; Henke et al., Reference Henke, Thuss-Patience and Behzadi2017) or between different ethnic groups (Cohen, Reference Cohen2008; Coupland et al., Reference Coupland, Madden and Jack2011). Access to specialized palliative care is often taken as a proxy for the quality of end-of-life care (Coupland et al., Reference Coupland, Madden and Jack2011). These assumptions are supported by the results from the Swedish Registry of Palliative Care (2018), which showed that specialized palliative care units do better in all, but one (pressure ulcers) quality indicator. The result also showed a little over representation of cancer diagnosis in foreign-born patients. Register studies from the SRPC have shown that patients with cancer receive better quality of end-of-life care in several end-of-life care areas when compared with patients dying with dementia (Martinsson et al., Reference Martinsson, Lundström and Sundelöf2017), respiratory disease (Ahmadi et al., Reference Ahmadi, Lundström and Janson2015, Reference Ahmadi, Wysham and Lundström2016), and heart disease (Brännström et al., Reference Brännström, Hägglund and Fürst2011). However, the statistics, in the present study, are adjusted for the type of end-of-life care unit and diagnosis.
The most unexpected result was that Nordic-born patients scored lower on almost all quality indicators compared with Swedish-born patients, despite them coming from countries with a low cultural distance [dissimilarities in language, social structure (e.g., family), religion, standard of living, and cultural values (Triandis, Reference Triandis2000)]. There might be great linguistic differences, especially between Finish and Swedish people. Finnish-born migrants dominated in the Nordic group (n = 2,941/4,379, 67%), as in the Swedish migrant population (Statistics Sweden, 2019). Finns immigrated to Sweden during the 1970s as labor migrants and most were Finnish-speaking. Previous longitudinal epidemiologic studies (Albin et al., Reference Albin, Hjelm and Ekberg2005, Reference Albin, Hjelm and Ekberg2006) have shown higher mortality and morbidity in foreign-born compared with Swedish-born persons, particularly among migrants from Finland. A larger number of deaths in the ICD code group “Symptoms, signs and ill-defined conditions” could especially be explained by language problems, but they might also be related to cultural factors affecting communication. Thus, migrants might express health, illness, and pain differently from native Swedes. However, there is no clear explanation for these differences, which is why further studies are needed.
The difference in offering consultations with spiritual counselor, being of a lesser extent for Swedish-born persons, is striking and may be due to the fact that Swedes are the most secularized people in the world (World Values Survey, 2014). Another explanation could be found in the study by Strang et al. (Reference Strang, Strang and Ternestedt2001), which shows that many nurses in their study thought that Swedish patients, compared with foreign-born patients, did not have specific spiritual needs. However, it was a very low proportion in all groups. The lower frequency of involvement by palliative care teams in caring especially for African and Asian born patients is hard to explain, These results indicate that foreign-born patients are disadvantaged, in terms of having poorer access to palliative care expertise. Immigrant patients might be less familiar with palliative care and lack of knowledge about the healthcare system in the new country might be obstacles in requesting and placing a demand on specialized care. Another explanation might be that many migrants with severe conditions and in palliative stage are cared for in their homes with the help of their relatives, as demonstrated in previous studies of Turkish and Moroccan immigrants (de Graaff et al., Reference de Graaff, Francke and van den Muijsenbergh2010, Reference de Graaff, Mistiaen and Lim Devillé2012).
End-of-life communication with patients and/or relatives, when informing about imminent death and making advance care planning for the remaining time in life, is considered as a cornerstone in palliative care. Moreover, the National Board of Health and Welfare (Socialstyrelsen. Nationella riktlinjer-utvärdering, 2016) in Sweden has listed end-of-life communication as one of six quality indicators of palliative care. We found no significant difference in end-of-life communication with the patients, and the only significant difference was that the families of patients born in Middle East, were more likely to have had an end-of-life communication. Their family members were in a higher degree present at time of death. Family involvement in end-of-life care might be seen as a shared responsibility in the society and a duty in many foreign cultures (de Graaff et al., Reference de Graaff, Francke and van den Muijsenbergh2010, Reference de Graaff, Mistiaen and Lim Devillé2012; Hiruy and Mwari, Reference Hiruy and Mwari2014; Javdan and Cassileth, Reference Javdan, Cassileth and Silbermann2016).
The presence of someone at the time of death, that is, the patient does not die alone has a high value in all cultures. In Sweden, it is not unusual that if the patient does nothas any relative that could be present, a total stranger (extra staff) could be called in to sit by the deathbed. A recent study from Sweden (Strang et al., Reference Strang, Bergström and Martinsson2020) about COVID-19 deaths, with data from the SRPC, has an extensive discussion about this topic as many patients are dying due to COVID-19 or died alone due to restrictions on visits.
Strengths and limitations
The main strength of this study is that the SRPC is a national register that covers a majority of deaths from all parts of Sweden and care facilities and registers several indicators for the quality of end-of-life care. Further, SRPC became a quality register in 2006 and has since been continuously evaluated, revised, and validated (Martinsson et al., Reference Martinsson, Heedman and Lundström2011; Lundström et al., Reference Lundström, Axelsson and Hedman2012); also, it has a coverage of approximately 60% of all deaths in Sweden. Another strength is the Swedish personal identification number, which allows for registers to be coordinated. In this study, the SRPC and the Swedish Cause of Death Register make it possible to identify country of birth.
The limitation of the present study is that all data were, retrospectively, reported by staff and based on documentation in the medical record; no patient-reported data were present. Furthermore, it was challenging to know how to group countries together, especially countries from the former Eastern Bloc of Europe; perhaps, the grouping could have been done differently. However, what was finally chosen was based on the fact that most of the deceased persons in the present study were old and had migrated to Sweden during a long and turbulent time when countries and borders in Europe underwent several changes.
Conclusion
Foreign-born patients were less likely to be cared for in specialized palliative care units than Swedish-born patients, despite a higher proportion of those with cancer diagnosis. However, no general patterns were found indicating that foreign-born patients were disadvantaged using the quality indicators measured in the present study. Perhaps, this is an indication that palliative care in Sweden is individualized; nonetheless, the quality of end-of-life care would be higher if dying patients, regardless of country of birth, have better access to specialized palliative care.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S1478951521000110.
Acknowledgments
We thank the SRPC and the Swedish National Board of Health and Welfare via the Swedish Cause of Death Register for generously providing us with data for the study. We also thank Ronnie Pingel, Associate Professor, for help with the statistics. We would also like to thank the National Board of Health and Welfare for financial support.
Conflict of interest
The authors declare that there is no conflict of interest.













