After experiencing an event in which one's life is in imminent danger and one feels completely helpless, the conditional risk for developing post-traumatic stress disorder (PTSD) is 9–14%. Reference Breslau, Kessler, Chilcoat, Schultz, Davis and Andreski1–Reference De Vries and Olff3 Two trauma-focused psychotherapy methods, trauma-focused cognitive–behavioural therapy (CBT) and eye movement desensitisation and reprocessing therapy (EMDR), are the most efficacious psychological treatments for PTSD currently available. Their effect sizes have proven to be equally large, 4–Reference Seidler and Wagner6 and there are some indications that EMDR leads to faster recovery. Reference Ironson, Freund, Strauss and Williams7 However, no studies have compared these treatments directly in sufficiently powered designs, and few studies have investigated the response pattern. The PTSD guideline of the National Institute for Health and Clinical Excellence (NICE) 4 has also emphasised that adequately powered randomised trials should be conducted to compare these treatments, and to provide information about their value in clinical practice. Therefore, our aim was to conduct a well-powered randomised trial comparing the efficacy of, and response patterns to, treatment with EMDR and brief eclectic psychotherapy for patients with PTSD resulting from various types of psychological trauma. Brief eclectic psychotherapy was originally developed in The Netherlands and classified as a trauma-focused CBT in accordance with the NICE guideline. 4 Although it includes some elements of other therapeutic schools, its main treatment components overlap with those of other trauma-focused CBT interventions. Some elements of ‘practical trials’ (trials that include elements of effectiveness designs) were included in the current trial to increase the extent to which results can be generalised to routine clinical practice and inform healthcare decisions. Reference Schnurr8 In line with a previous pilot study, Reference Ironson, Freund, Strauss and Williams7 we hypothesised that EMDR would lead to faster improvements in PTSD symptomatology than brief eclectic psychotherapy and that the improvements at the end would be equal. Trial registration: Dutch Trial Register, number NTR46 and ISRCTN64872147.
Method
Participants were recruited from the Centre for Psychological Trauma of the Academic Medical Centre in Amsterdam, The Netherlands, between December 2003 and January 2009 following ethics committee approval. Participants were civilian trauma survivors, who were referred to our centre by general practitioners, victim support workers, occupational physicians and other Academic Medical Centre departments. If a PTSD diagnosis was presumed at intake, individuals were approached for the study. After potential participants received a complete description of the study, written informed consent was obtained.
Study entry criteria
Study entry criteria were: a PTSD diagnosis according to DSM-IV; 9 a single traumatic event (which had stopped at the time of inclusion) that led to the development of PTSD; age between 18 and 65 years; and mastery of the Dutch language. Exclusion criteria were: acute suicidality; current severe major depressive disorder or current severe alcohol or substance dependence according to DSM-IV (patients were allowed to enter after initial treatment of these disorders); lifetime psychotic disorder according to DSM-IV; and severe personality disorder according to the Structured Clinical Interview for DSM-IV Axis II Disorders (SCID-II) Reference First, Gibbon, Spitzer, Williams and Benjamin10 and DSM-IV. Patients with a history of earlier traumatic events were allowed to participate in the trial. Prior to entering the trial, patients who were on parallel pharmacological treatment were required to be on a stable medication dose for at least 4 weeks, and patients with prior alcohol or substance dependence were required to be abstinent for at least 3 months. During treatment, medication dosage was maintained as much as possible, but in agreement with clinical guidelines patients were allowed to stop anxiolytic medication to better engage in trauma processing. Participants were not allowed to attend any other trauma-focused intervention during their treatment in the trial.
Design
The study was a randomised controlled trial in which brief eclectic psychotherapy was compared with EMDR. The choice of brief eclectic psychotherapy, instead of another trauma-focused CBT intervention, was made because it explicitly combines the most effective ingredients of trauma-focused CBT such as psychoeducation, imaginal exposure, cognitive restructuring and writing assignments. Its effect sizes in previous studies with similar populations Reference Lindauer, Gersons, Van Meijel, Blom, Carlier and Vrijlandt11,Reference Olff, De Vries, Güzelcan, Assies and Gersons12 are equal to those of other trauma-focused cognitive–behavioural interventions. Reference Bradley, Greene, Russ, Dutra and Westen13
Participants were randomised to brief eclectic psychotherapy or EMDR in a parallel design. Random assignment was done on a 1:1 basis by a computer program, with a weighted maximum of subscribing four times the same treatment in a row. To ensure masking of assessors, one psychologist who had no other engagement in the study, had access to the computer program, kept a log file of all random assignments and assigned the patients to the therapists.
Both EMDR and brief eclectic psychotherapy were carried out according to treatment manuals and administered as in clinical practice, allowing for the number of sessions to vary depending on recovery. Leading trainers and supervisors in brief eclectic psychotherapy (B.P.R.G.) and EMDR (A.d.J.) were included in the study to control for an investigator allegiance effect. The primary outcome measure for self-reported PTSD symptoms was the Impact of Event Scale – Revised (IES-R), Reference Weiss, Marmar, Wilson and Keane14 which was administered at baseline and at every weekly treatment session, as well as during a final assessment at week 17 when treatments had finished. Secondary outcomes were clinician-rated PTSD, depressive and general anxiety symptoms, which were also assessed at baseline and at week 17 (i.e. second post-assessment). Brief eclectic psychotherapy differs from EMDR in treatment duration and consists of two phases. Therefore, at mid-term an additional assessment was scheduled (first post-assessment) that was conducted after the EMDR treatment (mean 6.5 sessions) and after the first phase of brief eclectic psychotherapy (6 sessions; Fig. 1).
Interventions
The therapists were psychiatry residents or master's level clinical psychologists, who received a 3-day level-I training for EMDR and for brief eclectic psychotherapy. Prior experience with PTSD treatment was not required. A total of 38 therapists delivered the treatments; of these 7 delivered both. They received biweekly group supervision. All sessions were audiotaped. Treatment adherence protocols were developed to rate six brief eclectic psychotherapy sessions (session 1, 2, 4, 11, 13 and 15) and three EMDR sessions (first, second and second to last). Treatment adherence coding systems were based on a previous brief eclectic psychotherapy study Reference Lindauer, Gersons, Van Meijel, Blom, Carlier and Vrijlandt11 and an EMDR Fidelity Scale Reference Korn, Zangwill, Lipke and Smyth15 adapted for use with the Dutch EMDR protocol.
Eye movement desensitisation and reprocessing
The weekly EMDR sessions lasted 90 min and were applied according to the Dutch treatment manual. Reference De Jongh and Ten Broeke16 During EMDR therapy, the most distressing images of the traumatic event are identified and processed consecutively. After the patient has focused on an image with the corresponding negative cognition, the most distressing emotion and the bodily location of the emotion, the patient is continuously asked to follow the therapist's finger making saccadic movements in alternation with the patient's own associations. Current distress is rated every 5–10 min, until the distress level is 0 or 1, after which a more positive cognition is introduced in relation to the target image. This procedure is repeated for the other distressing images and treatment sessions are terminated when the trauma memory feels neutral. Auditory bilateral stimulation was used if problems with eye movements were encountered (such as if they induced headaches).
Brief eclectic psychotherapy
Brief eclectic psychotherapy was applied according to a detailed manual Reference Gersons, Carlier and Olff17 and consisted of weekly sessions of 45–60 min as administered in previous studies. Reference Lindauer, Gersons, Van Meijel, Blom, Carlier and Vrijlandt11,Reference Olff, De Vries, Güzelcan, Assies and Gersons12,Reference Gersons, Carlier, Lamberts and van der Kolk18 The treatment was initially developed and applied in The Netherlands and 400 therapists have been trained in this country in the last decade. Its main treatment components are also used in other trauma-focused CBT, such as psychoeducation, imaginal exposure, writing assignments and cognitive restructuring. Two main phases can be clearly distinguished; from session 2 to 6 imaginal exposure takes place, whereas sessions 7–15 are dedicated to cognitive restructuring. Session 1 consists of psychoeducation and session 16 of a farewell ritual. Some of the elements in the second phase can also be understood from other therapeutic perspectives, including grief therapy, directive therapy and a psychodynamic approach. These elements include taking mementos to the treatment session (objects that are linked to the traumatic event, such as the clothes that the person was wearing at that time, to stimulate the imaginal exposure), performing a farewell ritual that is intended to symbolically leave the trauma behind, and giving meaning to the traumatic event. The exposure in brief eclectic psychotherapy is very detailed, using sensory memories to stimulate reliving and focusing on experiencing grief. The aim is to relive the whole traumatic event in detail – in parts, over several sessions.
Measures
Assessments were conducted by trained, independent, masked assessors who were master's level clinical psychologists or master's level psychology students supervised by an experienced clinical psychologist. To ensure comparability among assessors, biweekly supervision took place. Before all post-assessments, patients were instructed to avoid mentioning details about the content or length of their treatment to ensure masking.
The primary outcome measure for PTSD symptom severity was the IES-R. Reference Weiss, Marmar, Wilson and Keane14 Unlike the original revised version in which categories from zero to four are used, the Dutch IES-R rates the frequency of each item in the preceding week as zero (not at all), one (rarely), three (sometimes) and five (often). Clinical PTSD diagnoses were established by means of the Structured Interview for PTSD (SI-PTSD), Reference Davidson, Malik and Travers19 which operationalises the DSM-IV criteria for PTSD. To assess comorbid psychiatric diagnoses, the Dutch version of the Structured Clinical Interview for DSM-IV Axis I Disorders (SCID-I) was administered. Reference Spitzer, Gibbon, Janet and Janet20,Reference Van Groenestein, Akkerhuis, Kupka, Schneider and Nolen21 The Hospital Anxiety and Depression Scale (HADS) Reference Zigmond and Snaith22 was used to measure the severity of the general anxiety and depressive symptoms by self-report. All these measures have been widely used in trauma research and have been shown to have strong psychometric properties. Reference Creamer, Bell and Failla23–Reference Spinhoven, Ormel, Sloekers, Kempen, Speckens and Van Hemert26

Fig. 1 Study design and patients’ flow throughout trial.
PTSD, post-traumatic stress disorder. a. Number of sessions refers to the sessions completed by the participants. b. Patients who prematurely dropped out of treatment (n= 32) were contacted and the following reasons for drop-out were given: patient did not notice any improvement (n = 8), patient felt no further need to continue therapy (n = 3), patient experienced a new trauma or recurring threat (n = 3), patient wanted a different focus in treatment (n = 2), unknown because patient could not be located (n = 16). c. Patients who did not receive any treatment (n = 13) had health problems (n = 3) or withdrew from treatment before the first session (n = 10).
Data analysis
Power calculations were based on post-treatment means and standard deviations of a previous study, Reference Olff, De Vries, Güzelcan, Assies and Gersons12 which found a mean IES-R score of 49.5 (s.d. = 14.1) after brief eclectic psychotherapy for PTSD. Based on this previous study, we considered eight points on the IES-R a clinically relevant difference between the treatment conditions at post-assessment. For an equivalence design, a sample size of 47 patients per arm was needed (power 80% and two-sided significance level 0.05) to detect medium-sized treatment effects, taking into account a difference of less than eight points (δ) between the post-treatment means for equivalence of the two arms. Sample size per arm was set at 70 to allow for patient attrition of 30%.
Chi-squared tests and independent t-tests were used to compare demographic and clinical characteristics between the treatment groups. Repeated measurement analyses were used to study changes over time between the treatment groups. We applied mixed linear models to take into account that measurements within the same individual are correlated, and to allow the model to calculate estimates when data were missing at certain assessments. An auto-regressive pattern was imposed on the covariance structure for measurements within the same individual (AR1). Mean scores for each outcome at the post-measurements (17 for IES-R and 2 for SI-PTSD and HADS) were modelled as a function of the intervention given (two levels), time since intervention (as a categorical variable with 17 or 2 levels), the baseline measurement (continuous), and the interaction between time and intervention. The main question, whether the response pattern was different between the treatment conditions, was evaluated by jointly testing whether the treatment difference was zero at all post-measurements. If the overall test was significant, we examined the size of the treatment effect by calculating the difference in mean scores between the treatment conditions at separate time points, with corresponding 95% confidence intervals in the linear mixed model. All analyses were carried out on an intent-to-treat basis, unless indicated otherwise. P-values of less than 0.05 were considered statistically significant and two-tailed tests were used throughout.
Results
Participants
Figure 1 shows the patient flow through the trial. Completer and drop-out rates did not significantly differ across treatment conditions (χ2 = 1.08, d.f. = 2, P = 0.58). Table 1 displays the baseline and clinical characteristics of the two groups. No significant differences were found in clinical or demographic variables between the groups at baseline, except that the IES-R total score was significantly higher in the brief eclectic psychotherapy group than in the EMDR group (Table 1). Proportions of patients on psychoactive medication did not differ between treatment groups (Table 1). Over the 17 weeks of the trial, proportions of patients who changed psychoactive medication (n = 28) did not significantly differ between treatment conditions (χ2 = 0.01, d.f. = 1, P = 0.91). Medication changes in most cases consisted of reduction or cessation of anxiolytics and these were also equally distributed across treatment conditions (χ2 =1.73,d.f.=1, P = 0.18). Proportions of patients attending concurrent alternative treatments over the course of the trial did not significantly differ between treatment conditions (χ2 = 1.54, d.f. = 1, P = 0.21). Alternative treatments consisted of physiotherapy (n = 17), alternative medicine (n = 15), supportive therapy (n = 10) and self-help groups (n = 1). Referrals at end of treatment (n = 18) were equally distributed across treatment conditions (χ2 = 0.00, d.f. = 1, P = 1.00).
Table 1 Demographic and clinical characteristics at baseline
| Brief eclectic psychotherapy group (n = 70) |
EMDR group (n = 70) |
Analysis | ||||
|---|---|---|---|---|---|---|
| χ2 | t-test | d.f. | P | |||
| Characteristics | ||||||
| Age, years: mean (s.d.) | 37.3 (10.6) | 38.3 (12.2) | 0.50 | 138 | 0.62 | |
| Female, n (%) | 43 (61.4) | 36 (51.4) | 1.42 | 1 | 0.23 | |
| Education,Footnote a n (%) | 2.35 | 2 | 0.32 | |||
| Low | 14 (20.0) | 17 (24.3) | ||||
| Middle | 38 (54.0) | 29 (41.4) | ||||
| High | 18 (25.7) | 24 (34.0) | ||||
| Ethnicity, n (%) | 0.76 | 4 | 0.94 | |||
| Dutch | 37 (52.9) | 36 (51.4) | ||||
| Surinamese | 10 (14.3) | 8 (11.4) | ||||
| Turkish | 7 (10.0) | 6 (8.6) | ||||
| Moroccan | 4 (5.7) | 5 (7.1) | ||||
| Other | 12 (17.1) | 15 (21.4) | ||||
| Trauma,Footnote b n (%) | 1.46 | 0.94Footnote c | ||||
| Assault | 39 (55.7) | 35 (50.0) | ||||
| Sexual assault | 7 (10.0) | 9 (12.9) | ||||
| Accident | 12 (17.1) | 14 (20.0) | ||||
| Disaster | 4 (5.7) | 6 (8.6) | ||||
| War-related | 4 (5.7) | 3 (4.3) | ||||
| Other | 4 (5.7) | 3 (4.3) | ||||
| Clinical features | ||||||
| Earlier traumatic experiences, n (%) | 40 (57.1) | 36 (51.4) | 0.60 | 1 | 0.44 | |
| Complex trauma | 15 (21.4) | 11 (15.7) | 0.76 | 1 | 0.39 | |
| On psychoactive medication, n (%) | 30 (42.9) | 29 (41.4) | 0.03 | 1 | 0.86 | |
| Antidepressants | 13 (18.6) | 12 (17.1) | 0.05 | 1 | 0.83 | |
| Anxiolytics or opiates | 18 (25.7) | 23 (32.8) | 0.86 | 1 | 0.35 | |
| Propranolol | 3 (4.3) | 2 (2.9) | 1.00Footnote c | |||
| Antipsychotics | 1 (1.4) | 1 (1.4) | 1.00Footnote c | |||
| Time since trauma in months, mean (s.d.) | 31.5 (50.6) | 29.1 (62.0) | 0.25 | 138 | 0.80 | |
| IES-R PTSD total, mean (s.d.) | 79.9 (16.9) | 72.8 (20.7) | 2.25 | 137 | 0.03Footnote * | |
EMDR, eye movement desensitisation and reprocessing; IES-R, Impact of Event Scale – Revised; PTSD, post-traumatic stress disorder.
a Low: completed elementary school or lower vocational education. Middle: completed high-school or middle-level vocational education. High: completed pre-university, college or university degree.
b All met criterion A1 and A2 of DSM-IV.
c Fisher's exact test.
* Significant at 0.05 level.
Reasons for treatment drop-out are given in Fig. 1. Participants who dropped out during sessions 4–8 scored higher on the IES-R than patients who continued treatment at those time points (all P<0.001). Non-completers were significantly younger than treatment completers (t = –3.60, d.f. = 138, P<0.001) and more likely to be of non-Dutch origin (χ2 = 11.76, d.f. = 1, P<0.005).
Treatment integrity
Of all the interventions started, 48 participants (37.8%, 24 for each condition) were randomly selected for independent scoring of protocol adherence by two raters. The overall mean treatment integrity score was 78 for brief eclectic psychotherapy (s.d. = 9.2) and 81 for EMDR (s.d. = 14.7). Thus, according to the raters, on average 78–81% of the desired elements of the treatment protocol were applied during the interventions. Kappa values ranged between 0.54 for brief eclectic psychotherapy and 0.75 for EMDR, which can be considered indicative of adequate to good agreement between the raters. Treatment integrity scores did not significantly differ for brief eclectic psychotherapy and EMDR (t = 0.73, d.f. = 37, P = 0.48).
Main outcomes
Primary outcome
The results of the intent-to-treat analyses of the primary outcome IES-R are shown in Fig. 2. The mixed-model analysis demonstrated a significant main effect of time (F = 17.99, d.f. = 1065, P<0.001), a significant main effect of treatment condition (F = 12.20, d.f. = 169, P<0.005) and a significant interaction between time and treatment condition (F = 4.00, d.f. = 1065, P<0.001). The response pattern proved to be significantly different for brief eclectic psychotherapy and EMDR (t = 3.49, d.f. = 169, P<0.005). The mean estimated difference on the IES-R between the treatment conditions across the 17 measurements was 13.10 (95% CI 5.69–20.50), corresponding with a large effect size (Cohen's d = 0.75). Mean IES-R total scores at the second post-assessment for brief eclectic psychotherapy were 38.0 (s.d. = 34.4, n = 41) and for EMDR 28.5 (s.d. = 29.6, n = 48). At the second post-assessment, the difference between the treatment conditions was no longer significant (t = 0.70, d.f. = 340, P = 0.48; mean estimated difference 3.70 (95% CI –6.63 to 14.03)).
Additional analyses comparing IES-R scores after every two EMDR sessions with every three brief eclectic psychotherapy sessions showed that the response pattern was also significantly different for brief eclectic psychotherapy and EMDR (t = 2.12, d.f. = 139, P<0.05). Improvement effect sizes from baseline to second post-assessment were large for both treatment conditions (Cohen's d = 1.55 for brief eclectic psychotherapy and Cohen's d = 1.73 for EMDR). The completers-only analysis yielded comparable results for the IES-R scores.
Secondary outcomes
The mixed-model analysis of the SI-PTSD showed a significant main effect of time (F = 37.06, d.f. = 86, P<0.001), a significant main effect of treatment condition (F = 11.05, d.f. = 98, P<0.005) and a significant interaction between time and treatment condition (F = 14.99, d.f. = 86, P<0.001). The response pattern proved to be significantly different for brief eclectic psychotherapy and EMDR (t = 3.32, d.f. = 98, P<0.005). Analysis by time point revealed that SI-PTSD scores were significantly lower for EMDR than for brief eclectic psychotherapy at the first post-assessment, but at the second post-assessment the difference was no longer significant (Table 2). Improvement effect sizes from baseline to second post-assessment were large for both treatment conditions (Cohen's d = 1.95 for brief eclectic psychotherapy and Cohen's d = 2.43 for EMDR).
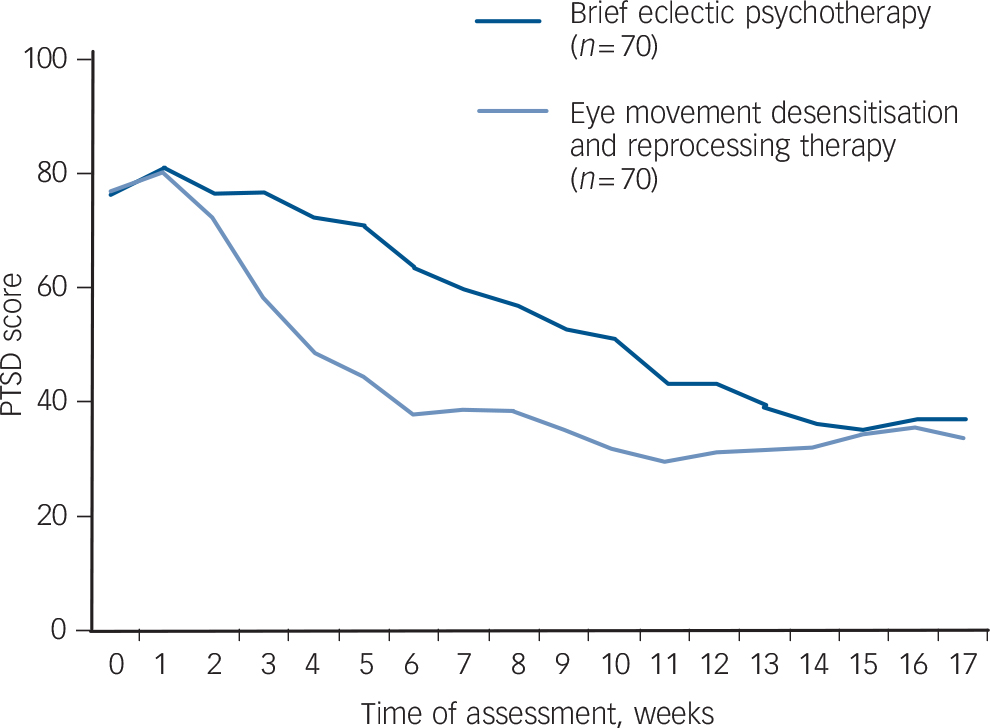
Fig. 2 Changes in post-traumatic stress disorder (PTSD) scores on the Impact of Event Scale – Revised for intent-to-treat analysis.
Mean values at assessment points from a repeated measures model adjusted for baseline value of PTSD score.
Table 2 Intent-to-treat analyses of the effects of treatment on clinician-rated post-traumatic stress disorder, depression and anxiety scores at baseline, first and second post-assessment
| Brief eclectic psychotherapy group | EMDR group | Effect sizes and mean estimated differences between the two groups | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Measure | n | Mean (s.d.)Footnote a | n | Mean (s.d.)Footnote a | d Footnote b | Mean (95% CI) | t-test | d.f. | P |
| SI-PTSD total | |||||||||
| Baseline | 70 | 40.11 (6.30) | 70 | 39.40 (6.16) | 0.71 (71.37 to 2.80) | 0.68 | 138 | 0.50 | |
| First post-assessment | 44 | 31.11 (12.47) | 51 | 19.94 (11.81) | 0.92 | 10.80 (6.37 to 15.23)Footnote c | 4.82 | 146 | <0.001 |
| Second post-assessment | 42 | 20.50 (12.79) | 48 | 17.67 (11.06) | 0.23 | 2.41 (72.10 to 6.92)Footnote c | 1.06 | 150 | 0.29 |
| HADS depression | |||||||||
| Baseline | 70 | 12.07 (4.05) | 69 | 10.93 (4.14) | 1.14 (70.23 to 2.52) | 1.65 | 137 | 0.10 | |
| First post-assessment | 41 | 8.68 (5.57) | 51 | 4.65 (4.39) | 0.80 | 3.58 (1.68 to 5.49)Footnote c | 3.72 | 142 | <0.001 |
| Second post-assessment | 42 | 7.38 (6.42) | 48 | 5.67 (4.54) | 0.31 | 1.47 (70.44 to 3.39)Footnote c | 1.52 | 144 | 0.13 |
| HADS anxiety | |||||||||
| Baseline | 70 | 13.01 (3.94) | 69 | 12.38 (3.49) | 0.64 (70.61 to 1.89) | 1.01 | 137 | 0.32 | |
| First post-assessment | 41 | 10.17 (5.68) | 51 | 5.94 (4.14) | 0.85 | 3.74 (2.03 to 5.46)Footnote c | 4.31 | 139 | <0.001 |
| Second post-assessment | 42 | 8.02 (5.77) | 48 | 6.65 (4.73) | 0.26 | 0.80 (70.93 to 2.52)Footnote c | 0.91 | 140 | 0.36 |
EMDR, eye movement desensitisation and reprocessing; SI-PTSD, Structured Interview for Post-traumatic Stress Disorder; HADS, Hospital Anxiety and Depression Scale.
a. Raw values.
b. Cohen's d, based on raw values.
c. Mean estimated differences from repeated-measures model with treatment condition, time, interaction time and treatment condition, and baseline value.
The mixed-model analysis on HADS depression scores revealed a significant main effect of treatment condition (F = 8.72, d.f. = 97, P<0.005) and a significant interaction between time and treatment condition (F = 5.61, d.f. = 83, P<0.05), but no significant main effect of time (P = 0.63). The response pattern was significantly different for brief eclectic psychotherapy and EMDR (t = 2.95, d.f. = 97, P<0.005). Analysis by time point showed that HADS depression scores were significantly lower for EMDR than for brief eclectic psychotherapy at the first post-assessment, but at the second post-assessment the difference was not significant anymore (Table 2). Improvement effect sizes from baseline to second post-assessment were large for both treatment conditions (Cohen's d = 0.87 for brief eclectic psychotherapy and Cohen's d = 1.21 for EMDR).
Mixed-model analysis on HADS anxiety scores revealed a significant main effect of time (F = 6.49, d.f. = 83, P<0.05), a significant main effect of treatment condition (F = 8.43, d.f. = 98, P<0.01) and a significant interaction between time and treatment condition (F = 14.90, d.f. = 83, P<0.001). The response pattern was significantly different for brief eclectic psychotherapy and EMDR (t =2.90, d.f.=98, P<0.01). Analysis by time point showed that HADS anxiety scores were significantly lower for EMDR than for brief eclectic psychotherapy at the first post-assessment, but at the second post-assessment the difference was no longer significant (Table 2). Improvement effect sizes from baseline to second post-assessment were large for both treatment conditions (Cohen's d =1.01 for brief eclectic psychotherapy and Cohen's d = 1.38 for EMDR).
We found similar results in the completers-only analyses of the SI-PTSD, HADS depression and HADS anxiety scores.
Numbers of patients with psychiatric diagnoses at the first and second post-assessment are shown in Table 3. Significant differences were found for PTSD and major depressive disorder at the first post-assessment; other differences were not significant.
Discussion
The current randomised controlled trial showed that EMDR and brief eclectic psychotherapy had equal effects in terms of reduction of self-reported and clinician-rated PTSD symptoms, depressive symptoms and general anxiety symptoms when statistically controlling for pre-treatment differences. Across all outcomes, the response pattern was significantly different for EMDR and brief eclectic psychotherapy when accounting for baseline differences, indicating that EMDR led to faster symptom decline and brief eclectic psychotherapy to more gradual improvement.
Table 3 Psychiatric diagnoses at baseline, first and second post-assessment
| Brief eclectic psychotherapy group n/N (%) |
EMDR group n/N (%) |
Analysis | |||
|---|---|---|---|---|---|
| χ2 | d.f. | P | |||
| PTSDFootnote a | |||||
| Baseline | 70/70 (100) | 70/70 (100) | |||
| First post-assessment | 21/44 (47.7) | 4/51 (7.8) | 19.38 | 1 | <0.001 |
| Second post-assessment | 6/42 (14.3) | 3/48 (6.3) | 0.30Footnote b | ||
| Major depressive disorderFootnote c | |||||
| Baseline | 47/70 (67.1) | 37/70 (52.9) | 2.98 | 1 | 0.08 |
| First post-assessment | 16/44 (36.4) | 7/51 (13.7) | 6.60 | 1 | <0.05 |
| Second post-assessment | 8/42 (19.0) | 7/48 (14.6) | 0.32 | 1 | 0.57 |
| Anxiety disorder other than PTSDFootnote c | |||||
| Baseline | 14/70 (20.0) | 8/70 (11.4) | 1.94 | 1 | 0.16 |
| First post-assessment | 4/44 (9.1) | 5/51 (9.8) | 0.01 | 1 | 0.91 |
| Second post-assessment | 5/42 (11.9) | 5/48 (10.4) | 0.05 | 1 | 0.82 |
EMDR, eye movement desensitisation and reprocessing; PTSD, post-traumatic stress disorder.
a. Structured Interview for Post-traumatic Stress Disorder.
b. Fisher's exact test.
c. Structured Clinical Interview for DSM-IV Axis I Disorders.
Efficacy and mechanism
Several explanations can be found for the faster symptom reduction in EMDR. First, the type of exposure to the traumatic event is different for brief eclectic psychotherapy and EMDR. In EMDR, short interrupted exposures to the ‘hotspots’ of the trauma are alternated with free association (which can involve moving quickly through scenes and associating with memories of other events that the person has experienced), and this associative process is seen as effective memory processing. Reference Schubert and Lee27 During brief eclectic psychotherapy, on the other hand, in every exposure session a part of the trauma is relived in great detail with a focus on experiencing grief, leading to more gradual trauma processing. The differences in exposure type and duration may explain the initial gradual change observed in brief eclectic psychotherapy and the faster change in EMDR. Due to the repetitive nature of interventions in both traditional prolonged exposure and EMDR, it is possible that the effects would be obtained faster than in brief eclectic psychotherapy. Further symptom reduction was observed for brief eclectic psychotherapy during the second treatment phase. So in this treatment the cognitive restructuring part, in which patients reflect on their trauma story and its meaning for their life, proved to be important for recovery from PTSD. Possibly, adding this phase to EMDR, as is sometimes done in clinical practice, could lead to further symptom reduction as well. Further research could address this by detailed study of the effective ‘ingredients’ of these treatments.
A second possible explanation for faster improvement with EMDR is that the session duration is 30–45 min longer than for brief eclectic psychotherapy. Additional analyses corrected for the difference in session duration still showed that EMDR led to faster symptom improvement. In this context it is interesting to note that strictly speaking the exposure time to the traumatic memory is shorter in EMDR than in brief eclectic psychotherapy. In brief eclectic psychotherapy the exposure is uninterrupted for 15–20 min, whereas in EMDR the exposure is limited to a few minutes in which the patient focuses on traumatic images. The session durations were those standard in clinical care and were therefore implemented as such in our study. Optimal session duration and frequency should be investigated in future research.
Comparison of our findings with previous studies
The results of our study are in line with previous trials that compared other trauma-focused CBT approaches with EMDR (i.e. the pilot study that found that EMDR leads to faster reduction in PTSD symptoms than trauma-focused CBT after a few sessions Reference Ironson, Freund, Strauss and Williams7 and trials reporting that both treatments led to equal improvements on PTSD symptoms post-treatment Reference Ironson, Freund, Strauss and Williams7,Reference Vaughan, Armstrong, Gold, O'Connor and Jenneke28–Reference Rothbaum, Astin and Marsteller32 ). Although the effects at the end-point were equal, it should be noted that the current study cannot address with certainty whether the treatments are equivalent at that point because the confidence interval of the primary outcome contains the pre-specified difference of eight points. Reference Jones, Jarvis, Lewis and Ebbutt33 This is attributable to the fact that the variance at the second post-assessment proved to be larger than we expected in our power analysis. The number of participants who completed their treatment and completed their assessment closely approximated the number of participants needed per arm in the power analysis, so we anticipate that drop out did not bias our results.
The magnitude of change in our trial is larger than in some previous studies. Although both baseline and post-treatment levels of the IES-R in our sample seem higher than in other studies, this is attributable to the different scoring method adopted by the Dutch version of the instrument. The PTSD improvement effect sizes from pre- to post-treatment for both brief eclectic psychotherapy and EMDR in our study were higher than those found across all active PTSD treatments in meta-analyses. Reference Bradley, Greene, Russ, Dutra and Westen13,Reference Bisson, Ehlers, Matthews, Pilling, Richards and Turner34 The improvement effect sizes of EMDR in the current study were higher than the overall effect size for EMDR as reported in these meta-analyses, and brief eclectic psychotherapy improvement effect sizes were comparable with those of trauma-focused CBT.
Strengths and limitations
A strength of the current study is that we succeeded in comparing response patterns in two trauma-focused treatment protocols in a large, culturally diverse urban sample using a design that took into account sound methodology as well as clinical relevance. We emphasised scientific rigour by randomisation, protocol adherence, treatment integrity checks and independent assessment of outcome. The clinical meaningfulness of the results was increased by the inclusion of some elements of practical trials (trials that include elements of effectiveness designs), such as the inclusion of a heterogeneous trauma population, treatment duration dependent on the patients’ recovery and the use of non-expert therapists.
We also recognise the limitations of our study. The foremost limitation is the drop out from both therapy and the assessments. However, the treatment drop-out rates of the current study are comparable with those in other trials. Reference Hembree, Foa, Dorfan, Street, Kowalski and Tu35–Reference Schottenbauer, Glass, Arnkoff, Tendick and Gray37 Interestingly, around 10% of patients dropped out before treatment, which might indicate a difficulty in starting trauma therapy. The drop-out rates from assessments were somewhat higher than in other studies, especially for brief eclectic psychotherapy. Nevertheless, for the primary outcome we were able to analyse a large proportion of the randomised patients because the data from the treatment sessions enabled us to calculate estimates of the response patterns if patients dropped out of later assessments.
A further limitation was that the number of brief eclectic psychotherapy exposure sessions fluctuated to a small degree, which could have exerted a small influence on our first post-assessment comparison. Finally, concurrent treatments such as pharmacological treatment, changes in pharmacological treatment and non-trauma-focused therapies may have contributed to the therapy effects for a minority of the patients. However, concurrent treatments were equally distributed across both brief eclectic psychotherapy and EMDR conditions and it may be presumed that they had an equal effect in both groups.
Clinical implications
In conclusion, this study demonstrates that both brief eclectic psychotherapy and EMDR are effective psychotherapeutic treatments, but EMDR may be a more time-efficient method for treating PTSD. Effect sizes and rates of diagnostic change were large for both treatment methods, indicating that the majority of people with PTSD benefit from trauma-focused psychotherapy. Symptom improvement appeared to occur at an earlier stage in EMDR than in brief eclectic psychotherapy, which may make patients more keen to choose this treatment method. However, brief eclectic psychotherapy may be preferred if patients value reflection on the trauma story and its meaning for their lives. Patient and therapist preferences have been shown to play an important role in the choice of treatment method. Reference Van Minnen, Hendriks and Olff38 Because with both treatments patients dropped out, we should keep searching for new therapeutic strategies. Reference Schnyder39 Future studies also need to prioritise investigating the reasons for premature treatment drop-out. Possibly, more attention should be given to psychoeducation and motivation to overcome persistent avoidance. This may especially be true for younger patients, those from minority ethnic groups and those who do not show symptom improvement over the first sessions and who drop out from treatment more frequently. Furthermore, future research needs to determine which patient groups benefit most from which form of psychotherapy. Finally, investigating long-term treatment effects is essential in order to offer individuals the best possible treatment option.
Funding
This study was supported by the Academic Medical Centre, Amsterdam, The Netherlands.
Acknowledgements
The authors thank the patients who gave their consent to participate in this study. We also thank the therapists and assessors for their contribution to the study, and especially the coordinators Noor de Bruijn, Ineke Vrijlandt and Renée Hutter.










eLetters
No eLetters have been published for this article.